A slowdown in the conduction of cardiac impulses through the ventricular myocardium occurs due to obstacles in the form of a focus of inflammation, scar tissue (after heart attacks), degenerative or tumor processes. Common causes of impaired conduction are: hypertension, atherosclerosis and heart defects.
Manifestations may be absent with local blocks; in case of widespread damage to the heart muscle, patients are concerned about dizziness and fainting. Treatment uses medications and may require a pacemaker.
Classification criteria
Intraventricular blockades are classified according to a number of characteristics:
- According to the localization of stopping the advance of the depolarization wave:
- single-bundle (block at the level of one segment of the His bundle);
- double-bundle (block at the level of two segments of the His bundle);
- three-beam (block for promoting the depolarization wave in all branches).
- According to the degree of blocking of the excitation wave:
- complete (no propagation of the excitation wave);
- incomplete (the impulse moves slowly in the conductive system).
- According to the frequency of arrhythmia registration:
- transient (appear periodically under the influence of certain factors);
- permanent (registered all the time).
- It is customary to distinguish such a form as focal (local) intraventricular block, when the impulse block occurs in a certain zone. This form is recorded with necrosis of myocardial fibers.
- There is also such a disorder as nonspecific (arborization) intraventricular block, which is characterized by changes that do not fall within the accepted criteria.
What is the danger of the condition
A conduction block on one leg, especially a partial one, does not pose a threat to the patient if the underlying disease is compensated, there are no signs of its progression, and the impaired conduction does not slow down the rhythm of contractions.
Two-bundle, and especially three-bundle, can stop the spread of impulses from the atria to the ventricular myocardium. This condition, complete atrioventricular block, is life-threatening as it leads to episodes of loss of consciousness similar to Morgagni-Adams-Stokes syndrome. The result of complete blocking of signals is the cessation of contractions and the death of the patient.
Watch the video about cardiac rhythm and conduction disturbances:
Etiology
- Diseases accompanied by disruption of the right side of the heart (chronic pathology of the bronchopulmonary system, mitral valve stenosis, congenital defects of the circulatory system).
- Chronic forms of myocardial ischemia, often combined with high blood pressure.
- Acute myocardial infarction (especially the lower wall and apex).
Due to the disruption of the propagation of excitation to the right parts of the heart, the impulse primarily covers the left ventricle and the interventricular septum.
Then, along the myocardial fibers, a wave of depolarization delays the right ventricle.
Treatment
Stable long-term intraventricular block does not require specific treatment. The initial detection of intraventricular changes, especially in an elderly patient, requires hospitalization and a full examination to determine the causes.
Ischemia suggests the use of coronary lytics and careful use of weak beta-blockers.
If the inflammatory nature of the changes is detected, a course of antibacterial therapy and hormonal agents is carried out.
In case of combination with chronic heart failure, small doses of digitalis and diuretics are used.
It is important to promptly decide on the advisability of installing a pacemaker. This is especially true in cases of two- and three-bundle blocks.
Etiological factors
- Diseases associated with pathological functioning of the right ventricle (mitral valve stenosis, pulmonary hypertension, severe tricuspid valve regurgitation).
- Chronic forms of myocardial ischemia.
- Arterial hypertension.
- Infectious pathologies (myocarditis).
- Overdose of drugs (quinidine, digitalis preparations, beta blockers).
- Acceptable norm at a young age, including children and adolescents.
The occurrence of such a conduction disorder is associated with a slow propagation of the depolarization wave along the right bundle branch due to destruction in the myocardial fibers or hypertrophy of the right parts of the heart.
Three-bundle blockades
Mechanism of conduction disturbance: when incomplete, the electrical impulse follows from the atria to the ventricles along one of the branches (less affected). In this case, signs of atrioventricular block are detected. Complete block is characterized by third degree atrioventricular obstruction and an altered source of ventricular rhythm.
The causes are severe organic damage to the myocardium, already listed above.
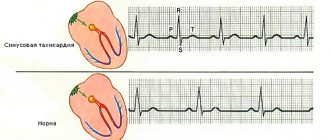
The shape of the teeth indicates the type of intraventricular block
Diagnostics
A pathology such as intraventricular block is diagnosed on the basis of complaints, anamnesis, examination, and examination. There are no specific complaints in patients with the pathology in question. The symptoms of the disease, which may be accompanied by a violation of intraventricular conduction, come to the fore.
Anamnestic information reveals the presence of chronic and previous diseases, cardiac pathology in close relatives, and existing risk factors.
During a physical examination, it is impossible to determine the presence of a blockade in a patient, since this arrhythmia does not have specific signs. It is possible to detect signs of the disease that lead to pathological changes in the circulatory system, which is subsequently accompanied by arrhythmia.
Such signs include changes in the color of the skin, heart murmurs during auscultation, an increase in the boundaries of cardiac dullness, pasty legs, shortness of breath and many others.
The diagnosis is based on recording an electrocardiogram in 12 standard leads and 24-hour Holter monitoring.
An ECG can detect characteristic signs inherent in each type of intraventricular conduction disorder. Transient arrhythmia is diagnosed based on Holter monitoring.
Additionally, ultrasound diagnostics, coronary angiography, scintigraphy, spirometry, computed tomography, radiography, and laboratory tests are prescribed.
Types of ventricular blocks
According to V.L. Doshchitsin’s classification, all intraventricular conduction disorders are divided into:
- mono-, bi- and trifascicular depending on the damage to one or two or three bundles;
- focal: local damage is not confirmed in all ECG leads;
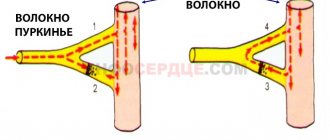
- arborization: localized in the terminal part of Purkinje fibers;
- transient: changes alternate with correct conductivity;
- persistent;
- complete and incomplete;
- alternating: first one or another type of blockade is detected.
A pathological process can cause an impulse block at any level
Depending on the location of the impulse interruption, blockades are distinguished:
- monofascicular (single-bundle): a block of the left anterior or posterior, only the right bundle branch is detected in isolation;
- bifascicular (two-bundle): available in two versions: unilateral (left leg) or bilateral (right with the left anterior branch, right with the left posterior).
- trifascicular (three-bundle).
The type of blockade is reflected in the transcript of the electrocardiogram. The conduction of impulses from the supraventricular nodes of the heart slows down or is completely interrupted. This disrupts the sequence of excitation of the ventricles, affects the biochemical processes in the myocardium, and the fullness of cardiac output.
The reasons for different types of blockades differ from each other and cause different changes. Let us consider how intraventricular conduction disturbance occurs in myocardial diseases.
Causes of the disease
In general, the causes of VZhB do not differ from those of other conduction disorders (atrioventricular, synatrial block). All etiological factors are divided into organic and functional. The former include congenital and acquired heart defects, valvular calcification, ischemic disease, idiopathic fibrosis in Lenegra and Lev's disease, myocardial tumors.
The most common cause of blockades is post-infarction cardiosclerosis with subsequent proliferation of connective tissue in the necrosis zone. Such forms of pathology are considered irreversible.
A common functional factor in the occurrence of pathology is the use of high doses of antiarrhythmic drugs of class 1C, 1A. Representatives of these groups are “Propafenone”, “Amiodarone”. Intraventricular blockades develop with hyperkalemia, acidosis, and insufficient oxygen in the blood. Sometimes it is not possible to determine the cause of the disease. In this case, they speak of the idiopathic form. It is important to remember that dysfunction of the autonomic nervous system, leading to the formation of AV blockade, does not affect intraventricular conduction.
Classification
There are several classifications.
According to the degree of violation there are:
- Incomplete blockade (partial), when the passage of the impulse only slows down, and the QRS complex has a length of 0.10-0.11.
- Complete blockade, when the conduction of the impulse completely stops and the QRS complex expands more than 0.12.
- According to the location of the violation, they are distinguished:
- Monofascicular or single-start, when a conduction disorder is formed in one branch of the His bundle - in the right leg, the left leg of the anterior branch, or the left leg of the posterior branch.
- Bifascicular or bifascicular block, when conduction is disrupted in the left leg, the left leg of the anterior branch and the right leg, or the left leg of the posterior branch and the right leg.
- Trifascicular or three-fascicle blockade, when the disorder occurs in all three branches.
- Local, peri-infarction or focal blockade, when local splitting of the QRS complex occurs. That is, the lesion occurs in some limited area of the left ventricle, in a certain area. As a rule, a lesion forms in the area adjacent to the resulting necrotic area during myocardial infarction. In other words, it arises distal to the main branches of the left and right bundle of His.
- Peripheral intraventricular block is called if the peripheral branches of the legs are involved in the process.
- Proximal, when the lesion is located inside the His bundle.
- Distal blockade is called if the lesion is localized at the level of the branches of the left leg or in the right.
By nature, intraventricular blockades are divided into:
- Permanent, when there is a constant disturbance in the conduction of the impulse.
- Variable or intermittent. You can also find names such as alternating, transitional or latent. All these are names of the same disorder, when the passage of the rhythm slows down, less often stops, for some reason, and then is restored again.
There is also the concept of nonspecific intraventricular blockades or arborization ones, when the electrocardiogram data in any one or several branches does not fit the currently available signs. At the same time, the width of the QRS complex does not change significantly. This picture is observed when the patency of the impulse along the distal (terminal) branches of the legs is impaired. However, with diffuse lesions of the heart muscle, the ventricular complex always expands.
They are also distinguished by the degree of damage: first, second, third and fourth degrees.
All types of intraventricular blockades can be combined with each other. In clinical cardiology, it is customary to indicate in detail what type of disorder. This further helps in prescribing adequate treatment.
Symptoms
As a rule, the disease does not have pronounced symptoms, except for general fatigue and tiredness. With transverse incomplete blockades, loss of pulse and/or heart sounds may occur. Patients sometimes complain of a feeling of a sinking heart. In cases of complete transverse blockades, persistent bradycardia occurs with all its clinical manifestations. In these cases, Dahms-Stokes-Morgagni syndrome often occurs. If the transverse complete block is also distal, then the risk of developing angina or heart failure, and sometimes sudden death, increases.
Diagnostics
Usually one ECG is enough to make a diagnosis. If necessary, the doctor may prescribe an ultrasound of the heart. And for intermittent blockades - Holter ECG monitoring.
Causes
- Myocarditis.
- Ischemic myocardial disease (CHD).
- Congenital heart defects.
- Cardiomyopathies.
- COPD
- Aortic stenosis, especially complicated by calcification.
- Heart bruise.
- Hyperkalemia.
- Hypertonic disease .
- Heart operations.
- Neoplasms of the heart.
- Muscular progressive dystrophy.
- Lenegra's disease.
- Syphilitic gumma.
- Lev's disease.
- Overdose of procainamide, quinidine, strophanthin K.
- Acquired defects, especially with rheumatoid lesions, usually cause the formation of a right leg.
- Cor pulmonale also usually causes damage to the right leg.
Treatment
The bundle branch block is mild and usually does not require any treatment. Moreover, it is not amenable to drug therapy. It should only be taken into account when prescribing medications. For proximal blockades, atropine or its analogues are sometimes prescribed, but the effect is short-lived. Therefore, all therapy ultimately comes down to treating the disease that caused the blockade. In other words, to eliminate the cause.
In case of Dams-Stokes-Morgagni syndrome or the occurrence of heart failure and/or peripheral circulation, as well as angina, permanent or temporary ventricular stimulation is prescribed.
Treatment prognosis and prevention.
The prognosis of treatment largely depends on the degree of damage to the myocardial conduction system and the timely administration of adequate treatment for the causative disease.
Prevention consists of timely treatment of the disease, which can lead to intraventricular blockades, maintaining a healthy lifestyle and regular professional activities. examinations by a doctor.
Most often it occurs in the form of blockade of the His bundle branch - right or left. No complaints. During auscultation, bifurcation or splitting of the first and second sounds is sometimes heard due to asynchronous ventricular systole.
ECG signs: The heart rhythm is sinus, regular. With complete blockade of the right leg
His bundle (Fig. 51) the duration of the QRS complex is more than 0.12 s; high R wave in lead V 1-2. Often in V 1-2 before the R wave a small r is recorded, the QRS complex in the form of rsR" or rSR", rR". The same QRS complexes are recorded in standard III and AVF leads. ST and T in these leads are deviated discordantly from the main QRS complex. In the left chest leads (V 5-6) a wide and jagged S wave is detected; the same shape of the QRS complex in standard I and aVL leads. The electrical axis of the heart is vertical or deviated to the right.
With complete blockade of the left leg
His bundle (Fig. 52) the duration of the QRS complex is more than 0.12 s; in I, aVL, V 5-6 a widened, jagged R wave is determined; in III, aVF, V 1-2 - wide S; ST and T are deviated discordantly from the main direction of the QRS complex. The electrical axis is horizontal or tilted to the left.