The structure of the walls of veins and their difference from arteries
- The inner wall is lined with epithelial cells
- Average MMC
- External RVST, fixed to surrounding tissues.
Veins have a thinner wall: they expand easily and collapse easily.
There are valves - folds of the inner membrane - distributed unequally: less in the arms than in the legs, the rest above the confluence of the venous tributaries. Designed to prevent reverse blood flow and prevent stagnation in venous inflows. If the valve is not developed, then varicose veins, if stagnation, then a blood clot, and possible damage to the vessel.
The peculiarity of the hemodynamic conditions of the veins is low pressure (15-20 mm Hg) and low blood flow rate, which causes a lower content of elastic fibers in these vessels.
The number of muscle elements in the wall of these vessels depends on whether the blood moves with or against gravity.
Veins of the muscleless type are found in the dura mater, bones, retina, placenta, and red bone marrow. The wall of muscleless veins is lined internally with endothelial cells on the basement membrane, followed by a layer of fibrous SDTK; there are no smooth muscle cells.
Veins of the muscular type with weakly expressed muscular elements are located in the upper half of the body - in the system of the superior vena cava. These veins are usually in a collapsed state. The tunica media contains a small number of myocytes.
Veins with highly developed muscular elements make up the vein system of the lower half of the body. A feature of these veins is well-defined valves and the presence of myocytes in all three membranes - in the outer and inner membrane in the longitudinal direction, in the middle - circular direction.
Interesting: Mysteries of the heart
[Total: 0 Average: 0/5]
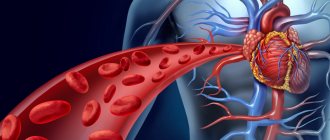
The heart (Latin cor, Greek cardia) is a hollow fibromuscular organ located in the middle of the chest between the two lungs and lying on the diaphragm. In relation to the midline of the body, the heart is located asymmetrically - about 2/3 to the left of it and about 1/3 to the right. The size of the average person's heart is approximately equal to the size of his fist, weighing on average 220-260 grams (up to 500 g).
How the heart works.
The heart pumps blood throughout the body, saturating cells with oxygen and nutrients. The heart can be considered a real crossroads of highways, a regulator of the “movement” of blood, since veins and arteries converge in it, and it continuously acts as a pump - in one contraction it pushes 60-75 ml of blood (up to 130 ml) into the vessels. The normal heart rate in a calm state for an ordinary person is 60-80 beats per minute, and in women the heart beats 6-8 beats per minute more often than in men. During heavy physical activity, the heart rate can accelerate to 200 or more beats per minute. During the day, the heart contracts about 100,000 times, pumping from 6000 to 7500 liters of blood or 30-37 full baths with a capacity of 200 liters.
The pulse is formed when blood is pushed from the left ventricle into the aorta and spreads in the form of a wave through the arteries at a speed of 11 m/s, that is, 40 km/h.
Heart cells are unusual in that they stop dividing even before a person grows up, writes Reuters. Doctors know that the heart contains stem cells that can develop into heart muscle cells. However, usually after serious failures, scar tissue forms on the heart, and the muscle never fully recovers. It has also recently been discovered that anger, anger and other strong emotions can negatively affect heart rate, causing death in people with poor health. Earthquakes, wars and even the loss of a national team in the World Cup can increase the number of deaths caused by sudden cardiac arrest...
With the development of scientific knowledge, European scientists accepted the view of the Italian naturalist Borell, who likened the functions of the heart to the work of a “soulless pump.” The anatomist Bernoulli in Russia and the French physician Poiseuille, in experiments with animal blood in glass tubes, derived the laws of hydrodynamics and therefore rightfully transferred their effect to blood circulation, thereby strengthening the idea of the heart as a hydraulic pump. And the physiologist I.II.Sechenov generally likened the work of the heart and blood vessels to the “sewage canals of St. Petersburg.” From then to the present, these utilitarian beliefs have been the basis of fundamental physiology: “The heart consists of two separate pumps: the right heart and the left heart. The right heart pumps blood through the lungs, and the left heart pumps blood through the peripheral organs.” The blood entering the ventricles is thoroughly mixed, and the heart, with simultaneous contractions, pushes out equal volumes of blood into the vascular branches of the greater and lesser circles. The quantitative distribution of blood depends on the diameter of the vessels supplying the organs and the action of the laws of hydrodynamics in them [2, 3]. This is how the currently generally accepted academic diagram of blood circulation is described.
Despite its seemingly obvious function, the heart remains the most unpredictable and vulnerable organ. This forced scientists in many countries to undertake additional heart research, the cost of which in the 1970s exceeded the cost of astronaut flights to the Moon. The heart was disassembled down to its molecules, however, no discoveries were made in it, and then cardiologists were forced to admit that the heart as a “mechanical device” can be reconstructed, replaced with a foreign or artificial one. The latest achievement in this area was the DeBakey-NASA pump, capable of rotating at a speed of 10 thousand revolutions per minute, “slightly destroying blood elements” [4], and the adoption by the English Parliament of permission to transplant pig hearts into people.
In the 1960s, Pope Pius XII gave an indulgence for these manipulations with the heart, declaring that “a heart transplant is not contrary to the will of God, the functions of the heart are purely mechanical.” And Pope Paul IV likened heart transplantation to an act of “micro-crucifixion.” Heart transplantation and its reconstruction became world sensations of the 20th century. They left in the shadows the facts of hemodynamics accumulated by physiologists over the centuries, which fundamentally contradicted generally accepted ideas about the work of the heart and, being misunderstood, were not included in any of the physiology textbooks. The French physician Riolan wrote to Harvey that “the heart, like a pump, is not capable of distributing blood of different composition into separate flows through the same vessel” [5]. Since then, the number of similar questions has continued to multiply. For example: the capacity of all human vessels has a volume of 25-30 liters, and the amount of blood in the body is only 5-6 liters [6]. How is a larger volume filled with a smaller one?
It is argued that the right and left ventricles of the heart, contracting synchronously, push out the same volume of blood. In fact, their rhythm [7] and the amount of blood ejected do not coincide [8] . During the phase of isometric tension in different places of the cavity of the left ventricle, pressure, temperature, and blood composition are always different [9], which should not be the case if the heart is a hydraulic pump in which the fluid is evenly mixed and has the same pressure at all points of its volume. At the moment the blood is pushed out by the left ventricle into the aorta, according to the laws of hydrodynamics, the pulse pressure in it should be greater than at the same moment in the peripheral artery, however, everything looks the other way around, and the blood flow is directed towards higher pressure [10]. For some reason, from any normally functioning heart, blood periodically does not flow into individual large arteries, and “empty systoles” are recorded on their rheograms, although according to the same hydrodynamics it should be distributed evenly throughout them [11]. The mechanisms of regional blood circulation are still unclear. Their essence is that, regardless of the general blood pressure in the body, its speed and quantity flowing through a separate vessel can suddenly increase or decrease tens of times, while in the neighboring organ the blood flow remains unchanged. For example: the amount of blood through one renal artery increases 14 times, and at the same second in another renal artery with the same diameter it does not change [12]. It is known in the clinic that in a state of collaptoid shock, when the patient’s total blood pressure drops to zero, in the carotid arteries it remains within normal limits - 120/70 mm Hg. Art. [13].
The behavior of venous blood flow looks especially strange from the point of view of the laws of hydrodynamics. The direction of its movement goes from low to higher pressure. This paradox has been known for hundreds of years and is called vis a tegro (movement against gravity) [14]. It is as follows: in a person standing at the level of the navel, an indifferent point is determined at which the blood pressure is equal to atmospheric pressure or slightly higher. Theoretically, blood should not rise above this point, since above it the vena cava contains up to 500 ml of blood, the pressure in which reaches 10 mm Hg. Art. [15]. According to the laws of hydraulics, this blood has no chance of getting into the heart, but the blood flow, not paying attention to our arithmetic difficulties, fills the right heart with the necessary amount every second.
It is not clear why in the capillaries of a resting muscle the blood flow speed changes by a factor of 5 or more in a few seconds, and this despite the fact that the capillaries cannot contract independently, they do not contain nerve endings, and the pressure in the supply arterioles remains stable [16]. The phenomenon of an increase in the amount of oxygen in the blood of venules after it flows through the capillaries, when almost no oxygen should remain in it, seems illogical [17]. And the selective selection of individual blood cells from one vessel and their targeted movement into certain branches seems completely implausible.
For example, old large red blood cells with a diameter of 16 to 20 microns from the total flow in the aorta are selectively turned only to the spleen [18], and young small red blood cells with a large amount of oxygen and glucose, and also warmer, are sent to the brain [19] . The blood plasma entering the fertilized uterus contains an order of magnitude more protein micelles than in neighboring arteries at this moment [20]. There is more hemoglobin and oxygen in the red blood cells of an intensively working hand than in a non-working hand [21].
These facts indicate that there is no mixing of blood elements in the body, but there is a targeted, dosed, targeted distribution of its cells into separate streams depending on the needs of each organ. If the heart is just a “soulless pump,” then how do all these paradoxical phenomena occur? Without knowing this, physiologists persistently recommend using the well-known mathematical equations of Bernoulli and Poiseuille [22] when calculating blood flow, although their use leads to an error of 1000%! Thus, the laws of hydrodynamics discovered in glass tubes with blood flowing in them turned out to be inadequate to all the complexity of the phenomenon in the cardiovascular system. However, in the absence of others, they still determine the physical parameters of hemodynamics. But what’s interesting: as soon as the heart is replaced with an artificial one, a donor one, or reconstructed, that is, when it is forcibly transferred to the clear rhythm of a mechanical robot, then the forces of these laws are carried out in the vascular system, but hemodynamic chaos sets in in the body, perverting the regional, selective blood flow, leading to multiple vascular thrombosis [23]. In the central nervous system, artificial circulation damages the brain, causes encephalopathy, depression of consciousness, changes in behavior, destroys intelligence, leads to seizures, visual impairment, and stroke [24]. It became obvious that the so-called paradoxes are actually the norm of our blood circulation.
Consequently, in us: there are some other, still unknown mechanisms at work, which create problems for the ingrained ideas about the foundation of physiology, at the basis of which, instead of a stone, there was a chimera... It seems that a certain mystifier, knowing the truth, deliberately hid these for centuries facts, purposefully leading humanity to realize the inevitability of replacing their hearts. Some physiologists tried to resist the onslaught of these misconceptions, proposing instead of the laws of hydrodynamics such hypotheses as “peripheral arterial heart” [25], “vascular tone” [26], the effect of arterial pulse oscillations on the venous return of blood [27], the centrifugal vortex pump [ 28], but none of them was able to explain the paradoxes of the listed phenomena and propose other mechanisms of heart function. We were forced to collect and systematize the contradictions in the physiology of blood circulation by a case in an experiment on modeling neurogenic myocardial infarction, since in it we also came across a paradoxical fact [29].
Unintentional injury to the femoral artery in a monkey caused an apical infarction. At her autopsy, it was discovered that a blood clot had formed inside the cavity of the left ventricle above the site of the infarction, and in the left femoral artery in front of the site of injury, six similar blood clots were sitting one after another. (When intracardiac blood clots enter the vessels, they are usually called emboli.) Pushed by the heart into the aorta, for some reason they all ended up only in this artery. There was nothing similar in other vessels. This is what caused the surprise. How did emboli, formed in a single section of the heart ventricle, find the site of injury among all the vascular branches of the aorta and hit the target?
When reproducing the conditions for the occurrence of such a heart attack in repeated experiments on different animals, as well as with experimental injuries to other arteries, a pattern was discovered that injured vessels of any organ or part of the body necessarily cause pathological changes only in certain places on the inner surface of the heart, and those formed on In them, blood clots always end up at the site of arterial injury. The projections of these areas on the heart in all animals turned out to be of the same type, but their sizes are not the same. For example, the inner surface of the apex of the left ventricle is associated with the vessels of the left hind limb, the area to the right and behind the apex with the vessels of the right hind limb. The middle part of the ventricles, including the septum of the heart, is occupied by projections associated with the vessels of the liver and kidneys; the surface of its posterior part corresponds to the vessels of the stomach and spleen. The surface located above the middle outer part of the cavity of the left ventricle is the projection of the vessels of the left forelimb; the anterior part with the transition to the interventricular septum is the projection of the lungs, and on the surface of the base of the heart there is a projection of the brain vessels, etc. Thus, a phenomenon was discovered in the body that has signs of conjugate hemodynamic connections between the vascular regions of organs or parts of the body and the specific projection of their places on the inner surface of the heart. It does not depend on the action of the nervous system, since it also manifests itself when nerve fibers are inactivated.
Further studies have shown that injuries to various branches of the coronary arteries also cause retaliatory lesions in associated peripheral organs and parts of the body. Consequently, there is a direct and inverse connection between the vessels of the heart and the vessels of all organs. If blood flow stops in some artery of one organ, hemorrhages will certainly appear in certain places in all other organs [30]. First of all, it will occur in a local place of the heart, and after a certain period of time it will certainly manifest itself in the associated area of the lungs, adrenal glands, thyroid gland, brain, etc. It turned out that our body is made of cells of some organs embedded in each other into the intima of the vessels of others.
These are representative cells, or differons, located along the vascular branches of organs in such an order that they create a pattern that, with enough imagination, can be mistaken for the configuration of the human body with greatly distorted proportions. Such projections in the brain are called homunculi [31]. In order not to invent new terminology for the heart, liver, kidneys, lungs and other organs, we will call them the same. Research has led us to the conclusion that, in addition to the cardiovascular, lymphatic and nervous systems, the body also has a terminal reflection system (RTS).
Comparison of immunofluorescence of representative cells of one organ with myocardial cells in the adjacent part of the heart showed their genetic similarity. In addition, in the portions of emboli connecting them, the blood turned out to have an identical glow. From which it could be concluded that each organ has its own set of blood, with the help of which it communicates with its genetic representations in the intima of the vessels of other parts of the body.
The question naturally arises, what kind of mechanism ensures this incredibly precise selection of individual blood cells and their targeted distribution among their representatives? His search led us to an unexpected discovery: the control of blood flows, their selection and direction to certain organs and parts of the body is performed by the heart itself. To do this, it has special devices on the inner surface of the ventricles - trabecular recesses (sinuses, cells), lined with a layer of shiny endocardium, under which there is specific muscle; through it, at their bottom, several mouths of Tebezium vessels, equipped with valves, emerge. Along the circumference of the cell there are circular muscles that can change the configuration of the entrance to it or completely block it. The listed anatomical and functional characteristics allow us to compare the work of trabecular cells to “mini-hearts”. In our experiments to identify conjugation projections, it was in them that blood clots were organized.
Portions of blood in mini-hearts are formed by the coronary arteries approaching them, in which blood flows with systolic contractions in thousandths of a second, at the moment of blocking the lumen of these arteries, are twisted into vortex-soliton packages, which serve as the basis (grains) for their further growth. In diastole, these soliton grains flow through the mouths of the Tebesia vessels into the cavity of the trabecular cell, where they wind streams of blood from the atria around themselves. Since each of these grains has its own volumetric electric charge and rotation speed, red blood cells, matching them in resonance of electromagnetic frequencies, rush towards them. As a result, soliton vortices of different quantity and quality of blood are formed1.
During the phase of isometric tension, the internal diameter of the left ventricular cavity increases by 1-1.5 cm. The negative pressure that arises at this moment sucks soliton vortices from the mini-hearts to the center of the ventricular cavity, where each of them occupies a specific place in the output spiral channels. At the moment of systolic ejection of blood into the aorta, the myocardium twists all the erythrocyte solitons located in its cavity into a single helical conglomerate. And since each of the solitons occupies a certain place in the outflow channels of the left ventricle, it receives its own power impulse and that helical trajectory of movement along the aorta, which direct it to the target - the associated organ. Let's call the way mini-hearts control blood flows “gemonics”. It can be likened to computer technology based on jet pneumohydrautomatics, which was once used in rocket flight control [32]. But hemonics is more perfect, since simultaneously with the jet interaction of flows it selects erythrocytes by solitons and gives each of them a targeted direction.
In one cube. mm of blood contains 5 million red blood cells, then per cubic meter. cm - 5 billion red blood cells. The volume of the left ventricle is 80 cubic meters. cm, which means it is filled with 400 billion red blood cells. In addition, each red blood cell carries at least 5 thousand units of information. Multiplying this amount of information by the number of red blood cells in the ventricle, we obtain that the heart processes 2 x 1015 units of information per second. But since the red blood cells that form solitons are located from each other at a distance from a millimeter to several centimeters, then, dividing this distance by the appropriate time, we obtain the speed of operations for the formation of solitons by intracardiac hemonics. It exceeds the speed of light! Therefore, the processes of cardiac hemonics have not yet been registered; they can only be calculated.
Thanks to these super speeds, the basis of our survival is created. The heart learns about ionizing, electromagnetic, gravitational, temperature radiation, changes in pressure and composition of the gaseous environment long before they are perceived by our sensations and consciousness and prepares homeostasis for this expected effect [33].
Thus, an experimental case helped reveal the action of a previously unknown terminal reflection system, which connects all genetically related tissues of the body with blood cells through mini-hearts and thereby provides the human genome with targeted and dosed information. Since all genetic structures are associated with the heart, it carries a reflection of the entire genome and keeps it under constant information tension. And in this most complex system there is no place for primitive medieval ideas about the heart. It would seem that the discoveries made give the right to liken the functions of the heart to a genome supercomputer, but events occur in the life of the heart that cannot be attributed to any scientific and technical achievements.
Forensic scientists and pathologists are well aware of the differences in human hearts after death. Some of them die overflowing with blood, like inflated balls, while others find themselves without blood. Histological studies show that when there is excess blood in a stopped heart, the brain and other organs die because they are drained of blood, and the heart retains the blood in itself, trying to preserve only its life. In the bodies of people who died with a dry heart, not only is all the blood given to diseased organs, but even particles of myocardial muscles are found in them, which the heart donated for their salvation, and this is already a sphere of morality and not a subject for the study of physiology.
The history of the knowledge of the heart convinces us of a strange pattern. In our chest beats the kind of heart we imagine: it is a soulless, a vortex, a soliton pump, a supercomputer, and the abode of the soul. The level of spirituality, intelligence and knowledge determines what kind of heart we would like to have: mechanical, plastic, pig, or our own - human. This is like the choice of Faith.
Sources of information: 1. Raff G. Secrets of physiology. M., 2001. P. 66. 2. Folkov B. Blood circulation. M., 1976. P.21. 3. Morman D. Physiology of the cardiovascular system. St. Petersburg, 2000. P. 16. 4. DeBakey M. New life of the heart. M, 1998. P.405. 5. Harvey V. Anatomical study of the movement of the heart and blood in animals. M., 1948. 6. Conradi G. In the book: Issues of regulation of regional blood circulation. L., 1969. C13. 7. Akimov Yu. Therapeutic archive. V. 2. 1961. P.58. 8. Nazalov I. Physiological Journal of the USSR. N> 11.1966. C.1S22. 9. Marshall R. Cardiac function in healthy and sick people. M., 1972. 10. Gutstain W. Atherosclerosis. 1970. 11. Shershnev V. Clinical rheography. M., 1976. 12. Shoameker W. Surg. Clin. Amer. No. 42. 1962. I3. Genetsinsky A. Course of normal physiology. M.. 1956. 14. Waldman V. Venous pressure. L., 1939. 15. Proceedings of the international symposium on the regulation of capacitive vessels. M., 1977. 16. Ivanov K. Fundamentals of the body’s energy. SPb., 2001.P.178; 17. Basics of the body’s energy. T. 3. St. Petersburg, 2001. P. 188. 18. Gunlhemth W. Amer. J. Physil No. 204. 1963. 19. Bernard S. Rech sur le grand sympathigue. 1854.
Functions of the venous system
Functions of veins:
- Transport of blood to the heart.
- Blood reservoir - deposition is facilitated by thin-walled, numerous veins (many in the abdominal cavity, they hold 80% of the blood in case of shock => GM, heart, liver, kidneys). In shock, blood pressure drops down to 0. The veins of the lungs can accumulate up to 28% of the blood, and swelling is possible due to inflammation.
- Regulates hemodynamics: blood flow speed, blood pressure provide blood supply, carried out reflexively. There are many receptors in the walls of the veins: chemo, mechano, baro. When they are irritated, reflexes are triggered:
- venovenous;
- venoarthrial (increased pressure, decreased arterial blood flow);
- venolymphatic.
- Participation in metabolic processes between blood and tissue. The walls of the capillaries are well permeable, metabolic processes are ensured by thin-walled venules, post-capillaries; with inflammation, permeability (swelling) increases, since the walls of the venules react to histamine.
Characteristics of venous blood
Venous blood is contained in the veins leaving organs, pulmonary arteries, and the right half of the heart. It removes carbon dioxide, metabolic products and toxins from tissues. In the alveoli of the lungs it turns into arterial.
The blood in the veins is darker, thicker, clots faster, flows slower, and is easier to stop; usually a tight bandage is enough. It is more suitable for laboratory research than finger capillary. If there is communication between arteries and veins, incomplete separation of blood occurs (heart defects, vascular disease, lung disease).
Venous blood: main indicators
Venous blood is that which flows from the internal organs, limbs, and brain through the veins . It is contained in the right atrium and pulmonary arteries. Functions: carries away carbon dioxide and metabolic products. Its color is darker, its viscosity and temperature are higher, its pressure and speed are lower than those of arterial blood.
Such properties, as well as the presence of microbial residues, toxins, immune complexes, and hormones, make it the main material for identifying diseases in laboratory diagnostics.
We recommend reading the article on coronary circulation. From it you will learn about the diagram of the coronary circle, physiology, regulation of the small coronary circle, and research methods.
And here is more information about hypoxemia and hypoxia.
What is it, its color, main characteristics and composition
Venous blood is that which flows from the organs to the heart, and from it enters the lungs. It takes in carbon dioxide and metabolic products. It is used for testing and medications are also injected into it through intravenous injections. There are differences in the main characteristics and composition between the blood in the arterial and venous beds; they are presented in the table.
| Removal of metabolic products and carbon dioxide | Nutrition and oxygen supply |
| Dark, cherry-burgundy, with a bluish tint |
It is important to note that the maximum difference between arterial and venous blood concerns gas composition, pressure and flow rate. All other physical and chemical properties differ only slightly.
Functions
Main functions of venous blood:
- removal of metabolic products (cleansing);
- transfer of absorbed nutrients from the intestine to the liver through the portal vein (transport);
- removal of excess hormones, salts (maintaining balance, equilibrium, homeostatic);
- delivery of carbon dioxide to the lungs for removal from the body (respiratory).
What is venous blood rich in?
Venous blood is rich in carbon dioxide; it also contains metabolic end products, toxins and microbial remains. Because of this, it is possible to identify the main diseases:
- infections;
- metabolic disorders (for example, atherosclerosis, diabetes mellitus);
- immune, allergic, autoimmune pathologies;
- blood diseases due to changes in the level of red blood cells, leukocytes, platelets;
- dehydration;
- risk of increased thrombus formation and blockage of veins and arteries;
- liver and kidney dysfunctions;
- hormonal disbalance.
Elements of the human circulatory system containing venous blood
Venous blood is contained in the following elements of the circulatory system:
- subcutaneous and deep venous vessels;
- venous networks of internal organs, brain;
- large vena cava (superior and inferior), carrying blood to the right atrium;
- the pulmonary artery emerging from the right ventricle and its branches in the lungs.
Artery through which venous blood flows
Venous blood flows through the pulmonary artery. This name is due to the fact that all the vessels leaving the heart are called arteries, and those coming to it are called veins. Therefore, in the veins of the lungs there is an arterial vein, rich in oxygen, and in the arterial network - carbon dioxide.
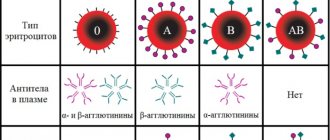
Which parts of the heart contain venous blood?
Venous blood is found in the right atrium and right ventricle of the heart. If there is a defect in the septum between the right and left parts, then a mixture of arterial and venous occurs.
Why are tests taken from a vein?
All metabolic products, hormones and toxins accumulate in the veins.
Therefore, by venous blood it is possible to determine diseases of internal organs and the brain, which are manifested by changes in the composition of cells or plasma (liquid part).
A puncture of a vein causes slight bleeding, which can be stopped very quickly by squeezing the vessel. If there is even slight damage to the artery, a tourniquet will be needed.
How to stop venous bleeding
In order to stop venous bleeding, you need:
- lift the limb up;
- Apply a pressure bandage to the site of damage to the vessel; if the bleeding is severe, then below the wound you should not apply too much pressure to the soft tissue with a tourniquet.
After providing first aid, the patient must be examined by a doctor.
You should not wash the wound yourself or remove traumatic objects from it or remove blood clots.
Arterial and venous blood
Differences between arterial and venous blood: dark blood flows from the veins, it is thicker, it clots faster, the bleeding is less intense, the stream is smooth and not strained. Venous blood is more suitable for laboratory tests than capillary blood from a finger. It flows through the pulmonary arteries, and in the capillaries of the alveoli it turns into arterial artery.
Which one is darker
Venous blood is darker. Its color depends on the form of hemoglobin. In the arterial blood, it is combined with oxygen (oxyhemoglobin), which gives it a bright scarlet color. The venous contains both oxyhemoglobin and 2 other forms:
- reduced (gave oxygen to cells, but has not yet added carbon dioxide);
- carboxyhemoglobin (a compound with carbon dioxide).
Most of the latter pigment, so the color becomes dark cherry.
Capillary and venous blood: differences
The main differences between capillary blood (from a finger) and venous blood are the contents:
- cells, especially platelets (higher in the venous), leukocytes (higher in the capillary);
- glucose (higher in the veins).
Analysis from a vein is considered more accurate, since it does not contain impurities of tissue fluid or surface epithelium of the skin. Also, circulatory disorders, vascular spasm, and fever can affect the indicators of capillary blood tests. For many types of laboratory diagnostics, a sufficient volume of material is needed, and up to 0.5 ml can be taken from a finger.
Therefore, capillary blood can be used only at the first stage of the examination. It will give reliable results only when determining hemoglobin, red blood cells and ESR. For biochemical and immunological analysis, studies of hormonal levels, as well as, if necessary, an in-depth study of cellular composition, blood from a vein is needed.
Why does venous blood clot faster?
Venous blood clots faster due to high platelet levels. These blood platelets form the basis of the clot, they are connected to each other, and fibrin threads give strength to the formed blood clots.
How to determine the type of bleeding
To determine the type of bleeding, you need to pay attention to the signs that distinguish them:
| Absent or thready pulse | |
| Pale with a bluish tint, cold | Normal color, some swelling, warm |
Through which veins does arterial blood flow?
Arterial blood flows through the veins that leave the lungs to the left atrium. Also, the entire internal venous network of the lungs is filled with hemoglobin, saturated with oxygen. Therefore, the contents in them are exactly the same in characteristics as in the arteries of all other organs (except the lungs).
Where venous blood turns into arterial blood
Venous blood is converted into arterial blood in the capillary network of the alveoli (vesicles) of the lungs. The pulmonary arteries branch into thin capillaries; they entwine the alveolar walls. Carbon dioxide enters the lumen of the pulmonary vesicle, and oxygen from it passes into the blood.
Oxygen molecules join the reduced hemoglobin, which has given up carbon dioxide, and it becomes oxyhemoglobin. Therefore, the blood changes its color and properties - from dark venous to light arterial. Through four pulmonary veins (two left and two right) it goes to the heart.
What kind of blood flows through the pulmonary veins
Arterial blood flows through the pulmonary veins, which is maximally saturated with oxygen. These vessels empty into the left atrium. When it contracts, the flow rushes into the left ventricle, and then into the aorta and through all the arteries of the systemic circle.
Incomplete separation of arterial and venous blood
Incomplete separation of arterial and venous blood occurs with heart defects and large vessels , as well as lung diseases:
- atrial septal defect;
- a hole in the septum between the ventricles;
- collapse of the walls (closing) of the alveoli of the lungs (atelectasis), filling with fluid (edema, pneumonia);
- fistula between a vein and an artery (congenital, less commonly acquired);
- transposition of the great vessels (aorta and pulmonary artery change places);
- underdevelopment of the heart chambers (two- and three-chamber);
- open arterial (ductus Botallus, connects the aorta and pulmonary artery).
Dark blood from a vein: what does it mean?
The dark color of blood from a vein means that the organ from which it flows is actively functioning. The higher the rate of metabolic processes, the more oxygen is absorbed from the blood, which means its color will be darker.
We recommend reading the article about venous congestion in the legs. From it you will learn about the causes and symptoms of the pathology, conservative and surgical treatment.
And here is more information about vascular injury.
Venous blood flows from the organs, collects in the large vena cava and then into the right half of the heart. Through the pulmonary arteries it approaches the alveoli and turns into the arterial artery.
The properties of blood from a vein are darker, thicker, and clot quickly. It is used for laboratory diagnostics, as it contains metabolic products, toxins, microbes, and hormones.
Venous bleeding is accompanied by a slow and uniform release of blood; it is easier to stop than arterial bleeding.
Watch the video about the circulatory system:
Source: https://CardioBook.ru/venoznaya-krov/
What connections between extra- and intracranial veins do you know? Their meaning
Extracranial: superficial, deep
Intracranial - GM veins, open in the sinuses of the dura mater, do not collapse, there are no valves. From the sinuses through the internal jugular vein is the main route for the outflow of venous blood from the cranial cavity.
Pathways of communication between intra- and extracranial veins:
- Through the venous outlet: 3 pairs, hole in the bones of the skull, blood from inside to outside
- The ophthalmic vein connects the cavernous sinus with the facial vein
- Through the diploe veins (the spongy substance of the skull bones between the plates)
- Through the foramen magnum into the vertebral venous plexuses
What is the difference between venous and arterial blood?
The vascular system maintains constancy in our body, or homeostasis. It helps him in the adaptation process, with its help we can withstand significant physical stress. Prominent scientists, since ancient times, have been interested in the structure and operation of this system.
If we imagine the circulatory apparatus as a closed system, then its main components will be two types of vessels: arteries and veins. Each performs a specific set of tasks and carries different types of blood. How venous blood differs from arterial blood will be discussed in the article.
Arterial blood
The task of this type is the delivery of oxygen and nutrients to organs and tissues. It flows from the heart and is rich in hemoglobin .
The color of arterial and venous blood is different. The color of arterial blood is bright red.
The largest vessel through which it moves is the aorta. It is characterized by high speed of movement.
If bleeding occurs, stopping it requires effort due to its pulsating nature under high pressure. The pH is higher than that of the venous one. On the vessels through which this type moves, doctors measure the pulse (on the carotid or radial).
Deoxygenated blood
Venous blood is that which flows back from the organs to return carbon dioxide . It contains no useful microelements and carries a very low concentration of O2.
But it is rich in metabolic end products and contains a lot of sugar. It is characterized by a higher temperature, hence the expression “warm blood.” It is used for laboratory diagnostic procedures.
Nurses administer all medications through veins.
Human venous blood, unlike arterial blood, has a dark, burgundy color. The pressure in the venous bed is low, the bleeding that develops when the veins are damaged is not intense, the blood oozes out slowly, and is usually stopped with a pressure bandage.
To prevent its reverse movement, the veins have special valves that prevent backward flow; the pH is low. There are more veins in the human body than arteries . They are located closer to the surface of the skin and are clearly visible visually in people with a light color type.
What is the normal platelet count in the blood?
Find out from this article how to deal with blood stagnation in the veins.
Once again about the differences
The table provides a comparative description of what arterial and venous blood is.
| Peculiarity | Arterial | Venous |
| Coloring | Bright red | Dark, burgundy |
| Acidity | High | Low |
| Travel speed | High | Low |
| Nutrients | A lot of | Few |
| Use for analysis | Rarely | Often |
| Bleeding intensity | Intense, pulsating in nature | Low intensity, slow |
Attention! The most common question is which blood is darker: venous or arterial? Remember - venous. It is important not to confuse this when you find yourself in an emergency situation. In case of arterial bleeding, the risk of losing a large volume in a short period of time is very high, there is a threat of death, and urgent measures must be taken.
Circulation circles
At the beginning of the article, it was noted that blood moves in the vascular system. From the school curriculum, most people know that movement is circular, and there are two main circles:
- Big (BKK).
- Small (MCC).
Mammals, including humans, have four chambers in the heart . And if you add up the length of all the vessels, you get a huge figure - 7 thousand square meters.
But it is precisely this area that allows you to supply the body with O2 in the required concentration and not cause hypoxia, that is, oxygen starvation.
BCC begins in the left ventricle, from which the aorta emerges. It is very powerful, with thick walls, with a strong muscle layer, and its diameter in an adult reaches three centimeters.
It ends in the right atrium, into which 2 vena cava flow. The ICC originates in the right ventricle from the pulmonary trunk, and closes in the left atrium with the pulmonary arteries.
Oxygen-rich arterial blood flows in a large circle and is directed to each organ . As they progress, the diameter of the vessels gradually decreases to very small capillaries, which give away everything useful. And back, through venules that gradually increase their diameter to large vessels, such as the superior and inferior vena cava, the depleted venous flows.
Once in the right atrium, through a special opening, it is pushed into the right ventricle, from which the small circle, pulmonary, begins . The blood reaches the alveoli, which enrich it with oxygen. Thus, venous blood becomes arterial!
Something very surprising happens: arterial blood moves not through the arteries, but through the pulmonary veins, which flow into the left atrium. Blood saturated with a new portion of oxygen enters the left ventricle and the circles are repeated again. Therefore, the statement that venous blood moves through the veins is incorrect; here everything works the other way around .
Fact! In 2006, a study was conducted on the functioning of the BCC and MCC in people with poor posture, namely scoliosis. Attracted 210 people under 38 years of age. It turned out that in the presence of scoliotic disease, there is a disruption in their work, especially among adolescents. In some cases, requiring surgical treatment.
In some pathological conditions, blood flow may be disrupted, namely:
Normally, mixing should not occur . During the newborn period, there are functional defects: open oval window, open Batalov duct.
After a certain period of time, they close on their own, do not require treatment and are not life-threatening.
But severe valve defects, reversal of the main vessels, or transposition, absence of a valve, weakness of the papillary muscles, absence of a heart chamber, combined defects are life-threatening conditions.
That is why it is important for the expectant mother to undergo screening ultrasound examinations of the fetus during pregnancy .
Conclusion
The functions of both types of blood, arterial and venous, are undeniably important. They maintain balance in the body and ensure its full functioning. And any violations contribute to a decrease in endurance and strength, and worsen the quality of life.
To maintain this balance, your body needs to be helped: eat right, drink plenty of clean water, exercise regularly and spend time in the fresh air.
Source: https://varikoznik.com/phlebos/chem-otlichaetsya-venoznaya-i-arterialnaya-krov.html
Around which organs are the periorgan venous plexuses more developed? Their meaning
In many places there are well-developed venous plexuses:
- Small pelvis,
- spinal canal,
- Around the bladder
The significance of these plexuses can be seen in the example of the intravertebral plexus. When filled with blood, it occupies those free spaces that are formed when cerebrospinal fluid is displaced when changing body position or during movements. Thus, the structure and location of the veins depends on the physiological conditions of blood flow in them.
What is the systemic and pulmonary circulation?
From the left ventricle, the contents are pushed out and enter the pulmonary artery, where they are saturated with oxygen. It is then distributed throughout the body through arteries and capillaries, carrying oxygen and nutrients.
The aorta is the largest artery, which is then divided into superior and inferior. Each of them supplies blood to the upper and lower parts of the body, respectively. Since the arterial system “flows around” absolutely all organs and is supplied to them with the help of a branched system of capillaries, this circle of blood circulation is called large. But the arterial volume is about 1/3 of the total.
Blood flows through the pulmonary circulation, which has given up all the oxygen and “taken away” metabolic products from the organs . It flows through the veins. The pressure in them is lower, the blood flows evenly. It returns through the veins to the heart, from where it is then pumped to the lungs.