Thanks to the advances of medicine, acquired heart defects are almost never seen today, compared to the first half of the 20th century. They affect the valve apparatus and lead to severe hemodynamic disturbances. They are extremely diverse in structure: they are caused by various factors, and the nature of the lesion itself can also be different.
As a rule, diagnosis is quite simple due to the characteristic clinical picture and the availability of modern equipment. Treatment is selected taking into account all the information about the defect. The main danger of this disease is complications, which subsequently cause disability or death. According to the ICD-10 code, all acquired heart defects are included in sections I34–I37, I05–I08, Q22–Q23.
Causes of development of acquired heart defects
The main cause of acquired heart defects is aortic atherosclerosis and myocardial infarction. Previously, the main cause was rheumatic valve disease. Today, in the era of antibiotics, rheumatism has faded into the background, if not into the background. At the same time, acquired vices are the lot of the adult population. Congenital heart anomalies are more common in children and adolescents. Other causes include endocarditis, systemic connective tissue diseases (SCTD), trauma, and syphilis.
Causes
A factor in the development of the decompensated form of heart failure is the lack of treatment for the disease in the presence of the diagnosis of the same name in the early stages.
If we consider the issue broadly, we are talking about a group of pathological processes. Long-term hypertension is one of the possible and common options.
Atherosclerosis of the coronary arteries is also common, as is left ventricular hypertrophy. Heart defects, congenital and acquired, play an equally important role.
Possible influence of previous injuries, myocardial infarction, inflammation of a muscular organ of an infectious nature (myocarditis).
Much less common are autoimmune or genetic diseases that lead to heart failure.
As a rule, violations of this kind are quickly discovered, but nothing can be done to help. The peak of diagnosis occurs at 10-12 years of age and even slightly less.
Addressing the root cause, especially in a timely manner, is the key not only to treatment, but also to effective prevention of heart failure.
Classification of acquired defects
According to modern clinical guidelines, the classification of all acquired heart defects includes several sections: according to etiology, anatomical location, severity and the presence of circulatory failure.
According to severity, all defects are divided into:
- minor;
- moderate;
- expressed.
Classification according to circulatory failure:
- heart failure (grades I–III, functional classes I–IV);
- cardiac asthma;
- presence of arrhythmias;
- the presence of thrombosis and thromboembolism.
Classification by anatomical location and etiology should be considered only in relation to symptoms.
Symptoms depending on valve damage
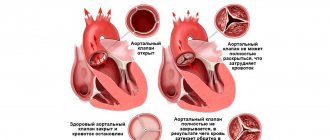
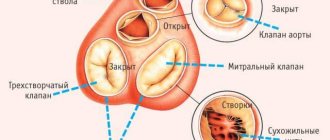
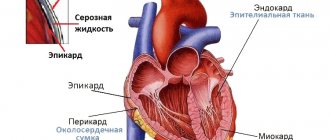
The clinical picture is largely determined by which valve and how exactly it is affected. There is stenosis (narrowing of the valve lumen), insufficiency (presence of reverse blood flow) and their combination. In some cases, they talk about regurgitation (reverse flow of blood when the valve leaflets are in normal condition).
Defeat of MK
The mitral valve can be involved in the process with rheumatism, autoimmune diseases, endocarditis, myocardial infarction (severation of the chord or papillary muscle), and become calcified.
Stenosis
Due to compaction and fusion of the valves, normal blood flow is disrupted. The pressure in the pulmonary circulation increases and the risk of thromboembolic complications increases.
Main symptoms:
- shortness of breath on exertion and at rest with difficulty breathing;
- cough, hemoptysis;
- fatigue;
- headaches and periodic loss of consciousness;
- pain in the heart area;
- stagnation of fluid in the lungs.
Fatal complications are pneumonia, myocardial infarction (MI), kidney, stroke, supraventricular disorders width=”560″ height=”350″[/img]
On auscultation, a flapping sound is detected, and the characteristic sound of a valve opening can be heard. There is a murmur in the fifth intercostal space on the left during diastole.
Regurgitation (insufficiency)
Mitral regurgitation occurs as blood flowing back through the valve. May occur due to autoimmune diseases or endocarditis. Nowadays, acute mitral regurgitation is more common in connection with acute MI (the function of the papillary muscles is impaired, the chordae are torn off).
In acute mitral regurgitation, the prevailing picture is MI in combination with acute left ventricular failure. Characterized by pain in the heart area, pulmonary edema, and rhythm disturbances. In the chronic form of the defect, the left ventricular type of CHF first develops, and then the right ventricular type joins. Pulmonary hypertension and pulmonary stagnation may occur.
Auscultation reveals a systolic murmur, predominantly at the apex of the heart.
Combined defect
Combined mitral disease - at the same time the MV suffers from stenosis and insufficiency. In autoimmune diseases, this form is usually found. The clinical picture and symptoms depend on the predominance of stenosis or insufficiency.
Prolapse
In the presence of prolapse, the valve leaflets bend during ventricular systole into the atrium cavity. Minor prolapse is considered normal. This defect becomes clinically significant when regurgitation occurs. As a rule, this occurs against the background of age-related degenerative changes.
The patient complains of anxiety, chest discomfort, palpitations, and fatigue. The addition of regurgitation gives a clinical picture characteristic of valve insufficiency. During auscultation, a systolic click and systolic murmur may be detected.
Aortic valve damage
The aortic valve is affected by calcification of its leaflets, CTD, diabetes mellitus, atherosclerosis, renal failure, endocarditis, rheumatism, syphilis, dissecting aortic aneurysm.
Stenosis
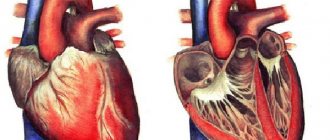
With aortic stenosis, the flow of blood into the aorta is impaired. Due to the fact that the myocardium of the left ventricle (LV) is quite powerful, this defect does not manifest itself for a long time. Over time, myocardial hypertrophy occurs. After the appearance of clinical signs, decompensation and death quickly occur.
One of the first symptoms is a rough murmur that can be detected during systole at the base of the heart. Aortic stenosis manifests itself as:
- angina attacks;
- fainting states;
- arrhythmias;
- left ventricular heart failure.
Regurgitation
When this valve fails, blood flows back into the LV from the aorta as the heart muscle relaxes. The myocardium in it is overloaded due to the large volume of blood, which is why it gradually dilates. The clinical picture is dominated by symptoms of chronic heart failure (CHF) of the left ventricular type. Possible development of angina pectoris and fainting.
On auscultation, a murmur can be heard during diastole. Mainly at the left edge of the sternum. In severe cases, capillary pulse and pulsation of the carotid arteries are determined.
Like mitral defects, aortic defects can be combined with each other.
Tricuspid valve stenosis and insufficiency
The tricuspid valve is most often affected by increased pressure in the arteries of the lungs. Its insufficiency develops and blood is thrown back into the right atrium. Quite often it is involved in the process of infective endocarditis, especially in injection drug addicts. Rheumatic lesions of the tricuspid valve are observed relatively rarely today and are mainly combined with other acquired defects.
With isolated damage to this valve, blood stagnation develops in the systemic circulation. Hepatomegaly and edema of the lower extremities are observed. Often these symptoms fade into the background and are covered by the clinical picture of damage to the mitral and aortic valves.
A murmur is detected during systole. It is heard at the xiphoid process.
Pulmonary valve disease
In the vast majority of cases, pulmonary valve anomalies are congenital. Acquired defects are associated with infective endocarditis, increased pressure in the vessels of the lungs, CTD, and rheumatism. They are quite rare. The main clinical manifestations are symptoms of right ventricular type CHF.
On auscultation, a murmur is heard in the second intercostal space on the left.
Combined defects
In the vast majority of cases, the aortic and mitral valves are simultaneously affected. Slightly less common - mitral and tricuspid/pulmonary arteries. There is a phenomenon of mitralization of aortic disease, when, against the background of aortic valve dysfunction, mitral valve insufficiency develops at some stage.
Symptoms depending on the cause of the defect
In addition to the fact that acquired heart defects differ significantly in their symptoms depending on the anatomical characteristics, their clinical picture largely depends on etiological factors.
Acute defects
Acute mitral regurgitation develops against the background of myocardial infarction. In addition to the clinical picture of the heart attack itself, there are two important additional criteria:
- acute formation of the defect;
- development of cardiogenic pulmonary edema and acute respiratory failure.
Another acute condition is aortic insufficiency due to dissecting aortic aneurysm. Accompanied by chest pain and heart failure.
Traumatic lesion
Injuries in the heart area are observed among motorists (the impact of the steering wheel falls directly on the chest), less often in other circumstances. Here, symptoms of myocardial damage (bruise, cardiac tamponade) may come to the fore. Damage to the valve apparatus manifests itself after 2-3 weeks, when scarring processes occur in the tissue of the injured valves.
Symptoms of rheumatism
Rheumatism is an autoimmune disease that primarily affects the heart. It begins after a sore throat or tonsillitis with a rheumatic attack, which manifests itself in the form of volatile arthritis and myocarditis. Subsequently, chorea may occur. The valve leaflets gradually “stick together” due to a chronic inflammatory process, and subsequently can become sclerotic.
Defects due to endocarditis
Endocarditis develops due to previous sepsis, cardiac surgery, prolonged or frequent intravenous administration of drugs, and in injection drug addicts. Vegetations form on the valve leaflets, which causes both stenosis and insufficiency. Infectious endocarditis manifests itself in the form of severe asthenia, including cachexia, anemia, and multiple organ failure.
Atherosclerotic damage to valves and their age-related changes
Due to atherosclerosis, the aortic valve is affected. Its valves become calcified and stenosis develops. In the future, mitralization of the defect is possible. Combined with other manifestations of atherosclerotic disease.
Age-related degenerative changes and calcification often affect the aortic and mitral valves. Their elasticity and mobility are impaired. Mostly elderly people suffer.
Autoimmune diseases
Systemic lupus erythematosus, scleroderma, rheumatoid arthritis and other CTDs can affect the valvular apparatus of the heart. Cardiologically, the defects are unremarkable. First of all, the leading symptoms of each disease always appear in the form of damage to joints, internal organs, skin, etc.
Syphilis
Damage to the heart and aorta develops with tertiary syphilis. Despite the fact that today cases of syphilis have increased significantly, tertiary forms practically do not occur. Combined with the formation of gummas, damage to internal organs, bones and joints.
Acquired heart disease in adults. Treatment
Acquired heart disease
is a physical damage or functional disorder of one or more heart valves. As a rule, these disorders develop as a result of infectious diseases, autoimmune disorders, overload and expansion of the heart chambers and manifest themselves in the form of valve stenosis or insufficiency.
Unlike congenital heart disease, acquired heart disease develops after birth under the influence of various diseases.
Diagnosis of acquired heart defects
In the vast majority of cases, the diagnosis is assumed based on auscultation data. Severe cases with a “blooming” picture of the defect are practically never encountered today due to the developed system of early diagnosis and medical examination. Less commonly, defects are first detected by chest x-ray.
Indicators of clinical analysis of blood and urine, biochemical blood tests directly depend on the etiological factor and are extremely variable. When recording an ECG, nonspecific changes may be observed:
- hypertrophy of the heart;
- signs of systolic overload and impaired myocardial repolarization;
- changes of ischemic nature;
- rhythm disturbances (mainly atrial fibrillation).
The basis of diagnosis is echocardiography. Using the ultrasound method, the condition of the myocardium and valve apparatus is determined. Changes in the structure of the valve leaflets and their abnormal movement are a characteristic sign of the defect. Echocardiography allows you to determine only the location and nature of the lesion; the etiology is revealed using laboratory research methods. Doppler mapping of the heart is used to assess the direction of blood flow.
As an additional diagnostic method, MRI with contrast enhancement of the ventricular cavities can be prescribed. Coronary angiography is performed to assess the condition of the coronary arteries.
Stress tests are necessary to assess the stage of the defect, the severity of heart and coronary insufficiency. Holter ECG monitoring is performed to detect rhythm disturbances and myocardial ischemia.
Diagnostics
In order to determine the origin of the disease, specialists conduct an examination in several stages. During the examination, doctors take into account the patient’s medical history and study his condition under conditions of physical activity and complete rest. A careful examination reveals cyanosis, swelling, position and structure of the peripheral veins. To determine the type of defect, doctors listen to the heart murmur and tone. Modern diagnostic methods include:
- Electrocardiography – heart rhythm, type of arrhythmia, signs of coronary artery disease are traced. If aortic insufficiency is suspected, additional weight-bearing manipulations may be performed.
- An X-ray is an instrumental method that determines the degree of pulmonary congestion and clarifies the type of defect. Performed in different projections using contrast.
- Phonocardiography – registers tones and noises, clarifies disturbances in the functioning of the organ.
- Echocardiography - with its help, doctors determine the type of defect, the condition of the orifice, valves, and ejection fraction of the heart.
To obtain more accurate information, magnetic resonance imaging is prescribed. In laboratory conditions, a rheumatoid test is performed to determine the level of cholesterol and sugar in the patient’s body. He is also sent for general urine and blood tests.
Treatment
Treatment of all acquired heart defects in adults is possible today exclusively by surgery. Medication is used either to improve quality of life or as part of palliative care in inoperable patients.
Physiotherapy, alternative medicine, and folk remedies in this case are weakly effective and have only a temporary, symptomatic effect.
Medication correction
All drug therapy consists of eliminating the symptoms of an existing defect, slowing its progression and preventing complications. In addition, it may differ slightly depending on the etiology of the disease:
- For rheumatism, antibiotics and anti-inflammatory drugs are used.
- For CTD – immunosuppressants and anti-inflammatory drugs.
- Endocarditis must be treated with antibiotics, anticoagulants, iron supplements, etc.
- Acute mitral regurgitation and dissecting aortic aneurysm require life support and emergency surgery. In case of mitral regurgitation against the background of a heart attack, medication is used to treat the latter.
For any acquired defects, depending on the symptoms, the following are used in therapy:
- Diuretics. Indicated for any manifestations of heart failure. Helps reduce fluid stagnation in the pulmonary and systemic circulation. Loop diuretics (“Furosemide”, “Torasemide”) are used in courses; “Indapamide”, “Spironolactone”, “Hydrochlorothiazide” with individual dosage selection are suitable for continuous use.
- Cardiac glycosides (Digoxin). Used for certain arrhythmias or in cases of decompensated heart failure. Used in courses. In inoperable patients they can be used continuously to improve the quality of life.
- Beta blockers (Bisoprolol, Metoprolol, etc.). They have an antiarrhythmic effect, slow the progression of CHF, reduce myocardial oxygen demand and prevent angina attacks, lower blood pressure.
- ACE inhibitors (Lisinopril, Perindopril, etc.) or angiotensin II receptor antagonists (Valsartan, Candesartan, etc.). Rarely used for defects. They have nephroprotective, hypotensive effects and slow down the progression of CHF.
- Nitrates (Nitroglycerin, isosorbide dinitrate, Nitrospray, etc.). Used on demand to relieve angina attacks.
- Antiplatelet agents (acetylsalicylic acid). Necessary to improve the rheological properties of blood and prevent thromboembolic complications.
- Anticoagulants. It is possible to use Warfarin, but in the case of defects, new oral anticoagulants (Dabigatran, Rivaroxaban, Apixaban) have shown better results. Indicated for atrial fibrillation, the presence of blood clots in the cavities of the heart, or thromboembolic complications in the past. Reduce the risk of thromboembolism.
- Antiarrhythmic drugs. Verapamil, Diltiazem, beta blockers, and Amiodarone are used. Prevents the development of arrhythmias and reduces the risk of complications associated with them.
Surgical interventions
Any surgical interventions to eliminate an acquired defect can be done before irreversible changes occur in the heart and other organs.
In acute mitral regurgitation, the integrity of the chordae tendineae or papillary muscles is restored. Aortic insufficiency due to dissecting aneurysm requires elimination of the latter.
Sometimes it is possible to perform commissurotomy or balloon valvuloplasty for stenosis, however, relapse is possible after them. In all other cases, valve replacement is indicated. Most often it is performed through a thoracotomy approach. One promising technique is percutaneous replacement, developed for the aortic valve.
Acquired heart disease: symptoms
Acquired heart defects are different. We will tell you more about this below. Here we list the main symptoms, since for all types of acquired heart defects the symptoms are almost the same:
- Fast fatiguability
- Discomfort or pain in the heart area
- Dizziness, less often – fainting
- Feeling short of breath (especially during exercise or lying down)
- Cardiopalmus
- Changes in skin color (pallor, bluishness)
- Heaviness in the right hypochondrium
- Swelling of the legs at the end of the day
- Dry cough, which indicates that heart failure is progressing
Acquired heart defects in adults differ in that they can produce specific symptoms. For example, hoarseness for no apparent reason (no diseases of the ENT organs), shaking of the head in rhythm with the pulse in aortic insufficiency and a number of others.
It is important to know:
acquired heart defects are dangerous. If one or another heart defect is not detected in time, sooner or later it will lead to serious consequences that can cost you your life.
If you have any of the symptoms we've outlined above, don't try to cure yourself or live with the expectation that "it will go away." It’s better to make an appointment with our cardiologist, who will thoroughly understand your situation, determine exactly whether you have a heart threshold, and tell you in detail what to do next.
Make an appointment now.
Make an appointment
Features during pregnancy
Acquired defects without signs of CHF and other symptoms pose a low risk for pregnancy. The stronger its manifestations, the greater the risks for mother and child associated with prolongation of pregnancy. In case of severe CHF, its interruption is indicated. Before conceiving a child, a woman with an acquired defect must undergo a course of treatment.
Prognosis without treatment and after it
Observation without any active measures is carried out only for asymptomatic patients. After the first symptoms appear without surgical intervention, death occurs within 2-5 years.
If the defect was eliminated promptly, the patient can continue to live a full life. Life expectancy, in the absence of complications, for such people is approximately equal to the average in the region. In some cases, heart surgery is complicated by infective endocarditis.
Did you like the article? Save it!
Still have questions? Ask them in the comments! Cardiologist Mariam Harutyunyan will answer them.
Ivan Nekrasa
Graduated from Rostov State Medical University with a degree in General Medicine.