The cause and source of origin of noises heard during atherosclerotic lesions of the carotid bifurcation (the place of further division of the common carotid artery into its internal and external branches), which has not yet led to the occurrence of a transient ischemic attack (TIA, microstroke) or cerebral stroke, is unknown. According to publications, the studies analyzed small populations, and in most of them it was not possible to establish the location and severity of stenosis (narrowing of the artery lumen) of the carotid bifurcation.
Examinations of patients with asymptomatic stenosis and cervical murmurs referred for major vascular surgery are characterized by similar shortcomings. Most studies have found that patients with cervical murmurs have an increased risk of heart disease, stroke, and death. Meanwhile, a stroke (cerebral infarction) does not necessarily develop in the basin of the vessel from which the noise comes. Taking this into account, it is not always advisable to perform operations on the carotid artery in patients with asymptomatic stenosis (narrowing of the internal lumen of the artery).
However, in patients with severe stenotic lesions at the beginning of the internal carotid artery (when 1.5 mm or less remains from the original lumen of the vessel during its narrowing), which reduces blood flow to the brain in the distal (overlying) sections of the internal carotid artery, the risk of thrombotic occlusion is increased (blockage of the artery lumen).
Although these patients have decreased blood flow in the superior internal carotid artery, the lesion remains asymptomatic due to sufficient ipsilateral (from the opposite side) blood flow through the anterior part of the circle of Willis into the ipsilateral middle and anterior cerebral arteries. Therefore, a stroke (cerebral infarction) may develop later due to arterioarterial embolism. The noise accompanying severe stenosis (narrowing of the lumen) at the beginning of the internal carotid artery is high-pitched and long-lasting, often heard during auscultation and during diastole. As the stenosis of the vessel supplying the brain progresses and the blood flow in it slows down, the noise weakens and disappears when occlusion occurs (complete blockage of the lumen of the artery).
Non-invasive methods for studying the carotid arteries, which include B-scanning, Doppler ultrasound examination of blood flow (USDG) immediately distal (above) the area of stenosis (narrowing) of the lumen of the vessel, quantitative spectral analysis of noise and determination of oculo-systolic pressure using oculoplethysmography, allow identification areas of pronounced stenosis.
There is no data studying the effectiveness of endarterectomy compared with antiplatelet therapy (aspirin, trental, etc.) for asymptomatic carotid bifurcation stenosis, so the doctor can choose any of these methods of treating the patient. More often, for stenosis (narrowing of the lumen) at the level of the carotid artery bifurcation, antiplatelet agents (aspirin, trental, etc.) are prescribed. If signs of progressive narrowing are documented (ultrasound, CT angiography, MRI angiography) and the diameter of the residual (remaining) lumen of the vessel (artery) is 1.5 mm or less from the initial lumen of the vessel during its narrowing, then surgical intervention is considered the method of choice when treating the patient - endarterectomy operation.
The complication rate of endarterectomy should not exceed 2%. However, there is no evidence yet that surgical treatment of patients with asymptomatic stenosis and cervical murmurs is more effective than conservative therapy, and therefore further collection of statistics is necessary.
The term “bifurcation” has been used in medical literature for quite a long time. Today, several concepts are known that include this word.
About the meaning of the term
Bifurcation is some kind of split. Moreover, this concept usually indicates that the division occurred into 2 parts with approximately the same diameter. It is important that both branches extend at comparable angles. Excellent examples are the bifurcation of the carotid artery, aorta or trachea.
Despite the fact that this term has taken root best in medicine, it is quite possible to use it in other areas. For example, in geography there is sometimes such a concept as
About the aorta
Bifurcation is a division into 2 approximately equal parts. In the case of the aorta, this term has been used for a very long time, but in fact it is not entirely correct. The fact is that the common ones are not equal continuations of the aorta, but just its branches. She herself descends even lower in the form of a small thin vessel.
Aortic bifurcation occurs at the level of the IV lumbar vertebra. This place is one of the critical ones in terms of the vessel’s stability against constant blood pressure. The fact is that this is where aortic dissection occurs quite often. This state of affairs is due to the fact that the bifurcation is a place that is constantly exposed to increased influence from the blood. It is here that it should be distributed along the two common iliac arteries. The result is various kinds of blood turbulence and the damaging effects of these flows on the vessel wall at the bifurcation site.
In addition to possible aneurysms in the area of the aortic division, there are excellent preconditions for the formation of atherosclerotic plaques. This is due to the fact that trauma to the vessel where the artery bifurcates into two parts occurs much more often than in any other areas. Gradually increasing in size, this plaque can significantly reduce the level of blood flow in the pelvic organs and lower extremities.
Aortic division
The aorta divides into arteries (common iliac) in the region of the fourth lumbar vertebra. These vessels, about 6 cm long, are directed downward and sideways at an angle of 30-60°. The left common iliac artery is slightly shorter than the right. The right one, in the area of the junction of the ilium with the lateral part of the sacrum, is divided into an external and internal vessel - they supply the peritoneal organs and legs with blood.
The bifurcation point is the weak point of the aorta; here the vessel often undergoes dissection due to constantly elevated blood pressure. The blood, dividing, swirls and negatively affects the aortic wall at the bifurcation site, provoking the development of:
- aneurysm - occurs due to the loss of elasticity and strength by the vessels. Patients need urgent treatment - there is a high probability of aneurysm dissection, aortic rupture and more serious consequences;
- thrombosis (Leriche syndrome) - more often diagnosed in elderly patients with atherosclerosis. It develops slowly, with adequate treatment the prognosis is favorable;
- embolism – can cause blood obstruction, ischemic damage to the vessels of the legs, peritoneal and pelvic organs. Requires surgery.
With the development of pathologies of the aortic bifurcation, the renal and common iliac arteries are often affected. In a quarter of patients, the damage spreads even further. The condition is characterized by severe pain. With intermittent claudication caused by damage to the aortic bifurcation, they are localized in the thighs and buttock muscles. In men, the pathology reduces libido and causes weakened erections, sometimes even impotence.
Aortic bifurcation syndrome
This pathology is very dangerous. It brings a lot of unpleasant sensations to the patient himself and can seriously harm his health. Most often, this syndrome is accompanied by damage not only to the area of the aortic bifurcation itself, but also to other areas. We are talking about the renal as well as the common iliac arteries. Further, the pathological process spreads only in a quarter of patients.
The main signs of aortic bifurcation syndrome are circulatory disorders in the vessels of the lower extremities and pelvis. Accordingly, the main clinical manifestations also relate to these areas. If we talk about the lower extremities, patients feel quite severe pain. They have a so-called
Such clinical manifestations are so pronounced for the reason that it is ischemic (with a lack of blood supply) pain that is the most severe. A distinctive feature specifically in aortic bifurcation syndrome is the fact that pain is localized not in the legs, but mainly in the hips and even
If we talk about manifestations from the pelvic organs, then it should be noted that they are typical only for men. They are expressed in weakening of erection, up to impotence. Diagnosis of aortic bifurcation syndrome is based on a decrease in blood flow in the vessels of the lower extremities, which is determined by measuring blood pressure in this area and the strength of the pulse wave. To confirm the diagnosis, sphygmo- or rheovasography is performed. Without specialized treatment, the severity of the disease worsens.
Carotid artery division
Bifurcation is a phenomenon characteristic not only of the aorta, but also of the aorta. Its division occurs at the level of the lower edge. In this case, the right and left carotid arteries, despite significant differences in their length, are still divided into external and internal branches here.
As in the case of the aorta, such a bifurcation is a place of increased danger. The development of aneurysms and other pathological processes is also possible here due to the increased impact of blood flow in this area of the vessel. The outgoing arteries are approximately 2 times smaller in diameter compared to their “progenitor”. As a result, it is at the site of bifurcations that there is an increased risk of thrombosis and embolization. For this reason, in the case of the emergence of a corresponding clinic, doctors first examine the sites of division of the arteries, and only then their remaining sections.
Carotid artery stenosis (CAS): symptoms, treatment, life prognosis
Stenosis of the carotid arteries (ICD-10 code – I65) is a pathology caused by persistent narrowing of these vessels or their overlap (occlusion) under the influence of a number of internal causes.
The left and right common carotid arteries (CCA), which are large vessels carrying blood to the head, are divided into internal and external branches. They supply blood to the brain, eyes, soft tissues of the face, and the thyroid gland. Impaired blood flow leads to noticeable disruptions in the functioning of the organs supplied. Brain disorders are especially dangerous.
Stenosis usually affects both arteries, but on one side it can be more pronounced, causing pathological symptoms.
If you do not respond to the disease in time, the visual system and memory suffer, and most sensory processes are disrupted.
Stenosis is considered the main cause of ischemic stroke.
Reasons for narrowing
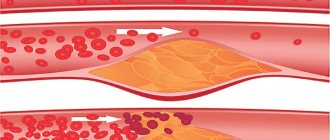
The main reason for the narrowing of the lumen of the carotid arteries is considered to be atherosclerotic lesions, expressed in the appearance of cholesterol plaques on their inner surface.
It is plaques formed in the area of the bifurcation of the carotid artery, or the mouth (division into external and internal branches), that most often become the cause of stenosis.
Other reasons include:
- Collagenosis caused by the proliferation of connective tissue.
- Inflammation of the vascular wall (arteritis) or its dissection.
- Congenital anomaly of the SA structure, the presence of pathological valves (pathology can manifest itself in both an adult and a child).
- Development of fibromuscular tissue dysplasia.
- Diseases accompanied by increased blood clotting.
The result of the above processes is a change in the direction of blood flow, increasing the risk of blood clots, which become harbingers of acute cerebrovascular accident.
The likelihood of negative symptoms increases if provoking factors are present:
- Diabetes.
- Violation of fat metabolism.
- Arterial hypertension.
- Injury to the vessels of the cervical spine.
- Elderly age.
- Long-term use of oral contraceptives.
- Smoking.
- Insufficient physical activity or physical inactivity.
Increased attention to one’s own health should also be present in the case of a hereditary predisposition to vascular pathology.
Symptoms and degrees of development
In the initial stage, narrowing of the carotid artery is asymptomatic: the quality of life and the usual rhythm are preserved. The disease begins to progress, and due to chronic oxygen starvation, brain structures begin to suffer, and neurological disorders develop.
This is indicated by a number of warning signs:
- Night sleep gets worse.
- Dizziness occurs periodically, headaches become more frequent (discomfort occurs on the right or left, depending on the side of the injury).
- There is inhibition in behavior. Perception of information and its reproduction occurs with difficulty.
- There is emotional instability.
Most of the listed signs are initially attributed to fatigue or considered as a manifestation of depression.
As a rule, the clinical picture described above is accompanied by occlusion of the right or left vessel by less than 50%. If further narrowing occurs, the condition is aggravated by transient ischemic attacks caused by a temporary disturbance of cerebral circulation.
Typical symptoms of attacks include:
- Headache.
- Slurred speech, difficulty perceiving information from the interlocutor.
- Uncoordinated movements, inability to perform usual everyday activities.
- Deterioration of vision, clouding of the “picture”, its blurriness.
- Feeling of numbness, tingling in the limbs.
- Difficulty swallowing.
- Sudden weakness up to loss of consciousness.
- Vomiting without precedent nausea.
The duration of the attack is determined by the degree of stenosis. Symptoms may persist for an hour, and over the next 24 hours the condition gradually recovers. Without treatment, ischemia worsens and stroke develops.
Classification of stenosis
One of the classification criteria is the prevalence of damage to the vascular walls. If the pathological area occupies no more than one and a half centimeters, then focal stenosing atherosclerosis is stated. With more extensive narrowing, ICA stenosis is diagnosed in its widespread form.
The main division occurs depending on the degree of narrowing of the lumen.
The following classification is generally accepted:
- I degree – characterized by an asymptomatic course without signs of cerebral ischemia. Diagnostic measures confirm clinically significant pathology of the head vessels. The narrowing of the lumen ranges from 30 to 50%.
- II degree - the patient suffers from transient ischemic attacks as a result of periodic cerebrovascular accidents. A focal neurological deficit is noted with elimination of negative symptoms over the next 24 hours. The lumen overlap is about 60-70%.
- III degree (hemodynamically significant process) – characterized by a chronic course of cerebrovascular insufficiency, the presence of severe neurological symptoms in the absence of a history of focal deficiency. The degree of blockage is up to 80%.
- Stage IV is a critical stage, diagnosed after a stroke with persistent focal neurological symptoms for 24 hours or longer. Vessel obstruction is up to 90%.
Only an experienced doctor can determine a developing disease at the initial stage. The first sign is an uncharacteristic murmur over the artery, detected during routine auscultation. If a vascular disorder is suspected, a set of examinations is prescribed, consisting of ultrasound of the cervical vessels with Doppler ultrasound, tomography (MRI or CT), and angiography.
Treatment methods
Therapeutic measures to restore the health of clogged carotid arteries are developed by a neurologist with the participation of a therapist, since simultaneous elimination of cerebral and somatic disorders is required.
Additionally, consultations with a cardiologist and angiosurgeon are prescribed. The latter, if necessary, plans surgical treatment, without which it is impossible to effectively treat severe stenosis.
Qualitative elimination of negative symptoms and restoration of quality of life is possible if a stroke has not occurred. Surgical intervention is prescribed for stenosis over 60%.
Without a radical approach, improvement in the condition is possible by no more than 30%.
For this reason, doctors first restore the patency of the vessel and only after that move on to measures that affect the cause of the stenosis.
Surgery
Radical therapy is indicated in the following cases:
- Narrowing of the lumen by more than 60% even without obvious clinical symptoms.
- Stroke suffered as a result of CA stenosis.
- Regular transient ischemic attacks even with 50% damage to the SA.
The table shows common operation options and their features:
| Method | Features of the intervention | Result |
| Carotid endarterectomy | Under general anesthesia, after incising the vessel, the pathological formation is removed, vascular grafting is performed and the incision site is sutured | Complete removal of a blood clot or atherosclerotic plaque |
| Carotid angioplasty, stenting | After widening the lumen of the vessel using a balloon catheter, a stent is inserted into the narrowed area. The operation requires local anesthesia and continuous monitoring of pulse and blood pressure. The intervention is carried out under x-ray control | Effective increase in lumen, prevention of the formation of atherosclerotic plaques in the area of stenosis |
| Arterial prosthetics | Practiced for extensive vascular lesions, replacing part of the wall with a special prosthesis | Renewal of the affected area |
As part of carotid endarterectomy, if necessary, it is planned to restore the geometry of the carotid artery. The technique is used for congenital anomalies of the SA structure. After removing the loop-shaped or bent segment, the vessel is straightened. The result is the elimination of deformations, including crimps and kinks.
Rehabilitation after surgical treatment lasts differently for each patient. If stenting was performed, hospital stay is limited to 2-3 days. With endarterectomy, this period increases to a week. Before discharge, the patient's skin sutures are removed.
If pain occurs in the operated area, short-term application of ice is allowed. Showering is allowed on the third day after surgery, taking a bath is only after 14 days.
Contraindications for intervention are:
- Development of Alzheimer's disease.
- Heart failure of 2-3 degrees, unstable angina.
- Recent myocardial infarction or major stroke.
- Detection of metastatic tumor.
- Intolerance to drugs used as part of the intervention.
It is important to take into account a number of complications that may occur in the postoperative period:
- Development of vascular thrombosis, stroke.
- Bleeding in the operated area.
The chosen method of surgical treatment determines its cost.
On average, amounts vary within the following limits:
- Carotid endarterectomy – from 30 to 50 thousand rubles.
- Stenting is an expensive procedure that will cost 200-280 thousand rubles.
Even after the intervention, the diagnosis means the need for a complete revision of the usual lifestyle. After recovery, you need to give up bad habits, correct dosage of physical activity with the addition of massage, and correction of your diet by creating a diet.
Drug treatment
It is performed for low degrees of stenosis, after an intervention to prevent deterioration, or as the main therapeutic measure if there are contraindications for surgery.
Effective therapy is possible using a combination of the following drugs:
| Pharmacological group | Action | Available funds |
| Antiplatelet agents | Blood thinning |
|
| Antithrombotic agents | Preventing the formation of blood clots, dissolving existing pathological structures |
|
| Statins providing a lipid-lowering effect | Reducing cholesterol levels |
|
| Antihypertensive drugs | Blood pressure correction | The type of drug and the appropriateness of its use are determined by the attending physician. |
The use of medications to detect carotid artery stenosis is indicated throughout life.
Therapeutic diet
Due to the high risk of re-formation of plaques, drug therapy must be combined with a dietary diet, the goal of which is to reduce the level of cholesterol entering the body.
When planning the menu, make the following amendments:
- It is allowed to consume only lean varieties of fish, meat, and low-fat fermented milk products.
- Butter is replaced with a vegetable product.
- Eat seasonal fruits and vegetables in sufficient quantities.
- Minimize the consumption of confectionery products and offal.
- Dishes are prepared using boiling or steaming modes.
- The number of meals per day is 4-5 times with small portions. Dinner is planned no later than 3 hours before bedtime.
It is advisable to measure the calorie content of prepared foods. The optimal daily intake is from 1500 to 2000 kcal. When calculating, be sure to take into account individual characteristics - height, weight, activity level. After calculation, the resulting value is reduced by 15%.
Bifurcation of the main airway
The trachea is a hollow organ that is responsible for conducting air to the bronchi and further to the lungs. Its structure contains a large number (up to 26) cartilaginous rings that do not allow the trachea to collapse.
Tracheal bifurcation occurs at the level of the upper edge of the V thoracic vertebra. In children it is located slightly higher. In addition, when inhaling, the level of the bifurcation shifts approximately 2-3 cm down. Here this large airway divides into the right and left main bronchi. Subsequently, they themselves are crushed many times. The main purpose of tracheal bifurcation is to split one large airway into 2 smaller ones. This is necessary to supply oxygen to both lungs at once. The bifurcation of the trachea occurs at an angle of approximately 70 o. When inhaling, this figure may increase slightly.
Anatomy of the vessels of the neck and head
The ASG, left CCA and RCA emerge from the aortic arch. At the level of the right sternoclavicular joint, the ASG is divided into the right CCA and RCA.
The RCA lies in an arc on the dome of the pleura, passes between the anterior and middle scalene muscles, and dives from under the collarbone into the armpit.
PKA branches:
- I segment to the scalene muscle - vertebral, thyroid-cervical, internal thoracic artery;
- II segment in the interscalene canal - costocervical trunk;
- The third segment at the exit from the interscalene canal is the transverse artery of the neck.
Click on pictures to enlarge.
The OCA passes behind the sternocleidomastoid muscle. The CCA has no branches; at the upper edge of the thyroid cartilage it is divided into the ECA and the ICA.
The expansion of the bifurcation (bulb) contains chemo- and baroreceptors that regulate the functioning of breathing, heart and blood vessels.
The ECA begins medially, then runs outward from the ICA; has a short trunk; near the angle of the lower jaw it divides into eight branches.
Branches of the ECA: superior thyroid, lingual, facial, ascending pharyngeal, occipital, posterior auricular, maxillary, superficial temporal.
The BSA is wider than the NSA; on the neck it rises between the pharynx and the IJV, does not give branches; passes into the cranial cavity through the canal of the pyramid of the temporal bone.
In the skull, the branches of the ICA are the ophthalmic, anterior cerebral, middle cerebral, and posterior connective; maxillary artery - middle meningeal.
The VA departs from the first segment of the RCA, ascends through the openings of the transverse processes C6-C1, and enters the skull through the foramen magnum.
The PAs of both sides merge into the main artery at the posterior edge of the bridge; The basilar artery divides into the posterior cerebral artery at the anterior edge of the pons.
I segment from the mouth to C6; II segment in the canal of the transverse processes C6-C2; III segment from C2 to the entrance to the skull; IV segment before merging into the basilar artery.
The ICA and VA form an arterial circle at the base of the brain with the help of the anterior and posterior communicating arteries; more often one of the branches is missing.
Diagnosis and treatment of pathology
To identify negative changes in vessel bifurcation, you need to undergo a medical examination:
- angiography – contrast X-ray examination of blood vessels;
- flowmetry (ultrasound and electromagnetic) – quantitative determination of blood flow in large vessels;
- segmental volumetric sphygmography – measurement of pulse fluctuations of the vascular walls;
- longitudinal segmental rheography – assessment of regional hemodynamics.
The most effective method of surgical intervention on the bifurcation of the carotid artery is considered to be endarterectomy with plastic surgery of the internal carotid artery with a patch and installation of a stent. When choosing a patch, the mechanical properties of its material are taken into account. The stent significantly affects the condition of the vascular wall and improves hemodynamics.
The right common carotid artery (a. carotis communis dextra) arises from the brachiocephalic trunk (thruncus brachiocephalicus), and the left common carotid artery (a. carotis communis sinistra) arises from the aortic arch. In this regard, the left common carotid artery turns out to be 2.5-3 cm longer than the right one. At the level of the sternoclavicular joints, the common carotid arteries exit to the neck. In the neck, the arteries are located in a large interfascial gap, which is delimited on the medial side by the trachea and esophagus, behind by the prevertebral fascia and the anterior scalene muscle (m. scalenus anterior), laterally and in front by the sternocleidomastoid muscle (m. sternocleidomastoideus) .
In the neck, the common carotid arteries pass as part of a neurovascular bundle, which includes, in addition to the common carotid artery, the internal jugular vein (v. jugularis interna), the vagus nerve (n. vagus). The parietal layer of the fourth fascia of the neck forms a sheath for the neurovascular bundle, which connects to the transverse processes of the vertebrae. The sheath of the neurovascular bundle begins at the level of the upper edge of the anterior mediastinum and reaches the base of the skull. Inside the vagina there are connective tissue septa separating the artery, vein and nerve. As a result, each of the beam elements has its own fascial sheath. The vagus nerve passes through the tissue of the vascular bed between the fascial sheaths of the artery and vein. Adjacent to the posterior wall of the vascular bed is the border sympathetic trunk, separated from it by the prevertebral fascia (fascia praevertebralis).
As a rule, the common carotid artery does not give branches, but in some cases (especially with a high version of the bifurcation), the superior thyroid artery (a. thyreoidea superior) can depart from its upper part - 0.2-1.5 cm below the bifurcation.
At the level of the upper edge of the thyroid cartilage, the common carotid artery is divided into two branches: the internal and external carotid arteries (a. carotis interna et a. carotis externa). Less commonly, the bifurcation of the common carotid artery has a higher or lower location and is located at the level of the III, IV or VI cervical vertebrae. The division angle of the common carotid artery ranges from 2 to 74°. The bifurcation of the common carotid artery can be located in the frontal or sagittal planes or in a plane close to them.
In the area of bifurcation, the common carotid artery forms an ampulla-shaped extension, the so-called carotid sinus (bulbus caroticus, sinus caroticus). The carotid sinus contains pressoreceptors: irritation of the nerve endings of the carotid sinus reduces blood pressure and slows down heart contractions.
Here, in the area of bifurcation of the common carotid artery, on its posteromedial surface at the origin of the internal carotid artery, there is the carotid glomus (glomus caroticum) (carotid gland, intercarotid tangle). It is a small flat formation 2.5 mm long and 1.5 mm thick, firmly connected to the wall of the vessel by connective tissue. According to its function, the carotid glomus is a specific sensory organ containing vascular chemoreceptors that respond to changes in the chemical composition of the blood and thereby participate in the regulation of the activity of the cardiovascular system.
Nerves from the glossopharyngeal nerve (n. glossopharyngeus), the vagus nerve and the sympathetic trunk approach the carotid sinus and carotid glomus. The branch of the glossopharyngeal nerve to the carotid sinus is called the sinus nerve. There are numerous connections between these nerves. The depressor nerve of Zion also branches in the same area. Together, the carotid sinus and carotid bodies, together with the nerves approaching them, form a reflexogenic zone, which plays an important role in the regulation of blood circulation.
Above the bifurcation of the common carotid artery, the internal carotid artery deviates laterally and posteriorly and passes in the paravertebral tissue to the external opening of the carotid canal (foramen caroticum externum). The external carotid artery runs inward and upward, with a slight turn to the medial side.
The internal carotid artery (a. carotis interna) is the largest branch of the common carotid artery in diameter. The internal carotid artery is usually divided into two sections: cervical and intracranial. In the intracranial section of the internal carotid artery, intraosseous, cavernous and intradural parts are distinguished.
The cervical part of the internal carotid artery does not give branches. Through the external opening of the carotid canal, the internal carotid artery penetrates the carotid canal (canalis caroticum) and through its internal opening enters the cranial cavity. Directly at the exit from the carotid canal, the internal carotid artery is surrounded by the cavernous venous sinus (sinus cavernosus). After leaving the carotid canal, the internal carotid artery makes an S-shaped bend (siphon) and passes through the dura mater into the subdural space behind the internal opening of the optic canal, lateral to the optic nerve. The ophthalmic artery (a. ophthalmica) originates from the convex part of the bend of the internal carotid artery. At the entrance to the subdural space, the internal carotid artery at the inner edge of the anterior sphenoid process is divided into two branches: the anterior cerebral artery (a. cerebri anterior) and the middle cerebral artery (a. cerebri media). The length of the cervical part of the internal carotid artery in an adult is 10-11 cm, the intraosseous part is 4-5 cm, the cavernous part is 5 cm, and the intradural part is 1 cm.
The external carotid artery is the second branch of the common carotid artery, which has a smaller diameter compared to the internal carotid artery. However, its diameter in the initial part may be greater than the diameter of the internal carotid artery. The external carotid artery gives off 9 branches, including 6 branches below the posterior belly of the digastric muscle (m. digastricus) and three branches above this muscle. At or above the bifurcation, the superior thyroid artery arises from the external carotid artery. Above the horn of the hyoid bone, the lingual artery (a. lingualis) and the facial artery (a. facialis) extend anteriorly from the artery, and the occipital artery (a. occipitalis) extends posteriorly. Distally, the posterior auricular artery (a. auricularis posterior) and the sternocleidomastoid artery (a. sternocleidomastoidea) originate. In the initial part of the external carotid artery or slightly higher, the ascending pharyngeal artery (a. pharyngea ascendens) departs. At the level of the neck of the lower jaw, the external carotid artery is divided into two terminal branches - the maxillary artery (a. maxillaris) and the superficial temporal artery (a. temporalis superficialis).
The carotid arteries have a complex relationship with surrounding structures. Thus, the section of the left common carotid artery, located in the thoracic cavity, borders in front with the left brachiocephalic vein (v. brachiocephalica sinistra). Lateral and posterior to it runs the subclavian artery (a. subclavia), adjacent to the mediastinal layer of the pleura. The trachea is located medial, higher and somewhat posterior to this section of the artery.
In the neck, the common carotid artery is covered anteriorly by the anterior edge of the sternocleidomastoid muscle. However, a variant of anatomical development is also possible in which the sternocleidomastoid muscle covers only the lower third of the common carotid artery or does not cover it at all. Between this muscle and the artery in the lower part of the neck pass the upper belly of the scapular-hyoid muscle (m. omohyoideus), the sternothyroid muscle (m. sternohyoideus) and the sternohyoid muscle (m. sternohyoideus).
Along the anterior wall of the artery, over its vagina, the lower branch of the cervical loop runs in an oblique direction - radix inferior ansae cervicalis, formed by the anterior branches of the I-III cervical nerves. The lower branch of the cervical loop connects with the upper branch (radix superior) of the cervical loop, extending from the hypoglossal nerve, which leads to the formation of ansae cervicalis.
In its middle third (before the bifurcation), the common carotid artery is covered in front only by fascia. Somewhat below the bifurcation of the artery, the common facial vein (v. facialis communis) and the superior thyroid vein (v. thyreoidea superior) pass along its anterior surface, flowing through a common mouth or separately into the internal jugular vein (v. jugularis interna).
Posteriorly, the common carotid artery is adjacent to the prevertebral fascia. Behind it are the anterior and middle scalene muscles (m. scalenus anterior et medius), the long colli muscle (m. longus colli), as well as the sympathetic trunk.
In the lower part of the neck, the common carotid artery lies in front of the vertebral artery (a. vertebralis), which enters the opening of the transverse process of the VI cervical vertebra. Behind the common carotid artery, at the entry point of the vertebral artery into the opening of the transverse process, passes the inferior thyroid artery (a. thyreoidea inferior), which is a branch of the thyrocervical trunk (truncus thyreocervicalis). On the left, behind the common carotid artery, slightly below the origin of the inferior thyroid artery, the thoracic lymphatic duct (ductus thoracicus) passes, flowing into the confluence of the left subclavian and internal jugular veins (venous angle).
Medial to the common carotid artery is the lobe of the thyroid gland, which separates the artery from the cervical esophagus and trachea.
The bifurcation area of the common carotid artery on the medial side is adjacent to the larynx behind the middle scalene muscle (m. scalenus medius). The internal jugular vein (v. jugularis interna) runs lateral and slightly anterior to the bifurcation. The vagus nerve runs along the lateral surface of the artery. Next, the artery passes under the styloid process and m. stylopharyngeus to the external opening of the carotid canal.
Below the posterior belly of the digastric muscle, the artery is covered by the anterior edge of m. sternocleidomastoideus. In the interval from the lower edge of the posterior belly of the digastric muscle to the bifurcation area of the common carotid artery, the anterior surface of the internal carotid artery is crossed by the hypoglossal nerve (n. hypoglossus), the sternocleidomastoid artery, the occipital artery, and above - the posterior auricular artery.
Under the stylohyoid muscle and on the anterior surface of the internal carotid artery lies the glossopharyngeus nerve (p. glossopharyngeus).
In the space between the hypoglossal and glossopharyngeal nerves, in front of the internal carotid artery, is the pharyngeal plexus, consisting of sensory (from the glossopharyngeal nerve), motor (from the vagus nerve) and autonomic (from the sympathetic trunk and vagus nerve) fibers.
Between the initial part of the posterior belly of the digastric muscle and the upper part of the sternocleidomastoid muscle along the anterior surface of the internal carotid artery there is a trunk of the facial nerve (n. facialis). The marginal branch of the mandible (ramus marginalis mandibulae) extends from it towards the lower jaw.
Adjacent to the posterior wall of the internal carotid artery, 1-2 cm above its mouth, crossing the artery, is a branch of the vagus nerve - the superior laryngeal nerve (n. laryngeus superius). Its position varies: the nerve can pass behind the common carotid artery, and sometimes crosses the internal carotid artery high at the level of the pharyngeal nerve plexus.
In front, the internal carotid artery is crossed by many veins of different calibers, flowing into the internal jugular vein.
At the level of the II and, partially, III cervical vertebrae behind the internal carotid artery and medial to the vagus nerve lies the superior cervical sympathetic ganglion (ganglion cervicale superior). The branches of the upper part of the node (n. carotis internus) form plexuses around the internal carotid artery (plexus caroticus internus and plexus cavernosus), which spread along the artery into the cranial cavity.
— We recommend that you further read the article “
Access to the carotid arteries. Selection"
In anatomy, the left and right common carotid arteries (carotid arteries) (English: /kərɒtɪd/) are the arteries that supply the head and neck with oxygenated blood; they divide in the neck to form the external and internal carotid arteries.
Doppler ultrasound of head and neck vessels
Assessment of cerebral blood flow includes the brachiocephalic arteries at the level of the neck and the intracranial vessels of the brain.
They use a 3-5 MHz convex or sector sensor, as well as a 7-18 MHz linear sensor.
Lying on your back, neck extended, head slightly turned in the opposite direction. There are 5 minutes of rest before the test.
Three approaches to the arteries of the neck: anterior - in front of the sternocleidomastoid muscle, lateral - along the CM, posterior - behind the CM.
In B-mode and CDC, the CCA is scanned up to the bifurcation; above the bifurcation, the ECA is examined through an anterior approach, and the ICA through a lateral approach.
Using a 3-5 MHz convex or sector sensor, the course of the arteries emanating from the aortic arch is examined - PGS, RCA, CCA, ECA and ICA to the entrance to the skull, as well as VA from the mouth to the entrance to the skull.
The course of the vessels is normally rectilinear, but there is tortuosity - C-, S- bends, loops. Up to 12 years of age, disruption of the course can be considered as a reserve of vessel length necessary during the period of intensive growth.
A 7-18 MHz linear sensor is used to examine arterial walls and the Doppler spectrum.
Thickness of the intima-media complex on ultrasound
The vessel wall is examined with a 7-18 MHz linear sensor. When the ultrasound beam is directed at 90°, the reflection and contrast of the image are maximum.
IMTs comprise the intima and media of the vascular wall. The adventitia merges with the surrounding tissues. IMT of the CCA and ICA is measured 1 cm below and above the bifurcation.
The intima is represented by endothelium and subendothelium; media - in the CCA there is predominantly elastic stroma, in the ICA with a pronounced muscle component.
IMT is better visible on the distant wall - an anechoic media between the hyperechoic intima and adventitia. Normally 0.5-0.8 mm, in older people 1.0-1.1 mm.
In M-mode, the diameter of the vessel is measured between the intima and adventitia in systole and diastole.
Duplex scanning of neck and head vessels
The distal part of the PGS, RCA, CCA along its entire length, ICA from the mouth to the entrance to the skull, ECA in the initial segment, VA in segments V1 and V2 are assessed.
To study the PGS, the sensor is placed in the jugular notch, and the beam is directed to the right. The ASG is divided into the right RCA and CCA. The ostium of the left CCA and RCA is too deep to see.
RCA segment I is examined above the sternoclavicular joint, segment II - above the clavicle, the beam is directed downwards, segment III - under the clavicle.
To study the CCA, the sensor is placed along the outer or inner edge of the sternocleidomastoid muscle. The CCA is assessed along its entire length from the mouth to the bifurcation.
At the base of the neck, inward from the CCA is the thyroid gland, outward is the internal jugular vein. Under the pressure of the sensor, the IJV is compressed, but the CCA is not.
From the base of the neck, move the sensor upward to the bifurcation of the CCA - the site of division into the ECA and ICA. There is a small extension here - an onion.
At the bifurcation of the CCA, the bulb expands, the bare trunk of the ICA and the branching ECA begin. The first branch of the ECA is the superior thyroid artery.
At the bifurcation level, the ICA is wider than the ECA; located outward and posterior to the ECA, above it moves inward; has no branches on the neck.
In the bulb, the laminar flow along the main axis of the ICA is red, and the turbulent flow zone at the outer wall is colored blue.
Outside the bulb there is a nerve plexus and carotid body. In rare cases, a tumor of the carotid body occurs.
The difference between the ECA and the ICA: at the bifurcation level, in 95% of cases the ECA is located medially; the diameter of the ESA is smaller; Small branches extend from the ECA on the neck.
The PA is scanned longitudinally inwards from the sternocleidomastoid muscle, from the angle of the lower jaw to the upper edge of the clavicle.
PA is characterized by asymmetry, usually the left is larger than the right. When PA is less than 2 mm, we can talk about hypoplasia.
To study the first segment of the VA, the sensor is moved to the clavicle. Normally, the VA leaves the RCA at the level of C7 and enters the bony canal at the level of C6.
Options are possible: the left VA arises from the aortic arch and enters the bony canal at the C5 level.
II segment of the PA has an intermittent appearance, because passes in the bone canal of the transverse processes C6-C2 and acoustic shadowing occurs at the site of the transverse processes.
If the blood flow speed is approximately the same in adjacent areas, then there are no pathological changes in the “blind” zone.
For PA segment III, a convex sensor may be useful; Due to physiological deformation, it is impossible to correctly assess blood flow.
For segment IV, the VA is examined with a 1.5-2.5 MHz sector sensor through the foramen magnum with the patient in the prone position.
Triplex scanning of neck and head vessels
Read the basics of triplex scanning. For normal indicators in the vessels of the neck and head in adults and children, see.
The CCA spectrum has a sharp rise and a narrow peak in systole, a low flow in diastole, and a dicrotic notch in late systole and early diastole.
The spectrum of ESA is similar to OSA, sometimes there is a retrograde flow in diastole, a “shooting” sound. Tap the superficial temporal artery and you will see T-waves on the ECA spectrum.
The ICA spectrum has a gradual rise and a wide peak in systole, a high antegrade flow in diastole, almost no pulsation, and a “blowing” sound.
The spectrum of segment II of the VA is similar in shape to the ICA, Vps and Ved are 1.5 times lower, the flow is exclusively antegrade. Vps may decrease in the upper sections, but not more than 20%.
The VAs of both sides have the same lumen only in 26-44% of cases, velocity asymmetry is often determined, in healthy
The ICA and VA carefully nourish the brain, the physiological deformation in the III segment of the arteries smoothes out the pulsation.
In the CCA and ECA there is high resistance, low flow in diastole; in the ICA and VA there is low resistance, high flow in diastole.
Blood flow velocities and indices are compared with normal values. On the vessels of both sides, the asymmetry of Vps should not exceed 20%, RI and PI indices - 10%.
Take care of yourself, Your Diagnosticer
!
The carotid arteries are the most important vessels that provide blood flow to the brain structures and are responsible for the blood supply to most of the cerebral hemispheres. A person has two carotid arteries located in the neck, on the right and on the left.
A phenomenon such as partial narrowing of an artery – stenosis or its complete blockage – occlusion is often noted. Carotid artery stenosis leads to circulatory problems, impaired brain activity, and also increases the risk of ischemic stroke.
Complete blockage of this important vessel leads to a number of severe consequences and can also cause instant death of the patient.
Carotid bifurcation
I. Branches of the aorta and proximal arteries:
a) Intracerebral stealing phenomenon
. Stenosis or occlusion of the brachial artery (right) or subclavian artery (left) causes return flow from the opposite VA.
Patients develop signs of vertebrobasilar insufficiency with dizziness, usually worsening with increased physical activity of the ipsilateral upper limb. 1. Diagnostics. Dopplerography and DSA can be used for diagnosis. The return blood flow of the opposite VA is recorded. 2. Indications.
Empirical, individual. 3. Treatment. Stenting of the trunk of the brachial or subclavian artery is sometimes possible even with occlusion of the vessel. One surgical option is carotid-subclavian anastomosis.
4. Complications.
With endovascular treatment, complications are minimal (dissection, arterial thrombosis with possible stroke), and in the case of surgery, complications include damage to surrounding structures (nerves, lymphatic ducts) and vascular/shunt occlusion.
b) Thoracic outlet syndrome
. External compression of the subclavian artery and/or brachial plexus causes decreased blood flow to the upper extremity, pain, and, less commonly, symptoms of brachial plexus compression.
Compression may be caused by the cervical ribs, scalene muscles, etc. 1. Diagnosis. Planned radiography, DSA, ultrasound. 2. Indications. Empirical, individual. 3. Treatment. Removing pressure by resection of the cervical rib, dissection of the scalene muscle, etc.
4.
Complications. Injuries to surrounding structures (nerves, lymphatic duct).
II. Carotid bifurcation/internal carotid artery stenosis
(
BCA
). The most typical sites of atherosclerotic lesions. Carotid endarterectomy (CE) is the third most common surgical procedure.
Atherosclerotic plaque causes stenosis, but clinical symptoms are caused by plaque fragmentation and/or blood aggregation on the plaque surface and distal embolization.
Hemodynamic origin of symptoms is extremely rare.
CE is a means of secondary prevention, and surgery is considered in the asymptomatic stage and in patients with transient deficiency or after minor stroke. Patients after a major stroke are candidates for surgical treatment much less often.
1. Diagnostics. Ultrasound, CTA, MRA and DSA.
2. Indications. Indications for treatment are based on data from large clinical multicenter randomized trials (NASCET, ECST, ACAS, ACST).
3. Recommendations of the American Heart Association. Surgery is indicated in symptomatic patients with a stenosis greater than 50%, an initial MM level of less than 6%, and a life expectancy of at least five years.
Asymptomatic patients with stenosis greater than 60% have an MM below 3% and an average life expectancy of at least five years.
In symptomatic patients, surgery should not be delayed (the best outcome was observed in patients who underwent surgery within two weeks of the last episode of ischemia) unless there are serious myocardial changes.
If they are present, the operation may be delayed for six weeks. The same criteria apply for carotid stenting (with distal protection). CE is superior to stenting in terms of reliability. Stenting should be considered as a treatment option in poor or elderly patients.
4. Treatment. Endarterectomy can be performed under general or regional anesthesia. It is necessary to closely monitor the neurological status (EEG, brainstem evoked potentials). Stenting is performed under local anesthesia and/or mild sedation.
A skin incision is made along the anterior border of the sternocleidomastoid muscle, the carotid artery bifurcation is dissected, the vessels are temporarily occluded, and the plaque is removed from the vessel. The use of an intraluminal shunt depends on the clinical protocol adopted in the range of “always-never”.
The plaque is removed. The main focus is on the distal end of the carotid artery, where the intima should be carefully checked and, if necessary, a suture should be placed to prevent dissection. The arteriotomy is sutured either directly or using a graft.
5. Restenosis. Restenosis occurs in 5% of patients. If necessary, restenosis is prevented by stenting.
6. Complications. Stroke, carotid artery occlusion, dissection, postoperative hematoma, peripheral nerve damage, cranial nerve injuries (VII, X, XII) and infections.
III. Carotid pseudoocclusion
. In some cases, the ICA does not thrombose, but its lumen decreases. Remnants of the lumen can be detected on DSA. 1. Diagnostics. DSA. 2. Indications. CE may be recommended.
3. Treatment. Standard FE.
4. Complications. Stroke, carotid artery occlusion, carotid artery dissection, postoperative hematoma, peripheral nerve injury, cranial nerve injuries (VII, X, XII) and monocular blindness.
IV. Carotid kinking and pathological tortuosity
. There are two types of carotid artery tortuosity. The first type probably arises on the basis of hereditary elongation of blood vessels; the second is observed in patients with atherosclerosis.
Symptoms (usually TIA) are due to either embolism or the hemodynamic effect of vessel occlusion during ipsilateral head rotation. Surgery is usually only indicated for patients in whom conservative treatment (TCM) fails to prevent further TIAs. 1. Diagnostics.
Ultrasound, CTA, MRA and DSA. 2. Indications. Empirical, individual. 3. Treatment. The bifurcation of the carotid artery is highlighted, the mobilized vessels with slight tortuosity are placed down and fixed to the surrounding structures.
If wider loops are present, the affected vessel segments are removed and the distal stump is either sutured end-to-end or sutured to the CCA. In the case of pathological tortuosity, the surgical approach is the same. Both procedures can be performed during routine CE.
4. Complications.
Stroke, carotid artery occlusion, dissection, postoperative hematoma, peripheral nerve injury, cranial nerve injuries (VII, X, XII), and infections.
V. Stump syndrome
. Emboli from the carotid artery stump can pass through natural or artificial (EICMA) anastomoses and enter either the retina or the cerebral vessels, resulting in blindness or TIA. The decision to operate is made only in case of repeated attacks and lack of response to TDC. 1.
Diagnostics. Ultrasound, CTA, MRA and DSA. 2. Indications. Empirical, individual. 3. Treatment. The bifurcation of the carotid artery is dissected and arteriotomy of the CCA and ECA is performed. After endarterectomy, the area of ICA occlusion is closed with a continuous suture.
Blood flow through the ICA can be restored in some cases, even if the vessel is thrombosed. If the reverse blood flow reaches the carotid artery canal, recanalization can be attempted. The Fogarty catheter is advanced into the carotid canal and inflated. The clot is removed by gently pulling on the catheter.
4.
Complications. Damage to peripheral nerves (VII, X, XII), stroke, infection, monocular blindness.
VI. Extracranial section of the vertebral arteries
:
a) Narrowing of the origin of the vertebral artery (VA)
. The origin of the vertebral artery (VA) is a typical location of its stenosis. Stenosis usually manifests itself as symptoms of VA insufficiency (dizziness, etc.). In addition, you can see symptoms of damage to the PCA (hemianopsia of the same name).
VA stenosis is also often encountered during examination for ischemic symptoms of the ICA region. One can also suspect a hemodynamic origin of symptoms in some patients, for example, with aplasia or hypoplasia of the opposite VA and insufficiently developed collaterals. 1. Diagnostics. Ultrasound, CTA, MRA and DSA. 2. Indications.
Empirical, individual; It is believed that treatment is necessary only for high degrees of stenosis. 3. Treatment. The endovascular approach is the first line of therapy. Stenting may be performed, but simple percutaneous transluminal angioplasty is preferred. In addition, PA-OCA anastomosis can be used.
Approach to the vessels through an incision in the lower half of the anterior border of the sternocleidomastoid muscle. The VA is divided at the origin and sutured to the CCA. Particular care is taken with respect to the recurrent nerve and lymphatic vessels (left side).
4. Complications.
With endovascular treatment, the number of complications is minimal (artery dissection, arterial thrombosis), while with open surgery, damage to surrounding structures (nerves, lymphatic pathways), occlusion of the shunt and vessel occurs.
b) Narrowing of the middle segment of the vertebral artery (VA)
(C2-C6). The symptoms are similar to those described above. The cause may also be external compression of the VA caused by hypertrophy of the uncovertebral joints in patients with degenerative diseases of the spine, or there may be a kink between the two holes. 1. Diagnostics.
Ultrasound, CTA, MRA and DSA. 2. Indications. Individual. 3. Treatment. Vertebral artery (VA) decompression can be achieved using routine anterior discectomy in patients with uncovertebral osteophytes. The preferred approach, however, is lateral.
Access the spine either anteriorly or posteriorly to the sternocleidomastoid muscle, posterior to the carotid artery and jugular vein. Osteophytes can be selectively removed, the VA is opened to the desired length (by moving two adjacent holes apart and accessing the VA for 40-50 mm) for tortuous resection or straightening. Atherosclerotic changes in this area are extremely rare.
If necessary, endovascular treatment is performed.
4. Complications. Root injury, thrombosis, embolism.
c) Narrowing of the upper segment of the vertebral artery
(PA) (from C2 to the PA confluence). In this area, atherosclerotic lesions are most common. For symptomatic lesions, the possibility of endovascular or surgical treatment is determined. 1.
Diagnostics. Ultrasound, CTA, MRA and DSA. 2. Indications. Rare and strictly individual.
3. Treatment.
Endarterectomy is not performed; Previously, bypass anastomoses (OSA-PA) were more often performed, but they have now been replaced by endovascular interventions (angioplasty, stenting).
d) Archer syndrome
. When the head is rotated to the maximum (as in archery), the contralateral VA is stretched and thus stenotic or occluded. In rare cases, with hypoplastic or aplastic opposite VA and insufficiently developed collaterals, PA-PCA ischemia can be detected.
These symptoms may be temporary or permanent (hemianopsia). Several deaths have been described. 1. Diagnostics. DSA without and with maximum head rotation. 2. Indications. Individual. 3. Treatment. Treatment involves fixation of C1-C2 or PA.
In case of compression of the VA, the formed bone C1 vertebral foramen is excised, and the VA is freed from the surrounding structures.
4. Complications. Injury to surrounding nerve structures.
VII. Direct revascularization
:
a) EICMA
. An end-to-side anastomosis between the donor (superficial temporal artery) and the acceptor (opercular branch of the MCA) provides approximately 18 ml/min. blood.
The ECIC International Collaborative Study Group failed to demonstrate the benefit of bypass for stroke prevention (especially in patients with MCA stenosis). - Indications. ICA/MCA aneurysms or tumors that are incurable by other methods. – Relative indications.
Occlusion of the ICA/MCA in patients with impaired cerebrovascular power reserve (proven by SPECT, PET, perfusion CT) and absent/small ischemic damage. - Diagnostics. Clinically, DSA, CT/MRI and determination of cerebrovascular power reserve. - Surgery.
A branch of the superficial temporal artery is identified. The center of a small craniotomy is a point 6 cm above the tragus, the dura mater is dissected in a Y-shape.
The acceptor artery is isolated, a linear arteriotomy is made between the two temporary clips, and both vessels are sutured end-to-side using 10/0 suture material.
Particular care must be taken to close the wound to avoid cerebrospinal fluid leakage, vascular distortion, or excessive pressure from the bone flap.
b) Anastomosis using venous/arterial insert
. In the case of an insufficiently developed superficial temporal artery, arterial and venous grafts are used to create a bypass anastomosis between the CCA/ECA and the intracranial ICA or proximal MCA. For occlusive diseases, this operation is rarely used, as there is a risk of rupture.
c) Anastomoses in the posterior circulation
. Anastomoses of the posterior circulation are performed in cases of ischemia in the VBB.
They consist of an anastomosis between the superficial temporal and superior cerebellar arteries, and between the superficial temporal/occipital arteries and the posterior inferior cerebellar artery. - Diagnostics.
Clinical data, DSA, CT/MRI, determination of cerebrovascular power reserve.
- Indications. Rare and individual, recently it is often replaced by endovascular angioplasty and stenting.
d) ICA-ICA anastomosis
. This is mainly an anastomosis between the ACA, for example, with a fusiform aneurysm of the A2 segment. - Indications. Indications are individual.
Many options have been described, with low- and high-flow anastomosis (for example, ELANA technique). To date, no randomized trial has demonstrated benefit from anastomosis in any subgroup of patients.
- Complications.
Stroke, hyperperfusion complications and wound healing problems.
VIII. Indirect revascularization
:
a) Encephaloduroarteriomyosynangiosis
.
Encephaloduroarteriomyosyangiosis ( EDAMS
) and its variations (EMS, EDAS) consist of laying an isolated temporalis muscle with unidentified branches of the superficial artery on the surface of the brain with open vessels.
Neovascularization with the development of ECA-ICA collaterals in moya-moya disease can be proven by angiography. - Indications. Individual, basically - the disease is mine, mine.
- Complications. Infections, long wound healing.
You can download this video and view it from another video hosting site on the page: Here.
– We also recommend “
Algorithm for the treatment of cerebrovascular diseases - European recommendations”
Table of contents of the topic “Cerebral vascular diseases.”:
Characteristics of the disease
Stenosis is a disease of the cardiovascular system, characterized by partial narrowing of the lumen of a vessel. This is fraught with the possibility of its subsequent complete closure (occlusion).
The left common and right carotid arteries are located in front of the transverse processes of the cervical vertebrae. Each of them is divided into an internal artery and an external one.
When stenosis develops, brain tissue experiences oxygen starvation, and the vital processes of cells are disrupted. Blockage of blood flow to the brain leads to ischemic stroke and death.
Men are more prone to developing this pathology.
The danger of arterial stenosis is the asymptomatic period of the initial stage, when the lumen of the vessel is slightly narrowed. It can last more than a year, and the patient does not even suspect the presence of such a pathology.
Treatment of blocked carotid artery
Before prescribing treatment, an examination is carried out, which allows you to find out the characteristics of the course of the disease and determine the exact location of the affected artery:
- Ultrasound with Dopplerography.
- Rheoencephalography (REG) – obtaining information about the elasticity and tone of the blood vessels of the head.
- Electroencephalography (EEG) is a study of the state of brain functions.
- Magnetic resonance imaging (MRI) - gives a detailed picture of the state of the brain, blood vessels and nervous system.
- Computed tomography (CT) is an X-ray examination of the structures of the brain.
After clarifying the diagnosis, depending on the degree and characteristics of the course of the disease, treatment is prescribed:
- Conservative. Preventive treatment with certain drugs (anticoagulants and thrombolytics) for several months or even years, with periodic monitoring of the degree of improvement.
- Surgical / neurosurgical treatment (for multiple blood clots, risk of thromboembolism):
- Novocaine blockade.
- Creating a bypass route for blood flow to a blocked section of the carotid artery.
- Replacement of part of a damaged vessel with vascular prostheses.
Higher education:
Kuban State Medical University (KubSMU, KubSMA, KubGMI)
Level of education - Specialist
Additional education:
Research Institute of Cardiology named after. A.L. Myasnikova
NTsSSKh them. A. N. Bakuleva
Russian Medical Academy of Postgraduate Education
Cantonal Hospital of Geneva, Geneva (Switzerland)
Russian State Medical Institute of Roszdrav
Factors contributing to the development of the disease
The following pathologies and abnormalities are related to narrowing of the carotid artery:
- atherosclerosis, in which plaques begin to form in the vessels. They narrow or block the lumen, complicating or stopping blood circulation;
- rheumatoid diseases caused by immune disorders;
- elevated blood cholesterol levels;
- the appearance of excess weight;
- genetic predisposition (presence of atherosclerosis, stroke, coronary artery disease in close relatives);
- diabetes;
- injuries (bruises, fractures, spinal osteochondrosis);
- Nonspecific aortoarteritis is an autoimmune disease. With it, large arteries become inflamed;
- thrombophlebitis;
Other predisposing factors include the presence of bad habits, old age, lack of physical activity, and poor nutrition.
When carotid artery stenosis occurs, the symptoms of which develop slowly, a person does not immediately notice the ailment.