Tricuspid valve
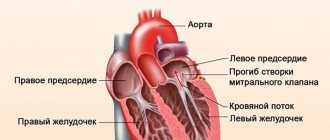
Large vessels arise from the chambers of the heart. The afferent veins are the aorta and pulmonary trunk, the afferent veins are the pulmonary veins and the vena cava. The chambers of the heart work alternately: first the atria contract, and then, when the atria relax, the ventricles begin to contract. The functioning of the heart and blood vessels is regulated by heart valves: bicuspid or mitral, located between the left sections, and tricuspid or tricuspid, located between the right atrium and the right ventricle.
All three leaflets of the valve of the right parts of the heart consist of elastic and elastic connective tissue, they fit tightly to each other, preventing the possibility of blood flowing back during contractile work of the right ventricle. The valve leaflets close the right atrioventricular orifice, that is, the round communication between the chambers of the heart.
Degrees and forms
Tricuspid regurgitation developing against the background of a defect can be:
- primary, not accompanied by pulmonary hypertension and appearing against the background of primary pathology of the heart muscle;
- secondary, appearing against the background of hypertrophy of the right ventricle and pulmonary hypertension;
In modern medical practice, there are 4 degrees of tricupid valve prolapse:
First. It is characterized by reverse blood flow, which does not disrupt the general process of its movement through the vessels. There is a slight prolapse of the tricuspid valve without significant regurgitation.
- Second. In case of prolapse of the tricuspid valve of the 2nd degree, reverse flow of blood is observed and passes at a distance of 20 mm from the tricupid valve.
- Third. The distance increases by more than 20 mm.
- Fourth. Regurgitation is clearly expressed, extending over a long distance from the cavity of the right atrium.
Tricuspid valve prolapse can be congenital, resulting from heart defects, or acquired, which develops in adulthood for a number of reasons.
The following video will tell you more about tricuspid valve regurgitation:
Clinical picture
In the early stages of the formation of TB prolapse or with the development of a pathological process of 1st degree of severity, the patient, as a rule, does not have any complaints from the heart, and the disease can only be suspected during a medical examination. The first symptoms of the disease appear when the volume of regurgitation increases. In severe forms of tricuspid valve insufficiency, patients experience the following clinical manifestations of the pathological process:
- feeling of weakness, tiredness and fatigue;
- swelling of the distal parts of the lower extremities and the anterior abdominal wall;
- visible pulsation of the neck veins;
- decreased diuresis;
- palpitations with rhythm disturbances (tachycardia);
- pain in the heart area;
- dyspnea;
- in severe cases - hemoptysis.
When visiting a doctor, patients with degrees 2, 3 and 4 of tricuspid valve prolapse complain of a feeling of weakness, loss of performance and heaviness in the abdomen and legs. Often in such patients, complaints related to a decrease in the volume of urine produced come to the fore, which they mistakenly perceive as kidney pathology.
Do you trust doctors and their prescriptions?
Yes
20.4%
No
11.94%
I trust, but I check all medications for reviews on the Internet from people who have already tried them and only then do I start taking them.
50.25%
Yes, but only to appointments and doctors from paid clinics.
17.41%
Voted: 201
Symptoms of PTC from the heart:
- hypertrophy of the right heart;
- symptoms of damage to other valves;
- pansystolic murmur, which increases with inspiration;
- On auscultation, the sounds of a “flapping sail” are heard above the heart
In addition to changes in the heart, tricuspid valve prolapse is also indicated by an increase in the size of the liver, dyspeptic disorders, heaviness in the right hypochondrium and portal hypertension.
According to statistics, prolapse with tricuspid valve insufficiency is most often diagnosed in patients who regularly use drugs.
This is due to the fact that taking intoxicating drugs in unsanitary conditions is one of the main causes of infectious or toxic endocarditis, as a result of which the valve leaflets lose their elasticity and ability to completely close in diastole.
Causes
The most common cause of PTC is infective endocarditis. Most often, this disease develops due to unsanitary conditions while taking drugs. In children, prolapse occurs due to congenital defects, such as Epstein's anomaly, during which the valve flap moves into the right ventricle. Other causes of PTC include:
- a carcinoid tumor that releases hormones that damage the valve;
- Marfan syndrome;
- trauma to the thoracic region;
- rheumatism;
- rheumatoid arthritis;
Regurgitation that occurs due to PTC can vary in level depending on several factors. It may increase due to pulmonary hypertension and other diseases that increase blood pressure.
Why does PTC occur?
Pathological failure of the tricuspid valve can be congenital or acquired. Most often, congenital abnormal defects of the valve leaflets and its fibrous ring arise as a result of intrauterine exposure to toxic factors on the fetus. This happens around 3-9 weeks of pregnancy, when vital organ structures are being formed in the body of the unborn baby. Congenital tricuspid valve insufficiency can also occur due to connective tissue pathologies, both genetic (Morphan's syndrome) and acquired.
Acquired tricuspid valve prolapse develops secondary, against the background of other pathological conditions:
- rheumatism;
- rheumatoid arthritis;
- drug addiction (less often alcoholism);
- carcinoid syndrome (the development of a carcinoid tumor provokes the appearance of a hormone in the blood that causes irreparable damage to the valve structures of the heart);
- infectious heart lesions (infectious endocarditis);
- damage to the chordae and muscles of the tricuspid valve;
- chest injuries.
In a healthy heart, the valve closes completely; with prolapse, the valve does not close completely.
Acquired tricuspid valve prolapse develops secondary, against the background of other pathological conditions:
Symptoms
If regurgitation is minor, prolapse does not have pronounced symptoms. Symptoms in this case will be subjective like:
- A decrease in the volume of urine produced over a specific period of time compared to normal health;
- Fatigue and high fatigue.
- Bloating.
- Swelling of the lower extremities.
- High heart rate.
Signs by which the disease can be differentiated from others are:
- increased liver size;
- increased size of the atrium and right ventricle;
- pansystolic heart murmur that increases with inspiration;
- heart disease;
While symptoms may vary depending on the characteristics of the patient’s body, the signs remain the same for everyone.
Classification
Mitral valve prolapse can be:
- Primary. Associated with connective tissue weakness, which occurs with congenital connective tissue diseases and is often transmitted genetically. With this form of pathology, the mitral valve leaflets are stretched, and the retaining leaflets of the chord are lengthened. As a result of these violations, when the valve closes, the flaps protrude and cannot close tightly. Congenital prolapse in most cases does not affect the functioning of the heart, but is often combined with vegetative-vascular dystonia - the cause of symptoms that patients associate with heart pathology (periodically occurring functional pain in the chest, cardiac arrhythmias).
- Secondary (acquired). Develops in various heart diseases that cause disruption of the structure of the valve leaflets or chords. In many cases, prolapse is provoked by rheumatic heart disease (an inflammatory disease of the connective tissue of an infectious-allergic nature), undifferentiated connective tissue dysplasia, Ehlers-Danlos and Marfan diseases (genetic diseases), etc. In the secondary form of mitral valve prolapse, pain that passes after taking nitroglycerin is observed, interruptions in heart function, shortness of breath after exercise and other symptoms. If the cardiac chords rupture as a result of a chest injury, emergency medical attention is required (the rupture is accompanied by a cough, during which foamy pink sputum is released).
Primary prolapse, depending on the presence/absence of noise during auscultation, is divided into:
- The “silent” form, in which symptoms are absent or scanty, and noises and “clicks” typical for prolapse are not heard. Detected only by echocardiography.
- Auscultatory form, which, when auscultated, is manifested by characteristic auscultatory and phonocardiographic “clicks” and noises.
Depending on the severity of the sagging of the valves, mitral valve prolapse is distinguished:
- I degree - the doors bend by 3-6 mm;
- II degree - there is a deflection of up to 9 mm;
- III degree - the sashes bend by more than 9 mm.
The presence of regurgitation and the degree of its severity are taken into account separately:
- I degree – regurgitation is mild;
- II degree – moderately severe regurgitation is observed;
- III degree - there is pronounced regurgitation;
- IV degree – regurgitation is severe.
- Mitral. It separates the cavity of the left atrium and the ventricle and consists of two valves - anterior and posterior. Prolapse of the anterior valve leaflet is much more common than the posterior one. Special threads called chords are attached to each of the valves. They provide contact between the valve and muscle fibers, which are called papillary or papillary muscles. For the full functioning of this anatomical formation, the joint coordinated work of all components is necessary. During cardiac contraction - systole - the cavity of the muscular cardiac ventricle decreases, and accordingly the pressure in it increases. In this case, the papillary muscles are activated, which close the exit of blood back into the left atrium, from where it flows out of the pulmonary circulation, enriched with oxygen, and, accordingly, the blood enters the aorta and then, through arterial vessels, is delivered to all organs and tissues.
- Tricuspid (three-leaf) valve. It consists of three doors. Located between the right atrium and ventricle.
- Aortic valve. As described above, it is located between the left ventricle and the aorta and does not allow blood to return to the left ventricle. During systole, it opens, releasing arterial blood into the aorta under high pressure, and during diastole, it is closed, preventing blood from flowing back to the heart.
- Pulmonary valve. It is located between the right ventricle and the pulmonary artery. Similar to the aortic valve, it prevents blood from returning to the heart (right ventricle) during diastole.
Diagnostics
With a low level of regurgitation, the disease is difficult to differentiate from others based on symptoms. Therefore, the doctor, after collecting family history and complaints, listening to the heart for murmurs, prescribes additional examinations:
- X-ray of the chest and heart with contrast of the esophagus.
- Phonocardiography.
- Ventriculography.
- ECG showing enlargement of the heart.
- Probing of the right parts of the heart muscle.
- EchoCG with Doppler to measure pressure in the heart.
Additional consultation with a cardiologist and therapist is also required.
Causes of congenital tricuspid regurgitation
The most common causes of this congenital pathology are:
- underdevelopment of valve leaflets;
- abnormal development (number) of valve leaflets;
- connective tissue dysplasia;
- Ehlers-Danlos syndrome;
- Marfan syndrome;
- Ebstein's anomaly.
Tricuspid regurgitation in the fetus is very rare in isolation; it is usually combined with other heart defects. This valve insufficiency may be part of the mitral-aortic-tricuspid defect.
Treatment
If PTC does not cause significant discomfort to the patient, then treatment is not required. However, if acute symptoms appear, it is necessary to immediately begin to eliminate them. Treatment is prescribed depending on the degree of pathology.
Therapeutic
The therapeutic technique is intended for first-degree tricuspid valve prolapse. It comes down to normalizing the patient’s condition and constant monitoring of him, that is, observation by a cardiac surgeon. The patient is shown:
- Give up bad habits like smoking and alcohol, which affect blood vessels.
- Stick to a low-fat diet.
- Perform minimal physical exercise to strengthen the heart muscle.
It is also recommended to visit a massage therapist or osteopath, and undergo acupuncture if desired.
Medication
Drug treatment is mostly aimed at relieving the symptoms of the disease rather than curing it, as well as treating heart failure and pulmonary hypertension. For this, the patient is prescribed:
- diuretics;
- venous vasodilators;
- ACE inhibitors;
- anticoagulants;
- beta blockers;
- cardiac glycosides;
- metabolic drugs;
Depending on the causes of PTC and concomitant diseases, other medications may be prescribed.
Surgical
Surgical treatment is indicated for PTC of the third or fourth degree. For this use:
- Tricuspid valve repair: according to Boyd. A U-shaped suture is placed and tightened on the fibrous ring, which narrows the valve opening.
- by De Vega. A semi-purse-string suture is placed on the fibrous ring.
- according to Carpentier. To narrow it, the support ring is hemmed.
Prosthetics are usually resorted to if the patient suffers from infective endocarditis, there is no effect from plastic surgery, or the valve is changed at the structural level. Prosthetics is a complex operation that can often be complicated.
Folk remedies
Treatment with traditional medicine can only be used in combination with conservative treatment and at the first stage of PTC. In other cases, it may interfere, since it will suppress symptoms, and the patient may miss a critical condition.
The following recipes are used to treat PTC:
- Herbal decoction. Flowers of hawthorn, heather and thorn are used in equal parts. Table. Add a spoonful of the mixture to a glass of hot boiled water and place in a water bath for 16 minutes. Strain the resulting broth and drink in two doses. Repeat the next day.
- Rosemary tincture. You need to take 100 grams of dried rosemary leaves and pour 2 liters of dry red wine over them. Infuse the mixture for 2 months in a dark place, then take 50 ml three times a day.
- Mint decoction. Chain. A spoonful of dry mint is poured into 300 ml of hot boiled water and left for an hour. Then it is filtered and taken half a glass three times a day.
It is also recommended to drink decoctions of hawthorn, motherwort, lemon balm, thyme, calendula, chamomile and oregano.
Process mechanism
With regurgitation of the 1st degree, the patient’s hemodynamics are initially locally disturbed, which over the years turns into a persistent anatomical defect.
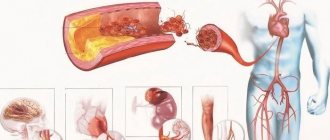
In a healthy person, blood moves through the parts of the heart in only one direction. The cycle ends in the left ventricle, the blood flows into the aorta, and from there along a large circle of branches. The heart is a group of chambers separated from each other by valves, so the connective fluid tissue does not move back.
The tricuspid structure separates the right atrium from the ventricle. If the connective tissue has defects, it weakens and the blood begins to flow backwards. This pathological process is called regurgitation.
The results of this deviation:
- blood is transported incorrectly through the pulmonary circulation;
- little blood is released into the aorta.
Over time, because of this, in the process of hemodynamics the following develop:
- generalized disorders;
- tissue hypoxia;
- multiple organ failure.
IMPORTANT! Anomalies of the tricuspid valve cannot be considered a death sentence. If the problem is detected before the development of the fourth stage, the patient can undergo surgery. Most often, such surgery is very effective. After it, patients quickly recover and can live their normal lives.
Disease prevention
The main prevention of PTC comes down to the treatment of rheumatism and the prevention of its relapses, the same applies to other diseases that can cause the appearance of pathology.
- A person at risk must be constantly monitored by a cardiologist and cardiac surgeon.
- It is also important to maintain a healthy lifestyle in terms of nutrition and exercise.
Now let's talk about a special case of the disease: primary prolapse of the tricuspid (grade 1) and mitral valves.
Types of pathology
The initial stage of the disease is divided into two types - with regurgitation (blood reflux) and without it. Doctors distinguish the following degrees of pathology:
- Zero. The valves only bend, but do not diverge, so there is no return of blood.
- First. With prolapse of the anterior leaflet of the mitral valve of the 1st degree, a slight divergence of the valve flaps is observed, which causes the blood to turn back.
- Second. The blood that is thrown from the ventricle reaches half of the atrium.
- Third. The blood stream is very intense, it reaches the back wall of the upper chamber.
Special case: mitral and tricuspid valve prolapse
Mitral valve prolapse is often accompanied by tricuspid valve prolapse. With treatment and diagnosis, the situation is the same as in the classic case with one PTC. Valve abnormalities may not cause discomfort to the patient and may not affect hemodynamics at all, and therefore do not require treatment.
In this case, anomalies are also divided by degree. Treatment will depend on the degree.
A video report from a famous TV presenter will tell you more about mitral and tricuspid valve prolapse:
What it is?
Left valve prolapse, or mitral valve prolapse, or bicuspid valve prolapse (BVP) is a disease accompanied by dysfunction of the valve located between the left atrium and the ventricle.
Normally, when the atrium contracts, the valve opens and blood flows into the ventricle. The valve then closes and the ventricle contracts, releasing blood into the aorta. With some pathology of connective tissue or changes in the heart muscle, a disturbance in the structure of the mitral valve occurs, which leads to “bending” of its valves into the cavity of the left atrium during contraction of the left ventricle, and part of the blood flows back into the atrium. The severity of this pathology is judged by the magnitude of the reverse flow.
It is believed that this disorder is most often observed in young people, but data from the Framingham study showed that there is no significant difference in the incidence of this disease depending on gender and in different age groups. In the case of a small return of blood (regurgitation), it is not clinically felt and does not require treatment. In rare cases, the amount of reverse blood flow is large and correction of the defect is required, including surgical intervention.
Complications
The most common complications relate to the causes of PTC. Thus, with insufficient treatment, the patient may develop secondary infective endocarditis and worsen rheumatism. PTC can also lead to:
- Thromboembolism of the pulmonary artery, that is, blockage of the latter.
- Thrombosis of the prosthesis after surgical treatment.
- Atrioventricular block, characterized by circulatory disorders.
You need to understand that PTC itself leads to hemodynamic disturbances, which affects all organs and can lead to other complications.
Causes of acquired tricuspid regurgitation
Acquired tricuspid valve regurgitation is much more common than congenital regurgitation. It can be primary and secondary. The primary causes of this pathology include rheumatism, drug addiction, and carcinoid syndrome.
- Rheumatism is the most common cause of this pathology. In 20% of cases, it is recurrent rheumatic endocarditis that leads to deformation (thickening and shortening) of the valve leaflets, and the tendon threads also change in the same way. Very often this pathology is accompanied by stenosis of the right atrioventricular orifice. This combination is called combined tricuspid defect.
- Rupture of the papillary muscles can also lead to tricuspid regurgitation. Such ruptures occur during myocardial infarction or may have a traumatic origin.
- Carcinoid syndrome can also lead to this pathology. It occurs in certain types of cancer, for example, cancer of the small intestine, ovaries or lungs.
- Taking hard drugs very often leads to infective endocarditis, which, in turn, can cause tricuspid regurgitation.
The most common causes of secondary tricuspid insufficiency are the following diseases:
- dilation of the annulus fibrosus, which occurs with dilated cardiomyopathy;
- high degree of pulmonary hypertension;
- weakness of the right ventricular myocardium, which occurs in the so-called cor pulmonale;
- chronic heart failure;
- myocarditis;
- myocardial dystrophy.
Preparation for valve repair
The first step in patient preparation is diagnosis. To clarify the diagnosis, a chest ultrasound, ECG, blood and urine tests are prescribed. In some modern clinics, the heart is examined using a computed tomograph. Angiography of the heart vessels and or CT scans show the heart muscle and blood circulation in detail; during the studies, the radiologist can accurately determine tricuspid stenosis or insufficiency. After the tests, the patient undergoes a consultation with a cardiac surgeon, neurologist, and therapist.
If valve disorders are accompanied by additional heart problems, they try to get rid of them before surgery. For example, in case of arrhythmia, the heart rhythm is first normalized. If the clinical picture is complicated by heart failure, a sodium-excluding diet is prescribed. All patients are prescribed a diet a few days before the procedure; they need to avoid salt, too fatty foods, too spicy foods, and drink less water. You cannot eat 8 hours before plastic surgery. As part of the patient's preparation, the attending doctor explains to his patient how tricuspid valve repair is performed. It is important that the person being operated on does not worry and does not overload the heart and nervous system. If you have concerns or fears, you should talk to your doctor about it.