Diseases of the vascular system are, first of all, dangerous because they are difficult to diagnose in the initial stages of development. Carotid artery aneurysm is one such disease. It is almost impossible to notice until serious health problems make themselves felt.
Aneurysm can occur in both adults and children. At the same time, it can develop for years, and a person does not even suspect it.
In this material we will look at the dangers of an aneurysm, how to recognize and treat it.
Carotid artery aneurysm - characteristics depending on location
Carotid artery aneurysm (ICD-10 code - I72.0) is a local increase in its diameter by more than 2 times. It is a limited protrusion formed by a stretched vascular wall.
The average age of patients is 47-53 years. Women suffer 2-2.5 times more often than men.
An aneurysm forms secondary to chronic diseases affecting the arterial bed. In the first stage, under the influence of a causative factor, nonspecific inflammation develops in the vessel wall: edema, destruction of endothelial cells and the muscle layer.
In the second stage, enzymes in the lesion lead to the destruction of collagen fibers. The artery wall becomes thinner and stretches. In the third stage, under the influence of a pulse wave, the thinned area is pressed and forms a protrusion.
Common artery
The vessel extends from the aortic arch to the angle of the maxilla and is affected in 27-30% of cases . Causes: atherosclerosis, Takayasu syndrome. Symptoms are associated with compression of the tissues and organs of the neck, and cerebral ischemia on the affected side. Formation within 2-4 weeks. The prognosis is relatively unfavorable, with frequent relapses. Surgical treatment is indicated for rapid progression and increasing clinical symptoms.
In the area of the angle of the mandible, the common carotid artery is divided into external and internal branches.
External SA
The ESA does not penetrate the cranial cavity, but supplies blood to the soft tissues of the face, the auricle, and the tissues of the nose. Affected in 12-14% of cases . Causes: Takayasu disease, congenital anomalies. Symptoms are associated with ischemia of the facial muscles, orbit, nasal cartilage, and external ear. Formation is slow, over 2-4 months. The prognosis is relatively favorable. Treatment is symptomatic and surgical.
Internal carotid artery (ICA)
An aneurysm of the internal carotid artery of the brain can be in one of the sections of the ICA - the cavernous sinus, supraclinoid section and bifurcation.
- Cavernous sinus . Aneurysms of this location are located below the sella turcica of the skull. The frequency of occurrence is 15-17%. Etiology: hypertension, Takayasu's disease. Formation within 3-4 weeks. Symptoms are associated with ischemia of the facial muscles and trigeminal nerve. The prognosis is relatively favorable, relapses are rare. Treatment is conservative and surgical.
- Supraclinoid region . Located behind the eyeballs. Affected in 17-20% of cases. The causes of aneurysm of the supraclinoid part of the ICA are vascular anomalies, hypertension, and trauma. Formation within 1 month. Manifestations are associated with ischemia of the 2nd, 3rd, 4th and 6th pairs of cranial nerves innervating the eyeballs. The prognosis is unfavorable; irreversible vision loss occurs in 12-15% of patients. Treatment is surgical.
- At the bifurcation site . Damage to this area occurs in 14-15% of cases and is localized in the center of the base of the skull. Causes: vascular abnormalities, genetic syndromes. Formation within 4-6 months. Symptoms: intense headache, decreased or loss of vision. The prognosis is unfavorable. Treatment is surgical.
Chapter 2: “Spinal Aneurysms”
Book: “Rare neurological syndromes and diseases” (V.V. Ponomarev)
Aneurysms (vascular malformations) most often represent congenital vascular malformations. Compared to cerebral aneurysms, spinal aneurysms are quite rare. There are arterial, arteriovenous, venous spinal aneurysms and cavernomas [3]. Arterial spinal aneurysms are saccular thin-walled protrusions of the wall of the spinal cord vessels, devoid of a muscle layer, which have a bottom, middle part and neck. Arteriovenous aneurysms are a tangle of varicose vessels of various diameters that provide shunting - direct discharge of arterial blood into the venous system.
Based on the nature of the clinical picture, four variants of the development of aneurysms are distinguished:
1) asymptomatic - accidentally detected during angiography or MRI; 2) pseudotumor unruptured - compressive structures of the adjacent nervous system; 3) ruptured, manifested by subarachnoid and (or) intracerebral hemorrhages; 4) causing ischemia of the spinal cord structures due to the “stealing” phenomenon.
Among spinal aneurysms, intradural arteriovenous ones are the most common [3]. Arterial aneurysms are observed less frequently and are localized on the anterior, posterior and lateral spinal arteries [2]. Isolated cases of diagnosis of aneurysms of the great radicular artery of Adamkiewicz, anterior and posterior radicular and radiculopineal, sulcocommissural or vascular corona arteries have been described [9, 10].
Venous spinal aneurysms are extremely rare. In 20% of cases, multiple spinal aneurysms occur [1].
The neurological manifestations of spinal aneurysms are extremely diverse and depend on their anatomical features (localization, level of location, relationship with the dura mater) and the pathogenetic variant of development. Most often, spinal aneurysms manifest as radicular pain and (or) spinal compression syndromes of spinal cord damage at various levels or clinical symptoms that mimic spinal circulatory disorders [6]. In cases of rupture, spinal aneurysms are manifested by a meningeal symptom complex, and hematomyelia may develop [4]. Unlike cerebral aneurysms, when a spinal aneurysm ruptures, meningeal syndrome is often not expressed. Repeated ruptures of the aneurysm are typical.
Due to clinical polymorphism, the diagnosis of spinal aneurysms is often difficult, as was the case in the presented case.
Patient A., 33 years old, banker, upon admission complained of weakness in the legs, more so in the left, difficulty urinating like incontinence, and periodic pain in the heart area. He was ill for 1.5 months, when suddenly intense pain in the heart area and an increase in body temperature to febrile levels appeared. Against this background, subacute weakness of the legs, more so on the left side, numbness of the torso and urinary retention were added. Twice he was treated in a neurological hospital at his place of residence with a diagnosis of “acute inflammatory myelopolyradiculoneuropathy”, received glucocorticoids according to a pulse therapy regimen, antibacterial and detoxification therapy. He noted some improvement in his condition: a decrease in pain, the appearance of minimal movements in his left leg. Transferred for further treatment and further examination. Of the previously suffered diseases, he noted colds. In early childhood, he was observed for minor chorea. There is no family history.
Upon admission, the patient’s general condition was satisfactory, with a correct physique and a well-developed muscular system. Somatically compensated. Blood pressure 120/80 mm Hg. Art. Higher nervous activity without features. Cranial nerves are normal. The strength and tone of the arm muscles are not impaired. The range of motion and strength in the left leg are significantly reduced (minimal movements are possible), muscle tone is significantly increased in a pyramidal pattern. The strength in the right leg is slightly reduced in the proximal parts to 4 points, the muscle tone in it is dystonic. Tendon-periosteal reflexes on the hands of medium vivacity, D=S, knee S
General blood test: hemoglobin reduced to 106 g/l, red blood cells 3.3 • 106/l, leukocytes increased 17.6 • 109/l (in the blood count, lymphocytes are reduced to 18%), ESR 34 mm/h. General urine test, biochemical blood test without any features. Blood sugar 4.7 mmol/l. CSF: yellow, transparent, protein content increased to 2.02 g/l, cytosis 12 • 106 cells/l. Oculist: visual acuity 1.0, fundus without features. ENMG: SPI along the peroneal and tibial nerves on both sides is reduced to 42-45 m/s, the amplitude of the M-response is slightly reduced.
Taking into account the medical history, objective examination data, and the results of paraclinical examination, the patient was diagnosed with subacute inflammatory demyelinating myelopolyradiculoneuropathy. Medrol (64 mg/day), rheopolyglucin, fresh frozen plasma, broad-spectrum antibiotics, baclofen, ozokerite applications and electrical stimulation of the leg muscles were prescribed. Against this background, the patient’s condition began to improve, strength in the left leg increased to the extent of moderate paresis, and sensory and pelvic disorders began to regress. However, 2 weeks after admission, for no apparent reason, girdle pain appeared in the thoracic region, and weakness in the legs increased again to the initial state. In this regard, MR myelography was performed: no bone-destructive changes were detected at the Thi-Thi2 level. In the spinal canal at this level, pathologically dilated vessels are detected (Fig. 26A). In the spinal cord at the Th5~Thg level, areas of hemorrhagic impregnation were identified (Fig. 26B). Conclusion: arteriovenous aneurysm of the thoracic spine with secondary signs of impaired spinal circulation and hematomyelia. After the diagnosis was established, the patient's condition began to slowly improve again, and no surgical treatment was performed. A year later, upon examination, only mild proximal paresis of the right leg was detected, the absence of knee and Achilles reflexes, and no sensory or pelvic disorders. Disability group II has been established.
Rice. 26A. MR myelogram of patient A., 33 years old, with a diagnosis of “arteriovenous aneurysm of the thoracic spinal cord” (coronal projection): pathologically dilated vessels are identified in the spinal canal at the Thi-Thi2 level (indicated by arrows)
Rice. 26B. MR myelography of the same patient (sagittal projection): areas of hemorrhagic impregnation were identified in the spinal cord at the Ths-Thg level (indicated by arrows)
Thus, the subacute development of radicular and radicular-spinal syndromes in combination with protein-cell dissociation in the cerebrospinal fluid and ENMG data made it possible to diagnose one of the forms of UDP, although the yellow color of the cerebrospinal fluid and mild anemia in the blood were not characteristic of this disease. Erroneous diagnosis led to the choice of incorrect treatment tactics. A retrospective analysis of the clinical picture can suggest that the disease began with a rupture of an aneurysm and, as a consequence, intracerebral and limited subarachnoid hemorrhage developed. Subsequently, the blood descended down the spinal canal and caused secondary (aseptic) inflammation of several underlying roots, simulating the picture of the upper respiratory tract. A similar diagnostic error was also described in the literature by R. E. Shields et al. [6]. Only the deterioration of the patient’s condition with clinical worsening of signs of focal spinal cord damage due to repeated intracerebral hemorrhage and the results of MR myelography helped make the correct diagnosis.
Currently, the hemodynamic theory of aneurysm formation is widespread in the literature, according to which this disease is caused by a congenital defect of the vascular wall and manifests itself with an increase in blood pressure [1]. This is confirmed by cases of several developmental defects: the presence of multiple spinal aneurysms, a combination of cerebral and spinal aneurysms, a combination with coarctation of the aorta or syringomyelia [8, 9]. There is also an inflammatory theory of the development of aneurysms, which explains the occurrence of the disease due to autoimmune damage to the vessel wall due to granulomatous angiitis [11].
Differential diagnosis of spinal aneurysm is carried out with spinal diseases: spinal form of multiple sclerosis, intra- and extramedullary tumors, spinal gliosis, spinal strokes, myelitis, various forms of VDP, vertebrogenic myelopathies.
The most radical method of treating spinal aneurysms is superselective embolization of the vessel feeding the aneurysm with thrombin or bucrylate [2, 4]. In case of ineffective embolization, as well as during vessel recanalization, open access removal of the aneurysm is proposed [7, 10]. In cases where the autoimmune genesis of the disease is established, it is advisable to prescribe immunosuppressive therapy [11].
Causes and risk groups
Causes:
- Atherosclerosis;
- Takayasu's disease;
- Hypertonic disease;
- Congenital vascular anomalies;
- Marfan syndrome;
- Syphilis;
- Tuberculosis;
- Connective tissue diseases;
- Periarteritis nodosa;
- Vasculitis.
Persons at risk are:
- With a family history;
- Over 50 years old;
- Suffering from cardiac ischemia and valve defects;
- Having had a heart attack or stroke;
- People with increased thrombosis.
Classification
Types of current:
- Acute - characterized by a sudden bright clinic, general cerebral symptoms, loss of consciousness. Observed during complications.
- Chronic - perennial, erased, wavy or asymptomatic.
Carotid aneurysms can be:
- Saccular - consist of a neck (through which they are connected to the vessel), a spherical body and a dome. This variety is more susceptible to rupture. The selection operation is clipping. The prognosis is relatively unfavorable.
- Fusiform - smoothly transition into a healthy vascular wall. Delamination is more typical for this variety. The operation of choice is resection. The prognosis is relatively favorable.
- Mixed - show signs of both forms. They are characterized by high vulnerability and rapid delamination. The operation of choice is resection. The prognosis is unfavorable.
Forms of the disease:
- Tumor-like – clinically resembles tumor growth. The course is chronic, the symptoms are associated with compression of anatomical structures and increasing compression syndrome.
- Apoplexy – clinically resembles apoplexy (convulsive syndrome). The course is acute, convulsions and loss of consciousness may be the first and only manifestation.
We wrote about the classification of cerebral aneurysm here.
You can read all the detailed information about this vascular lesion - what types there are, where they can occur, why saccular aneurysms, as well as true and false aneurysms, are dangerous - in separate articles.
Symptoms
Any change in the blood circulation of the carotid arteries leads to the development of neurological disorders. They arise due to insufficient supply of oxygen and nutrients to the brain tissues.
At the initial stages of formation, they may not give a clinical picture. The first symptom that guides the doctor to diagnose an aneurysm is general weakness (a person is sleepy, tired, lazy for no reason).
In some patients with carotid aneurysm, symptoms include sleep disturbances, tinnitus, dizziness, and a throbbing sensation in the head or ears. Visual disturbances may also develop. As the aneurysm grows, adjacent structures are compressed (cervical neurovascular bundle, esophagus, trachea), resulting in hoarseness, nosebleeds, and impaired speech and breathing.
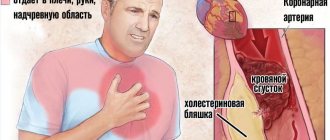
The danger of artery expansion lies not only in the possibility of rupture of its wall, but also in the formation of a blood clot. If it comes off, there is a risk of developing embolism. If there are signs of carotid artery aneurysm dissection, a sudden headache occurs, accompanied by nausea/vomiting, increased light sensitivity, double vision, anxiety, and also in some patients – fainting, coma.
Possible complications
Complications may include dissection and rupture, thrombosis, stroke, compression of the esophagus, loss of vision or hearing, memory loss, thyroiditis, paralysis of half the body.
Rupture is a common complication of the natural course of the disease . It occurs due to overstretching of the carotid artery, which has undergone irreversible dystrophic changes.
Causes:
- Hypertensive crisis;
- Injuries;
- Detachment of an atherosclerotic plaque.
Risk factors are hypertension, smoking, diabetes, stress, physical overexertion.
Symptoms of a rupture:
- Anxiety;
- Dyspnea;
- Tachycardia;
- Increased pressure;
- Violation of visual, auditory, cognitive functions;
- Paralysis of half the body;
- Lack of response to external stimuli;
- Loss of consciousness.
Treatment in 100% of cases is surgical. The prognosis is unfavorable. Stroke occurs in a third of patients.
Symptoms of the disease
First symptoms:
- Bursting headaches and neck pains.
- Fatigue, tiredness.
- Increased pressure.
Symptoms depending on the location of the lesion:
- Common carotid artery - pain, feeling of a foreign body in the neck, hoarseness, pain when swallowing.
- NSA – loss of facial sensitivity, nosebleeds, pain in facial muscles.
- Cavernous sinus – decreased sensitivity of the tongue, facial skin, pain in the orbit.
- Supraclinoid region – paralysis of the eyeball, myopia.
- Bifurcation - flickering before the eyes, narrowing of the visual field.
Left and right side affected
Right-sided lesion appears:
- Loss of speech functions.
- Epilepsy.
- Impaired sensitivity (numbness, “crawling goosebumps”).
- Visual disorders.
Left-sided lesion is characterized:
- Migraine;
- Cramps;
- Fainting;
- Disorders of consciousness;
- Hypertension;
- Dizziness.
Signs of deterioration
As it progresses, symptoms of cerebral ischemia appear:
- Fainting;
- Decreased hearing, memory, attention;
- Frontal and occipital pain;
- Changes in personality traits;
- When the CCA and ICA are affected - paresis of half the body, hypertension;
- When the neck veins are compressed, they become swollen, swollen, and blue in the upper half of the body;
- When the ECA is affected, there is paralysis of the facial muscles, disturbances in swallowing and chewing, and jaw pain.
The threat of complications is indicated by increased headache, persistent hypertension, loss of consciousness, migraine with aura, convulsions, stupor, stupor, decreased reflexes.
Diagnosis of neck and brain disease
Examination algorithm:
- Survey and inspection . Complaints of bursting pain, fainting, decreased vision and hearing, sensory disturbances; history of vascular pathology. On examination, there is pastiness, facial hyperemia, and swelling of the veins of the neck.
- Objective research . Swelling and enlargement of the neck and thyroid gland, vascular murmur, hypertension.
- Laboratory data . Increased levels of platelets, fibrinogen, cholesterol.
- Angiography of neck vessels . Defect in the contour of the vascular wall, contrast leakage beyond the vessel.
- Ultrasound of neck vessels with duplex scanning . Limited vascular expansion, tortuosity of the branches of the carotid artery, atherosclerotic plaques, blood flow turbulence.
- CT (MRI) . Local edema, atrophy of cranial nerves 2, 3, 4, 6, hemorrhage, cidrocephaly, compression of the esophagus and trachea, foci of calcification.
- EEG . Disappearance of alpha waves, registration of theta and delta ranges.
You can read how to diagnose a cerebral aneurysm in a separate material.
Diagnostics
Diagnosis begins with the doctor examining the patient, studying the patient’s complaints and medical history.
After drawing up the clinical picture of the pathology, instrumental research methods are prescribed, which may include:
- Duplex or triplex scanning of the carotid arteries. The doctor examines the condition of the blood vessels in a two-dimensional or three-dimensional projection.
- Ultrasound of the carotid artery. This type of study helps to understand the structure of the vascular wall, the speed of blood flow and the state of the lumen. Doppler ultrasound will allow you to examine in detail the condition of the vessels and identify possible violations.
- MRI and CT. It helps to identify the exact location of the aneurysm, its shape and size down to the smallest detail. This will help you choose the right treatment strategy.
- Angiography. A special contrast agent is injected directly into the blood vessel, after which a series of x-rays are taken.
- EEG (electroencephalography). Helps identify vascular disorders in the brain.
Based on the results obtained, the doctor makes a diagnosis and decides which treatment methods to resort to.
Therapy tactics
Treatment of carotid artery aneurysm is divided into conservative and surgical. Indications for conservative therapy:
- Preparation for surgery;
- No complaints;
- Size up to 1 cm;
- No progression.
Conservative therapy includes:
- Statins, antihypertensive, diuretic drugs;
- Symptomatic drugs (analgesics, NSAIDs);
- Vasodilators and nootropics.
Surgery
Indications for surgery:
- Growth more than 4 mm in 6 months;
- The appearance of the clinic;
- Hypertension;
- Increased thrombus formation;
- History of heart attack or stroke;
- Risk of complications.
Contraindications for surgery:
- Exacerbation of infectious diseases;
- Multiple organ failure;
- Sepsis;
- High risk of surgical complications.
Types of operations:
- Clipping is the removal of an aneurysm from the bloodstream by placing a clip on it. Selection operation for pouch shape;
- Resection – removal of the enlarged area and replacing it with a prosthesis. The prosthesis can be a segment of a peripheral artery or a synthetic tube;
- Endovascular embolization is the filling of an aneurysm with surgical glue through a balloon inserted from the femoral artery. The operation of choice in uncomplicated patients.
Conservative treatment is indicated for patients for whom surgery is contraindicated. In case of increased intracranial pressure, a palliative operation is performed - installation of drainage for the outflow of cerebrospinal fluid.
Emergency assistance in case of rupture
If signs of rupture appear, you must call an ambulance.
Algorithm of actions:
- Provide the patient with rest and fresh air;
- Offer an analgesic or sedative;
- Help the patient take a horizontal position with the head down.
When an ambulance appears, the following is carried out:
- Transportation;
- Stabilization of hemodynamics;
- Introduction of plasma substitutes;
- If clinical death develops, resuscitation measures are taken.
Emergency diagnostics (CT, ultrasound) and surgery are performed in the hospital. The intervention is carried out by a surgical team under angiography control.
Aneurysms of the vessels of the heart, brain, lungs, aorta, neck and splenic artery are no less dangerous. And when they rupture, professional, emergency care and prompt hospitalization are also very important.
Prevention recommendations
To maintain blood vessels in normal tone and try to reduce the risk of an aneurysm, you should adhere to the following recommendations:
- Monitor your body weight.
- Follow your diet.
- To refuse from bad habits.
- Try to eat as little smoked meats and fatty foods as possible.
- Avoid stress, conflicts, worries, and excessive physical strain.
- Get proper rest and sleep.
- Regularly undergo preventive examinations and, if necessary, periodically take a course of blood thinning medications.
If a person belongs to the risk group of patients who may develop an aneurysm, he should be especially careful about following the recommendations. This will help preserve not only your health, but possibly your life.
Vessels
Arteries of the Head and Neck: Anatomy, Diagram, Atherosclerosis
Feb 06, 2020 Kokh V. A.
16582
Vessels
Anterior Cerebral Artery: Segments, Resistance Index, Normal, Aneurysm, Branches
Feb 03, 2020 Kokh V. A.
11487
Vessels
Preventive actions
Primary prevention:
- To give up smoking.
- Normalization of blood pressure.
- Low-salt diet.
- For persons over 50 years old - annual medical examinations with ultrasound.
- Laboratory screening for the detection of atherosclerosis, diabetes mellitus, hypertension.
Secondary prevention:
- Clinical examination.
- Dynamic monitoring of the condition of the aneurysm (ultrasound, CT).
- Treatment of concomitant diseases.
Aneurysm of the carotid artery and its branches is a common complication of chronic vascular diseases. The pathology is distinguished by a progressive course and an increasing clinical picture. Treatment is surgical. Prevention is aimed at early detection and treatment of cardiovascular pathology.
Treatment
An aneurysm cannot heal on its own. In most cases, the pathological formation increases in volume, the walls of the vessel become thinner. If left untreated, the aneurysmal sac ruptures and bleeding begins, often leading to the death of the patient.
Vascular surgeons treat aneurysmal deformation of the carotid artery. The only effective way to treat pathology is surgery, during which the affected area is “switched off” from the bloodstream.
The type of operation is determined by the patient’s age, his condition, the presence of concomitant diseases and the course of the underlying pathology.
- Complete removal of the aneurysm and replacement of the affected area with a plastic prosthesis or a piece of blood vessel from another part of the body. As a result, the patency of the carotid artery is completely restored. During the operation, the afferent and efferent ends of the artery are isolated, clamped with rubber tubes, the aneurysmal sac is opened, the affected vessel walls are removed, and the resulting defect is replaced with a prosthesis. At the same time, the integrity of the veins is preserved. If the size of the aneurysm exceeds 5 cm, the entire affected segment of the artery is removed and rubber hoses are implanted instead.
- Partial resection of the aneurysmal sac is performed in cases where it is not possible to completely remove the formation. At the same time, part of it is excised, all collaterals and the cavity of the sac are sutured, and blood flow is restored using a prosthesis. If such an intervention is not possible, bypass anastomoses are sewn in - special shunts through which blood will circulate.
- Endovascular techniques are used for small aneurysms located in hard-to-reach places. The operation is performed inside the vessel using a special catheter. This is a minimally invasive technique that requires only one small incision in the neck through which a catheter is inserted into the vessel. Using angiosurgical optics, the affected area of the artery is removed and a prosthetic replacement is made.
When an aneurysm ruptures, the prognosis is often unfavorable: about 30% of patients die. To provide emergency care, surgery and further rehabilitation, patients are hospitalized. They are provided with strict bed rest, blood pressure levels are monitored, and medications are prescribed:
- Sedatives – “Valocordin”, “Bellaspon”, “Persen”,
- Anti-pain medications – “Ketonal”, “Ibuklin”, “Brustan”,
- Drugs that improve cerebral circulation - Vinpocetine, Cavinton, Cerebrolysin,
- Vasodilators - “Papaverine”, “Pentoxifylline”, “Cinnarizine”,
- Medicines that improve the rheological properties of blood - “Nicotinic acid”, “Complamin”, “Trental”,
- Antiplatelet agents – “Aspirin”, “Curantil”, “Cardiomagnyl”,
- Antihypoxants - Actovegin, vitamins - Neuromultivit.
Conservative treatment is aimed at stabilizing the process and strengthening the walls of blood vessels.
Treatment with folk remedies should be carried out only after consultation with a specialist. Tincture of dill and hawthorn, decoction of rose hips and chokeberry increase vascular tone. Propolis tincture is an effective tonic.
Complications and adverse consequences of the pathology are:
- Aneurysmal rupture,
- Internal bleeding
- Hemorrhagic shock
- Thrombosis,
- Brain abscess.
If you deal with this problem in a timely manner, you can prevent a disaster.