Rules for nursing care in newborns and older children with heart defects
The nursing process for heart defects provides the needs of the child’s body, contributes to the normalization of all its functions and the speedy recovery of young patients.
Responsibilities of a nurse caring for children with heart defects:
- Determination of body temperature.
- Monitoring of general condition.
- Monitoring bed rest.
- Preparation for medical procedures.
- Maintaining medical records.
- Sanitation of the respiratory tract.
- Collection of laboratory material for analysis.
- Providing information to parents about the required diet.
The nurse's responsibilities include informing parents about the treatment, life prognosis and complications that may arise during therapy or surgery.
Nursing care in departments for children with cardiac problems is necessary to create the most comfortable conditions for young patients before and after surgery.
Application of the nursing process in preventive work with parents:
- The nurse should teach parents how to assist with episodes of shortness of breath and cyanosis.
- The sister's responsibilities include teaching parents how to properly assess the health and general condition of their child.
- Parents or guardians, with the support of staff, learn how to properly raise a child with a heart defect - avoiding overprotection.
- The medical staff teaches the mother and father the correct use of physical activity and massage techniques.
- The nurse is obliged to inform parents about the need for constant monitoring by a cardiologist and provide advice regarding the documentation of social disability benefits.
How to treat heart defects
A heart defect is considered to be organic damage to the heart valves, septum, and myocardium, which leads to persistent disruption of the pumping of blood mass. During decompensation, these changes cause stagnation in the veins, tissues, organs, and severe oxygen depletion (hypoxia).
Cardiac pathology also includes defects of large vessels (for example, stenosis of the aortic isthmus, patent ductus botallus, and others), although some scientists believe that there are no sufficient grounds for this.
The problem of how to treat a heart defect is always associated with determining the type of defect, its main cause, the degree of compensatory capabilities of the myocardium, the presence and prognosis of complications.
There is a division of diseases into 2 large groups of pathology:
- acquired,
- congenital.
Vices have different causes. Acquired ones develop over the years and are diagnosed closer to adolescence and adulthood, while congenital ones are detected in newborns (6–8 cases per 1000). The mechanism of heart damage is the same.
What is damaged in the heart when there is a defect?
The most common acquired defects are:
- Lesions of the valve apparatus (cusps and structures involved in closing the chambers of the heart), with rheumatism, mitral and tricuspid defects are formed in young people 10–30 years old, with syphilis, insufficiency of the aortic valves upon reaching 40 years of age and older, in the case of severe atherosclerosis, defects develop in individuals in old and senile age.
- Narrowing or widening of the openings between the chambers of the heart through which blood flows (mitral stenosis, narrowing of the aortic orifice, narrowing of the right atrioventricular orifice).
- Pathology of the cardiac membranes (epicardium, myocardium and endocardium) against the background of severe inflammatory diseases such as rheumatism, sepsis, severe forms of childhood infections lead to the participation of the heart wall in the formation of the defect.
With congenital defects, the pathology is formed during the formation of organs in the embryonic period. As a result, the newborn is determined to have a disturbed heart structure:
- ventricular septal defects, patent foramen ovale;
- the ductus botallus remains unopened;
- stenosis of the aortic isthmus or pulmonary artery is formed;
- the localization of the main drainage vessels changes dramatically;
- underdevelopment (hypoplasia) of one of the ventricles.
How to determine the type of defect?
It is customary to classify defects into 3 types:
- simple - one of the valves or hole is damaged;
- complex - there is a combination of narrowing or widening of the holes with valve changes;
- combined - multiple structural abnormalities, most typical of congenital defects.
The number of types of heart defects exceeds a hundred. For early diagnosis, all newborns are examined by a neonatologist; ultrasound methods, magnetic resonance and computed tomography, and angiography are used at the modern level.
What influences the decompensation of the defect?
In the case of acquired defects, it is impossible to cure cardiac pathology without preventive measures in relation to the underlying causes. The following is required:
- prevention of rheumatic attacks, since the defect increases each time;
- treatment of infectious complications after acute illnesses, injuries, sore throats;
- carrying out therapy for hypertension and atherosclerosis in adults suffering from these diseases;
- complete cure of syphilis before deregistration with a venereologist.
The development of decompensation of cardiac activity is determined by disruption of the structures. Due to insufficient closure of the valves, the blood that came out during systole from one part of the heart to another or into the vessels partially returns. Together with the next portion, it overfills the chamber and causes stagnation in the afferent vessels.
When the opening is narrowed, similar difficulties are created for the functioning of the heart: through the narrowed opening, blood passes with difficulty into the next section and accumulates with the portion received during diastole, causing expansion and hypertrophy. After a certain time, the performance of the stretched heart muscle is lost. Myocardial cells do not have enough energy to push the required volume of blood. This is how oxygen starvation caused by heart failure begins to manifest itself.
The goal of conservative treatment is to maintain the energy balance of the myocardium and combat tissue hypoxia.
What is used to treat heart disease?
Acquired defects require the prescription of special medications depending on the specific disease: antibiotics, steroid hormones, antihypertensive drugs.
Drugs used:
- groups of cardiac glycosides;
- diuretics;
- containing potassium and magnesium;
- anabolic hormonal agents;
- vitamins B, C, E to provide antioxidant activity and support immunity;
- if necessary, antiarrhythmic drugs are prescribed;
- during an attack, oxygen inhalation is necessary;
- According to indications, drugs that reduce blood clotting are prescribed.
Conservative therapy is indicated during preparation for elective surgery and in the postoperative period. Patients are recommended to undergo annual treatment in a specialized center, cardiology hospital, or sanatorium.
Here, attention is necessarily paid to the regimen, feasible physical activity, and dietary nutrition. To prevent hypoxia, oxygen baths, cocktails, and inhalations are prescribed. Walking in a coniferous forest helps improve breathing and provides the patient with phytoncides.
Why is surgery needed?
If an adult is responsible for his own health and the consequences of refusing the proposed type of treatment, then parents and close relatives should worry about children. Observation by a cardiologist with annual monitoring of the development of the defect in a growing baby is an important ongoing responsibility of the mother and father.
You shouldn’t hope that “everything will go away on its own.” Statistics show rather disappointing information: there are very few birth defects among the adult population, because 60% occur in children under 14 years of age. Of these, without timely surgical treatment, up to 70% die in the first year of life.
Depending on the severity of the defect, surgery may be delayed until an older age, when the baby has developed sufficient immunity and a willingness to deal with the consequences of surgery.
In cardiac surgery, there are phases of primary adaptation and compensation, when the child’s condition is stable and most suitable for surgery. In addition, the timing is determined by the state of blood circulation in the pulmonary circle.
The phase of irreversible changes (terminal) is expressed in degeneration of internal organs and the heart, and the addition of severe complications.
What complications are possible if you refuse surgery?
Possible complications concern the heart itself and the organs most interested in sufficient blood supply - the lungs and brain.
From the side of the heart the following are observed:
- attacks of heart failure;
- various arrhythmias and conduction disorders;
- septic endocarditis;
- continuously sluggish rheumatic carditis.
The respiratory organs react:
- frequent colds;
- chronic bronchitis;
- prolonged cases of pneumonia.
In the central nervous system there are:
- circulatory disorders with areas of ischemia or hemorrhage in the cerebral cortex;
- abscesses in brain tissue;
- thromboembolism.
Therefore, it is recommended to operate on severe defects already in infancy.
Types of surgical interventions
The specific operation is selected by the cardiac surgeon depending on the type of defect and the degree of defects in the heart chambers and large vessels. Currently, cardiology centers have been organized with special equipment that makes it possible to operate on a stopped heart with connection to artificial circulation, and to use hypothermia (lowering body temperature).
- If the ductus arteriosus is open, ligation and intersection of the unnecessary vessel are performed.
- A defect of the interventricular or interatrial septum requires suturing, plastic surgery of the septal tissue with the application of a “patch” to completely stop communication between the atria or ventricles.
- If possible, narrowed vessels are widened with stents or a narrow section is removed (for stenosis of the aortic mouth).
- If the position of the efferent arteries is disturbed, it is necessary to correct the localization with movement of the vessels.
- Valve defects are eliminated by installing artificial analogues or a homograft.
- When there is stenosis of the valves and atrioventricular orifice, commissurotomy and dilation are performed with the installation of a ring to prevent re-union.
There are no ideal valves yet. They are divided into 2 types:
- mechanical - made of metal, synthetic fabrics, single- or double-leaf, designed for up to 50 years, require constant use of anticoagulants;
- biological - made from human or pig tissue, after 12 years they may lose elasticity and require replacement. Indicated in old age and when it is impossible to take anticoagulants.
If artificial valves were used, the patient must take blood thinning medications for the rest of his life. When using homografts, cytostatics are needed to prevent tissue rejection.
Complex, combined defects may require repeated interventions with breaks from several months to a year.
Treatment in the postoperative period
In the intensive care unit, hemodynamic monitoring is carried out after surgery. The patient is connected to a continuous monitor and heart rate, blood pressure, and respiration are monitored.
Analgesics are administered for pain relief. An oxygen mask for breathing must be used. A nutrient solution, vitamins, and antibacterial drugs are injected drip into the subclavian catheter to prevent pneumonia.
Breathing exercises are recommended from the third day. The patient's regimen depends on the degree of complexity of the operation and is determined by the attending physician.
When installing a mechanical type of artificial valve, indirect anticoagulants (Phenilin, Warfarin) are prescribed from the first days. The dosage is selected based on the results of determining the prothrombin index. It is maintained at 35–45%.
After discharge from the hospital, prothrombin will have to be checked at least once a month. In addition, it is necessary to exclude foods rich in vitamin K from food, since it increases coagulation and reduces the effect of anticoagulants.
These products include:
- green tea,
- cabbage (especially broccoli),
- spinach,
- legumes,
- cheese,
- coffee,
- leaf salad.
How is physical activity restored?
The recovery period for different operations is 3–6 months, depending on the condition of the heart before the intervention. During the first 3 months, the bone tissue of the sternum grows together, so it is not recommended to lift weights of more than 5 kg, pull heavy objects with your hand, or push with your shoulder. It is quite possible to do light housework. It is recommended to start driving a car 3 months after the operation.
Forecast
Repeated attacks of rheumatism in childhood and adolescence significantly worsen the prognosis for the patient's life.
If surgical treatment is delayed, the child becomes disabled at an early age. He can't play fast games, he can't study hard.
Against the backdrop of successes in cardiac surgery, postoperative mortality is still up to 3% when ligating the ductus botellus. A successful operation allows the patient to live and work fully.
After radical complex interventions in the stage of decompensation, up to 30% of patients cannot be saved. Therefore, the timing of surgical treatment is so important.
Parents should think in advance about the health of their future children. Factors such as alcohol intake, smoking, and infectious diseases suffered by the expectant mother in the early stages of pregnancy significantly affect the proper development of the fetus.
In childhood, a child must be protected from colds, dressed according to the season, and sore throats treated. Strengthening the immune system helps overcome possible diseases.
Providing nursing care for rheumatism in children
The nursing process for rheumatism includes several stages. At the first stage, the staff records in writing the symptoms voiced by the parent or the patient himself:
- poor appetite;
- elevated temperature;
- joint pain;
- arrhythmia;
- dyspnea;
- symptoms of minor chorea.
At the first stage of the nursing process, an anamnesis of the disease and the life of the child’s family is compiled. The family history records information about whether family members have congenital heart defects, rheumatic diseases, etc.
The nurse fills out a medical record with test results (general blood serum analysis, biochemical analysis, urinalysis).
At the second stage of the nursing process, therapeutic measures are carried out for children with rheumatic heart disease and the nuances of care are substantiated, as well as problems that require immediate solutions are identified.
This mainly concerns general intoxication of the body: elevated temperature; weakness, fever; tachycardia; swelling; hyperkinesis. Such conditions increase the risk of developing myocarditis, heart failure, and acquired heart defects.
At the third and fourth stages, nursing care is necessary to ensure that recovery is faster and complications do not arise.
Nursing staff work plan:
- Ensuring ward and bed rest: for this purpose, conversations are held with the baby and his parents about the fact that there is a vessel or potty in the ward, and the patient does not need to get out of bed and go to the toilet if complete bed rest is prescribed. The requirement is caused by the need to provide maximum comfort necessary for the affected joints and heart in children and reduce painful manifestations.
- The sister monitors the leisure time of children who are prescribed bed rest; she informs parents about books and toys that they should bring to the ward.
- Medical staff monitors the sanitary condition of the wards. The sister supervises the cleaning of the room, ventilation, and change of bed linen.
- The nurse assists small patients in the process of eating and is responsible for hygiene procedures. Parents should be informed about what hygiene products they need to bring for their children.
- The department staff monitors compliance with the diet. If there are problems with the cardiovascular system, the amount of salt and fluid intake in children's diet is limited. Parents are advised not to bring prohibited foods to their children.
- Nurses monitor manipulations, medications, vitamins and sedatives. They collect biological material for analysis and take children to diagnostic procedures (ultrasound, cardiogram, x-ray). Parents are informed about the side effects of medications and the expected effectiveness of treatment.
At the fifth stage of the nursing process, the child’s condition is assessed after treatment. Proper organization of care for young patients with rheumatism allows you to effectively restore health and discharge the patient with a referral to a sanatorium for a full recovery.
Heart defects in children and adults: essence, signs, treatment, consequences
Have you been struggling with CHOLESTEROL for many years without success?
Head of the Institute: “You will be amazed at how easy it is to lower your cholesterol just by taking it every day...
Read more "
The unknown is always, at a minimum, alarming or people begin to fear it, and fear paralyzes a person. On a negative wave, wrong and hasty decisions are made, their consequences worsen the situation. Then again fear and again wrong decisions. In medicine, such a “loop” situation is called circulus mortum, a vicious circle. How to get out of it? Let shallow but correct knowledge of the basics of the problem help solve it adequately and on time.
What is a heart defect?
Each organ of our body is designed to function rationally in the system for which it is intended. The heart belongs to the circulatory system, helps the movement of blood and its saturation with oxygen (O2) and carbon dioxide (CO2). As it fills and contracts, it “pushes” the blood further into large and then small vessels. If the usual (normal) structure of the heart and its large vessels is disturbed - either before birth, or after birth as a complication of the disease, then we can talk about a defect. That is, a heart defect is a deviation from the norm that interferes with the movement of blood or changes its filling with oxygen and carbon dioxide. Of course, as a result, problems arise for the whole organism, more or less pronounced and of varying degrees of danger.
A little about the physiology of blood circulation
The human heart, like that of all mammals, is divided into two parts by a dense septum.
The left one pumps arterial blood, it is bright red and rich in oxygen. The right one is venous blood, it is darker and saturated with carbon dioxide. Normally, the septum (called the interventricular septum) has no openings, and the blood in the cavities of the heart (atria and ventricles) does not mix. Venous blood from the whole body enters the right atrium and ventricle, then into the lungs, where it gives off CO2 and receives O2. There it turns into arterial, passes through the left atrium and ventricle, reaches the organs through the vascular system, gives them oxygen and takes in carbon dioxide, turning into venous. Then - again to the right side of the heart and so on.
The circulatory system is closed, which is why it is called the “circulatory circle”. There are two such circles, both involve the heart. The circle “right ventricle – lungs – left atrium” is called small, or pulmonary: in the lungs, venous blood becomes arterial and is transmitted further. The circle “left ventricle - organs - right atrium” is called a large circle; passing along its route, the blood from arterial again turns into venous.
Functionally, the left atrium and ventricle are under high load, because the major circle is “longer” than the small circle. Therefore, on the left, the normal muscular wall of the heart is always somewhat thicker than on the right. The large vessels entering the heart are called veins. Exiting through arteries. Normally, they do not communicate with each other at all, isolating the flow of venous and arterial blood.
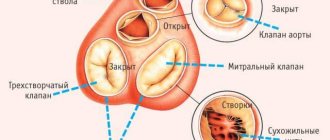
Heart valves are located both between the atria and ventricles, and at the border of the entrance and exit of large vessels. The most common problems are with the mitral valve (bicuspid, between the left atrium and the ventricle), in second place - the aortic (at the place where the aorta exits the left ventricle), then the tricuspid (three-cuspid, between the right atrium and ventricle), and in the “outsiders” - the valve of the pulmonary artery, at its exit from the right ventricle. The valves are mainly involved in the manifestations of acquired heart defects.
Video: principles of blood circulation and heart function
What are heart defects?
Let's consider the classification, adapted for patients.
- Congenital and acquired - changes in the normal structure and position of the heart and its large vessels appeared either before or after birth.
- Isolated and combined - changes are either single or multiple.
- With cyanosis (so-called “blue”) - the skin changes its normal color to a bluish tint, or without cyanosis. There are generalized cyanosis (general) and acrocyanosis (fingers and toes, lips and tip of the nose, ears).
I. Congenital heart defects (CHD)
Disturbances in the anatomical structure of the child’s heart are formed in utero (during pregnancy), but appear only after birth. To get a more complete picture of the problem, see pictures of heart defects.
For convenience, they were classified based on the blood flow through the lungs, that is, the small circle.
- CHD with increased pulmonary blood flow - with and without cyanosis;
- CHD with normal pulmonary blood flow;
- CHD with reduced blood flow through the lungs - with and without cyanosis.
Ventricular septal defect (VSD)
VSD occurs most often, usually in combination with other anomalies. Through the hole, arterial blood from the left ventricle (where the pressure is higher) passes into the right, increasing the load on the pulmonary circle, and then on the left side of the heart. The muscle wall increases, and an x-ray shows a “spherical” heart.
Treatment: if the septal opening is small and does not particularly affect blood circulation, then surgery is not required. In case of serious violations, surgical intervention is mandatory - the hole is sutured, the interventricular septum becomes normal.
Cholesterol will drop to normal! Will help on…
A tricky recipe for cleaning blood vessels from bad cholesterol! 4 drops and all plaques will disappear...
Prognosis: patients live long, into old age.
Absence of the interventricular septum, or its large defect
Another name is the Eisenmenger complex. The blood mixes in the ventricles and has low oxygen levels, causing severe cyanosis. The pulmonary circulation is overloaded, the heart is spherically enlarged. A cardiac hump is visible, pulsation on the right; to reduce shortness of breath, patients squat (the so-called forced position).
Treatment: it is important to perform the operation in time, while the wall of the pulmonary artery still has a normal structure.
Prognosis: Without adequate measures, patients rarely live beyond 20 to 30 years.
Patent foramen ovale
The septum between the atria does not heal. Blood flows from left to right, along a pressure gradient, the wall of the right atrium and ventricle thickens, and the pressure increases. Now there is a reset from the right to the left, and the heart enlarges (hypertrophies) in the left parts.
A small hole does not give any special manifestations, people live well with it. If the defect is pronounced, then acrocyanosis is visible and shortness of breath is tormented.
Combined defect: patent foramen ovale and narrowing of the mitral or aortic valves. The heart greatly increases in size, a “heart hump” is formed - the sternum protrudes forward, pallor, shortness of breath.
Treatment: surgical if the defects are severe and functionally dangerous.
Prognosis: for an isolated defect - positive, for a combined defect - cautious (depending on the stage of blood flow disturbance).
Patchy ductus arteriosus
After the birth of the child, the communication between the aorta and the pulmonary artery was not interrupted. Again the same principle: blood leaves the high pressure zone to the lower pressure zone, that is, from the aorta along the ductus botallus to the pulmonary artery. Venous blood mixes with arterial blood, and the small circle experiences overload. First, the right and then the left ventricle enlarges. Pulsation of the arteries in the neck is visible, cyanosis and severe shortness of breath (lack of air) develop.
Prognosis and treatment: such a defect, if the diameter of the non-overgrown duct is small, may not make itself felt for a long time and is not life-threatening. If the defect is serious, surgery is inevitable, and the prognosis in most cases is negative.
Narrowing (coarctation) of the aorta
It is observed along the thoracic and abdominal sections of the aorta, more often in the isthmus region. Blood cannot flow down normally, and additional vessels develop between the upper and lower parts of the body.
Signs: heat and burning in the face, heaviness in the head, numbness in the legs. The pulse is tense in the arteries of the arms, and weakened in the legs. Blood pressure measured in the arms is much higher than in the legs (we only measure it while lying down!).
Treatment and prognosis: surgery is needed to replace the narrowed section of the aorta with a graft. After treatment, people live a long time and do not experience any discomfort.
Tetralogy of Fallot
Tetralogy of Fallot is the most severe and most common defect in newborns. Anatomically - combined, with a violation of the exit from the right ventricle of the pulmonary artery and its narrowing, a large hole in the interventricular septum, dextraposition (located on the right, and not on the left, as is normal) of the aorta.
Symptoms: cyanosis even after light exertion, attacks with severe shortness of breath and loss of consciousness develop. The functioning of the stomach and intestines is disrupted, there are nervous system disorders, and the child’s growth and development are slowed down.
Treatment: in not too severe cases - surgery to eliminate stenosis (narrowing) of the pulmonary artery.
Prognosis: unfavorable. Unfortunately, children with severe cyanosis and profound developmental disorders cannot live long.
Narrowing (stenosis) of the pulmonary artery
Usually the problem is improper development of the valve ring; less often, the cause of narrowing of the pulmonary artery can be a tumor or dilatation (aneurysm) of the aorta. Children are developmentally delayed (infantilism), hands are cyanotic and cold, and sometimes a hump of the heart is visible. The appearance of the fingers on the hands is characteristic: they become like drumsticks - with widened and thickened tips. The main complications are infarction (death) of the lung and purulent processes, blood clots, and in about 1/3 of cases - tuberculosis.
How to treat: surgery only.
Prognosis: depending on the presence and severity of complications.
Summary: Congenital heart defects, for the most part, can be cured in both children and adults. There is no need to be afraid of heart operations; now the technology is being improved and cardiac surgeons are constantly undergoing training. The result largely depends on the general condition of the patient and the timing of the operation.
Video: congenital heart defects in children
II. Acquired heart defects
In the period from birth to the formation of the problem, the heart has a normal structure, blood flow is not impaired, and the person is completely healthy. The main cause of acquired heart defects is rheumatism or other diseases, with the localization of pathological (disease-related) processes in the heart and large vessels extending from it. Changed valves can narrow the openings for blood inlet and outlet - this is called stenosis, or widen them compared to normal, forming functional valve insufficiency.
Depending on the degree of defect and disturbance of blood flow, the concepts of compensated (due to thickening of the walls of the heart and increased contractions, blood flows in normal volumes) and decompensated (the heart enlarges too much, the muscle fibers do not receive the necessary nutrition, the strength of contractions decreases) acquired defects were introduced .
Mitral valve insufficiency
Incomplete closure of the valves is the result of their inflammation and consequences in the form of sclerosis (replacement of “working” elastic tissues with hard connective fibers). When the left ventricle contracts, blood is pumped in the opposite direction into the left atrium. As a result, a greater contraction force is needed to “return” the blood flow towards the aorta, and the entire left side of the heart hypertrophies (thickens). Insufficiency in the pulmonary circulation gradually develops, and then - a violation of the outflow of venous blood from the systemic circulation, the so-called congestive insufficiency.
Signs: mitral flush (pinkish-blue color of lips and cheeks). Trembling of the chest can be felt even by the hand - it is called a cat's purring, and acrocyanosis (a bluish tint of the hands and toes, nose, ears and lips). Such picturesque symptoms are possible only with a decompensated defect, but with a compensated defect they do not occur.
Treatment and prognosis: in advanced cases, to prevent circulatory failure, replacement of the valve with a prosthesis is required. Patients live a long time, many do not even suspect about the disease if it is in the compensation stage. It is important to treat all inflammatory diseases in a timely manner.
Mitral stenosis (narrowing of the valve between the left atrium and ventricle)
Mitral valve stenosis is more common (2-3 times) in women than in men. The cause is rheumatic changes in the endocardium, the inner lining of the heart. This defect is rarely isolated; it is usually combined with problems of the aortic and tricuspid valves.
Blood does not flow in normal quantities from the atrium to the left ventricle, pressure increases in the system of the left atrium and pulmonary veins (through which arterial blood from the lungs enters the heart), an attack of pulmonary edema occurs. A little more detail: in the lungs, CO2 is replaced with oxygen in the blood, this happens through the smallest capillaries of the alveoli (vesicles), with a wall only one cell thick. If the blood pressure in the pulmonary capillary system increases, the liquid part is “pushed” into the cavity of the alveoli and fills them. When you inhale, the air “foams” this liquid, exacerbating the problem with gas exchange.
Picture of pulmonary edema: bubbling breathing, pinkish foam from the mouth, general cyanosis. In such cases, immediately call an ambulance, and before the doctors arrive, have the person sit down; if there is a diuretic in ampoules and you know how to give injections, administer the drug intramuscularly. The goal is to reduce the volume of fluid, thereby reducing pressure in the small circle and swelling.
Consequences: over time, if the problem is not solved, mitral lung is formed with tissue sclerosis and a decrease in the volume of the lungs useful for gas exchange.
Signs: shortness of breath, mitral flush and acrocyanosis, attacks of cardiac asthma (it is difficult to inhale, and with bronchial asthma it is difficult for a person to exhale) and pulmonary edema. If mitral stenosis appeared in childhood, then a decrease in the chest on the left (Botkin’s symptom), a lag in development and growth is visible.
Treatment and prognosis: it is important to determine in time how critically narrowed the mitral orifice is. If the narrowing is small, then the person lives a normal life, but if the area is less than 1.5 square centimeters, surgery is necessary. After it, you need to regularly undergo antirheumatic treatment courses.
Aortic valve insufficiency
Aortic heart defects are in second place in frequency, they are more common in men, and in 1/2 of cases they are combined with mitral defects. The cause can be both rheumatic and atherosclerotic changes in the aorta.
During systole (contraction and compression) of the left ventricle, blood passes into the aorta, this is normal. If the aortic valve does not close completely, or the aortic opening is dilated, then blood returns back to the left ventricle during its “relaxation” - diastole. There is overstretching and expansion of its cavity (dilatation), at first only compensatory (temporary “smoothing out” of discomfort to preserve function), and then the left atrium and mitral opening are stretched. As a result, we get stagnation in the small circle, hypertrophy of the muscular walls of the heart.
Signs: if the defect is decompensated, when measuring blood pressure, the lower number (diastolic pressure) may drop to almost zero. Patients complain of dizziness if the body position changes quickly (lying down and standing up), and attacks of suffocation at night. The skin is pale, the pulsation of the arteries in the neck (carotid dancing) and the shaking of the head are visible. The pupils of the eyes and the capillaries under the nails (visible when pressing on the nail plate) also pulsate.
Treatment: preventive – in case of compensated defect, radical – an artificial aortic valve is sewn in.
Prognosis: an isolated defect is found by chance in approximately 30% of cases during a routine examination. If the valve defect is small and there is no severe heart failure, people do not even suspect about the defect and live a full life.
Aortic stenosis, isolated defect
It is difficult for blood to escape from the left ventricle into the aorta: this requires more effort, and the muscular walls of the heart thicken. The smaller the aortic opening, the more pronounced the left ventricular hypertrophy.
Signs: associated with a decrease in the flow of arterial blood to the brain and other organs. Paleness, dizziness and fainting, heart hump (if the defect developed in childhood), attacks of pain in the heart (angina pectoris).
Treatment: we reduce physical activity, carry out restorative treatment - if there is no severe circulatory failure. In severe cases, only surgery, valve replacement or dissection of its valves (commissurotomy).
Combined aortic disease
Two in one: valve insufficiency + narrowing of the aortic mouth. This type of aortic heart disease is much more common than an isolated one. The signs are the same as for aortic stenosis, only less noticeable. In severe cases, stagnation begins in the small circle, accompanied by cardiac asthma and pulmonary edema.
Treatment: symptomatic and preventive - in mild cases, in severe cases - surgery, replacement of the aortic valve or dissection of its “fused” valves. The prognosis for life is favorable, with adequate and timely treatment.
Video: causes, diagnosis and treatment of aortic stenosis
Tricuspid (three leaflet) valve insufficiency
Due to the leaky closure of the valve, blood from the right ventricle is thrown back into the right atrium. Its ability to compensate for the defect is low, so stagnation of venous blood in the systemic circle quickly begins.
Signs: cyanosis, neck veins are congested and pulsating, blood pressure is slightly low. In severe cases - edema and ascites (fluid accumulation in the abdominal cavity). Treatment is conservative, mainly to eliminate venous stagnation. The prognosis depends on the severity of the condition.
Stenosis of the right atrioventricular (between the right atrium and ventricle) opening
The outflow of blood from the right atrium to the right ventricle is difficult. Venous congestion quickly spreads to the liver, it enlarges, then cardiac fibrosis of the liver develops - active tissue is replaced by connective (scar) tissue. Ascites and general edema appear.
Signs: pain and feeling of heaviness in the hypochondrium on the right, cyanosis with a yellow tint, always pulsation of the neck veins. Blood pressure is reduced; the liver is enlarged and pulsating.
Treatment: aimed at reducing swelling, but it is better not to delay surgery.
Prognosis: normal health is possible with moderate physical activity. activity. If atrial fibrillation and cyanosis appear, quickly consult a cardiac surgeon.
Summary: acquired – mainly rheumatic heart defects. Their treatment is aimed both at the underlying disease and at reducing the consequences of the defect. In case of severe circulatory decompensation, only surgery is effective.
Important! Treatment for heart defects may have a better chance of success if people see their doctor on time. Moreover, malaise as a reason for going to the doctor is not at all necessary: you can simply ask for advice and, if necessary, undergo basic examinations. A smart doctor does not allow his patients to get sick. An important note: the age of the doctor does not really matter. What is really important is his professional level, ability to analyze and synthesize, and intuition.
Step 2: after payment, ask your question in the form below ↓ Step 3: You can additionally thank the specialist with another payment for an arbitrary amount ↑
Nursing care for hospitalized children
Congenital heart defects in children are treated in a hospital setting, and in most cases surgically.
The nursing process in such cases is aimed at preparing children for surgery and at their speedy rehabilitation in the postoperative period.
Responsibilities of medical personnel in the pre- and postoperative ward:
- Provide complete information about the symptoms of the disease, its course, possible complications, prognosis, and tactics of medical interventions.
- Medical staff should provide support to parents at all stages of treatment.
- Create comfortable conditions, monitor the sanitary condition of the premises and carry out preventive measures aimed at combating infections inside the hospital.
- Prepare children for surgery and provide postoperative care.
- Carry out the necessary manipulations.
- Collect material for biological research.
- Measure the temperature and monitor the physical condition of the child.
- Ensure proper nutrition of hospitalized children.
How is the nursing process carried out for heart defects?
Other cardiac pathologies
07.10.2016
12.2 thousand
8.2 thousand
2 minutes.
Nursing process for patients with heart defects is important in the treatment of cardiovascular diseases. Nowadays, most deaths occur due to disorders of the cardiovascular system, in particular, heart defects become the cause of mass mortality. Let us dwell in more detail on the topic: nursing process for heart defects.
- 1. The essence of pathology
- 2. General principles of nursing
Heart defects are significant changes in the structure of valves and other components of the cardiovascular system, which result in a malfunction in intracardiac and systemic hemodynamics.
Acquired heart defects are valvular in structure. Valvular heart defects are as follows:
- defects in valve operation;
- orifice stenosis;
- combined valve defect and orifice stenosis;
- combinations of defective stenosis of the orifice and valve function;
- without a predominant combination of valve defects.
Valve stenosis is a narrowing of the opening in which the valve is located, formed by the fusion of several valves. Valve insufficiency is the failure of the valve to close during diastole, the reason for this is destruction or damage to the leaflets, as well as expansion of the fibrous ring of the valve, which is manifested by incomplete closure of the leaflets.
The defect can be compensated or decompensated. Compensation for a defect is when the defect is present, but there are no clinical manifestations of it. With decompensation, there is a defect and there are its symptoms.
The defect can be the result of rheumatism, endocarditis as an infectious disease, post-infarction cardiosclerosis, endocarditis in the case of systemic diseases.
As with other diseases, nursing care for patients suffering from heart defects is important. What is it and what is the purpose of such care?
The cardiac department nurse reports to the cardiologist and carries out her activities under his leadership.
In her work, the nurse is guided by job practice, as well as methodological recommendations aimed at improving the activities of mid-level medical personnel working in inpatient facilities, according to which she is obliged to:
- organize your working time rationally, both in the department and in the prevention room;
- do everything possible to reduce the risk of bacteria entering the patient’s body (follow the rules and regulations of work, store, disinfect and use instruments);
- carry out the stages of nursing care for patients (correctly assess the general condition of the patient at the time of admission, process data and information about his health, plan care with the consent of the patient, and also monitor the effectiveness of the measures taken);
- immediately and at a high-quality level ensure the implementation of procedures and doctor’s instructions, provide assistant assistance during medical procedures;
- promptly notify about detected complications and disturbances in the patient’s well-being that occur during medical procedures;
- ensure proper storage and use of materials and tools;
- interact with employees of the medical institution and other services acting in the interests of the patient;
- maintain medical records;
- take advanced training courses;
- carry out health education work in order to prevent and improve the health of patients.
In the situation of caring for patients suffering from diseases of the circulatory system, patients address the nurse with various complaints about their well-being. With heart defects, there is often the presence of pain in the chest area, palpitations, shortness of breath, suffocation, swelling, and a feeling of painful interruptions in the functioning of the heart.
When monitoring patients, a distinction is made between general-purpose and special-purpose measures.
General measures include constant care, monitoring changes in health status; the patient himself has a special need for these measures.
Special events include diagnosing heart diseases, preventing the occurrence of defects, conveying information to the population, and promoting a healthy lifestyle.
Source: https://vashflebolog.com/other-heart-diseases/sestrinskij-process-pri-porokax-serdca.html
Help in the rehabilitation of children with PS
In case of congenital heart defects, the main task of the hospital staff is to save the lives of children, which consists in carrying out measures aimed at preserving heart tissue and preventing complications.
To do this, the nurse, following the instructions of the doctors, administers antibiotics, immune correction drugs, and detoxification agents to young patients.
The tasks of the nurse at the stage of patient rehabilitation:
- Follow doctor's orders, perform manipulations and preventive measures.
- Report any problems to your doctor in a timely manner so that they can be resolved immediately.
- Prepare patients for surgery and provide support to parents.
- Give advice on dietary nutrition and monitor their implementation.
With congenital heart disease, emergency conditions often occur, such as shortness of breath, fainting, cyanosis; medical personnel must recognize these conditions in a timely manner and provide pre-medical care.
The nursing process includes preventive work with expectant mothers, aimed at a correct lifestyle that reduces the risk of having children with heart defects.
Nursing assistance in parent education
Children's hearts grow as quickly as they do, and the little patient's condition changes very quickly. Parents should be able to do a number of pre-medical and emergency procedures:
- First of all, parents must learn to provide assistance in case of choking.
- Congenital myocarditis can inhibit the mental development of a child; it is necessary to teach parents how to properly treat the patient so that he does not feel overprotective and does not turn into a capricious and weak touchy person.
- It is necessary to teach parents to treat each other with respect and understanding, and not to single out a sick child from other, healthy children.
- Parents must be able to properly conduct physical therapy. Make sure that the child does not overexert himself.
- Parents should understand the importance of constant monitoring of the child by a pediatric cardiologist. They should regularly take the baby for examination to the doctor. With congenital defects, the situation can change very dramatically, and instead of a planned operation, you will have to do an emergency one. All these changes are seen by a cardiologist, so visits to him should not be neglected.
- It is important to convince parents of the advisability of applying for disability and, as a result, financial benefits.
Nursing Process Performance Indicators
The main indicator of the effectiveness of the nursing process is the “observation sheet”, which records the sequence of treatment measures and basic hemodynamic parameters.
The document states:
- Rh factor and blood group;
- patient's age;
- reaction to medications;
- diet features;
- control over secretions;
- general dynamics of the state;
- Waterlow scale (assessment of the risk of pressure ulcers).
The observation sheet allows the nurse to properly organize the work and evaluate its results.
Assistance from medical staff during emergency surgery
Severe heart defects in newborns require immediate surgical intervention.
The nurse is creating a plan to prepare for surgery.
In terms of preparation:
- anamnesis;
- results of general examination;
- results of palpation, percussion and auscultation.
The staff collects material for tests, urine and blood, delivers the baby for x-rays, ultrasound, echo, cardiogram and other studies, and prepares the newborn for surgery.
The responsibilities of the nurse include conversations with parents and their psychological preparation for the upcoming operation of their child, as well as providing postoperative care.
Nursing care for acquired heart defects.
Heart disease is a violation of the anatomical structure of the heart and the resulting hemodynamic disturbance. There are vices:
1) Congenital - violation of the partitions between the atria and ventricles. They appear in early childhood. 2) Acquired - in 80% of cases are associated with the development of heart defects. - consequences of septic endocarditis, but the aortic valves are affected in isolation. - atherosclerosis (damage to all valves). - chronic syphilitic lesion - isolated position of the aortic valves. - diffuse connective tissue disease
Lecture No. 9 Topic: “Nursing care for heart disease”
Lecture
№ 9
Topic: “Nursing care for heart disease”
Content:
—
Congenital heart defects (CHD)
— Rheumatism
The formation of the heart occurs at 3-8 weeks of intrauterine development. By the end of the 4th week, the heart begins to contract, by the end of the 6th it has a four-chamber structure, and by the 8th week the heart is almost anatomically formed.
UPS
- these are anomalies in the morphological development of the heart and great vessels that arise as a result of disruption of the processes of embryogenesis.
Etiology:
1 – genetic inheritance (CHD in 1st degree relatives) – the risk level is 30-50%
2 – viral diseases of the mother during pregnancy (rubella, influenza, herpetic, enterovirus infections, etc.) 3 – chronic diseases of the mother, occurring with hypoxia (BA, HD, DM, etc.) 4 – occupational hazards (paint and varnish production, hairdresser, in beauty salons, etc.) 5 – mother’s age over 35, father’s age over 50 6 – intoxication (alcohol, nicotine, etc.) 7 – intrauterine infections
Classification
:
1- defects with enrichment of MCC
(MPC - pulmonary circulation) – PDA (patent ductus arteriosus), ASD (atrial septal defect), VSD (ventricular septal defect).
2 – defects with depletion of the ICC
— ISPA (isolated pulmonary artery stenosis - without cyanosis), tetralogy of Fallot (with cyanosis)
3 – defects with depletion of BCC
(BCC - systemic circulation) – coarctation of the aorta (without cyanosis)
4- defects without hemodynamic disturbances
- anomalies in the location of the heart and blood vessels, etc.
Common clinical manifestations that suggest the presence of congenital heart disease:
- deformation of the chest on the left or in the middle - changes in skin color: pallor, cyanosis or acrocyanosis (cyanosis of the heels, fingers, tip of the nose, ears, chin) - shortness of breath, especially at rest - changes in heart rate, pulse quality - pathological pulsation of blood vessels - expansion of the borders of the heart - systolic murmur in the heart area (25%) - retardation in physical development
Phases of development of defects:
Phase 1 of primary adaptation (emergency) lasts 1 year - the child adapts to hemodynamic disturbances. 2-phase of relative compensation from 2 to 5 years. Phase 3 is terminal, occurs after the exhaustion of protective adaptive mechanisms and is characterized by a circulatory disorder that cannot be treated.
Defects with MCC enrichment:
PDA – patent ductus arteriosus (Ductus Arteriosus)
Normally, the ductus arteriosus ceases to function and closes in the first hours, days, and less often in 2-3 months of life. When the duct is not closed, part of the blood is discharged from the aorta into the pulmonary artery, resulting in hypervolemia of the ICC. Clinical manifestations of PDA
: shortness of breath, pain in the heart area, increased fatigue (children suck sluggishly, with breaks for rest), an increase in the size of the heart; upon auscultation in the second intercostal space to the left of the sternum, a rough, “machine” systolic murmur is detected, which is carried out on the aorta, cervical vessels and in the interscapular region. Children with PDA often and for a long time suffer from bronchitis and pneumonia, while the symptoms of intoxication are not pronounced, but a large number of moist rales are always heard.
ASD – atrial septal defect
Blood through the defect in the septum is partially thrown from the left atrium to the right. In the right half of the heart, pressure increases, and hypertrophy of the right atrium develops. First clinical manifestations
appear at 5-6 months - cough, frequent acute respiratory infections, poor weight gain, pale skin. With a small defect there are no complaints. The defect is diagnosed most often at 2-3 years of age. During auscultation, a systolic murmur is heard in the 2-3 intercostal space to the left of the sternum, and sometimes dilatation and pulsation of the neck veins are noted.
VSD – ventricular septal defect
If the defect
is located
in the muscular part of the septum
, the diameter of the hole is not large (up to 1 cm) and hemodynamic disturbances do not affect the child’s condition.
There are no complaints, however, upon auscultation, a rough, scraping systolic murmur is heard with the epicenter in the 4-5 intercostal space to the left of the sternum. Defects in the membranous part
are wider and a significant part of the blood from the left ventricle is discharged into the right.
Both ventricles work under heavy load. Clinically,
the patient has rapid fatigue, shortness of breath, periodic cough, cyanosis, retardation in physical development, and chest deformation. The borders of the heart are expanded, the apical impulse is high, diffuse, and displaced downward. On auscultation there is a systolic murmur to the left of the sternum, which is carried out in all directions.
Defects with depletion of the ICC:
ISLA – isolated pulmonary artery stenosis
With this defect, the ejection of blood from the right ventricle into the pulmonary artery is difficult. Clinically the defect
manifested by complaints of fatigue, pain in the heart, shortness of breath.
Noticeable pallor
. In the 2nd intercostal space to the left of the sternum, a rough systolic murmur is heard, which is carried to the left subclavian region and to the carotid arteries. The first sound at the apex of the heart is enhanced, the second sound at the pulmonary artery is weakened or absent.
Tetralogy of Fallot
The defect includes a combination of four anomalies:
1 – pulmonary artery stenosis; 2 – ventricular septal defect; 3 – transposition of the aorta to the right; 4 – right ventricular hypertrophy. The ICC is not sufficiently supplied with blood; mixed blood enters the BCC through the aorta, which is located above the defect in the interventricular septum - arterial from the left and venous from the right ventricle. Due to narrowing of the pulmonary artery and increased pressure in the aorta, the right ventricle hypertrophies.
Clinic
: the first sign of the defect is
shortness of breath
, which appears first during feeding and anxiety, and then at rest.
Cyanosis
is rarely noticeable immediately after birth, most often appearing by 2-3 months.
From birth, a rough systolic murmur
in the
2-3 intercostal space
.
As a rule, children lag behind in physical and psychomotor development; after a year, deformation of the fingers appears - “drumsticks”;
epigastric pulsation and systolic trembling to the left of the sternum are detected.
On the Rg -gram, the shadow of the heart is in the form of a “shoe”;
in the peripheral blood there is
polycythemia
(increased hemoglobin and red blood cells).
Dyspnea-cyanotic crises
are not uncommon , which are accompanied by increased shortness of breath and cyanosis, loss of consciousness, and convulsions in infants. Older children experience milder attacks, during which the child assumes a forced squatting position. Children complain of headaches, dizziness, and may faint. Complications: hypoxic coma, thromboembolism, septic (abscesses, endocarditis), bleeding, dystrophy, heart failure.
Defects with BCC depletion:
Coarctation of the aorta –
This is a narrowing of the aorta in the lower thoracic or abdominal region, as a result of which the vessels of the lower half of the body receive little blood, and above the narrowing site, on the contrary, hypertension is observed.
Clinic:
complaints appear late and are associated with hypertension syndrome and cardiac decompensation.
Boys get sick more often. Patients complain of headaches, dizziness, tinnitus, nosebleeds, and cold feet
.
Upon examination, the better development of the upper half of the body in comparison with the lower half is striking. Characteristically, high blood pressure in the arms (up to 250-300 mm Hg) and at the same time a decrease in it in the lower extremities, sometimes to 0
(normally, blood pressure in the legs should be 15 - 20 mm Hg higher than in the arms) Pulse weak on the lower extremities, tense on the upper extremities.
On the Rg-gram of the chest there are “uria” on 4-9 pairs of ribs. Complications:
aortic rupture, heart failure, hemorrhagic stroke, development of aortic aneurysm.
Diagnosis of congenital heart disease
is based on anamnesis data, characteristic clinical manifestations and data from additional research methods: ECG, PCG, Rg-gram of the chest organs, cardiac angiography, ultrasound, probing of the cardiac cavities.
Treatment of congenital heart disease
. The main method is surgery, which leads to normalization of hemodynamic disorders. The most favorable period for surgery is 3–12 years. Conservative treatment includes emergency care for acute heart failure and hypoxic attack, treatment of complications and supportive care.
Rheumatism
is a systemic disease of connective tissue of an infectious-allergic nature with primary damage to the heart, as well as joints and the nervous system. It is most common in children aged 7-15 years.
Etiology.
Causes β-hemolytic streptococcus gr. A.
It begins 2-3 weeks after a sore throat or scarlet fever (or other streptococcal infection).
There are three main forms of the rheumatic process:
1. Rheumatic carditis - damage to all three membranes of the heart.
2. Polyarthritis – damage to the joints.
3. Chorea – damage to the nervous system.
Rheumatic carditis clinic:
I. Myocarditis
- damage to the heart muscle. In children with rheumatism it occurs in 100%.
1. The temperature is often low-grade or normal,
2. cardialgia (pain in the heart area),
3. tachycardia turning into bradycardia,
4. expansion of the borders of the heart to the left,
5. dullness of heart sounds,
6. systolic murmur, often at the apex of the heart.
P. Endocarditis
– damage to the inner lining of the heart and valves, most often the mitral, less often the aortic.
1. the temperature is always elevated,
2. the borders of the heart are expanded, up and to the left,
3. The main syndrome of endocarditis is a systolic murmur of a “blowing” nature at the apex of the heart and an increase in the second sound in the pulmonary artery. In approximately 10% of patients, the aortic valve is affected. This is manifested by a diastolic murmur along the left sternal border.
III. Pericarditis
- damage to the outer lining of the heart (pericardium.)
1. the child’s condition is very serious,
2. the temperature is always elevated,
3. shortness of breath,
4. general cyanosis,
5. severe pain in the heart, due to which children take a forced sitting position,
6. on auscultation – sharp dullness of heart sounds and arrhythmia.
Polyarthritis Clinic:
The medium and large joints of the extremities (knees, elbows, ankles) are symmetrically affected. There is pain and limitation of movement. The skin over the joint is hyperemic, swollen, and hot to the touch.
The main differential differences between rheumatic arthritis and rheumatoid:
1. The pain is fleeting;
2. Rheumatic arthritis goes away without a trace after treatment, leaving no joint deformities.
Chorea
is a lesion of the nervous system. It begins gradually: sleep and school performance worsen. The child becomes absent-minded, whiny, and irritable. After 1-2 weeks, the main symptom of chorea appears - hyperkinesis
(involuntary erratic movements, twitching of the muscles of the face and limbs, intensifying with emotions and disappearing during sleep). The child constantly grimaces, his handwriting changes, his gait becomes unsteady and uncertain.
Diagnostics.
Based on medical history and clinical data + AOC, where ESR and leukocytosis are always elevated. In a biochemical blood test: “C” reactive protein appears, dysproteinemia, increased fibrinogen, increased titer of antistreptolysin - 0 (ASL - 0), antistreptohyaluronidase (ASH), antistreptokinase (ASA).
Treatment (in hospital):
1. Strict bed rest (duration is determined by the doctor) from 1 week to 1 month or more. Extension of the regimen only with the permission of the doctor. Child care is carried out in bed (combing, washing, feeding). Physiological functions using a bedpan.
2. Bed rest (2-3 weeks). The child is allowed to take part in board games in bed.
3. Gentle regime with permission to walk to the dining room and to the toilet.
The implementation of the regime must be strictly monitored by the m/s of the ward. With prolonged bed rest, bedsores may develop. Therefore, careful skin care is necessary. The child's bed should be comfortable, it must be remade, eliminating folds.
Drug treatment:
1. Penicillin antibiotics
(amoxicillin, augmentin).
Macrolides
(spiramycin, etc.),
oral cephalosporins
(cephalexin, cefaclor) from 750 thousand units to 2 million per day for about 10 days, then
bicilin - or bicilin 1
.
2. Anti-inflammatory drugs
(Voltoren, Brufen) +
antihistamines
,
3. Drugs that support the heart muscle: these are potassium drugs (panangin, potassium orate) - vitamins, ATP, KKB.
4. Hormones (in severe cases),
5. For chorea, bromine preparations, nootropil, valerian.
Nutrition:
complete, fortified, rich in potassium (raisins, dried apricots, prunes, baked potatoes, cabbage). Slightly limit proteins, fats and salt.
"D" observation:
Have been with a rheumatologist for at least 5 years, sometimes transferred to the adolescent office.
Monitoring of OAK, ECG, FCG, consultation with ENT, dentist, neurologist is carried out.
Prevention:
1. Primary (prevention of rheumatism itself) is the sanitation of foci of chronic infection, treatment of streptococcal infection.
2. Secondary – prevention of exacerbation of rheumatism: Bicillin and anti-inflammatory drugs in courses in spring and autumn. Honey. withdrawal from prof. vaccinations individually (decided by a rheumatologist).
The topic is vast
Acquired heart defects
Nursing process for heart defects
Heart defects are the result of organic lesions of the valve apparatus of the heart, which leads to circulatory disorders. Defects can be congenital or acquired.
Acquired ones are much more common
heart defects resulting from rheumatism, syphilis, infective endocarditis, atherosclerosis, chest trauma, etc.
There are heart defects: mitral
(
valve
and stenosis of the left mitral orifice),
aortic
(aortic valve insufficiency and aortic stenosis),
tricuspid
(usually tricuspid valve insufficiency),
pulmonary valve defects
(
ostial stenosis and
valve insufficiency).
Mitral and aortic heart defects are much more common.
Heart defects can be complex or combined, when valve insufficiency and orifice stenosis occur simultaneously. In this case, the signs of two defects are combined.
In addition, there are combined heart defects,
when there are heart defects localized on different valves, most often mitral-aortic, for example, mitral stenosis and aortic valve insufficiency. And in this case, the signs of defects are combined.
In most cases, congenital heart defects and developmental anomalies of large vessels are defects of the embryonic development of the cardiovascular system.
Congenital defects
the development of heart valves and blood vessels is divided into: 1) defects with increased blood flow through the lungs; 2) defects with normal blood flow through the lungs; 3) defects with reduced blood flow through the lungs.
Acquired heart defects
Mitral valve insufficiency. This type of heart defect is characterized by incomplete closure of the valves during left ventricular systole as a result of damage to the valve apparatus.
Etiology
.
The mitral valve is affected by atherosclerosis, rheumatism (organic lesions);
with excessive expansion of the left ventricle, fibrous ring and circular muscles of the atrioventricular orifice (myocarditis, cardiopathy, myocardial infarction) -
relative valve insufficiency.
With endocarditis, deformation of the valve occurs, shortening of the valve leaflets, as well as the tendon strands attached to them. There is an obstacle to the approach of the valves during systole.
Normally, in the systole phase, the atrioventricular orifice is tightly closed, all blood from the left ventricle
enters
the aorta.
In mitral valve insufficiency, some
blood volume returns to the atrium during
systole
.
The volume of blood
in the atrium increases.
Constant overflow of the left atrium causes an increase in pressure in it, as a result of which expansion of its cavity and muscle hypertrophy develops. More than normal blood will flow into the left ventricle, which subsequently causes expansion of its cavity and myocardial hypertrophy.
Mitral valve insufficiency is compensated by hypertrophy of the myocardium of the left ventricle and atrium. In some cases, the left atrium, expanding, is no longer capable of completely emptying the blood, resulting in stagnation of blood in the left atrium, and then in the pulmonary circulation. Congestive circulatory failure develops - heart failure.
Etiology
Acquired heart defects are diseases based on morphological and/or functional disorders of the valve apparatus (valve leaflets, annulus fibrosus, chordae, papillary muscles), developed as a result of acute or chronic diseases and injuries, disrupting the function of the valves and causing changes in intracardiac hemodynamics .
ACQUIRED HEART DEFECTS
Questions: Acquired heart defects. Definition. Etiology. Classification. Hemodynamic disturbances due to heart defects. The concept of “compensation”, “decompensation”.
Differential diagnosis of the main types of heart defects (mitral, aortic). Course and complications. Principles of treatment (conservative, surgical). Nursing. Dynamic observation.
Heart defects and pregnancy.
Frequency. PPPs occur in 1.4-2% of the population and lead to permanent disability.
1. rheumatism – more than 75% of cases (in young patients in 95-97%)
2. infective endocarditis
3. atherosclerosis and calcification 25%
4. syphilis – causes aortic valve disease
5. myocardial infarction
6. other, rare causes
There are two types of teaching staff:
1) Valve insufficiency , when altered and deformed valves do not completely close the valve opening and blood flows back through the resulting gap;
2) Stenosis of the valve opening , most often due to fusion of the valve leaflets at the base, and an obstacle to the free flow of blood occurs.
If there is simultaneous damage to the heart valve such as stenosis and insufficiency, the defect is considered combined, and if different valves are affected, it is considered combined. Combined defects can be with a predominance of stenosis, insufficiency, or without a clear predominance.
When making a diagnosis of a combined defect, the more pronounced lesion is given first place. For example,
combined heart disease: combined mitral disease with predominant stenosis, aortic valve insufficiency.
More than half of all acquired heart defects occur in lesions of the mitral valve and about 10–20% in the aortic valve.
Defects of rheumatic etiology are characterized by the formation of combined and combined forms of lesions.
Pulmonary valve and tricuspid valve defects in isolated form are rare. More often there is a relative insufficiency of these valves, caused by increased pressure in the pulmonary artery.
The formation of the defect lasts 1-3 years.
Classification of defects (New York Association of Cardiac Surgeons).
According to this classification, all defects can be divided into 4 classes.
1. The first functional class - there is a defect, but there are no changes in the parts of the heart (the defect is insignificant), an example is mitral valve prolapse.
2. Second functional class - there are changes in the heart, but they are reversible. There are no changes in other organs. The success of the operation is 100%.
3. Third functional class - irreversible changes in the heart and reversible changes in other organs appear.
4. The fourth functional class is characterized by the appearance of irreversible changes on the part of other organs and systems.
This classification makes it possible to assess the prognosis of working capacity and give recommendations regarding physical activity.
The clinical manifestations of any PPS can be included in three main syndromes:
valve syndrome
· syndrome of a pathological process that led to the development of heart disease (rheumatism, infective endocarditis, etc.);
· syndrome of systemic circulatory disorders (most often chronic heart failure).
Heart valve syndrome includes two groups of symptoms: direct (valve) and indirect, or indirect.
The appearance of direct symptoms
caused by impaired functioning of a pathologically altered valve. Their presence makes the diagnosis of the defect reliable.
These signs include palpation-detectable phenomena of systolic or diastolic tremors (“cat’s purring”), data from auscultation of the heart (changes in tones, the appearance of noise and additional tones), the results of phonocardiography and ultrasound examination of the heart (the state of the chords, valves, features of their movement in the same direction). or another phase of the cardiac cycle, the area of the valve openings, the presence of reverse blood flow).
To indirect symptoms
include: compensatory hypertrophy and dilation of various parts of the heart, impaired blood flow in various vascular areas.
The severity of indirect signs (presence of heart failure) characterizes the severity of the defect.
Compensated heart defects are defects that are not accompanied by circulatory failure.
Decompensated heart defects are defects accompanied by circulatory failure in the pulmonary or systemic circulation.
STENOSIS OF THE LEFT ATRIOVENTRICULAR ORIFICE (mitral stenosis)
Stenosis of the left atrioventricular orifice is the most common acquired heart defect. In almost all cases, it develops as a result of rheumatic endocarditis.
The essence of the anatomical changes is the fusion of the valve leaflets along the free edge, sclerosis of them and tendon threads. The valve takes the form of a funnel or diaphragm with a narrow hole in the middle.
Hemodynamic changes. The area of the left atrioventricular orifice in healthy individuals is 4-6 sq.cm.
Significant hemodynamic disturbances develop when the cross-section of the opening decreases to 1.5 cm2.
The narrowing of the mitral orifice creates an obstacle to the expulsion of blood from the left atrium, which becomes overfilled with blood (remaining in the atrium and flowing through the pulmonary veins).
To ensure normal blood filling of the left ventricle, a number of compensatory mechanisms are activated:
1. Acceleration of blood flow through a narrowed opening is ensured by hypertrophy of the left atrium, and then by its dilatation (expansion) and an increase in pressure in it and further in the pulmonary veins, capillaries, arterioles and pulmonary artery. Pulmonary hypertension develops.
2. A further increase in pressure in the left atrium and pulmonary veins due to irritation of baroreceptors causes a reflex constriction of arterioles (Kitaev reflex).
The Kitaev reflex protects the pulmonary capillaries from excessive increases in pressure and sweating of the liquid part of the blood into the cavity of the alveoli, but the narrowing of the pulmonary arterioles leads to a significant increase in pressure in the pulmonary artery.
Prolonged spasm of arterioles leads to narrowing of the lumen and diffuse sclerotic changes in the pulmonary artery.
3. Reducing the lumen of the pulmonary artery increases the load on the right ventricle, which causes its hypertrophy, and then dilatation.
4. A significant increase in pressure in the pulmonary artery and right ventricle makes it difficult to empty the right atrium, which leads to an increase in pressure in its cavity and the development of hypertrophy, and then to dilatation. Decompensation develops in the systemic circulation.
Didn't find what you were looking for? Use the search:
Source: https://studopedia.ru/1_90454_etiologiya.html
First presentation slide: Nursing care for heart defects
Heart disease is a persistent defect in the structure of the heart, characterized by anatomical changes in the valve apparatus and large vessels, leading to impaired hemodynamics and cardiac function.
Types of heart defects: congenital - formed during the intrauterine development of the fetus and in most cases are diagnosed in childhood. Acquired developmental defects are often combined with other developmental defects - they arise as a result of some disease (rheumatic fever, atherosclerosis, infective endocarditis, etc.)
Under the influence of etiological factors there may be: valve insufficiency - due to a violation of the integrity of the valves, their wrinkling, when the edges become uneven, leading to their incomplete closure and regurgitation of blood (reverse flow); orifice stenosis - due to fusion of adjacent valves, narrowing of the opening to which the valves are attached, which leads to insufficient blood flow.
Types of defects: isolated - damage to 1 valve or 1 orifice; combined - damage to both valve and orifice (mitral stenosis + insufficiency); combined - mitral-aortic, mitral-aortic-tricuspid defect. Phases of the course of defects: compensation: despite the presence of a defect, the heart copes with its work due to compensatory mechanisms, which include muscle hypertrophy and dilatation of the cavity; decompensation: the heart cannot cope with its work and blood stagnates, first in the cavities, and then in the circulation (small, then large), which is accompanied by symptoms of heart failure. With stagnation according to the ICC: shortness of breath, attacks of suffocation, cough with pink serous sputum, hemoptysis, cyanosis, pulmonary edema. With stagnation according to the BCC: swelling of the extremities, enlarged liver and its pain, ascites, hydrothorax, hydropericardium, anasarca.
Diagnosis of heart defects: anamnesis: history of ARF in childhood and adolescence; external examination: cyanosis, pallor of the skin, the presence of pathological pulsations, chest deformities (heart hump), etc. auscultation: changes in tones, the appearance of noises.
Types of acquired defects and their symptoms
There are different types of acquired defects, which have different manifestations and developmental features.
Mitral regurgitation
The pathological condition is characterized by incomplete closure of the left atrioventricular orifice by the bicuspid valve during contraction. Because of this, blood is thrown back into the atrium.
The defect develops as a result of myocarditis, myocardial dystrophy. These pathologies weaken the circular muscle fibers or affect the papillary muscles, which are involved in closing the valve during systole.
Relative insufficiency is not accompanied by modification of the mitral valve, but the opening increases in size, and the leaflets cannot close it completely.
An organic form of deficiency may occur. Endocarditis due to rheumatism has a particular impact. It is characterized by the formation of connective tissue on the valve leaflets, gradually causing them to shrink and shorten. Under the influence of these changes, the valves cannot close completely and form a gap through which blood flows back into the atrium cavity.
Functional deficiency disrupts the functioning of the muscular system that regulates valve closure. In this case, the blood is thrown back into the left ventricle, and from it enters the atrium.
If the heart compensates for this violation, then the patient does not feel any discomfort and is no different from a healthy person. At this stage, the disease can remain for quite a long time, but if the contractility of the myocardium weakens, a stagnant process develops in the blood circulation.
With decompensation, the patient suffers from:
- shortness of breath;
- sensations of heartbeat;
- cyanosis;
- swelling of the lower extremities;
- painful and enlarged liver;
- acrocyanosis;
- swelling of blood vessels in the neck.
Symptoms increase gradually with the development of deterioration of blood circulation and oxygen deficiency.
Mitral stenosis
The atrioventricular opening narrows as a result of a long course of rheumatic or infective endocarditis.
Stenosis of the orifice occurs if the valve leaflets become compacted and fused.
The mitral valve takes the shape of a funnel with a gap in the middle. With a long course of the disease, calcification of the valve tissue occurs.
With the development of pathology, a person develops:
- shortness of breath;
- cough with blood in the sputum;
- interruptions and pain in the heart area.
Examination will show that the patient is very pale, and his cheeks are covered with a thick blush. In this case, children may be infantile, suffer from insufficient physical development, and there is a protrusion of the chest due to a strong heartbeat.
The pulse rates in both arms with stenosis are different. There is a risk of developing atrial fibrillation.
Aortic insufficiency
If the semilunar valves, which should close the opening of the aorta, do not completely close, the blood from the aorta returns to the cavity of the left ventricle during relaxation. This condition is called aortic regurgitation.
The pathological process develops when:
- Rheumatic endocarditis.
- Infective endocarditis.
- Atherosclerosis.
- Syphilis.
- Injuries.
During rheumatism, under the influence of inflammatory and sclerotic processes, the valves are shortened.
If a person has syphilis or atherosclerosis, then the pathological process affects the aorta itself. It expands and pulls back the valve flaps.
During the septic process, parts of the valve disintegrate, defects form on them, they become scarred and shortened.
At the initial stages of development, the work of the left ventricle increases, due to which there is no deterioration of the condition. Coronary insufficiency gradually develops, causing pain in the heart. They are associated with hypertrophic changes in the myocardium.
Decompensated heart disease manifests itself:
- Weakness.
- Pale skin.
- Pulsation in the area of large arteries.
- Rhythmic shaking of the head.
- Changes in nail color.
- Constriction of the pupils during contraction and dilation during relaxation.
These manifestations cannot be ignored. It is necessary to urgently visit a doctor and undergo an examination.
Aortic stenosis
Due to the narrowing of the aorta, blood does not enter it from the left ventricle during contraction.
With severe stenosis and insufficient blood ejection into the arteries, manifestations of decompensation are observed. Symptoms will be different, depending on which area the blood supply is disrupted:
- Myocardium. The patient has pain in the heart area similar to angina pectoris.
- Brain – pain and dizziness, possible loss of consciousness.
The clinical picture becomes more pronounced if the patient is exposed to physical or emotional stress.
Since the vessels are not filled enough with blood, the skin turns pale, the pulse becomes rare, and blood pressure decreases.
Also read: Cardiac asthma: causes, symptoms, diagnosis and treatment, prognosis
Tricupidal insufficiency
Abnormalities are observed in the structure and function of the tricuspid atrioventricular valve. The disease occurs if a person suffered from rheumatism, sepsis, or received a serious injury to the heart area.
Usually the problem is combined with others; it is very rarely observed in isolated form.
Insufficiency is accompanied by stagnant processes in the venous vessels. It leads to:
- swelling;
- accumulation of fluid in the abdominal cavity;
- feeling of heaviness on the right under the ribs;
- pain associated with an increase in liver size;
- blue discoloration of the skin;
- swelling and pulsation of the veins in the neck.
In this condition, there is an increase in pressure in the veins. Congestive processes that occur with tricuspid defects cause the development of severe heart failure, malfunctions of the liver, kidneys, and gastrointestinal tract.
In serious cases, connective tissue begins to develop in the liver, causing the formation of cardiac fibrosis and severe metabolic disorders.
Combined defects
Defects that arise as a result of rheumatism are often combined. Stenosis can be combined with insufficiency, and several valves are simultaneously affected.
Of all the combined defects, the most common are mitral valve insufficiency and orifice stenosis.
Such defects in the initial stages are accompanied by shortness of breath and bluish discoloration of the skin.
With more developed mitral insufficiency, changes in blood pressure and pulse do not occur. If stenosis is more developed, then pulse and systolic blood pressure decrease, and diastolic blood pressure increases.
Combined aortic defects usually occur under the influence of rheumatic endocarditis.
With combined defects, symptoms are observed that are characteristic of each lesion individually. In this case, it is very important to identify which valve is most affected in order to select a treatment method and make a prognosis for the future.
Slide 8: DMI
ECG: atrial and ventricular hypertrophy, heart rhythm disturbances. X-ray of the heart in three projections: enlargement of individual cavities of the heart, state of blood circulation in the pulmonary circle. EchoCG: the most informative method for studying the heart.
Invasive methods (in cardiac surgery hospitals according to strict indications): probing of the right and left parts of the heart with manometry, study of the gas composition of blood from the cavities of the heart, contrast radiological methods. EPI (transesophageal echocardiography)
Slide 11: Mitral stenosis
Complications of mitral stenosis: cardiac asthma, pulmonary edema, pulmonary artery aneurysm, arrhythmia (MA, TP), thromboembolism.
Treatment of mitral stenosis: Basic principles: treatment of the underlying disease; regimen: limitation of physical activity (starting with a moderate degree of narrowing of the A V hole), diet with limited salt and fluid; drug therapy: for tachycardia - beta-blockers; for pulmonary hypertension, CHF - diuretics; cardiac glycosides. surgical treatment - commissurotomy
Until recently, patients with heart defects only underwent open heart surgery. To gain access to the problem area, surgeons opened the chest. Fortunately, modern technologies make it possible to perform surgical interventions in a gentle way. Now it is possible to eliminate a heart defect using a special device that opens like an umbrella and completely covers the defect of the cardiac septum.
Slide 18: Mitral regurgitation
As an isolated defect, it is rare, most often with stenosis (combined mitral disease) Causes of mitral regurgitation: ARF IHD syphilis infective endocarditis dilated cardiomyopathy
Clinical picture: Complaints: In compensated MN, the defect is detected by chance. As it progresses, complaints of shortness of breath during exercise, palpitations, and then at rest; attacks of cardiac asthma: cough is dry or with a small amount of sputum, often mixed with blood (hemoptysis). Pain in the heart area (more often than with MS): aching, stabbing, pressing; not always associated with physical activity.
Complications of mitral regurgitation: thrombosis, cardiac arrhythmia, embolism (in the kidneys, spleen, limbs, brain) acute left ventricular failure (pulmonary edema) AMI
Treatment of mitral regurgitation: prevention of rheumatism, infective endocarditis treatment of the underlying disease regimen: limitation of physical activity (for moderate and severe MR) drug therapy: anticoagulants, ACE inhibitors, nitrates, calcium antagonists, diuretics, cardiac glycosides surgical treatment - valve replacement (before the development of LV decompensation )
Respiratory failure and its manifestations
Have you been trying to cure HYPERTENSION for many years?
Head of the Institute of Treatment: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
Respiratory failure (RF) is not an independent disease, but is considered a syndrome accompanying pathological conditions with impaired oxygen metabolism in the lungs.
With this process, disturbances occur either in the composition of blood gases, or its maintenance occurs due to overstrain of the system that provides external respiration.
What types are there?
This symptom is divided into acute and chronic process.
Acute respiratory failure manifests itself very quickly. With it, the clinical picture develops within a matter of hours, and without urgent assistance it poses a serious threat to human life. It may occur in the presence of a chronic process during its exacerbation.
Chronic deficiency can occur in a patient for many years. It occurs as a result of certain types of diseases, as well as the result of an acute process that is not fully cured.
There are three degrees of severity of respiratory failure:
- First degree - shortness of breath appears only when overloaded.
- The second is characterized by shortness of breath when performing daily activities.
- In the third degree, shortness of breath is constantly present, even with complete rest.
Based on the type of gas exchange disorder, hypoxemic and hypercapnic forms are distinguished.
What pathology causes the disease?
To provide assistance with this condition, it is very important to know what pathological processes can lead to its development. Due to the occurrence of DN, it is divided into several types:
- obstructive. With this type, there is difficulty in exhaling. Occurs in bronchial asthma, foreign body in the respiratory organs, bronchitis, compression of the trachea and bronchial tree, or their structure.
- Restrictive. With it, the maximum ability to inhale is impaired. It is observed in pneumosclerosis, pneumothorax and other pathologies localized in the cavity between the layers of the pleura. Sometimes the cause is impaired mobility of the ribs due to kyphoscoliosis.
- Mixed. With a long-term problem in the heart muscle and pulmonary system, in some cases a mixed type of failure develops, with one of them still predominant.
- Hemodynamic. Occurs due to hemodynamic disorders. Most often observed with thromboembolism, when part of the lung is blocked, or with heart disease (due to mixing of venous and arterial blood).
Respiratory failure in children often occurs due to acute inflammatory processes, or as a result of congenital disorders of the structure of the respiratory organs.
Manifestation of the syndrome
In the classic version, the pathology manifests itself in the form of increased breathing, which refers to the body’s compensatory reactions in response to a lack of oxygen.
This syndrome is sometimes accompanied by paradoxical movements of the chest. When examined, the patient is characterized by a posture in which he sits, leaning on his outstretched arms and leaning forward a little.
Since an increase in pressure occurs in the pulmonary circulation, the body reacts to this condition with a rapid heartbeat.
Oxygen starvation of the brain leads to the fact that in an acute condition the patient may lose consciousness. Sometimes, as the amount of carbon dioxide in the blood increases, coma develops and the patient may die.
When measured, such a patient has a decrease in pressure; many diseases that end in respiratory failure are accompanied by a dry or wet cough.
Oxygen starvation of brain cells, combined with problems in the functioning of the heart, leads to fear of death and overexcitation. Tissue ischemia leads to blue discoloration of the skin (acrocyanosis).
Hypertension will go away, and the pressure will be 120 over 80 if you include it in the diet...
Hypertension will disappear forever! Here's the secret...
On examination, a sign of chronic failure is the syndrome of “drumsticks” and “watch glasses” (characteristic thickening of the terminal phalanges of the fingers and nails).
How to help with respiratory failure?
Methods of providing assistance depend on the severity of the process. During the development of an acute condition, the patient requires emergency assistance to restore free breathing.
For chronic deficiency, treatment is predominantly symptomatic.
Acute failure
Only an experienced specialist can provide it; depending on the reason, it is carried out in several stages:
- performing mechanical ventilation;
- removal (if any) of a foreign body;
- tracheostomy;
- puncture of the pleura with removal of fluid;
- relief of edema;
- relieving an asthmatic attack.
In case of acute deficiency, antibacterial drugs are also used if the cause is bacterial inflammation. In case of pulmonary vein thrombosis, administration of thrombolytics is necessary, and in case of poisoning, detoxification is necessary.
Chronic failure
Most often, providing care for chronic failure does not require the patient to stay in the hospital, except in cases where an exacerbation occurs.
The patient undergoes regular examination and examination, and takes the treatment prescribed by the doctor.
Drug therapy
The following medications are commonly used:
- Respiratory analeptics.
- Diuretics.
- Mucolytic and expectorant agents.
- Bronchodilators.
- Glucocorticoids.
Diet
The diet of such a patient should be varied to meet the needs of the body and strengthen it. Dishes should contain a lot of proteins and vitamins.
If necessary, the patient takes additional vitamin complexes.
Salt and foods that cause excess gas formation in the intestines are subject to restrictions. To improve the general condition of the patient, it is recommended to adhere to the regime, eliminate bad habits, and use physiotherapy and traditional medicine.
In the most extreme case, the doctor may suggest a lung transplant. However, this operation is very expensive and does not always lead to a positive result.
Slide 26: Aortic stenosis
Causes of development: ARF atherosclerosis syphilis infective endocarditis Clinical and hemodynamic disorders occur when the opening is narrowed by 70% or more.
Clinical picture: In the compensation stage - no complaints, patients are able to tolerate significant physical activity. In the stage of decompensation - dizziness, sudden staggering when walking, lightheadedness, fainting during physical exertion; some have attacks of severe weakness with darkening of the eyes, forcing them to stop for rest. A typical combination of dizziness and fainting with attacks of retrosternal pain of an anginal nature: they occur at the height of physical activity, compressive, pressing, localized behind the sternum, radiating to the left arm, stopping at rest. Shortness of breath due to cerebrovascular accident, attacks of cardiac asthma. There may be palpitations, increased fatigue, swelling in the legs, heaviness and pain in the right hypochondrium. Examination: - pale skin or acrocyanosis. - increased apical impulse, pathological pulsation in the region of the heart. Palpation: The apical impulse is strengthened and diffuse, can shift to the VI m/r, outward from the midclavicular line. In the II m/r to the right of the sternum and in Botkin’s point - systolic trembling (in the position on the right side while exhaling); M.B. in the jugular, supraclavicular fossa, along the carotid arteries. Percussion: The boundaries of the OST during decompensation are shifted to the left. Auscultation: I tone is not changed or slightly weakened; There may be a bifurcation of the first tone, the second tone is weakened or not determined. Rough systolic murmur in the second m/r above the aorta and in Botkin's point, carried out in the jugular fossa, supraclavicular fossa, carotid arteries (better in the position on the right side as you exhale). Pulse: small amplitude, slow, rare. Blood pressure: systolic reduced to 90-100 mm Hg. Art., diastolic slightly increased.
Pathognomonic signs of AS: pronounced pallor of the skin, raised apical impulse in V m / r pulse rare, slow, hard, decreased systolic and pulse pressure, increased diastolic pressure
Nursing process for congenital heart defects Author: Ph.D. Vasilyeva L.E. - presentation
Nursing process for congenital heart defects Author: Ph.D.
Vasilyeva L.E. The student must know: Causes, clinical manifestations, features of s/p for congenital heart defects and rheumatism Causes, clinical manifestations, features of s/p for congenital heart defects and rheumatism The student must be able to: Carry out s/p for diseases of the cardiovascular system in children Carry out s/p for diseases of the cardiovascular system in children
Anatomy of the heart
Diagram of normal blood circulation
The formation of the heart occurs between 2 and 8 weeks of pregnancy, and it is during this period that defects develop. They can be hereditary, or they can arise under the influence of negative factors
Age-related characteristics of pulse rate and blood pressure Pulse rate (beats/min) Newborn Newborn year year year years years years years years years years years years years years years old years old years old years old years old years old years old years old years old years old years old years old years old years old years old Systolic blood pressure = 90+2 x n Diastolic blood pressure = 60+n Where n is age at years
Risk groups for having a child with congenital heart disease Women with: a history of spontaneous abortions (miscarriages) and stillbirths; with a history of spontaneous abortions (miscarriages) and stillbirths; over 35 years old; over 35 years old; smoked and drank alcohol during pregnancy; smoked and drank alcohol during pregnancy; burdened by family heredity; burdened by family heredity living in environmentally unfavorable areas; living in environmentally unfavorable areas; have had infectious diseases during pregnancy (especially rubella); have had infectious diseases during pregnancy (especially rubella); who used certain medications during pregnancy (sulfonamide drugs, some antibiotics, aspirin). who used certain medications during pregnancy (sulfonamide drugs, some antibiotics, aspirin).
Types of heart defects “blue” type defects (blue skin) “blue” type (blue skin) Tetralogy of Fallot Tetralogy of Fallot Pulmonary artery stenosis Pulmonary artery stenosis “pale” type defects (pale skin) ASD VSD VSD Open Duct of Batallo Open Duct of Bathallo Coarctation aortaCoarctation of the aorta
Anatomy of the heart with atrial septal defect
Clinic of ASD Complaints: shortness of breath, especially during physical activity, shortness of breath, especially during physical activity, palpitations, tendency to fainting. tendency to faint. sometimes - a loud cough with hoarseness. sometimes - a loud cough with hoarseness. fragile constitution, with pale skin; fragile constitution, with pale skin; during physical activity, transient cyanosis of the skin and mucous membranes. during physical activity, transient blueness of the skin and mucous membranes. Recurrent bronchitis and pneumonia are possible. Recurrent bronchitis and pneumonia are possible. the average life expectancy of these patients without treatment is on average 36 years the average life expectancy of these patients without treatment is on average 36 years incidence rate - 10% incidence rate - 10% Girls are 4 times more likely than boys
Anatomy of the heart with ventricular septal defect
VSD Clinic Complaints: shortness of breath during exercise shortness of breath during exercise palpitations palpitations tendency to fainting tendency to fainting fragile constitution, with pale skin fragile constitution, with pale skin during physical exertion transient cyanosis of the skin and mucous membranes during physical exertion transient cyanosis of the skin and mucous membranes Recurrent bronchitis and pneumonia are common. Recurrent bronchitis and pneumonia are common. The average life expectancy of these patients without treatment is on average 40 years The average life expectancy of these patients without treatment is on average 40 years
Open Batalov duct
Clinic of the patent duct of Batallova Complaints: general inhibition of growth and development with significantly reduced physical ability. general inhibition of growth and development with significantly reduced physical performance. children are thin, their weight is below normal children are thin, their weight is below normal heartbeat heartbeat pulsation of blood vessels in the neck and head pulsation of blood vessels in the neck and head feeling of heaviness in the chest feeling of heaviness in the chest cough, shortness of breath during physical exertion, a quick feeling of fatigue cough , shortness of breath during physical activity, a quick feeling of fatigue dizziness dizziness Fainting Fainting Frequency of occurrence 10% Frequency of occurrence 10% More common in girls
Coarctation of the aorta is the first complaint between years of life. first complaints between years of life. ringing in the ears, ringing in the ears, flushes of blood, flushes of blood, burning and heat of the face and hands, burning and heat of the face and hands, pulsation of the vessels of the neck and head, a feeling of heaviness in it, pulsation of the vessels of the neck and head, a feeling of heaviness in it, headache, dizziness, headache, dizziness, palpitations, palpitations, shortness of breath. shortness of breath. a feeling of numbness, coldness, weakness in the legs, a feeling of numbness, coldness, weakness in the legs, cramps during physical activity, cramps during physical activity, they have well-developed muscles of the shoulder girdle and weak leg muscles. they have well-developed muscles of the shoulder girdle and weak leg muscles. An important sign is that the pulse is different in strength in the upper and lower extremities, blood pressure in the arms is increased, and in the legs it is decreased. An important sign is that the pulse is different in strength in the upper and lower extremities, blood pressure in the arms is increased, and in the legs it is decreased. The average life expectancy without treatment does not exceed 35 years. The average life expectancy without treatment does not exceed 35 years. frequency 6-7% more common in boys
Coarctation of the aorta
Anatomy of the heart in pulmonary stenosis
Tetralogy of Fallot stenosis (narrowing) of the pulmonary artery up to complete closure of the lumen, stenosis (narrowing) of the pulmonary artery up to complete closure of the lumen, dextroposition of the aorta (the aorta sits astride the right and left ventricles, that is, it communicates with both of them) dextroposition of the aorta ( the aorta seems to sit astride the right and left ventricles, that is, it communicates with both of them) ventricular septal defect ventricular septal defect hypertrophy (enlargement) of the right ventricle hypertrophy (enlargement) of the right ventricle
Tetralogy of Fallot Clinic Shortness of breath Shortness of breath Forced squatting position, they get used to sitting with their legs crossed under them and sleeping with their knees pulled up to their stomach. A forced squatting position, they get used to sitting with their legs crossed under them and sleeping with their knees pulled up to their stomach. They are weak, chilly, and often experience fainting and convulsions. They are weak, chilly, and often experience fainting and convulsions. Well-being is adversely affected by changes in atmospheric conditions, excessive heat, cold - increased shortness of breath, general weakness, and cyanosis. Well-being is adversely affected by changes in atmospheric conditions, excessive heat, cold - increased shortness of breath, general weakness, and cyanosis. The physical development and growth of the child is delayed, the physical development and growth of the child is delayed, mental and sexual development is delayed. Mental and sexual retardation. Inappropriately long and thin limbs, especially the lower ones. Inappropriately long and thin limbs, especially the lower ones. Important signs are bluish fingers, thickened in the form of drumsticks. Important signs are bluish fingers, thickened in the form of drumsticks. Average life expectancy is 12 years. Average life expectancy is 12 years.
Extract from the medical history. Boy, 5 years old. According to the mother, the pregnancy proceeded without complications. Denies taking medications, alcohol, or the presence of damaging factors during pregnancy. At birth he was blue. Tetralogy of Fallot was diagnosed. Clinically: decreased physical activity, cyanosis of the skin and mucus. membranes, “drumsticks and watch glasses”, expansion of the borders of the heart in both directions by percussion, in the second and third intercostal spaces on the left there is a rough systolic murmur, dyspnea, orthopnea, frequent infectious diseases of the lungs, malnutrition. X-ray shows a slight enlargement of the heart in the shape of a “wooden shoe”, depletion of the pulmonary pattern, retraction of the pulmonary trunk arch.
5 year old child with tetralogy of Fallot
Tetralogy of Fallot
Tetralogy of Fallot
Diagnostics Clinic Clinic ECG ECG echography echography
Treatment Regimen Maximum stay in the fresh air Maximum stay in the fresh air Hardening Hardening Protect from infection Protect from infection Nutrition Feed more often, but little by little Feed more often, but little by little Limit salty foods Limit salty foods Drink according to diuresis Drink according to diuresis Foods rich in potassium Foods rich in potassium
Treatment Cardiac glycosides digitalis, digoxin, digitoxin digitalis, digoxin, digitoxin 1 hour before meals 2 times a day with an interval of 12 hours Overdose symptoms: Bradycardia, depression, visual impairment (decreased vision, seeing objects in green, trembling of objects), loss loss of appetite, diarrhea Bradycardia, depression, visual impairment (decreased vision, seeing objects in green, shaking objects), loss of appetite, diarrhea
Treatment Potassium preparations Asparkam, panangin Diuretics Hypothiazide, furosimide Means stimulating energy production ATP, KKB, vit.gr.B, C
Treatment Surgical treatment from 3 to 12 years of age
S/p with congenital heart disease Child problems Malnutrition Malnutrition Ineffectiveness of breathing Ineffectiveness of breathing Fluid deficiency Fluid deficiency Physical inactivity Physical inactivity Change in appearance Change in appearance Increased risk of developing infections Increased risk of developing infections Risk of social isolation Risk of social isolation Problems of parents Knowledge deficiency Knowledge deficiency Lack of faith in the prosperous outcome Disbelief in a successful outcome Chr. Fatigue Chr. Fatigue Overprotection Overprotection Loss of professional activity Loss of professional activity Decrease in material level Decrease in material level
S/p with congenital heart disease Nursing intervention Inform about the disease Inform about the disease Provide the child’s vital needs (temperature regime, elevated position in bed) Provide the child’s vital needs (temperature regime, elevated position in bed) Monitoring: heart rate, blood pressure, respiratory rate, skin color, thermometry Monitoring: heart rate, blood pressure, respiratory rate, skin color, thermometry
Control 1st option 1. Reasons for time. heart defects 2. List the defects of the blue type Option 2 List the defects of the pale type List the defects of the pale type Clinic of tetralogy of Fallot Clinic of tetralogy of Fallot
Homework assignment V.D. Tulchinskaya “S/d in pediatrics” C
References 1. N.G. Sevostyanova “S/d in pediatrics” 2. N.V. Ezhov “Pediatrics” 3. V. Tulchinskaya S/d in pediatrics” 4. Directory “Childhood diseases” edited by V.N. Samarina 2004.