Malformations or anatomical defects of cardiac structures develop in every ten thousand patient at some point in life.
Many conditions do not pose a major threat to health and are discovered accidentally during diagnosis for other diseases. The same applies to congenital defects, which account for up to 60% of all deviations from the norm.
A cardiac aneurysm is a protrusion of the wall of one of the chambers or anatomical structures. In 80% of recorded situations, the left ventricle or interventricular septum is affected.
The symptoms are nonspecific at first glance. You will not be able to distinguish one condition from another on your own. We need echocardiography and an ECG, at a minimum.
Sometimes the disorder is so well masked that an MRI is indispensable. On your own, you can only guess the nature of the problem. This is important because it gives reasons to see a doctor or call an ambulance.
Treatment is always surgical. But in the early stages or if there are indications, you can limit yourself to drug therapy (when - see below).
Nevertheless, doctors consciously recommend not to refuse surgery, if there are reasons for this.
Mechanism of development of the condition
It is based on a combination of two factors.
- The first is heart overload, an increase in blood pressure, and hence the impact on the myocardial wall.
- The second is degenerative changes in the tissues themselves as a result of existing cardiac pathologies. Basically, these are a previous heart attack, ischemic heart disease and chronic heart failure.
With the parallel influence of both moments, the thin wall cannot withstand it, bends outward and remains in this position.
Some of the blood stagnates in the aneurysm, a sac-like structure, and does not enter the large or small circle. This is fraught with significant hemodynamic impairment.
The pathology is cyclical, constantly progressing and will not stop until it leads to heart rupture and the death of the patient from massive bleeding - this is its main danger.
Types and symptoms of false aneurysm
A false aneurysm can occur as a result of injury, for example, after a puncture wound that hits a vessel. Pathology can also appear after surgery.
Experts distinguish three types of false (traumatic aneurysms);
- An aneurysm on an artery (“sacs” may be several in the case of a through wound).
- Arteriovenous aneurysms that occur in the event of a through lesion affecting an artery and vein. In this case, a connecting channel in the form of a vessel appears between them.
- Combined aneurysms. They may combine the characteristics of the first two types.
The arteriovenous connection must be eliminated as quickly as possible, since the increased direction of blood flow from the artery to the vein leads to disruptions in the functioning of the heart and can lead to myocardial hypertrophy and decompensation of cardiac activity.
For a false aneurysm to appear at the site of an artery injury, the lesion site must be small, and the wound area must be “wrapped” in soft tissue at the entrance and exit holes.
Traumatic aneurysms are characterized by the following symptoms:
- Swelling in the area of the aneurysm;
- Increased pulsation;
- Redness of the skin;
- Painful sensations of varying degrees at the location of the aneurysm.
Classification
This is done for a number of reasons.
| By etiology | By localization | By shape |
|
|
|
Classifications are used by doctors to determine the severity of the condition and develop treatment tactics.
Diagnostic methods
Signs that can be detected when examining a patient include:
- inspection and palpation - asynchronous pulsation in the 3rd - 4th intercostal space outside the apical impulse zone (yoke symptom);
- Auscultation – murmur during systole with relative mitral insufficiency;
- radiography - pathological protrusion of the left ventricular arch, expansion of the borders of the heart, pulmonary congestion;
- ECG – “frozen” symptoms of a heart attack, no improvement (ST recovery);
- EchoCG - an aneurysm is determined, its size, the presence of blood clots, as well as hemodynamic parameters - ejection fraction, final ventricular volumes in systole and diastole can be examined;
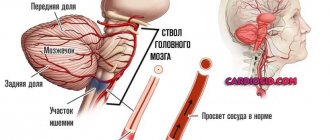
- coronary angiography – blockage of the coronary artery and changes in blood flow behind it;
- ventriculography and MRI - help to establish the size, shape, location, changes in the heart muscle outside the aneurysm, thrombosis of the ventricular cavity;
- PET of the heart (positron emission tomography) – needed to determine the “sleeping” myocardium in adjacent areas;
- EPI (electrophysiological study) is indicated in the presence of arrhythmia.
Causes and how to prevent the development of the disease?
Factors:
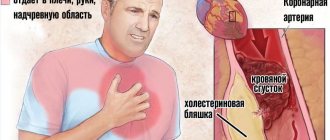
- Myocardial infarction. It accounts for 95% of all aneurysms. According to statistics, every tenth patient with a similar diagnosis in history “receives” an anatomical defect. Prevention - cessation of alcohol, smoking, diet, timely treatment of ischemic processes, atherosclerosis.
- Chest injuries. Bruises, fractures and others. The way to prevent it is to follow safety precautions.
- Exposure to ionizing radiation. Prevention - constant monitoring, taking cardioprotectors (Mildronat).
- Infections. From myocarditis to third-party conditions, up to syphilis and tuberculosis. Prevention: avoiding infection, at the beginning of the process - urgent treatment with antibiotics and taking protective medications.
Slightly less common are heart surgeries and congenital defects that can no longer be prevented.
How to make a diagnosis
Diagnosis is based on the doctor’s knowledge of the symptoms and course of an acute heart attack and its complications. In addition to characteristic manifestations, the doctor, when auscultating the heart, listens to typical rhinitis and murmurs.
The right contour of the heart shadow bulges
ECG signs are alarming when there is no dynamics of the infarction curve. This is important already at the stage of inpatient treatment of the patient.
X-ray examination shows an expansion of the shadow of the heart, a change in contours as the aneurysm bulges.
An X-ray kymogram allows you to track the movements of the parts of the heart along contour lines and reveals a stationary area.
Ultrasound of the heart notes changes in cavities, the formation of protrusion during contraction of the ventricles, and the formation of a parietal thrombus.
MRI allows you to more accurately display all the characteristics of the aneurysm site.
Symptoms
The clinical picture is extremely variable. Specific manifestations depend on the size of the formation, the initial cause of the pathological process, how long it has existed, and functional disorders.
Chest pain of moderate intensity
Pressing or burning, which directly indicates the ischemic nature of the condition associated with insufficient blood circulation. They are localized somewhere in the center or slightly to the left.
They manifest themselves during physical activity and stress. That is, after the intensification of cardiac activity and an increase in heart rate.
Discomfort develops as a result of insufficient blood circulation to the tissues around the wall protrusion.
As it progresses, oddly enough, the symptom disappears. An additional circulatory network develops. It compensates for ischemia.
Compression of tissue by an aneurysm also causes pain, as does excessive load on the entire muscular organ.
Increased heart rate
Heart rate reaches 120-180 beats per minute. This is the so-called tachycardia. An aneurysm leads to a spontaneous drop in hemodynamics (blood circulation).
The reason is that some of the blood remains in the formation and does not reach the large circle. This means that the tissues do not receive enough oxygen and nutrients.
The body intensifies cardiac activity to restore its own trophism (nutrition). At the initial stage, the patient feels a beating, then he gets used to it and stops noticing that something is wrong.
Non-productive cough
No phlegm. It develops as a result of compression of the lung, but more often as a result of insufficient gas exchange due to the meager release of blood into the pulmonary circle, and therefore poor saturation of the liquid connective tissue with oxygen.
Weakness
Drowsiness, asthenic manifestations, decreased ability to work and the ability to perform household duties.
These are typical symptoms of a left ventricular aneurysm, in which the intensity of cardiac output into the systemic circle decreases. It is through it that the brain, kidneys, liver, organs and tissues generally receive nutrition.
The aneurysm retains some of the blood, which means that the cerebral structures are also less well supplied. Hence the asthenic signs.
Dyspnea
A logical continuation of a cough. The result of lung compression or a drop in blood flow velocity in the pulmonary circle. Occurs during periods of physical activity.
If the aneurysm reaches a significant size, the symptom makes itself felt even at rest.
Arrhythmia
Abnormal heart rate. On the other hand, the intervals between each subsequent blow. Most often, the symptom is represented by tachycardia, an increase in heart rate to 120-180 beats. (as already said).
As it progresses, the opposite phenomenon is discovered. Bradycardia. It indicates weakness of cardiac activity, poor nutrition of the myocardium and inability to compensate for the disorder.
Ventricular or atrial fibrillation, that is, chaotic contractions of individual chambers, and extrasystole (extraordinary contractions) are also possible.
It is difficult to detect them on your own, but there are specific disturbances in well-being: a feeling of freezing in the chest, missing blows, turning over, etc.
Hyperhidrosis
Excessive sweating. At any time of the day, especially after minor physical activity. Caused by increased stress on the heart and poor muscle nutrition.
Edema of the lower extremities
At first, the process affects only the feet and ankles. Then the calves rise higher. On the one hand, this is the result of cardiac dysfunction, on the other, renal problems.
Advanced forms of aneurysm with the development of heart failure cause swelling of the face and hands.
Dizziness, pain in the back of the head, eyes
An indication of poor blood circulation in cerebral structures. Nervous tissues are demanding in terms of nutrition. Even a slight drop in trophism gives neurological symptoms.
Fainting and loss of consciousness
They act as a continuation, evolution of manifestations from the central nervous system. A syncopal episode most often occurs after excessive physical activity.
The heart is not able to provide the required amount of nutrition. Acute cerebral hypoxia ends in loss of consciousness. Then there is no connection with mechanical loads.
Thus, the symptoms of cardiac aneurysm have three planes:
- Actually cardiac. Arrhythmia, burning, impaired contractility.
- Neurogenic. Fainting, headache, vertigo.
- Respiratory. Shortness of breath, asphyxia when lying down, cough.
The first group develops immediately after the process reaches a certain critical mass. Until then, there are no manifestations at all or they are so meager that they have no meaning for the patient and do not pay attention to their own existence.
The third variety also occurs parallel to cardiac symptoms.
But neurogenic manifestations indicate an initially dangerous location of the aneurysm or rapid growth. Central nervous system disorders require urgent surgery.
Edema indicates renal and chronic heart failure. These are also negative prognostic points. Usually we are talking about an advanced version of the pathological process.
Causes of cardiac pathology
Cardiac aneurysm can be diagnosed even in newborns. Often children have to deal with a congenital type of disease that occurs due to inherited weakness of connective tissue. Pathology can also occur as the baby grows.
Other pathologies can provoke the disease, such as:
- atherosclerosis;
- hypertension;
- vasculitis
Teenagers who ignore a healthy lifestyle, prefer to smoke openly or secretly from their parents, with their own hands increase the risk of hypertension, atherosclerosis, and subsequently aneurysm.
Also, such a dangerous pathology often occurs in adolescents if the child has previously been in a traffic accident or received any injuries. Among adolescent patients, there are many who were previously fond of extreme sports.
In adults, this pathology is most often diagnosed after a heart attack. Patients whose hearts have been injured also have to deal with this disease. In this case, the muscle area dies, and the heart is no longer able to function normally. The heart can also be injured during surgery. In any case, if heart problems are determined, patients should be under the strict supervision of doctors. Only preventive examinations can prevent the further development of pathology and prevent the health condition from deteriorating.
The following diseases can also provoke an aneurysm:
- angina;
- tuberculosis;
- syphilis.
Abuse of alcoholic beverages and smoking is not only an addiction, but also a provocateur, a trigger, as a result of which such a dangerous disease as an aneurysm occurs.
Diagnostics: how to distinguish an aneurysm from other conditions on your own?
Without specialized research, it is impossible to say exactly what is the cause of the above symptoms. But there is a chance to guess. This is necessary for a timely response.
What is the distinction being made?
- Myocardial infarction. Actually acute coronary insufficiency, tissue necrosis. In contrast, the symptoms of an aneurysm increase gradually, not all at once.
The pain is not so severe, there is no loss of consciousness, no activity of the central nervous system. There is also no acute onset. Because the disorder is chronic and ongoing.
Read about the symptoms of a pre-heart attack in this article.
- Defects of the mitral, tricuspid, aortic valves. The difference is in the sequence of development of symptoms.
Against the background of an aneurysm, pain first appears, then rhythm disturbances. In this case, there may be no discomfort at all, or it may develop in the later stages of the pathological process.
- Angina pectoris. As in the case of a heart attack, a paroxysmal course is not typical for an aneurysm. The signs are approximately the same throughout the entire period of existence of the defect.
The progression follows a clear logic. The longer the disorder is present, the more pronounced the clinical picture.
- Cardiomyopathy. There is also virtually no pain. But there are dangerous arrhythmias and shortness of breath.
In this way, doctors assess the patient’s condition and build rough hypotheses. Specialist - cardiologist.
The list of studies is as follows:
- Oral interview and history taking. To build a model of the pathological process.
- Blood pressure measurement. Against the background of an aneurysm, it is consistently high at an early stage. Corresponds to symptomatic hypertension. Reduced after progression and development of persistent heart failure. 20-30 mm Hg less than the individual norm.
- Assessment of the frequency of organ contractions. The same. The main period gives tachycardia. Then - a decrease in heart rate. Which indicates a violation of contractility and an increase in tissue ischemia.
- Echocardiography (Dopplerography). The main technique at any stage. Provides a lot of information about the anatomical state of the heart and surrounding structures. It is an ultrasound method for visualizing tissue and measuring pressure in the chambers during systole (ejection) and diastole (relaxation).
- If necessary, MRI is prescribed. The study provides detailed images of the muscular organ.
- ECG. To assess the functional activity of the heart. All arrhythmias are visible immediately. Typically, the study is carried out after identifying the cause, to record the severity of the process.
Before the operation, scintigraphy is prescribed. It allows you to determine the safety of the functional activity of the myocardium, as well as the volume of blood that stagnates in the sac-like structure, and the permissible load during the upcoming anesthesia.
To identify the aneurysm itself, echocardiography is sufficient. Other methods are aimed at assessing the degree of disturbances that are caused by the disease. The examination is carried out on an outpatient basis.
Interesting:
The standard diagnosis of “chronic cardiac aneurysm” does not make sense, since the process is not acute. This is a terminological error that has developed in Russian medical practice.
How long do people live with post-infarction aneurysm without treatment?
The formation of a protrusion of the heart wall is an unfavorable variant of the course of myocardial infarction. If the operation is not performed in time, then within 2 - 3 years from the moment of aneurysm formation, patients die from acute coronary or cardiac decompensation, thrombosis. Factors that increase the likelihood of death include:
- progression of circulatory failure;
- resumption of angina attacks during treatment;
- relative mitral valve insufficiency due to dilation of the left ventricular cavity;
- severe types of rhythm disturbances;
- large size of the aneurysm, sac-like or mushroom-shaped.
A more benign course is observed in asymptomatic and small formations formed after 2 months from the onset of a heart attack.
Watch the video about an aneurysm and the danger it poses:
Treatment
Dual. At the initial stage or if the aneurysm does not grow, remains stable in size, and does not cause functional disorders (arrhythmias), conservative treatment and dynamic observation are indicated.
In case of expectant management, regular screening is prescribed for at least 3-5 years. Every 3-6 months a consultation with a cardiologist and a full diagnostic cycle (ECG, ECHO, 24-hour monitoring, MRI if indicated) are carried out.
An insignificant growth rate (less than 0.5 cm per six months) provides grounds for extending observation. Half a centimeter or more is an absolute indication for surgery. Here the doctor’s discretion no longer plays a role.
In preparation, the duration of the course of drug therapy is about 2-3 months. A week before the intervention, the last set of diagnostics takes place.
In both cases, the drugs are the same:
- Organic nitrates. Promote artificial expansion of the coronary arteries. Better nutrition of the myocardium due to normalization of hemodynamics. The classic remedy is Nitroglycerin. According to indications - others.
- Mild diuretics. Which conserve potassium and mania. For example, Veroshpiron or Spironolactone. Not constantly, 2-3 times a week. To relieve swelling and reduce stress on the heart.
- Antiplatelet agents and thrombolytics. They thin the blood, improve its fluidity, and prevent the development of clots. Aspirin-Cardio, Warfarin.
- Beta blockers. Anaprilin, Carvedilol. They normalize oxygen supply to the myocardium and simultaneously reduce blood pressure.
It is possible to use cardioprotectors, Mildronate and others. To improve metabolism in the heart.
Self-administration is strictly unacceptable. This is a direct path to aneurysm rupture, bleeding and death in a matter of seconds.
Treatment of cardiac aneurysm is predominantly surgical; surgery is required in 65-80% of cases.
Absolute indications for urgent treatment:
- Rupture of an aneurysm or ventricular wall/myocardial tissue.
- Thrombosis. Threat of stroke, heart attack or previous conditions of this kind.
- Detection of pathology in a child under 3 years of age.
- Risk of blood clots.
- Heart failure due to aneurysm.
- Rapid growth in education. More than 0.3-0.5 cm in six months.
- Arrhythmias resistant (unresponsive) to drug treatment.
In other cases, the question remains at the discretion of the cardiologist. If there is any doubt about competence, it is recommended to consult a second doctor. It definitely won’t be superfluous.
The essence of the intervention is to remove the formation and suturing the walls.
The operation is not necessarily performed using an open approach with a dissection of the chest. For relatively small aneurysms, endoscopic treatment is possible.
Afterwards, medications are prescribed:
- Antibiotics. To prevent infectious complications.
- Antiarrhythmic. To get your heart rate in order.
- Diuretics. Reduces the load on the heart.
- Beta blockers and nitrates according to indications.
Attention:
It is strictly forbidden to be treated with folk remedies. At best, they are useless and risk wasting precious time; at worst, they are dangerous and therefore threaten death.
During the rehabilitation period, recommendations are given on the way of future life.
- Quit smoking and alcohol (forever).
- Sexual rest (3-6 months).
- Diet correction. A minimum of fatty, fried, smoked foods, salt no more than 7 grams per day, no processed foods, fast food, canned food (all the time).
- Limitation of physical activity (from 6 months to lifelong change).
- Adequate rest is about 7-10 hours per night (always).
- Avoiding stress, mastering relaxation techniques.
Recovery lasts about six months.
Clinical manifestations of acute aneurysm
Diagnosis of the acute post-infarction form is difficult, since all the symptoms merge with signs of a severe heart attack, and the chronic form is erased by an increase in heart failure.
An aneurysm develops in the first days of a heart attack. The patient is in serious condition. I am concerned about intermittent pain in the heart area, weakness, possible rhythm disturbances, and dizziness.
If you place your palm on the heart area, then, in addition to the normal apical impulse in the fifth intercostal space, another additional pulsation is felt. It can be felt in those places where the apical impulse is not palpable: in the third or fourth intercostal space near the sternum.
Symptoms of a cardiac aneurysm appear in the first hours of a heart attack. An attentive physician will notice additional (precordial) pulsation in lateral lighting. If you place two fingers on the skin in the area of detected pulsation, then upon impact they will diverge. The symptom is called “spreading fingers.” It is observed in 74% of patients.
Prognosis and complications
Favorable in the early stages, in the absence of the need for surgery or if it is possible. Survival rate is close to 95%.
Mortality is higher when persistent arrhythmias or heart failure are associated. But even then the chances are good.
Cardiac aneurysms are dangerous due to the following consequences: the formation of wall thrombi, embolism, respiratory, renal, and heart failure. The result is always rupture of the formation, massive bleeding and death of the patient.
What is a cardiac aneurysm?
A cardiac aneurysm is a bulging, limited defect located in the heart wall.
A similar disease was first described back in 1757 by the outstanding English scientist D. Gunther. In more than 90% of cases, an aneurysm is detected after a myocardial infarction, but this is far from the only reason for its appearance. In 65% of cases, the formation is diagnosed in males. Most often it forms in the area of the left ventricle of the heart, which is accompanied by a sharp disruption in the functioning of the affected area. In rare cases, it forms in the right ventricle and interatrial septum. The size of a cardiac muscle aneurysm can reach 20 centimeters in diameter.
In cardiological practice, it is a fairly common phenomenon and a very pressing problem, since there is always a high risk of rupture of this formation, which is always accompanied by massive bleeding and a high chance of death.
What types are there? How does a true aneurysm differ from a false one?
Aneurysms can be classified according to various parameters, which allows choosing the necessary treatment tactics and making a prognosis for the patient’s life.
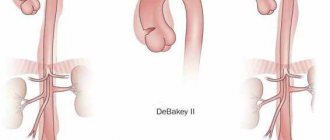
Post-infarction aneurysms are divided into:
- acute - form during the first two weeks after a heart attack, are prone to rupture and have a fairly poor prognosis. Some minor protrusions tend to resolve on their own as the connective tissue grows;
- subacute - formed in the third to eighth week, the risk of rupture is less, but blood clots may be present in the formation cavity. The original shape of the aneurysm may undergo changes;
- chronic , having a dense shell, rarely rupture, but complications such as rhythm disturbances and the formation of blood clots bother patients much more often. They develop eight weeks after myocardial infarction.
With each subsequent heart attack, the risk of developing a cardiac aneurysm increases greatly.
The division of aneurysms by size is quite arbitrary. There are:
- small - practically indistinguishable from the scar formed after a heart attack, most noticeable during heart contraction - systole;
- medium - the diameter can reach a couple of centimeters, the formations do not extend beyond the pericardium - the outer lining of the heart muscle;
- giant - capable of changing the shape of the heart, the diameter can approach the size of the left ventricle, and significantly affect the general well-being of the patient.
The larger the size of the heart aneurysm, the higher the risk of rupture.
The following types of protrusions are distinguished by shape (determined using ultrasound):
- saccular. A thin-walled formation with a wide base, with the greatest protrusion in the bottom area. Blood often stagnates in the cavity, resulting in the formation of blood clots;
- diffuse _ It has a small diameter, a massive base, is formed after extensive types of infarction, they rarely rupture;
- mushroom- shaped The shape is similar to an inverted jug with a narrow mouth, has thin walls and is small in size;
- "aneurysm within an aneurysm" . The most dangerous and life-threatening type, indicating a serious deformation of the structures of the heart muscle. It is a saccular and diffuse formation at the same time.
The most common type of aneurysm is diffuse, followed by saccular formations.
According to the structure of the aneurysm wall, they are divided into:
- muscular , consisting mainly of muscle components;
- fibrous - from connective tissue fibers;
- muscular-fibrous.
The likelihood of rupture depends on the thickness of the aneurysm wall, not on its composition.
There is also a true type of aneurysm , which contains in its structure the walls of the heart and a large number of connective tissue fibers.
It differs from a false one in that the latter is, in fact, a small rupture of the myocardium (muscular membrane), limited by the pericardium and fibrous adhesions, through which blood can flow into the resulting pathological cavity. In addition, there is a physiological type of cardiac aneurysm, the walls of which are formed due to the practically unchanged tissue of the muscular membrane, which has stopped contracting for any reason.
Clinic
The clinical picture of a cardiac aneurysm is not dominated by one symptom. It consists of a variety of manifestations observed in the patient in the period after a heart attack.
The patient notes:
- pain;
- shortness of breath;
- increased heart rate;
- altered heart rhythm;
- paleness of the skin;
- cough;
- increased fatigue.
The pain is localized behind the sternum (slightly to the left), occurs in the form of attacks, is not acute, and intensifies after exercise or smoking. Pain does not necessarily accompany the disease, since aneurysm tissue consists of connective cells that do not have nerve endings. Discomfort causes circulatory disturbances in the coronary vessels of any etiology.
As the disease progresses, the patient's symptoms of heart failure increase. Subsequently, the patient develops edema, the liver becomes enlarged, and there are signs of respiratory dysfunction (shortness of breath, suffocation). Changes in heart rhythm occur (tachycardia, bradycardia, arrhythmia). Angina pectoris is observed at exertion, as well as at rest.
The cause of weakness and malaise with a cardiac aneurysm is insufficient myocardial contraction. This dysfunction of the heart muscle leads to a decrease in the volume of circulating blood, a decrease in the transport of oxygen to the tissues, resulting in their hypoxia. For the same reason, pale skin and decreased sensitivity are observed. In addition, the patient notices swelling of the neck veins and increased sweating.
What can cause an aneurysm to rupture?
Factors that increase the risk of such a serious complication as heart rupture are:
- elderly and senile age;
- extensive penetrating infarction;
- severe arterial hypertension, especially during crises;
- heart attack due to new-onset angina pectoris;
- start of treatment a day after the attack;
- high patient activity, excessive physical or emotional stress;
- relapse of angina after a heart attack;
- exhaustion, concomitant diseases (diabetes, thyrotoxicosis, anemia);
- long-term treatment with hormones or non-steroidal anti-inflammatory drugs;
- administration of drugs to dissolve a blood clot after 10 hours from the onset of a heart attack.
Most often, rupture occurs 3–8 days from the onset of cardiac muscle necrosis and can be fatal.
Signs of the development of this condition include:
- pallor, then cyanosis of the skin;
- cold sweat;
- dilatation and bulging of veins in the neck;
- loss of consciousness;
- noisy breathing, wheezing, followed by rare breathing movements.
In most patients, heart rupture occurs instantly.