What is heart disease
To understand what a heart defect is, you need to understand the basic anatomy of this organ and the principles of its operation.
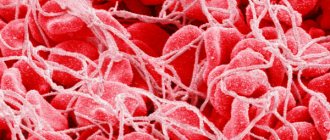
The human heart consists of 4 chambers - 2 atria and 2 ventricles. Blood moves from one chamber to another through openings that have valves. From the left ventricle, blood is released into the systemic circulation (aorta), saturates all organs and tissues of our body with oxygen, and returns to the left atrium through the vena cava. From there it goes to the right ventricle, then to the pulmonary artery in order to be enriched with oxygen in the lungs, and through the pulmonary veins returns to the right atrium, then to the left ventricle. Then the cycle repeats.
To prevent mixing of arterial and venous blood inside the heart, the left and right sections are separated by partitions - interatrial and interventricular. To prevent blood from flowing back (from the ventricles to the atria or from the aorta to the left ventricle), there are valves that open and close at certain times.
All heart defects are divided into 2 types - congenital and acquired.
As the name implies, congenital defects appear in a person from his very birth, and acquired defects arise in the course of later life.
The incidence of congenital heart defects (CHD) is approximately 5-8 cases per 1000 children. Acquired heart defects (AHD) occur in 100-150 people per 100,000 population.
To make it easier to understand the differences between CHD and PPS, I note that with the former, an anomaly develops, deformation of the main vessels (aorta and pulmonary trunk) or a septal defect, and with acquired ones, the valves are affected. But such a division can be considered conditional, since the valves can be damaged even with congenital defects.
All this leads to disruption of hemodynamics (normal blood flow) inside the heart, predominance of blood supply to some chambers and depletion of others. As a result, arterial blood mixes with venous blood, certain chambers become filled with blood, stretch, and their walls thicken. The filling of other parts of the heart, on the contrary, decreases compared to normal.
Most people with heart disease receive a disability rating. They cannot live a full life, like all healthy people, they need to constantly observe some restrictions. Even purely psychologically it is difficult.
On the issue of the army - people with heart defects are classified as “unfit” or “limitedly fit” for military service.
Is it possible to die from pathology?
Unfortunately, death from heart disease is quite possible. The statistics of deaths from congenital heart disease are quite sad. Without timely medical intervention, it occurs in 70-80% of cases.
People with PPS die approximately 15-20% of the time. The main cause of death with heart defects is heart failure, i.e. deterioration of the main function of the “pump” - pumping blood.
Other causes of death include heart rhythm disturbances, such as paroxysmal ventricular tachycardia, atrial fibrillation, and atrioventricular block. Due to atrial fibrillation, thromboembolism often occurs in the brain, leading to stroke.
How long can a person with heart failure live?
Heart failure can develop in a person due to the progression of a number of ailments or the presence of age-related changes in the body.
This disease negatively affects the ability of the myocardium to contract; organs cannot be supplied with blood in sufficient volume.
In heart failure, congestion is often observed, causing ascites - the accumulation of fluid in the abdominal cavity.
Features of the disease
Ascites is often called dropsy of the abdomen, since this disease is characterized by the accumulation of a significant amount of fluid in the abdominal cavity. The pathology occurs due to weak blood pumping, which occurs due to insufficient myocardial contractions.
A large number of stagnant masses in the vessels provokes the penetration of blood through their walls, since the liquid part simply has no way out. The released moisture takes up free space in the body, settling in the abdominal cavity, which is the most suitable place for this.
Against the background of these changes, the patient experiences a rapid enlargement of the abdomen with tension in its anterior wall. This is observed against the background of a general decrease in body weight, which causes concern in most patients. Weight loss or cachexia occurs due to leaching of protein from tissues, which indicates advanced heart failure.
Stagnation that occurs in the systemic circulation negatively affects the liver, causing chronic diseases and the development of cirrhosis. Typically, ascites occurs after these changes in the body.
The mechanism of formation of ascites in heart failure is similar to the formation of edema in any part of the body: an imbalance occurs between internal and external pressure. The pathogenesis of the disease can be a number of conditions, including:
- oncological diseases;
- liver diseases;
- advanced heart failure;
- pancreatitis;
- renal failure.
Liver cirrhosis, which often precedes the development of this disease, is its main cause.
In more rare cases, the course of ascites is possible without cirrhosis, but in this case another severe liver disease is required. For example, due to the growth of a cancerous tumor.
Significant pressure may be exerted on the vessels, which will interfere with normal blood flow and peritoneal fluid will begin to accumulate in the peritoneal area.
In heart disease, ascites develops as a result of blood stagnation in the heart chambers. When the organ ceases to cope with excess fluid, its accumulation occurs, which is most often observed in the veins of the lower extremities and the peritoneum.
Symptoms of the disease
In addition to a noticeably bloated abdomen, patients with ascites complain of the following symptoms:
- The occurrence of discomfort and pain in the abdomen, difficulty breathing. As the condition worsens, the patient has difficulty eating and performing daily activities.
- The development of spontaneous bacterial peritonitis, which can provoke abdominal pain, cause nausea and fever.
In the absence of timely diagnosis and treatment, this disease provokes renal failure. The circulatory system becomes infected, and the patient may experience confusion. In such cases, there is a significant risk of death. - Problems with urination.
- Improper functioning of the digestive system.
- Swelling of the limbs.
- Shortness of breath and lack of air at the slightest exertion, including at rest. This occurs due to the accumulation of fluid in the sternum area.
Most often, if ascites is suspected in heart failure, the patient is referred for ultrasound and computed tomography. In some cases, paracentesis is performed.
This procedure is characterized by the insertion of a small needle into the abdominal cavity, which serves to collect samples and then study them in the laboratory.
The resulting fluid is examined for the presence of oncology and infection, which makes it possible to determine the primary cause of its accumulation in the body.
The above symptoms often lead to an incorrect diagnosis. Due to lack of experience, young doctors often diagnose patients with CHF (chronic heart failure) with viral hepatitis. In the future, this can significantly complicate the treatment process.
With a significant increase in fluid volume, patients experience the following symptoms:
- the navel protrudes;
- There is no abdominal movement when breathing;
- the presence of skin stretch marks;
- when the patient lies on his back, a “frog belly” effect is observed, in which he lies flat;
- protrusion of veins on the anterior abdominal wall;
- fluctuation or fluctuation appears - one of the most characteristic signs of this disease.
Experts' forecast
Ascites is a very dangerous disease, which is characterized by rapid progression and complications in the form of diseases occurring against its background. Therefore, to accurately answer the question: “How long do people live with ascites from heart failure?” Only a doctor with extensive experience can do this based on a thorough examination of the patient’s condition.
On average, in the absence of adequate treatment, the patient's life expectancy can range from five months to several years. In most cases, the patient manages to live 5-7 years.
If the liver is destroyed, then only finding a donor can prevent death.
Due to various complications, there is a significant decrease in the quality of life of patients, because in addition to an enlarged abdomen, ascites can manifest as pain. Due to the development of liver cirrhosis, the skin may become yellowish. Acrocyanosis is also possible, which occurs when there is a lack of blood supply to small capillaries, causing the skin to become bluish.
In many ways, the patient’s life expectancy is determined by treatment, which is individual in nature, as well as the following factors:
- environment;
- nutrition;
- attitude to life and self-hypnosis;
- the presence of concomitant diseases and their stage.
Features of treatment
Ascites should be treated as early as possible, since the disease can progress rapidly, causing significant complications.
First, the doctor must identify the stage of the disorder by determining what condition the patient is in.
If the person has symptoms of heart or respiratory failure, the next step is to reduce the pressure in the abdomen and reduce the amount of fluid accumulated in the area.
Most often, such situations arise when there is a significant amount of accumulation, sometimes reaching 15 liters. Increasing pressure in the peritoneal area can negatively affect the functioning of not only the heart and lungs, but also the intestines. Because of this, problems with eating arise. Such patients require urgent hospitalization.
Modern treatment of abdominal ascites in heart failure involves the following:
- taking diuretics;
- maintaining a diet that includes a balanced diet and limited fluid intake;
- low-intensity exercise;
- laparocentesis, which involves puncturing the abdominal wall to remove accumulated fluid;
- traditional medicine, which can only be taken under the close supervision of a doctor.
If the form of the disease is not advanced and treatment is started in a timely manner, the prognosis will be favorable, the patient can live for many more years. If the patient ignores the symptoms, then the disease ultimately leads to death.
The life expectancy of patients with ascites in heart failure largely depends on the severity of the disease, the complications present and on how professional and fast the treatment will be.
An accurate prognosis can only be made by an experienced specialist based on a thorough diagnosis.
The methods of modern medicine can significantly alleviate the course of the disease and provide a greater likelihood of a favorable outcome.
Heart failure in the elderly: symptoms and treatment
Heart failure is a pathological condition in which the heart is unable to cope with the volume of blood that the body needs. The heart works, as before, to the maximum, but is not able to supply all organs with blood.
Heart failure in the elderly - what is it?
This is an acute or chronic disorder of the heart in an elderly person. HF entails insufficient blood supply to organs and tissues. The root cause of this condition is the deterioration of the heart’s ability to fully fill and empty due to damage to the myocardium. This is a common problem among older people.
- Chronic deficiency develops over a long period of time and is characterized by the following symptoms: fatigue, shortness of breath, swelling, decreased physical activity, etc.
- Acute heart failure is caused by toxins, trauma, and heart disease. If left unattended, this condition can lead to death.
Heart failure in the elderly is usually a symptom of other heart diseases: coronary artery disease, hypertension, heart attack, etc. HF does not occur on its own.
Source: https://baby-clinic-vozr.ru/narodnaya-medicina/skolko-mozhet-prozhit-chelovek-s-serdechnoj-nedostatochnostju.html
Possible causes
Among the causes of acquired defects, the most common are:
- Rheumatism, or more precisely, chronic rheumatic heart disease is an inflammation of its inner lining (including the valve apparatus), which develops after suffering (mainly in childhood) a streptococcal infection (tonsillitis).
- Infectious endocarditis is the gradual destruction of the heart valves due to the proliferation of bacteria on them. Infection can occur during the removal of a carious tooth, poor antiseptic treatment of the skin during an injection, or the use of unsterile syringes.
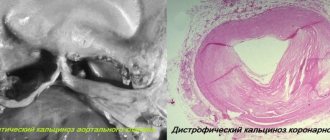
- Atherosclerosis and degenerative changes in valves are typical for older people.
More rare causes include syphilis and systemic pathologies - rheumatoid arthritis, lupus erythematosus, scleroderma.
The specific etiological factor of birth defects is difficult to determine. It can be:
- hereditary mutations – Down syndrome, Patau;
- maternal diseases - diabetes mellitus, thrombophilia, systemic vasculitis;
- intrauterine viral infections - rubella, cytomegalovirus, chickenpox;
- bad habits - smoking, drinking alcohol during pregnancy;
- exposure to ionizing radiation;
- the use of drugs that adversely affect fetal development - antitumor agents, sulfonamides, tetracyclines.
What is sudden cardiac death?
Sudden cardiac death ( sudden cardiac arrest ) is, by definition, an unexpected and natural death caused by cardiac causes in people with known or unknown heart disease, which begins with a sudden loss of consciousness and occurs within 24 hours of the onset of symptoms.
Sudden cardiac arrest is a consequence of cardiac arrhythmia , that is, a disorder of cardiac conduction of excitation. The heart no longer receives regular electrical impulses that normally cause the heart muscle to contract. As a result, the heart refuses its normal rhythm. The number of beats increases greatly in most cases to more than 500 beats per minute. A healthy person has between 60 and 80 beats per minute. This increase in heart rate leads to ventricular fibrillation , an uncoordinated contraction of the heart's muscle fibers. Heart failure occurs , in which uniform contraction of the heart muscle is no longer possible, resulting in the heart being unable to pump blood into the circulatory system.
If the condition is not treated immediately, ventricular fibrillation causes circulatory failure within seconds (circulatory arrest). After 1-2 minutes, patients lose consciousness, after 3-5 minutes irreversible damage occurs, and on average brain death occurs after 10 minutes .
How to determine the presence of a heart defect
To find out whether a person has a heart defect, I focus on the following data:
- symptoms and complaints bothering the patient;
- physical status – the appearance of the patient;
- electrocardiography;
- echocardiography (ultrasound of the heart);
- X-ray of the chest organs.
Symptoms, signs and typical appearance of the patient
People with heart defects mainly suffer from symptoms of heart failure. They experience difficulty breathing, especially at night, which is associated with a horizontal position of the body and increased pressure in the vessels of the lungs. For the same reasons, they may be bothered by paroxysmal cough.
Patients (especially with congenital heart disease) get tired very quickly, even after very little physical activity, they constantly want to sleep, they feel dizzy, and they may even faint.
Due to the enlarged liver, the patient feels heaviness or nagging/aching pain in the right hypochondrium. By evening my legs swell very much. Often bothered by aching pain in the left side of the chest, palpitations, and discomfort in the chest. Patients with certain congenital heart diseases regularly experience lower respiratory tract infections.
I often notice the so-called “drumstick symptom” in people with heart defects. This is a thickening of the terminal phalanges of the fingers. This sign indicates a long-term circulatory disorder throughout the body.
Newborns and infants with congenital heart disease are stunted and have reduced body weight. Often their lips, nose, and fingertips become bluish (cyanosis).
There are specific symptoms of heart disease. For example, with coarctation of the aorta, due to its pronounced narrowing, the blood circulation of the head, arms and upper body remains at the proper level, while the lower parts of the body and legs are depleted of blood. This leads to the fact that the muscles of the upper shoulder girdle stand out against the background of the underdeveloped muscles of the lower extremities. And a false impression of an “athletic physique” is created.
Another example is mitral stenosis. In the later stages of this PPS, against the background of general pallor of the face, a bright bluish-pink blush appears on the cheeks, while the lips and nose have a blue tint. This is called "facies mitralis", or "mitral face".
I would like to note that a person with PPS can feel quite healthy for a long time and not experience any pain or difficulty breathing. This is due to the fact that the heart tries to compensate for hemodynamic disturbances and at first copes well with this. However, sooner or later these mechanisms are not enough, and the disease begins to manifest itself clinically.
When I examine such patients, I am able to identify some pathological signs, for example, an increased cardiac impulse of the left or right ventricle, trembling of the chest. During auscultation of patients with heart disease, I often hear murmurs at the projection points of the valves, septa and carotid arteries; strengthening, weakening or splitting tones.
Instrumental diagnostics
Basic instrumental research methods for diagnosing heart defects:
- Electrocardiography. On the ECG, I can see signs of hypertrophy of different parts of the heart by changes in the height, width and shape of the teeth. Arrhythmias are often detected (atrial fibrillation is especially common).
- Echocardiography is perhaps the main diagnostic method that allows one to reliably establish a heart defect. Echo-CG clearly identifies the condition of the valves, septa, wall thickness and chamber volume. In Doppler mode, you can see the direction of blood flow between sections (regurgitation) and measure the pressure in the pulmonary artery. If a defect is suspected, I prescribe a transesophageal echocardiogram (a sensor is installed in the esophagus directly behind the heart) to obtain a more detailed image.
- X-ray of the chest organs - the image clearly shows the bulging of the pulmonary artery trunk, increased pulmonary pattern due to increased pressure in the vessels of the lungs, changes in the shape of the heart shadow, usuration of the ribs (uneven contour due to compression of them by the intercostal arteries).
Life expectancy
Despite the seriousness of this disease, patients should not despair. Today, there are many techniques that can stabilize the condition, alleviate symptoms and slow down the progression of pathology.
Important! This time can be used for a detailed examination of the body and preparation for surgical treatment, which ensures complete normalization of blood flow and hemodynamics, and contributes to a significant improvement in well-being.
The prognosis of patients also depends on the type of defect and its severity. Congenital defects tend to be worse and can cause early death. However, with timely detection and surgical treatment, it is possible to achieve normalization of heart function. But without surgery, patients do not live long, since already at the initial stages they experience significant disturbances in the body.
In the case of acquired defects the situation is different. This pathology does not lead to a rapid deterioration of the condition and a sharp increase in the risk of death. However, the presence of a defect means that the patient has a hemodynamic disorder. In addition, the disease that caused the development of the defect also plays a certain role. After all, even with valve replacement, chronic pathologies of the cardiovascular system do not disappear anywhere and can cause other dangerous conditions.
All this leads to the fact that the heart has to work in unfavorable conditions, it becomes exhausted, and patients develop or worsen heart failure and coronary heart disease.
Remember! As a result, how quickly the correct diagnosis is made plays a huge role.
If you start treatment in the early stages, you can significantly slow down or stop the progression of the pathology. In addition, surgical treatment is highly effective. But if you miss the time, then even after the operation the patient will suffer from various complications caused by prolonged overload of the heart.
Types of defects and their differences
As already mentioned, all heart defects are divided into congenital and acquired. They differ from each other in pathophysiology, severity, and human life expectancy.
There are many classifications of congenital heart disease, but most often clinicians use the Marder classification, which divides all congenital heart disease into defects with cyanosis and without cyanosis (i.e., “blue” and “white”).
Table 1. Characteristics of congenital heart disease
| Type | Name | Highlighting feature | Mechanism of hemodynamic disturbance |
| CHD without cyanosis (pale type) | Defects of the interventricular and interatrial septa | “Cardiac hump” (protrusion of the anterior chest wall) due to severe enlargement of the pancreas. Intense systolic murmur in the III-IV intercostal space to the left of the sternum | Discharge of blood from left to right. Overload of the left ventricle, then the right parts of the heart. Rapid development of pulmonary hypertension due to reflex spasm of the pulmonary arteries |
| Patent ductus arteriosus | Systole-diastolic murmur in the II-III intercostal space to the left of the sternum | Discharge of blood from the aorta into the pulmonary artery, increased blood flow in the pulmonary circle, overload of the left parts of the heart | |
| Isolated pulmonary stenosis | Weakening of the second tone and rough systolic murmur over the pulmonary valve | Sharp overload of the pancreas, depletion of pulmonary blood flow | |
| Coarctation of the aorta | High blood pressure, “athletic physique”, “chillness of the legs”, weakening or pulsation in the arteries of the lower extremities, Usuration of the ribs on the radiograph, systolic murmur along the entire left sternal border | Obstruction of blood flow through a narrowed section of the aorta, LV overload | |
| CHD with cyanosis (blue type) | Transposition of the great vessels | Severe general hypoxia (cyanosis, “drumsticks”), cardiac hump, loud first sound at the apex | Lack of oxygen in the organs through which the large circulation passes. |
| The only ventricle of the heart | Signs of hypoxia, systolic murmur at the apex | Mixing of arterial and venous blood, increased pulmonary blood flow, rapid overload of the ventricle | |
| Tetralogy of Fallot | Sharp weakening of the second tone over the pulmonary artery | Discharge of blood from right to left |
Acquired heart defects are divided into 2 types - stenosis, i.e. narrowing of the opening between the chambers, and insufficiency, i.e. incomplete valve closure. All PPS come down to the overflow of blood in some chambers of the heart and depletion of others, with all the ensuing consequences.
The most common PPS in adults is aortic stenosis (about 80%).
Combined defects can occur - when a person simultaneously has both insufficiency and valve stenosis. I also quite often see people who have multiple valves affected. This is called a combined heart defect.
Table 2. Characteristics of teaching staff
| Type | Name | Highlighting feature | Mechanism of hemodynamic disturbance |
| Mitral valve defects (MV) | MK deficiency | Weakening of the first tone, systolic murmur at the apex | Reverse discharge of blood into the left atrium |
| Mitral stenosis | Loud first sound, diastolic murmur at the apex. Facies mitralis. | Severe overload of the left atrium, its hypertrophy and expansion. Increased pressure in the pulmonary vessels due to reflex spasm | |
| Aortic valve defects (AV) | AC deficiency | Increased pulse blood pressure, visible pulsation of the carotid arteries, protodiastolic murmur on the AC | Distension of the left ventricle by reverse flow of blood from the aorta |
| Aortic stenosis | Pain resembling angina pectoris, constant fainting. Rough systolic murmur on the AC, extending to the carotid arteries | Deterioration of blood ejection into the aorta, left ventricular overload | |
| Pulmonary valve defects (PA) | LA insufficiency | Weakening of the second sound on the pulmonary valve, protodiastolic murmur in the second intercostal space to the left of the sternum | Backflow of blood into the right ventricle |
| PA stenosis | Strengthening and splitting the second tone. Pronounced pulsation of the right ventricle | Obstruction of blood ejection into the PA, overload of the RV | |
| Tricuspid valve defects (TC) | TC deficiency | Systolic murmur on TC | Reverse discharge of blood into the right atrium |
| TC stenosis | Strengthening the first tone on TC | Overload of the right atrium, its expansion and hypertrophy |
Classification
Congenital heart defects can be divided into 3 large groups:
- Pathology with preserved pulmonary blood flow:
- aortic stenosis;
- coarctation of the aorta.
- Defects with increased pulmonary blood flow:
- ventricular or atrial septal defect;
- open ductus arteriosus.
- Conditions accompanied by decreased pulmonary blood flow:
- triad or tetralogy of Fallot;
- pulmonary artery stenosis.
In addition, among doctors there is a distinction between “white” and “blue” defects based on the rate of development of acrocyanosis. However, this classification is conditional, because any defect in the final stages causes cyanosis of the skin and mucous membranes.
How are heart defects treated?
Unfortunately, there is no medicine that can cure a person from heart disease. And all congenital heart disease can only be treated surgically. An exception is the patent ductus arteriosus, a congenital defect that can be completely eliminated pharmacologically. But this is effective only in the first day of a person’s life. To do this, I prescribe intravenous administration of a non-steroidal anti-inflammatory drug (Ibuprofen, Indomethacin) for 3 days.
If cyanosis and signs of severe heart failure are present, surgery is performed immediately. Often, surgeons even have to operate on infants and one-year-old children. If the defect was discovered by instrumental examination methods, and the patient is not worried about anything, or there are minor symptoms, the operation can be postponed.
Traditionally, surgical interventions to eliminate congenital heart disease are performed under general anesthesia, on an open heart, with connection to a heart-lung machine. The defect is either sutured or covered with a patch of pericardium or synthetic tissue. The open duct is ligated or divided.
Recently, in specialized cardiology centers with appropriate equipment, it has been possible to perform minimally invasive endovascular interventions. In such operations, under ultrasound and X-ray guidance, a catheter is inserted through the femoral vein and reaches the right atrium. An occluder is inserted through the catheter, which consists of connected disks of nickel-titanium wire. This occluder closes the defect.
The main contraindication to such operations is advanced pulmonary hypertension with severe vascular sclerosis. In these cases, so-called palliative interventions are performed, which eliminate not the defect itself, but its consequences. Communications (anastomoses) are artificially created between large vessels so that blood flows bypassing the overloaded parts of the heart.
Now let's look at the treatment of acquired defects. Things are a little different with them.
If PPS developed against the background of rheumatism, then, according to the protocol, I always use antibacterial therapy with penicillin antibiotics. This point is very important, since the presence of streptococcal bacteria in the body can cause the development of new heart defects.
I also always prescribe drug therapy that will help stabilize the patient’s condition.
First of all, medications are used to slow the progression of heart failure:
- ACE inhibitors – Perindopril, Ramipril;
- beta blockers – Bisoprolol, Metoprolol;
- diuretics - Torasemide;
- aldosterone antagonists – Spironolactone, Eplerenone;
In case of heart rhythm disturbances, I use antiarrhythmic drugs - Sotalol, Amiodarone.
It is important to carry out anticoagulant therapy, since some of the PPS, especially mitral stenosis, are often accompanied by atrial fibrillation, in which blood clots form in the cavity of the left atrium, leading to cardioembolic stroke. To prevent this, I prescribe Warfarin or low molecular weight heparins.
When the patient’s condition is serious, when medications no longer help, I refer patients for surgical treatment.
There are 2 main types of operations for PPP:
- valve replacement;
- reconstructive operations - valve repair, commissurotomy, balloon valvotomy.
Valve prostheses can be mechanical (artificial) or biological. Their key difference is as follows. When installing a biological valve, the patient must receive anticoagulant therapy for the first 3 months after surgery, and when implanting a mechanical valve, for life. The question of choosing the type of valve is decided on an individual basis each time.
The only anticoagulant approved for long-term use with an artificial heart valve is Warfarin.
Mechanical valves are more durable, but their cost is much higher compared to biological ones.
Death from Heart Failure: How to Recognize the Signs
In medicine, sudden death from heart failure is regarded as a fatal outcome that occurs naturally. This happens both to people who have had heart disease for a long time, and to people who have never used the services of a cardiologist. A pathology that develops quickly, sometimes even instantly, is called sudden cardiac death.
Often there are no signs of a threat to life, and death occurs within a few minutes. The pathology can progress slowly, starting with pain in the heart area and rapid pulse. The duration of the development period is up to 6 hours.
Statistics of mortality from heart failure and age characteristics
One in five people will experience symptoms of heart failure during their lifetime. Instant death occurs in a quarter of victims.
The mortality rate from this diagnosis exceeds the mortality rate from myocardial infarction by approximately 10 times. Up to 600 thousand deaths are reported annually due to this reason.
According to statistics, after treatment for heart failure, 30% of patients die within a year.
More often, coronary death occurs in persons 40-70 years old with diagnosed vascular and cardiac disorders. Men are susceptible to it more often: at a young age 4 times, in the elderly – 7 times, by the age of 70 – 2 times. A quarter of patients do not reach the age of 60 years.
The risk group includes not only elderly people, but also very young people.
The cause of sudden cardiac death at a young age can be vascular spasms, myocardial hypertrophy caused by drug use, as well as excessive stress and hypothermia.
What does the prognosis depend on: how long do patients live?
I am often asked: “How long do people live with heart disease?”
This depends on many factors such as:
- type of defect;
- its heaviness;
- degree of heart failure;
- presence of complications;
- timeliness of diagnosis and treatment;
- following the doctor’s recommendations (correctly taking medications in compliance with all dosages, etc.);
- the quality of the operation performed.
Without surgical intervention, patients with many congenital heart diseases die in early childhood (up to 2-5 years). CHDs in which a person can live to adulthood without surgery include coarctation of the aorta and atrial septal defect.
The most favorable PPS in terms of prognosis are mitral and tricuspid regurgitation. Serious complications develop rarely and over a long period of time. With other PPS (mitral, aortic stenosis), patients die approximately 5-10 years after the first onset of symptoms.
Modern treatment options, both pharmacological and cardiac surgery, make it possible to extend the life of such people to 60-70 years.
How long do people live with coronary heart disease (CHD) - the cause of death in the chronic form?
For patients suffering from this pathology and their relatives, the answer to the question is very important: how long do they live with coronary heart disease?
This pathology is the main cause of death and disability in all developed countries.
It affects the most working-age part of the population - the age group up to 65 years, causing 15 million deaths per year worldwide (according to WHO).
- All information on the site is for informational purposes only and is NOT a guide to action!
- can give you an ACCURATE DIAGNOSIS !
- We kindly ask you NOT to self-medicate, but to make an appointment with a specialist !
- Health to you and your loved ones!
Causes of sudden death
The main cause of sudden death in adulthood and old age is various forms of ischemic heart disease in combination with hypertension, or separately from it.
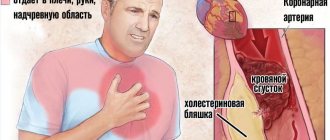
The essence of this pathology is that the myocardium is insufficiently supplied with arterial blood, or it does not flow at all. This results in an acute lack of blood for optimal myocardial function, and the reason for this is the coronary arteries altered by destructive processes.
Causes of changes in arteries and pathological blood supply to the myocardium:
- formation and growth of atherosclerotic plaques;
- thrombus formation;
- regional arterial spasms;
- epithelial dysfunction;
- microcirculation disturbance.
These reasons underlie the classification of IHD, which is based on the recommendations of the World Health Organization.
She positions this pathology as a chronic or acute transient condition, which is caused by disturbances in the functional state of the coronary arteries (their spasms, dysregulation of vascular tone), or their organic lesions (thrombosis, stenosing atherosclerosis).
Clinical forms of coronary heart disease:
- Myocardial infarction, which is divided into large-focal, small-focal, subendocardial, intramural. According to the degree of occurrence, it can be acute, repeated, recurrent.
- Angina pectoris, which is divided into angina pectoris, resting angina, and progressive angina.
- Post-infarction cardiosclerosis, developing 2 months or more after a heart attack.
- Focal myocardial dystrophy.
- Heart rhythm disturbances.
- Acute coronary insufficiency, or primary cardiac arrest, often leading to instant death.
Most often, sudden death is caused by such clinical forms of IHD as angina pectoris, myocardial infarction, acute heart failure, cardiac arrhythmia, in particular ventricular fibrillation against the background of acute myocardial ischemia.
The so-called instant death is preceded by myocardial hypoxia, lasting from 2 to 5 hours. During this period, changes in the structure of heart tissue develop.
Coronary artery disease develops against the background of atherosclerotic damage to the arteries of the heart. It is this factor that becomes decisive in the occurrence of the clinical picture of IHD. Although manifestations of atherosclerosis are not uncommon in the age group of 40 years and older, not everyone develops manifestations of cardiac ischemia.
In people suffering from this pathology and suddenly dying from it, the phenomena of atherosclerosis appear 20-30 years earlier, these destructive changes progress much faster, the lumen of the coronary arteries becomes stenotic earlier.
A heart that has pathological changes in its structure is unable to adequately adapt to changes in the external and internal environment.
When these changes are combined in a single complex, a breakdown occurs in the coronary system, and, as a result, premature death. Internal risk factors leading to sudden death in patients with coronary artery disease:
- arterial hypertension;
- obesity;
- elevated cholesterol levels;
- chronic tobacco intoxication.
In addition to these factors, external risk factors are of great importance for the onset of premature death in patients with coronary artery disease:
- mental stress, chronic or momentary stress;
- alcohol intoxication;
- physical stress;
- sudden change in weather.
In order for these factors to become fatal, the cardiovascular system and coronary circulation must be in an unstable position.
In persons suffering from coronary artery disease, a state of unstable compensation is the natural state of the vascular system, and the trigger for cardiac circulatory disorders is any of the above external influences, or a complex of them.
The gender factor also matters in the statistics of premature deaths, since men are more susceptible to them than women of the same age with manifestations of coronary artery disease.
How long do people live with coronary heart disease?
According to specialists from the Institute of Cardiology named after. A.L. Myasnikov, the mortality rate of patients with coronary artery disease can be compared with the mortality rate from complicated lung cancer.
What are the prognoses for coronary artery disease, angina pectoris FC3 and post-infarction cardiosclerosis, read here.
If we analyze how many people live with coronary heart disease depending on the functional class of the disease, then the results per 10 years following the onset of the disease will be as follows:
One of the main aspects when predicting survival over the next 10 years in chronic ischemic heart disease is electrocardiogram data:
The combination of arterial hypertension, previous myocardial infarction and ST segment with signs of depression is the most unfavorable prognosis that can be made by analyzing the ECG results.
To predict the state of myocardial function and coronary circulation, an informative indicator is the results of a test using a bicycle ergonometer.
It is carried out in combination with heart rate recording, ECG and blood pressure monitoring at regular intervals. The survival prognosis is better the longer the signs of fatigue during physical activity do not appear, as well as the shorter the duration of the displacement and severity of the ST segment on the cardiogram.
If one of the pronounced symptoms of coronary artery disease is arrhythmias, the prognosis is determined depending on the type of heart rhythm disorder:
To reduce the risk of mortality in such arrhythmias, implantation of a defibrillator is advisable. This treatment method is indicated:
With a heart attack, the prognosis is heterogeneous depending on the age group to which the person who suffered it belongs:
Additional factors that worsen the prognosis of survival with coronary artery disease:
When establishing a survival prognosis, it is necessary to take into account many factors, among which the most significant are: the severity of angina (angina pectoris), resistance to physical activity, the degree of damage to the coronary arteries, and the contractile function of the left ventricle.
Source: https://serdce.hvatit-bolet.ru/skolko-zhivut-s-ishemicheskoj-boleznju-serdca.html
Consequences of pathology
A patient with a heart defect, both congenital and acquired, has a high risk of developing acute heart failure (pulmonary edema, cardiogenic shock), which without prompt medical intervention leads to death.
Also, people with heart defects develop coronary disease much earlier, which means they are several times more likely to have a myocardial infarction.
Almost any heart defect is accompanied by rhythm disturbances. The most dangerous of them are ventricular tachyarrhythmias and atrioventricular block.
With some defects, due to severe overload of the pulmonary circulation and reflex narrowing of the pulmonary vessels, pulmonary hypertension occurs - a very serious condition, difficult to respond to drug therapy, requiring surgical intervention.
Due to prolonged severe oxygen starvation (hypoxia) of the whole body, the immune system suffers, which is why patients with heart defects constantly suffer from infectious diseases, especially bronchitis and pneumonia.
With any heart defect, as well as the presence of prosthetic valves, the risk of infectious (bacterial) endocarditis increases several times - a dangerous disease that affects the heart valves, often ending in death.
Do you want to know how long you have left to live?
Scientists have identified 12 risk factors that determine the chance of a person over 50 years old dying in the next four years.
The test is based on data from the 1998 National Health Survey of 11,701 Americans over the age of 50.
So what is the probability of death in the next 4 years:
1. Age: 60-64 years = 1 point; 65-69 = 2 points; 70-74 = 3 points; 75-79 = 4 points; 80-84 = 5 points; 85 and older = 7 points.
2. Gender: Male = 2 points.
3. Body mass index: less than 25 (normal weight or less) = 1 point.
4. Diabetes: 2 points
5. Cancer (excluding minor skin cancers): 2 points.
6. Chronic lung disease that limits activity or requires the use of oxygen at home: 2 points.
7. Chronic heart failure: 2 points.
8. Smoking: 2 points
9. Difficulty taking a shower due to health or memory problems: 2 points.
10. Difficulty paying bills on time or keeping track of all expenses due to health or memory problems: 2 points
11. Difficulty walking several blocks due to health problems: 2 points.
12. It is difficult to move or drag a heavy object, such as a chair.
due to health problems: 1 point.
Result: 0 to 5 points = less than 4 percent risk of death; 6-9 points = 15% risk; 10-13 points = 42 percent risk; Score of 14 or more = 64 percent risk.
The accuracy of this test is approximately 81%. Many experts question the results because many factors remained unexamined - family history, blood pressure and cholesterol levels, etc.
“Even if your risk of death is 60%, it is not an absolute number. “You can still change everything for the better, for example, quit smoking or take up exercise and improve your health,” says study co-author Dr. Kenneth Covinsky.
Particularly interesting is the third point of the test, which states that people of normal weight are at greater risk. In fact, the idea is different - points are awarded to those who have lost weight due to illness. Overweight people will "earn" their points by answering the last few items on the test.
Most patients are skeptical about this test: “I don’t know how long I have to live, but no one else can tell me the date of my death,” says Willie Hood Jr. 74. “The doctors told my grandmother that she would not survive the night, but she lived after that for another three years.”
Published in the Journal of the American Medical Association.
Source:
Qyl.ru
If you notice a spelling, stylistic or other error on this page, simply highlight the error with your mouse and press Ctrl+Enter. The selected text will be immediately sent to the editor
Case study: a teenager with coarctation of the aorta
Let me give you one interesting case from my practice.
A mother came to see me with her 15-year-old son, who has been troubled by headaches, chilliness and strange weakness in his legs since early childhood. At the age of 7 years, the boy was in the hospital in the pediatric department, where he was diagnosed with high blood pressure up to 150/90 mm Hg. A diagnosis was made: “Hypertension”, medications were prescribed. The patient took medications irregularly. The young age of the patient, as well as the absence of hypertension in the mother and father, made me doubt the diagnosis and suspect the “secondary nature” of high blood pressure. During a general examination of the patient, in addition to elevated blood pressure (155/90 mm Hg), I was able to detect weakened pulsation in the arteries of the legs and a systolic murmur at the back at the level of the lower angle of the scapula. I ordered an echocardiogram, which showed thickening of the left ventricle and an area of narrowing in the thoracic aorta. The radiograph clearly showed another sign of coarctation of the aorta – rib usuration (uneven contour). The patient underwent surgery - plastic surgery of a narrowed section of the aorta. The boy's condition improved, blood pressure returned to normal, and the need to take medications to correct blood pressure disappeared.
Why is heart disease dangerous and can it be cured?
Heart disease is a disease of the heart valves in which the organ begins to malfunction. As a result of congenital or acquired changes in the structure of the valve apparatus*, cardiac septa, walls, or large vessels extending from the heart, a disturbance in the blood flow of the heart occurs. Congenital heart defects are distinguished by a variety of anomalies in the development of the heart and blood vessels and usually appear in childhood. Acquired defects form at different age periods due to heart damage due to rheumatism and some other diseases.
Expert advice: living with heart disease
I would like to give a few recommendations that will help avoid most of the negative consequences and increase the effectiveness of treatment:
- sports – professional training will have to be stopped. Minor physical activity is allowed;
- Regular examination - it doesn’t matter whether you were successfully operated on as a child or have only recently been diagnosed with mild mitral regurgitation. In case of heart disease, it is necessary to visit a cardiologist at least once every six months to a year, do an ECG and Echo-CG to check the state of heart function, as well as to monitor the occurrence of possible complications;
- table salt - if you have been diagnosed with signs of chronic heart failure and you have been prescribed medications for its treatment, for greater effectiveness you need to limit the use of table salt with food to 2-3 grams per day;
- Warfarin – This drug is often prescribed to patients with heart defects to prevent blood clots. In order for its use to be effective and at the same time safe, you need to regularly do a blood test (coagulogram). The INR in this study should be greater than 2 but less than 3;
- a visit to an otolaryngologist - if you have been diagnosed with PPS of rheumatic origin, be sure to go for a consultation with an ENT doctor, since the main cause of rheumatism is tonsillitis (tonsillitis). In the presence of chronic tonsillitis, treatment of the tonsils (washing, antibiotics) is necessary, and possibly their removal. This is necessary to prevent relapse of rheumatism and the appearance of a new heart defect.
- prevention of infective endocarditis - all people with heart defects and prosthetic valves have an increased risk of developing infective endocarditis. Therefore, to prevent it, they must take penicillin antibiotics (Amoxicillin, Ampicillin) once, approximately 30 minutes/1 hour before medical procedures (tooth extraction, bronchoscopy, cystoscopy, etc.).
How long do people live with coronary heart disease (CHD)?
How to help a person who has heart pain?
Alevtina, Kostroma
– Sit him down or lay him down, give him a nitroglycerin tablet under the tongue. This drug causes headaches for some. Then it can be replaced with Votchal drops (drop 6-8 drops onto a piece of sugar and let it dissolve in the mouth). If one tablet does not help, a second tablet should be given along with an aspirin tablet.
It is recommended to chew aspirin and wash it down with hot water. If you have a tonometer, measure your blood pressure; for numbers below 100/60 mmHg, nitroglycerin should be given with caution and preferably in a lying position. In cases where repeated use of the medication does not stop the attack, you should immediately call an ambulance.
Exercise or walking
Doctors say that physical activity protects the heart and blood vessels from diseases. What should the load be for it to really be beneficial?
Alena, Uglich
– Any regular physical activity (gym classes, swimming, skiing, skating) at least 4 times a week and at least 40 minutes at a time can strengthen the heart and blood vessels. Vigorous walking can also help in this matter.
In men, a heart attack often occurs after unusual physical activity, for example, a dacha rush. The load on the heart should increase gradually.
Healthy eating is the best treatment
I was diagnosed with angina pectoris. The doctor advises you to lose weight, quit smoking and take half a tablet of aspirin a day. Where is the treatment?
Evgeniy Petrovich, Mytishchi
– The main thing that needs to be done before the disease goes too far is to change your lifestyle. American doctors managed to reduce mortality from cardiovascular diseases by almost 20% only through preventive work with the population. Smoking has long gone out of fashion there, and it has become good practice to exercise and ensure that your food does not contain too many carbohydrates.
Nicotine has a bad effect on blood vessels, making them more sensitive to factors that cause spasms; In addition, it inhibits a protein in endothelial cells that promotes the dissolution of blood clots (thrombi) in blood vessels.
Excess weight also leads to the development of cardiovascular diseases. If you want your diet to be healthy, eat more vegetables, fruits, cereals, fish, low-fat dairy products and less fatty meat. A study in India found that improving diet alone could lead to a significant reduction in deaths from heart disease.
Now about aspirin. The European Society of Cardiology recommends taking it at a dose of 75 to 150 mg daily for those who suffer from angina or have already suffered a myocardial infarction. With angina pectoris, the formation of blood clots is especially dangerous. This can be avoided by taking aspirin; it reduces the blood's ability to clot.
The older the patient, the more difficult it is
In what cases is heart surgery performed for angina? Are there age restrictions?
Olga Evgenievna, Murmansk
– There are no clear age restrictions, although, of course, the older a person is, the more other diseases he may have that may limit operations.
A preliminary examination of the blood vessels is carried out. A so-called coronary angiography is performed, during which the heart vessels are filled with a contrast agent. This allows you to determine exactly where the disruption of blood supply to the myocardium occurs.
The most common procedure now performed is angioplasty.
During this procedure, a special probe is inserted into the artery of the heart through a puncture of the peripheral vessels without any incisions in the chest or the heart itself.
At the end of this probe there is a device that, under the influence of forced air, expands the narrowed area of the affected artery of the heart and restores impaired blood circulation.
To prevent the straightened vessel from narrowing again, a special wire frame, called a stent, is inserted into the site of its lesion, again through a probe. In the vast majority of cases, this procedure not only prevents a heart attack, but also returns the sick person to normal life.
In cases where angioplasty cannot be performed, one has to think about surgery on the heart vessels, which is called coronary artery bypass grafting. An additional vessel taken from the veins of the legs or from the arteries of the patient is sewn into the vessels of the heart, which also ensures the restoration of blood flow in the heart muscle.
There are different forms
I heard that not all angina is dangerous. This is true?
Elena, Tambov
– Yes, there are patients who live with angina into old age. It all depends on the form of the disease.
The greatest concern is unstable angina, in which attacks of chest pain become more frequent and prolonged.
Pain begins to occur not only during physical activity, but also at rest. To stop them, not one, but 2-3 or more nitroglycerin tablets are required.
American doctors, for example, have developed a special program to equip public places with defibrillators. In Germany, there are defibrillators even in the subway. With the help of equipment that acts on a stopped heart with an electric discharge, there is a much greater chance of saving a person.
Interesting
Family support
Psychological support from the family can work wonders, say members of the European Society of Cardiology. If someone in your family is sick, help him change his lifestyle. A patient is more likely to quit smoking if his wife and household members do not smoke. Eat differently by changing the diet of the whole family. Walking and playing sports in the fresh air will benefit everyone.
Diet instead of drugs
A group of European scientists has developed a preventive diet, the effectiveness of which is comparable to the effect of drugs. It includes red wine, fish, dark chocolate, almonds, garlic, olive and soybean oil, soybeans, tomatoes, oats, bran, corn, peas and green tea.
150 ml of red wine daily reduces the risk of cardiovascular diseases by more than 30%, 100 g of chocolate - by 20%, 114 g of fish 4 times a week - by almost 15%.
Fruits and vegetables help lower blood pressure, and almonds and garlic reduce cholesterol levels.
By the way
Let's measure your waist
As an indicator of obesity, you need to focus not on body weight, but on waist circumference.
| No obesity | Deviation zone | Qualified help needed | |
| Men | Less than 94 cm | 94-101 cm | More than 102 cm |
| Women | Less than 80 cm | 80-87 cm | More than 88 cm |
If your waist size is in the “deviation zone”, you need to move more and lose weight. Those who find their result in the last column are advised to seek help from nutritionists.
Source: https://marta2.ru/skolko-zhivut-stenokardiey/
How is heart surgery performed?
Most heart surgeries are performed under artificial circulation. After operations, patients require long-term rehabilitation with a gradual restoration of their physical activity. The deterioration of the operated patient's condition may be associated with the development of complications caused by surgery, so patients should undergo periodic examinations in cardiology centers. If the postoperative period is uncomplicated, many patients can return to work 6–12 months after surgery.
* Heart valve - a part of the heart formed by the folds of its inner membrane, ensures unidirectional blood flow.
** Myocardium is the middle muscular layer of the heart, constituting the bulk of its mass.
*** Heart valve insufficiency is a type of heart defect in which, due to incomplete closure of the valve, due to its damage, part of the blood flows back to the parts of the heart from which it came.
**** Myocardial infarction is an acute form of coronary heart disease.
What is the chance of recovery for a person suffering from heart disease?
No matter what diagnosis you are given, you never need to program yourself for negativity. You should always count on the best, because modern medicine provides many guarantees and hopes. Speaking about modern surgical techniques, the hopes of seriously ill patients cannot be called unfounded. Innovative equipment, modern medical inventions and high professionalism of doctors make it possible to give a fairly good chance of recovery for people with severe forms of heart disease.
Heart disease is not a death sentence, because there are many other diseases that are potentially life-threatening. It is always worth considering that even the most experienced and highly qualified doctor will not be able to determine the period that the patient can count on. Each individual case is individual; in most cases it is physically impossible to predict the course of the disease. The best diagnostic equipment is not able to determine life expectancy, so you need to work on your own recovery and prevent the progression of the disease yourself.
It is necessary to understand that minor pathologies of the heart muscle can be fully treated at the earliest stages. The task of any person who is faced with such an illness is to make a timely diagnosis and follow all medical instructions. A systematic examination, observation by a cardiologist and preventive procedures will help get rid of symptoms or completely recover from the disease.
How real is the risk of cardiac arrest?
Heart disease is a heart failure that can have various causes:
- pathologies in the structure of the heart muscles;
- deviations in the functionality of valves and their mechanisms;
- irregular structure of the myocardium of varying levels of complexity.
Functional malfunctions in the mechanism of the heart provoke changes in the functioning of the vascular system, which can lead to diseases of other organ systems. Poor circulation can manifest itself in a variety of ways.
People with heart disease are the first to be at risk when it comes to the likelihood of a heart attack or stroke.
Frightening forecasts from doctors worry many people who are faced with the problem of the functionality of the cardiovascular system. But you should take the words of doctors adequately and realize that mortality risks are common among advanced cases of heart failure. Timely treatment and medical support will help you completely get rid of risks and pain. Modern medical technologies allow heart patients to live peacefully without worrying about dire prognoses.
Severe forms of heart defects should be reviewed by a cardiac surgeon. Modern approaches to surgical intervention often give a person a chance for a second life.
What is the difference between a congenital heart defect and an acquired one?
Congenital heart defect
Congenital heart disease is detected in approximately 1% of newborns. The cause of the disease is improper development of the organ inside the womb. Congenital heart disease affects the walls of the myocardium** and large adjacent vessels. The disease may progress. If surgery is not performed, the child may develop changes in the structure of the heart, which in some cases can lead to death. With timely surgical intervention, complete restoration of heart function is possible.
Prerequisites for the development of congenital heart disease:
- impaired fetal development under the influence of pathogenic factors in the first months of pregnancy (radiation, viral infections, vitamin deficiency, uncontrolled use of medications, including some vitamins);
- parental smoking;
- alcohol consumption by parents.
Acquired heart defect
Acquired heart disease does not occur immediately after birth, but over time. It manifests itself in the form of malfunction of the heart valve apparatus (narrowing of the walls or insufficiency of the heart valves***).
Surgical treatment consists of replacing the heart valve with a prosthesis.
If damage to two or more orifices of the heart or valves is detected simultaneously, they speak of a combined acquired defect. To prescribe surgery for an acquired defect, it is classified according to the degree of anatomical changes and disorders.
Causes of acquired heart disease:
- endocarditis - rheumatic or (less often) of another nature. For more details, see the information about inflammatory heart diseases;
- atherosclerosis;
- myocardial infarction****;
- heart injury.