0
Author of the article: Marina Dmitrievna
2017.08.05
235
Red blood cells
Hemolysis of erythrocytes is the process of destruction of red blood cells with the release of hemoglobin into the bloodstream. Hemolysis can be both the cause of a failed test and a symptom of such a dangerous disease as anemia. Physiological hemolysis also exists. So let's try to understand the reasons for this phenomenon.
Lifespan of red blood cells in human blood
Red blood cells are the most abundant cells in the bloodstream and contain a special iron-based protein called hemoglobin, which is responsible for carrying oxygen molecules from the lungs to the rest of the body. These cells are produced at an incredible rate: 2 million per second. The average lifespan of red blood cells is 120 days.
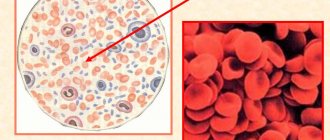
Where and how are they formed
The hormone erythropoietin and low oxygen levels regulate the production of red blood cells. Any factor that reduces oxygen levels in the body, such as lung disease or anemia (low number of red blood cells in the blood), increases erythropoietin levels. The hormone then stimulates the production of red blood cells, causing the stem cells to produce more red blood cells and increasing the rate at which they mature. The duration of the development process from bone marrow erythropoietic cells to mature red blood cells is 7 days.
Red cell formation
The common material of the hematopoietic system for the formed elements of blood are considered to be pluripotent undifferentiated cells, from which erythrocytes, leukocytes, lymphocytes and platelets are produced at various stages of synthesis.
When these cells divide, only a small portion remains as stem cells, which remain in the bone marrow, and the number of original mother cells naturally decreases with age.
Most of the resulting bodies differentiate, and new types of cells are formed. Red blood cells are produced inside the blood vessels of the red bone marrow.
Video:
The process of creating blood cells is regulated by vitamins and microelements (iron, copper, manganese, etc.). These substances accelerate the production and differentiation of blood components and participate in the synthesis of their components.
Hematopoiesis is also regulated by internal factors. The breakdown products of blood elements become a stimulator for the synthesis of new blood cells.
Erythropoietin plays the role of the main regulator of erythropoiesis. The hormone stimulates the formation of red blood cells from previous cells and increases the rate of release of reticulocytes from the bone marrow.
Erythropoietin is produced in the adult body by the kidneys, and a small amount is produced by the liver. The increase in red blood cell volume is explained by a lack of oxygen in the body. The kidneys and liver more actively produce the hormone in case of oxygen starvation.
The average lifespan of red blood cells is 100 – 120 days. In the human body, the depot of red blood cells is constantly renewed, which is replenished at a rate of up to 2.3 million per second.
The process of red blood cell differentiation is strictly monitored to maintain a constant number of circulating red cells.
READ Increase or decrease in red blood cell distribution index - what does it mean?
The key factor influencing the time and rate of red blood cell production is the concentration of oxygen in the blood.
The red blood cell differentiation system is highly sensitive to changes in oxygen levels in the body.
How long do they live?
Understanding what red cells are, how long human red blood cells live in the blood, and how they die, makes it possible to monitor your health and correct it in a timely manner.
The production of red blood cells in the bone marrow occurs at a staggering rate of more than 2 million cells per second. For the production of red blood cells to occur, the “raw materials” must be present in sufficient quantities. “Raw materials” include the same nutrients needed for the production and maintenance of any cell, such as glucose, lipids, and amino acids. However, the production of red blood cells also requires several micronutrients:
- Iron. Each heme group in a hemoglobin molecule contains an iron ion. Heme iron from animal foods is absorbed more efficiently than non-heme iron from plant foods. The bone marrow, liver and spleen accumulate iron in protein compounds - ferritin and hemosiderin. When erythropoietin stimulates red blood cell production, iron is released from storage, bound to transferrin, and transported to the bone marrow, where it attaches to red blood cell precursor cells.
- Copper is a component of 2 plasma proteins, hepestin and ceruloplasmin. Without them, hemoglobin cannot be adequately produced. Hephaestin, located in the intestinal villi, ensures the absorption of iron by intestinal cells. Ceruloplasmin transports copper. Both allow the oxidation of iron from Fe 2+ to Fe 3+, a form in which it can be bound to its transport protein transferrin for movement into the body's cells. With copper deficiency, iron transport for heme synthesis is reduced and iron begins to accumulate in tissues, leading to organ damage.
- Zinc functions as a coenzyme that facilitates the synthesis of the heme portion of hemoglobin.
- B vitamins: Folic acid and vitamin B12 function as coenzymes that facilitate DNA synthesis. Thus, both are critical for the synthesis of new cells, including red blood cells.
Unlike many other cells, red blood cells do not have a nucleus and can easily change shape, which helps them pass through different blood vessels in the body. Although the absence of a nucleus makes the red blood cell more flexible, it also limits the life of the cell as it passes through the smallest blood vessels, damaging the membrane and depleting energy reserves. The average lifespan of an erythrocyte is 115-120 days.
Pathogenesis
The mechanism of destruction can be of several types:
- natural - not caused by any pathology, but simply the result of the life cycle of red blood cells in the blood;
- osmotic - due to the presence in the blood of substances that have a destructive effect on the CCT shell;
- thermal - when exposed to extremely low temperatures;
- biological - caused by exposure to pathogenic microorganisms as a result of viral or infectious systemic diseases;
- mechanical - due to an impact that leads to damage to the erythrocyte membrane.
Why are red blood cells destroyed? As a result of the completion of the life cycle or under the influence of certain etiological factors, the following occurs:
- The CCT grows in size, the shape changes - from a disc-shaped erythrocyte to a round one;
- the shell of the CCP is not able to stretch, which leads to rupture of the CCP;
- the contents of the red blood cell enter the blood plasma.
There are many reasons for the process. Even severe stress can provoke hemolysis of an unnatural type.
Where and how do they die?
Worn-out red blood cell cells are removed by myeloid phagocytic cells called macrophages, located primarily in the bone marrow, liver, and spleen. Part of the hemoglobin of destroyed red blood cells is additionally processed as follows:
- Globin, the protein portion of hemoglobin, is broken down into amino acids that can be sent back to the bone marrow to produce new red cells. Hemoglobin that is not phagocytosed is broken down in the bloodstream, releasing alpha and beta chains, which are cleared from the bloodstream by the kidneys.
- The iron contained in the heme portion of hemoglobin may be stored in the liver or spleen, primarily in the form of ferritin or hemosiderin, or transported through the bloodstream via transferrin to the red bone marrow for recycling into new red blood cells.
- Non-iron heme is broken down into biliverdin and then into bilirubin. Bilirubin binds to albumin and travels through the blood to the liver, which uses it to produce bile. In the colon, bacteria break down bilirubin and convert it into urobilinogen and then stercobilin. It is then excreted from the body in feces. Broad-spectrum antibiotics kill these bacteria and may change the color of the stool. The kidneys also remove any circulating bilirubin and other associated metabolic byproducts, such as urobilins, and excrete them into the urine.
Thus, red blood cells are formed in the red bone marrow and sent into the blood circulation. At the end of their life cycle, they are destroyed by macrophages, and their components are recycled.
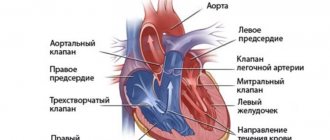
Physiology of blood
The single circulatory system in the human body is formed by blood and organs involved in the production and destruction of blood cells.
The main purpose of blood is transportation, maintaining the water balance of tissues (adjusting the ratio of salt and protein, ensuring the permeability of the walls of blood vessels), protection (supporting human immunity).
The ability to clot is the most important property of blood, necessary to prevent heavy blood loss in the event of damage to body tissues.
The total blood volume in an adult depends on body weight and is approximately 1/13 (8%), that is, up to 6 liters.
In a child’s body, the blood volume is relatively larger: in children under one year old – up to 15%, after one year – up to 11% of body weight.
The total volume of blood is maintained at a constant level, while not all of the available blood moves through the blood vessels, some part is stored in blood depots - the liver, spleen, lungs, and skin vessels.
The role and properties of red blood cells
Erythrocytes are red blood cells that perform a transport function. Thanks to the hemoglobin they contain (up to 95% of the cell mass), blood bodies deliver oxygen from the lungs to the tissues and carbon dioxide in the opposite direction.
Although the cell diameter is from 7 to 8 microns, they easily pass through capillaries whose diameter is less than 3 microns due to the ability to deform their cytoskeleton.
Red blood cells perform several functions: nutritional, enzymatic, respiratory and protective.
Red cells carry amino acids from the digestive organs to the cells, transport enzymes, carry out gas exchange between the lungs and tissues, bind toxins and help remove them from the body.
The total volume of red cells in the blood is enormous; red blood cells are the most numerous type of blood element.
When conducting a general blood test in the laboratory, the concentration of bodies in a small volume of material is calculated - 1 mm3.
Acceptable values of red blood cells in the blood vary for different patients and depend on their age, gender and even place of residence.
Types of hemolysis
Cellular breakdown is classified depending on what led to it:
- Hemolysis osmotic
- Hemolysis from chemical factors
- Hemolysis from biological factors
- Physico-mechanical
- Hemolysis from temperature
Let's look at each type in more detail.
- Osmotic hemolysis. Occurs in hypotonic solutions. This is a solution whose osmotic pressure is lower than the osmotic pressure of blood plasma. Under the influence of physical forces, water from the environment enters the erythrocyte, where the concentration of dissolved substances is much higher. The cells swell, increasing in size, the membrane stretches and collapses, bursting. The solution that contained blood becomes transparent and becomes bright red, scarlet in color (the so-called varnish blood). Osmotic hemolysis occurs already in solutions of sodium chloride at a concentration of 0.45-0.47%, and at a concentration of 0.32-0.31% all red blood cells undergo decay.
In some pathologies, the process can occur even with high salt contents.
- Chemical hemolysis. The breakdown of the erythrocyte membrane is caused by chemicals such as acids, alkalis, various toxins and poisons, heavy metals, ethers, benzene, and even some medications: quinine (used in the treatment of malaria), antipyrine. All of them lead to an increase in the content of free hemoglobin in the blood (hemoglobinemia) and its appearance in the urine (hemoglobinuria).
- Biological hemolysis. Cell destruction can occur due to incompatible blood transfusions or excessive physical exertion.
- Mechanical hemolysis. Occurs when there is a strong physical impact on the membranes of blood cells, for example, when shaking a test tube, or when passing blood through hemodialysis machines.
Sharp cold or, conversely, too high a temperature also leads to a hemolytic reaction.
Hemolysis is classified according to the location of the process:
- intravascular (flowing in the bloodstream)
Intravascular type of hemolysis
- intracellular (occurs in the liver, spleen, bone marrow).
Intracellular type of hemolysis
- hemolysis in vitro
- Intravascular form. Characteristic of such pathologies as: hemolytic anemia, cold agglutinin disease, the action of hemolytic toxins. This condition is diagnosed by testing for acidity and sucrose, determining the content of free hemoglobin in plasma. Specific symptoms may include muscle pain, fever, and high temperature.
- Intracellular form. When red blood cells are utilized in the above organs, the released hemoglobin combines with a substance called haptoglobin, then the complex is oxidized, divalent iron leaves it, hemoglobin is destroyed, all this leads to the formation of the final product of hemoglobin metabolism - bilirubin. This type is accompanied by high hemoglobinemia and hemoglobinuria. The main clinical signs of intracellular hemolysis are yellow color of the skin and mucous membranes, increased size of the liver and spleen. This pathology is most often caused by genetic factors.
- Hemolysis of red blood cells in vitro or in vitro is non-pathological among other types. Decay can also occur during a clinical blood test in the laboratory. Incorrect sampling technique, non-sterile containers for storage and analysis, violation of storage conditions, exposure to temperature factors - these reasons can lead to hemolysis of red blood cells in the collected blood. Even if you shake the test tube vigorously, you can damage the cell membranes, as mentioned above. In this case, the results of the study are naturally distorted and it is necessary to re-sample.
Lifespan of red blood cells: average life expectancy in a healthy body
Red blood cells are the main and most numerous blood cells. These little helpers perform many important functions. The most important and vital thing is the delivery of oxygen from the lungs to the organs. Blood is the universal internal environment of the body. It is present throughout the body and its changes lead to disruption of vital processes.
Physiology and functions of blood
Blood consists of plasma and formed elements. They originate outside the hematopoietic organs, after full maturation these cells enter the blood and perform their main functions, after approximately 90 days the red blood cells begin to age and then are destroyed outside these organs. Most of the blood in the body is constantly moving.
The amount of blood is from 4 to 6 liters. At birth, the baby has much more blood (14% of body weight). Maintaining volume is a vital criterion for the human body.
With the loss of 1/3 of all blood, a person may not survive, and with the loss of 1/2 of all blood, inevitable death occurs.
- Transport function - blood carries oxygen, acids and vitamins throughout the body.
- Protective (immunity).
- Stopping bleeding (hemostasis).
Hemoglobin gives blood its red color.
Blood density is 1.05-1.06, osmotic pressure is 7.6 atmospheres. Despite its small value, osmotic pressure plays a very important role; it keeps water inside the vessels. If this pressure does not cope with its functions, the human organs begin to swell. The kidneys are mainly responsible for this pressure.
Prevention of sickle cell anemia
Vitamin therapy and physiotherapy provide additional protection, especially if work or living are associated with harmful conditions. With the slightest characteristic symptoms and an unknown reason why hemolysis occurred, it is important to bring the body back to normal as quickly as possible.
The condition of pathological hemolysis is dangerous to human health and requires emergency medical care with monitoring of the patient throughout the entire period of treatment. Its peculiarity is that in the initial stages the disease has almost no symptoms, but in the latter stages it progresses too quickly. To prevent this condition, it is recommended to follow preventive measures, and when planning a pregnancy, families must consult with a specialist about the formation of the Rh factor in the child and its compatibility with the mother’s blood.
- prevent infectious or inflammatory diseases;
- Healthy food;
- exclude poisoning from heavy poisons, metals and other toxic substances;
- systematically undergo a medical examination.
If you feel unwell, you should consult a doctor, and not carry out therapeutic measures at your own discretion.
Tags: collapse, human, red blood cell
About the author: admin4ik
« Previous entry
The role and properties of red blood cells
An erythrocyte (translated from Greek as red cell) is a component of blood that does not have a nucleus and contains hemoglobin. Red blood cells are shaped like a biconcave disc. They do not have a core, so they are very elastic and pass into capillaries, which are much smaller than themselves.
These cells begin their lives in the red bone marrow and end in the liver and spleen. They live for about 120 days. At the stage of development of red blood cells, they have a nucleus; as they mature, it is converted into hemoglobin, which makes up 90% of the dry matter of red blood cells.
- respiratory;
- enzymatic;
- protective;
- buffer;
- nutritious.
Hemoglobin is the main element of red blood cells, it also has its own set of functions:
- Respiratory - it is hemoglobin that carries oxygen from the lungs to the organs and back carbon dioxide.
- Regulates blood reaction.
According to its chemical structure, hemoglobin is a protein that has a complex composition and includes the globin protein and the heme prosthetic group. It contains iron, which is responsible for the attachment and detachment of oxygen molecules.
The normal level of hemoglobin in human blood is considered to be 166.7 g/l.
For men, this norm is higher than for women, since male sex hormones have a stimulating effect on red blood cells and hemoglobin, while women’s hormones, on the contrary, inhibit this process.
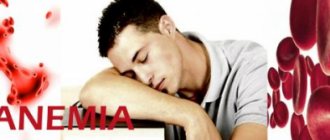
With a decrease in hemoglobin in the blood, anemia develops. This is very dangerous for the human body. Therefore, it is important to monitor the number of red blood cells and hemoglobin (undergo examinations, take tests).
The process of destruction and features of the life activity of an erythrocyte
The main components of blood, red blood cells, live in the body for no more than 120 days, and on average 60 days. Then they begin to age. Old red blood cells (damaged and deformed) lose their flexibility and end their life cycle in the blood vessels. After being cleaved from hemoglobin, the heme it contains becomes the yellow pigment bilirubin.
Carrying out analysis
A blood test is taken from a finger or a vein. Venous blood gives a much larger, faster and more accurate result, so taking such an analysis from a finger is not advisable. It is better to take this test on an empty stomach. If this is not possible, then it is not advisable to eat for at least four hours before the test. It is also advisable to eliminate emotional and physical stress the day before the test. If you need to take tests several times for diagnosis, then this must be done at the same time, with the same preparation and in the same hospital.
How the procedure goes:
- The analysis at the clinic is taken by a laboratory assistant using a syringe.
- The patient's blood is transfused into a special flask, which must be signed.
- After blood is collected, the resulting material is placed in a special device - an analyzer; this device itself separates and counts the number of each type of cell.
If any abnormalities are detected, a laboratory employee examines the blood using a microscope and notes his observations. The results of the analysis can be found out within a week. This depends on the work schedule of the laboratory where the analysis was taken. Today, many clinics do not have modern analyzers, and in such clinics, red blood cell counting is carried out by laboratory assistants using a microscope. The laboratory worker enters the research results into the analysis form; only a specialist can decipher and make a diagnosis. The form indicates the patient’s indicators and normal indicators.
Using this analysis, not only anemia, but also erythrocytosis can be detected. This means an increased number of red blood cells. This disease may be a consequence of prolonged dehydration. Externally, this disease can manifest itself as redness and itching of the skin, and unbearable pain in the head.
When red blood cell counts are low, a diagnosis of anemia is made, and this can also occur due to high water content in the body. Symptoms of this disease may include tinnitus, pale mucous membranes and discolored skin, a slight increase in temperature, and weakness.
Anemia is a low level of hemoglobin in the blood. This is not an independent disease, but a secondary one.
Anemia is always a symptom of an underlying disease. Around the world, about two billion people live with this disease. Life expectancy of red blood cells in animals. In different animal species, the life process of red blood cells takes different amounts of time. For example, in horses they live and function for about 100 days, and in rabbits no more than 60 days.
Determining the number, size and shape of red blood cells in human blood is of great diagnostic importance. This study helps to identify a number of asymptomatic pathological processes in the body (anemia, diseases of the hematopoietic system). Allows you to clarify the nature and stage of a previously diagnosed disease and effectively treat it. In fact, problems with red blood cells should be resolved promptly. Therefore, you should never neglect blood tests, because timely detection of the disease will help achieve better results in treatment.
Sickle cell anemia. Causes, symptoms, diagnosis and treatment of pathology
General blood analysis
Most modern laboratories are equipped with hematological analyzers - devices that allow you to quickly and accurately determine the quantitative composition of all cellular elements, as well as many other blood parameters.
General blood analysis
4.0 – 5.0 x/l.
3.5 – 4.7 x/l.
General blood analysis
4.0 – 5.0 x/l.
3.5 – 4.7 x/l.
- Decreased amount of urine.
- Pale skin, weakness and other symptoms of anemia, especially when they intensify.
- Urine color is brown or red (tea-colored).
The doctor begins the examination after asking the following questions:
- When and what exactly were the symptoms of hemolysis noticed.
- Whether the patient has previously had hemolytic anemia or G6PD deficiency.
- Whether the person has any relatives with a history of hemoglobin abnormality.
Testing to identify the disease will require:
- General and chemical blood test.
- Coombs test (determines incomplete erythrocyte antibodies to the Rh factor for testing Rh incompatibility between maternal and fetal blood).
- CT or ultrasound of the abdomen or kidneys.
Average lifespan of red blood cells
Life span of red blood cells Red blood cells have a limited life span: in humans it is 120 days. They must then be removed from the circulatory system to prevent their accumulation in the vessels. Dead red blood cells are removed from the bloodstream by macrophages in the spleen, bone marrow and liver. Such systematic removal of red blood cells could lead to their disappearance if new red blood cells did not enter the blood at the same rate. Anemia occurs only as a result of an uncompensated increase in the rate of removal of red blood cells from the blood or a decrease in the rate of their formation and entry into the blood. In other words, some forms of anemia arise mainly due to increased destruction of red blood cells or their loss from the body, not accompanied by an increase in their formation, while others are due to a decrease in their formation. The results of a reticulocyte count help determine the cause of anemia - whether it is associated with increased destruction of red blood cells or insufficient formation of them.
Reticulocyte count In a normal blood smear stained with a common dye, almost all red blood cells are light pink. Only 1-2% of them have a bluish tint. Such red blood cells are called polychrome. Let's consider what causes this shade.
The nuclear precursor of red blood cells is a large cell called an erythroblast. This cell produces hemoglobin, which is found later in mature red blood cells. Hemoglobin synthesis in erythroblasts is carried out by numerous polyribosomes, which makes their cytoplasm basophilic. During the formation of erythrocytes, erythroblasts divide several times, and polyribosomes are distributed so that very few of them remain in immature erythrocytes, as a result of which only traces of basophilia remain in the cytoplasm.
Polychrome red blood cells are difficult to identify in smears stained with conventional dyes. It is much better to use supravital staining with bright cresyl blue for this purpose. The dye is mixed with a fresh drop of blood, a smear is prepared from it, which is then stained with regular dye. The bright cresyl blue interacts somehow with the rRNA so that network-like bluish structures are formed. If there is little rRNA, then only a few scattered spots are visible (color photograph
Causes and symptoms
- There is a feeling of nausea, which often ends in vomiting.
- Painful sensations in the abdomen.
- Change in skin color.
If a complicated form appears, the patient may experience convulsions, severe malaise, paleness, and shortness of breath. Test results show anemia. The objective feature of this condition is characterized by the appearance of heart murmurs. At the same time, one of the most obvious signs of destruction of red blood cells are enlarged organs (for example, the spleen).
Note! If an intravascular type of hemolysis occurs, then an additional sign will be a change in urine color.
Human red blood cells, unlike animals, do not have a nucleus, but before losing it, they must go from the erythroblast cell, where hemoglobin synthesis begins, to reach the last nuclear stage - the normoblast, which accumulates hemoglobin, and turn into a mature nuclear-free cell, the main component of which is red blood pigment.
What people have not done with red blood cells, studying their properties: they tried to wrap them around the globe (4 times), and put them in coin columns (52 thousand kilometers), and compare the area of red blood cells with the surface area of the human body (red blood cells exceeded all expectations , their area turned out to be 1.5 thousand times higher).
- The entry of heavy metal compounds into the blood.
- Poisoning with arsenic or acetic acid.
- Old infectious diseases.
- Acute sepsis.
- DIC syndrome.
- Burns of a chemical or thermal nature.
- Mixing blood that does not match the Rh factor.
An experienced specialist must know not only the reasons why hemolysis of red blood cells develops, but also the characteristic signs, since in the first stages the pathology is asymptomatic and appears only during the acute stage, which develops quickly. Clinically this manifests itself in the following:
- Nausea, vomiting.
- Stomach ache.
- Change in skin color.
In a severe form of hemolysis, a person experiences convulsions, consciousness is depressed, and anemia is always present, externally manifesting itself in the form of malaise, pale skin and shortness of breath. An objective feature is listening to a systolic murmur in the heart. Both forms of hemolysis are characterized by an enlargement of the spleen and liver. Intravascular destruction of red blood cells changes the color of urine.