1 / 5 ( 1 voice )
Heart failure is a condition in which the heart muscle cannot contract fully. As a result, the organs suffer from a lack of blood.
The outcome of this condition is decompensated heart failure. Various instrumental methods are used for diagnosis, treatment is carried out conservatively and surgically.
Decompensated heart failure - end-stage disease
Treatment
Before prescribing a treatment method and specific medications, the doctor conducts a full examination. This includes studying the medical history, since if the last stage of the disease has developed, then the person already has a medical history. A physical examination is also performed.
The patient must undergo blood and urine tests. Instrumental studies include x-ray and echocardiography. Modern diagnostic methods include MRI and CT. They are very informative and can be prescribed instead of x-rays and ultrasound. After the necessary studies, medications are prescribed.
Treatment should be aimed at eliminating decompensation of the body and restoring its basic functions, neutralizing stagnant processes. Therapy must be carried out under the supervision of doctors, that is, only in a hospital setting. The patient needs bed rest; any stress (physical and emotional) must be excluded. The patient should periodically sit down or take a few steps. This will help prevent stagnation and the formation of blood clots.
Drug therapy
Decompensated heart failure is treated with a complex of various drugs
It is important to take: . ACE inhibitors. Beta inhibitors
These drugs help reduce myocardial demand. Cardiac glycosides. These drugs help increase cardiac output. Aldosterone antagonists. These drugs increase blood pressure and remove excess fluid from the body. Antiarrhythmic drugs.
- ACE inhibitors.
- Beta inhibitors. These drugs help reduce myocardial demand.
- Cardiac glycosides. These drugs help increase cardiac output.
- Aldosterone antagonists. These drugs increase blood pressure and remove excess fluid from the body.
- Antiarrhythmic drugs.
It is important to take antihypertensive drugs, drugs that affect the rheological quality of blood and lipid metabolism. Additionally, diuretics are required.
For advanced heart failure, other medications are also prescribed. Since the whole body suffers from cardiac dysfunction, it is necessary to take hepatoprotectors, immunomodulators and vitamin complexes.
It is important that a complex of drugs is prescribed by a qualified specialist, because all heart medications have a fairly large list of side effects. Only a doctor can prescribe therapy based on all the individual characteristics of the patient’s body in order to reduce the likelihood of such actions affecting the body.
Surgical operations
Most often, surgical treatment is prescribed for cardiac decompensation. These methods include:
- vascular bypass;
- coronary angioplasty;
- installation of a defibrillator or pacemaker.
Radical surgical treatment is prescribed to patients who have irreversible changes in the structure of organs. This may require a lung, heart or large artery transplant.
In case of heart failure of the left ventricle, patients are implanted with a special device that functions for it. Some time ago, doctors installed this device temporarily, but now it has been proven that it significantly prolongs the life of patients.
Heart failure in the stage of decompensation is a serious condition in which in most cases death occurs. Therefore, self-medication in this case is simply contraindicated. According to statistics, about 75% of men and 62% of women do not live more than 5 years with this pathology. But such figures are due to the fact that people do not consult doctors in a timely manner.
Diagnostics
If you consult a doctor at the first symptoms, the problem can be resolved in a fairly short period of time. Sometimes diagnostic techniques can become complicated. For example, when you have two different illnesses with similar symptoms.
It is important to understand that during heart disease it is impossible to immediately make an accurate diagnosis. This will take more time. It is important to monitor the patient's condition during the day and at night.
Today, the diagnosis of edema, which is provoked by the cardiac disease in question, is simple. But, for some reason, many patients apply only when severe swelling is already present. Due to delay, treatment becomes noticeably more complicated.
The primary examination is mainly carried out by a general practitioner. But more serious actions that require special skills and certain special equipment are carried out by cardiologists and other specialists.
Research methods during the diagnosis of cardiac edema:
- blood analysis;
- monitoring the state of pressure at different times of the day (CVD);
- obtaining anthropometric data;
- conducting the Kaufman experiment;
- Analysis of urine;
- ultrasound examinations;
- use of electrocardiography (ECG) techniques;
- echocardiographic studies (EchoCG);
- radiography;
- physical examination of the patient (visual examination, percussion, history taking, auscultation and other methods).
A characteristic symptom of decompensated insufficiency is general weakness, as well as severe swelling of the limbs. Often, with the disease, patients gain weight sharply.
The set of diagnostic measures includes a study of the level of change in beta-type uretic peptide, H-neutral peptide, as well as echocardiography and x-rays of internal organs, transcoronal echocardiography.
Experts can obtain more accurate information about the strength of blood pressure in the heart chambers by performing a special procedure, during which a catheter is inserted into the central vein or pulmonary artery and the necessary measurements are taken.
Also, the diagnosis of any form of HF consists of conducting a number of laboratory tests, including a blood test for creatinine and urea levels, for the content of electrolytes, transaminases and glucose, and other blood and urine tests are also performed; study of the presence and ratio of gases in the blood of the arteries.
If you consult a doctor at the first symptoms, the problem can be resolved in a fairly short period of time. Sometimes diagnostic techniques can become complicated. For example, when you have two different illnesses with similar symptoms.
It is important to understand that during heart disease it is impossible to immediately make an accurate diagnosis. This will take more time. It is important to monitor the patient's condition during the day and at night.
Today, the diagnosis of edema, which is provoked by the cardiac disease in question, is simple. But, for some reason, many patients apply only when severe swelling is already present. Due to delay, treatment becomes noticeably more complicated.
The primary examination is mainly carried out by a general practitioner. But more serious actions that require special skills and certain special equipment are carried out by cardiologists and other specialists.
A characteristic symptom of decompensated insufficiency is general weakness, as well as severe swelling of the limbs. Often, with the disease, patients gain weight sharply.
The patient examination program includes the following mandatory activities:
- Collecting a complete medical history is the first measure, which means a thorough analysis of the patient’s medical history, assessing the severity of symptoms at each stage of the process. The specifics of the diagnosis show that the patient was already registered with a cardiologist, but either the therapy was ineffective, or the process was aggravated by some external factor. As a result, heart failure progressed to its extreme form. The specialist will be required to pay maximum attention to the treatment process and look for errors in past prescriptions.
- A general blood test shows the content of glucose, creatinine, urea, electrolytes, and transminase. It can also be used to assess the condition of the thyroid gland and the level of blood gas pressure in the arteries.
- ECG and EchoCG determine the thickness of the myocardium, the structure of the heart, and find anomalies and disorders.
- Chest X-ray visualizes the organ, helps determine the exact size; using an X-ray, the diagnostician assesses the condition of the lungs, determines the presence of pathology and the stage of the problem.
- Insertion of a catheter into the pulmonary artery or central vein. This method helps measure the pressure level as the chambers fill, resulting in cardiac output.
Diagnosis of the disease involves conducting instrumental studies. For this purpose the following methods can be used:
- electrocardiography;
- chest x-ray;
- determination of B-type natriuretic peptide or N-neutral.
Causes
The causes of chronic heart failure in the decompensation stage are various diseases of the cardiovascular system that were not treated in time.
Decompensated heart failure occurs for the following reasons:
- Hypertension, or rather, a hypertensive crisis can trigger an irreversible process.
- Congenital heart defects. These are abnormalities of the heart valves, as a result of which cardiac function fails.
- Myocarditis.
- Stable tachyarrhythmia.
- Hypertrophic type cardiomyopathy.
The above reasons relate to cardiac pathologies. Other factors can also cause heart failure:
- Chronic alcoholism.
- Poisoning of the body of a bacterial-toxic type.
- Bronchial asthma, which was not treated and became advanced.
- Incorrect treatment or its absence at the first stage of the pathology.
- Obesity.
- Diabetes.
Chronic form of DSN
Chronic decompensation is divided into two types:
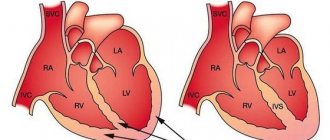
- Left ventricular is provoked by a decrease in myocardial contraction or as a result of overload of the left ventricle. The situation can be provoked, for example, by a violation of the integrity of the heart muscle, in which the balance between the pulmonary and systemic circulation is lost: blood is retained in the pulmonary circulation, and an insufficient amount of blood enters the systemic circle.
- The right ventricular type has the opposite picture: in the large circle there is stagnation, in the small circle there is a lack of blood. The problem is provoked by painful changes in the lungs, as a result of which there is overstrain of the right ventricle.
There are several pathogenetic mechanisms that lead to the onset of the disease:
- myocardial failure due to its damage or excessive load;
- mechanical obstacles of the cardiovascular system;
- arrhythmias;
- A combination of several mechanisms is also possible.
In 1934, a classification of heart failure was developed and adopted. The following stages of the disease were determined:
- Stage 1. Considered compensated. With moderate physical activity, the patient experiences a number of symptoms: shortness of breath and tachycardia.
- 2A stage. The stage is considered decompensated - reversible. In addition to tachycardia and shortness of breath, the patient has swelling of the lungs, as well as an enlarged liver. Symptoms also include swelling of the legs and feet.
- 2 B, uncompensated, poorly reversible stage. Symptoms appear with minor physical and emotional stress. Characteristic changes in liver tissue, swelling of the legs above the shin. The signs are persistent and more obvious than in previous stages.
- Stage 3 - decompensated, irreversible. The most complex form of the disease. Treatment requires a lot of effort and time. Alleviation of the patient's condition is achieved through intensive therapy, which is aimed mainly at eliminating symptoms.
One of the signs of the disease is shortness of breath
Symptoms
Signs of decompensation include:
- inappropriate behavior;
- lack of criticality towards one's actions;
- a clear increase in mental changes;
- decreased intelligence;
- deterioration in performance;
- problems with social adaptation.
The consequence of such an episode of decompensation is, as a rule, an increase in psychological and psychiatric problems. And the longer the period of decompensation, the more severe the consequences can be.
Factors that may influence the specificity of the observed reactions:
- motor skills;
- mental activity;
- rigidity or mobility of nervous processes;
- a person's intra- or extroversion.
Signs of heart failure
Severe heart failure is accompanied by:
- gas exchange disorder;
- swelling;
- stagnant changes in internal organs.
Gas exchange disorder
Slowing down the speed of blood flow in the microvasculature doubles the absorption of oxygen by tissues. As a result, the difference between the oxygen saturation of arterial and venous blood increases, which contributes to the development of acidosis.
Under-oxidized metabolites accumulate in the blood, activating the basal metabolic rate. As a result, a vicious circle is formed, the body requires more oxygen, but the circulatory system cannot provide these needs.
A gas exchange disorder leads to the appearance of symptoms of heart failure such as shortness of breath and cyanosis.
Stages of the disease
Conventionally, the development of this disease can be divided into three stages:
- compensation,
- subcompensation and
- decompensation.
This division, based on the names themselves, is based on the magnitude of the functional capacity of the liver during a given disease - to what extent it performs its assigned function.
Compensated stage
In the compensated stage, the patient does not even suspect that he has this disease. The fact is that the impaired function of hepatocytes damaged by cirrhosis is taken over by healthy liver cells. They hypertrophy, i.e. increase in size. Accordingly, their functional ability increases. But in general, liver function is not yet affected. Subjectively, nothing bothers the patient; he feels quite well, completely unaware that he has this disease.
Subcompensation stage
With subcompensation, on the one hand, the presence of the first signs of the disease is already evident, and on the other hand, the liver is still coping with its work. At this stage, there is a line, crossing which, the disease goes into the stage of decompensation.
Stage of decompensation
In the last stage, the symptoms of the disease already become obvious, which can be determined both by an objective examination of the patient and confirmed by laboratory and biochemical tests. The liver is no longer able to perform its function. Nothing can help her with this, because the liver is an unpaired organ, and there is no need to talk about any compensatory mechanism in which the function of one suffering paired organ is taken over by another (as can be observed, for example, in the case of the kidneys).
This happens because all hepatocytes are practically destroyed and are replaced by connective tissue. Despite the fact that the liver is externally enlarged in size (in this situation, larger does not mean good), its function suffers and ultimately comes to zero. At this stage, using the drugs of modern medicine, it is only possible to prolong the days of the patient’s life, to alleviate his fate, but his complete cure, unfortunately, is problematic.
When diagnosing liver cirrhosis, it is necessary to pay due attention to the complaints that the patient makes. They may indicate a deterioration in appetite or a complete absence of it
Weight loss may be observed against the background of the patient’s usual lifestyle without the use of any diets or increased physical activity. The patient may experience causeless fatigue and increased fatigue. Sleep may be disturbed, and the emotionally ill person becomes unbalanced.
Skin itching and icteric coloration of the skin appear. The appearance of so-called spider veins on the skin is typical. Problems with the digestive tract appear in the form of various dyspeptic disorders, accompanied by nausea, vomiting, and bloating (flatulence) may occur. The patient may complain of heaviness in the right side. Low-grade fever develops.
Objectively, an enlargement of the liver and spleen is observed, and the spleen, like the liver, can reach impressive sizes. Varicose veins are widespread throughout the body. The skin has a icteric coloration.
There is a loss of muscle mass, which is caused not only by a decrease in muscle mass, but also in fat mass. Externally, the patient looks thinner. Nosebleeds and bleeding gums are common.
The presence of liver cirrhosis is confirmed by laboratory tests. A biochemical blood test clearly shows changes in the pattern of liver enzymes, an increase in some and a decrease in others. The level of bilirubin in the blood increases significantly, but the amount of albumin, on the contrary, decreases. Changes are also observed in the levels of specific liver enzymes.
Varieties and clinical picture
Decompensated heart failure is characterized by the presence of symptoms:
- Myocardial damage;
- Difficulty breathing with or without exercise, regardless of the time of day;
- General weakness of the body as a result of oxygen starvation of the body;
- Increase in body weight;
- Edema;
- As a result of fluid stagnation in the lungs, a wet cough appears;
- An increase in the size of the heart leads to a rapid heartbeat: in order to push out the required amount of blood, the organ begins to contract more often.
Chronic heart failure, the stages of which sometimes do not have clear symptoms, is often detected during the progression of the disease. The main part of the symptoms is provoked by stagnation of fluid in tissues and organs, as well as their insufficient blood supply. Some signs of fluid accumulation:
- shortness of breath during physical exertion—climbing stairs, lifting heavy objects;
- cough and wheezing in the lungs;
- sudden, causeless weight gain;
- swelling of the extremities in the ankle area.
Insufficient blood supply to organs and tissues provokes a number of symptoms:
- dizziness, fainting, “blackout” in the eyes;
- general weakness;
- cardiopalmus;
- frequent urination at night;
- loss of appetite.
To a number of physical ailments, some emotional disorders are often added: anxiety, depression.
In the acute form of the disease, symptoms occur quickly, sometimes with lightning speed. There are different signs of failure manifested in the right ventricle:
- swelling of the neck veins;
- blueness of fingers, limbs, tip of the nose and earlobes;
- swelling of the arms and legs;
- due to the sharp swelling of the liver, the skin acquires a yellowish tint.
A left ventricle with pathology can be identified by the following signs:
- breathing problems: shortness of breath, suffocation, intermittent breathing;
- sharp attacks of coughing, during which sputum is released, sometimes foam;
- when taking a sitting position, the patient feels better, he tries to use his legs;
- When listening to the lungs, moist rales are detected.
Examination in a clinical setting may reveal the following symptoms:
- increased blood pressure;
- oxygen starvation, wheezing in the lungs;
- signs of arrhythmia;
- decreased urine production;
- decreased temperature of the extremities.
X-ray of the sternum makes it possible to diagnose venous congestion, as well as interstitial edema.
In women, heart failure often manifests itself with a number of symptoms:
- burning pain in the chest;
- loss of appetite provokes a sharp decrease in body weight;
- hypertension;
- swelling of the limbs, as well as bluish skin of the fingers.
Other symptoms are typical for men:
- chest pain is of a pressing nature, often also affecting the left arm;
- the cough can be not only of a wet nature, but also the formation of hemoptysis;
- swelling of the upper and lower extremities;
- respiratory failure leads to redness of the skin in the chest area;
- the acute form of the disease can provoke loss of consciousness.
Unlike acute heart failure, which must be treated immediately, chronic heart failure often requires lifelong therapy with a series of medications.
In order to diagnose decompensated heart failure, an examination is carried out, based on the results of which a final diagnosis is made. To confirm the presence of the disease, instrumental research methods are used.
The study uses electrocardiography, as well as chest x-ray. A blood test is performed. Urine analysis is also carried out. Based on the levels of urea, glucose, and the amount of electrolytes, a preliminary diagnosis is made. Creatinine levels are checked.
A test called transthoracic echocardiography is used to study the contraction and relaxation of the heart muscle (systole and diastole). Based on catheterization, cardiac output is examined, as well as the pressure in the heart chambers and their filling with blood.
In order to begin effective treatment, a quick diagnosis is necessary, which is possible if certain symptoms are present. The procedure is complicated by the fact that the clinical manifestations of one disease are often superimposed by signs of another.
Attention! Due to the heterogeneous nature of end-stage heart failure, there is no clear specific sign that would 100% confirm the diagnosis.
Decompensated heart failure has the following symptoms:
- history of myocardial injury or heart failure;
- shortness of breath during the day and at night, during physical activity and at rest;
- general weakness;
- swelling, increase in body weight or abdominal volume.
A physical examination can reveal the following signs of the disease:
- increased pressure in the jugular vein;
- wheezing in the lungs, hypoxia;
- arrhythmia in any of its manifestations;
- decreased volume of urine production;
- cold lower limbs and hands.
Diagnosis is impossible without instrumental tests. For example, chest radiography is performed to determine venous stasis and interstitial edema.
Before considering the symptoms of decompensated heart failure, it should be noted that the clinical picture directly depends on the type of disease. There are two forms of DHF - chronic and acute. Let's look at each of them in more detail.
Acute form
Diagnosis requires the presence of certain symptoms. However, it must be taken into account that the signs of one disease overlap with the symptoms of other pathologies. Apart from this, there is no clear-cut sign that would allow a diagnosis to be made with confidence.
The initial stages of chronic heart failure can develop according to the left and right ventricular, left and right atrial types. With a long course of the disease, there are dysfunctions of all parts of the heart. In the clinical picture, the main symptoms of chronic heart failure can be identified:
- fast fatiguability;
- shortness of breath, cardiac asthma;
- peripheral edema;
- heartbeat.
Most patients complain of fatigue. The presence of this symptom is due to the following factors:
- low cardiac output;
- insufficient peripheral blood flow;
- state of tissue hypoxia;
- development of muscle weakness.
If we are dealing with hypodiastolic decompensation, then the decrease in cardiac output is explained by insufficient filling of the ventricles. Hypodiastolic decompensation has not only a primarily cardiac form: this also includes that form of peripheral circulatory failure, when the cause of a decrease in diastolic filling is not primarily in the heart, but in an imbalance of peripheral factors that regulate blood circulation.
Hyposistolic decompensation. In hyposystolic decompensation, the primary cause of circulatory imbalance is a decrease in myocardial systolic force.
First (compensated) stage. In this situation, shortness of breath occurs, fatigue increases and the heart rate increases. During physical exertion, a state of suffocation occurs. As for hemodynamics, it is not disturbed.
Second stage. Period II A (decompensated, reversible). If the patient is in a calm state, then the pathological symptoms are expressed moderately. With exertion, everything is complicated by tachycardia and shortness of breath. Often, acrocyanosis and congestive wheezing appear in the lower parts of the lungs. After rest, in the morning, the liver remains enlarged. As for the feet and ankles, the swelling on them decreases slightly, but not for long.
Second (irreversible decompensated failure) stage. Period II B. In a calm state, without the use of loads, an attack of shortness of breath may appear from time to time. When the patient is given a little load, things become more complicated:
- swelling spreads to the thighs and lower legs;
- severe wheezing is observed in the lungs;
- the size of the liver remains increased.
In some cases, effusion of the pleural cavity is observed (even after rest, the symptoms do not decrease).
Third stage (irreversible decompensated failure). Severe attacks of suffocation occur, especially during sleep. Severe shortness of breath is constantly present in the form of asthma. Edema develops, accompanied by dilation of the jugular veins. During the third stage, all symptoms may be complicated by the appearance of hydrothorax or hydropericardium.
According to the prognosis of cardiologists and other experienced specialists, chronic heart failure, which is in the stage of decompensation, has an unfavorable outcome in most cases. During the third irreversible stage, dangerous diseases such as ascites and anasarca develop.
Glucometer and test strips
This home device will help control two criteria for decompensation of diabetes mellitus at once - the level of glucose in the blood on an empty stomach and 1.5-2 hours after meals (the so-called postprandial glycemia).
The first indicator must be checked every morning, the second - 4-5 times a day, preferably after each meal. They help continuously monitor blood glucose levels and proactively regulate them through diet or medication. Of course, each diabetic himself decides how many times a day he can carry out such measurements. But you should remember that this should happen at least 2 times a day - on an empty stomach and after one of the meals.
Advice: when prescribing new antidiabetic drugs or if there are errors in the diet, it is better to test your blood sugar more often. With stable therapy and diet, you can slightly reduce the frequency of measurements. From time to time, these tests must be taken in the laboratory of a medical institution.
Analysis for sugar and acetone in urine at home
If the concentration of glucose in the blood is normal, its determination in urine can be carried out no more than 1-2 times a month. However, if high sugar levels are detected - more than 12 mmol/l, the level of glucose in the urine must be checked immediately. But keep in mind that with normal compensation there should be no sugar in the urine, and its presence indicates decompensation of diabetes mellitus.
In this case, you should consult with your treating endocrinologist to adjust the dose of glucose-lowering tablets or insulin. To analyze the amount of sugar in urine at home, special test strips are used.
The presence of glucose in the urine requires a test to determine acetone (ketone bodies) in the urine. This study can be done at home, without much difficulty, also using special test strips for determining acetone in urine. Depending on the amount of ketone bodies in the urine, the test strip changes color. This procedure will only take a few minutes, but its indicators allow you to begin timely treatment and avoid many complications.
Glycosylated hemoglobin
Ego is also called glycated. The indicator is considered the most accurate in diagnosing decompensated diabetes, because it shows the state of carbohydrate metabolism over 3 months.
In the body of a healthy person, glucose combines with all proteins without exception, and therefore with hemoglobin - this forms glycosylated hemoglobin. The higher the glucose level, the more hemoglobin it has added. An erythrocyte containing hemoglobin, including its glycosylated fraction, lives on average 120 days. Thus, by determining the amount of glycosylated hemoglobin, we find out the blood sugar level for 3 months.
Also at home it is necessary to measure blood pressure 2 times a day and weight once a week. These criteria for decompensation are important for prescribing comprehensive treatment and preventing health problems.
Causes of diabetes decompensation
Of course, each organism is individual and the reasons in each individual case may vary. However, the most common reasons are:
- violation of diet, overeating;
- refusal of treatment;
- incorrectly selected dose of diabetes medication or type of treatment;
- self-medication;
- the use of dietary supplements instead of medications;
- incorrectly calculated insulin dose;
- refusal to switch to insulin;
- stress, mental stress;
- some infectious diseases that lead to severe dehydration of the body;
adiabet.ru
Research methods and principles
What decompensated heart failure is is clear; it is when the cardiovascular system is unable to perform basic functions. Instrumental studies are widely used for diagnosis. These include electrocardiography, radiography of the internal organs of the chest, as well as measurement of B-type natriuretic peptide or N-neutral. Laboratory tests are carried out, namely blood/urine analysis. The level of urea, creatinine, electrolytes in the blood, transminase, and glucose is determined. These tests evaluate arterial blood gas pressure and thyroid function.
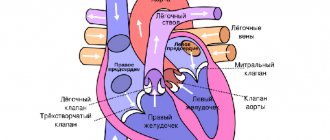
Types of Heart Failure
In some situations, transthoracic echocardiography is performed, it allows you to evaluate the systolic and diastolic functions of the left ventricle, valves, as well as blood filling pressure in the left atrium, right ventricle and inferior vena cava. Central venous or pulmonary artery catheterization provides valuable information on the filling pressure of the cardiac chambers, after which cardiac output can be easily calculated.
Goals and drugs used in treatment
Having an accurate idea of what this disease is, the goals become clear, the action of which is aimed at:
- eliminating manifestations of stagnation;
- optimization of volumetric performance indicators;
- detection and, if there are trigger factors for decompensation, their elimination;
- optimization of long-term therapy;
- minimizing side effects.
Diabetes compensation criteria
The main criteria for diabetes compensation:
- glycated (or glycosylated) hemoglobin;
- blood sugar on an empty stomach and 1.5-2 hours after meals;
- sugar level in urine.
There are also additional criteria:
- blood pressure indicators;
- cholesterol level;
- triglyceride levels;
- body mass index (BMI).
These indicators will help both the patient and the doctor to monitor the quality of treatment and quickly react if they change.
| Indicators | Compensation | Subcompensation | Decompensation |
| fasting blood sugar (mmol/l) | 4,4—6,1 | 6,2—7,8 | >7,8 |
| blood sugar after meals (mmol/l) | 5,5—8 | 8,1 – 10 | >10 |
| Sugar in urine (%) | <0,5 | >0,5 | |
| Glycosylated hemoglobin (%) norm 6% | <6,5 | 6,5—7,5 | >7,5 |
| Total cholesterol (mmol/l) | <5,2 | 5,2—6,5 | >6,5 |
| triglycerides (mmol/l) | <1,7 | 1,7—2,2 | >2,2 |
| Body mass index in men (kg/(m)2) | <25 | 25—27 | >27 |
| Body mass index in women (kg/(m)2) | <24 | 24—26 | >26 |
| Blood pressure (mm Hg) | <140/85 | <160/95 | >160/95 |
From the table we can conclude that the closer a diabetic’s test results are to normal, the better his diabetes is compensated and the less likely it is to develop unwanted complications.
Home laboratory
Unfortunately, it is impossible to assign a medical professional to every diabetic patient. The diabetic himself learns to control his disease and live with it.
The patient’s health largely depends on how he learns to control his illness. To do this, he can do simple tests at home. Being your own laboratory technician is very convenient and vital for every diabetic. After all, the level of glucose in the blood is very labile, and every indicator is valuable to monitor the correctness of treatment.
It is best to keep a special diary in which you write down the test results in your home laboratory, your well-being, menu, and blood pressure readings every day.
Research methods and principles
What decompensated heart failure is is clear; it is when the cardiovascular system is unable to perform basic functions. Instrumental studies are widely used for diagnosis. These include electrocardiography, radiography of the internal organs of the chest, as well as measurement of B-type natriuretic peptide or N-neutral. Laboratory tests are carried out, namely blood/urine analysis. The level of urea, creatinine, electrolytes in the blood, transminase, and glucose is determined. These tests evaluate arterial blood gas pressure and thyroid function.
Types of Heart Failure
In some situations, transthoracic echocardiography is performed, it allows you to evaluate the systolic and diastolic functions of the left ventricle, valves, as well as blood filling pressure in the left atrium, right ventricle and inferior vena cava. Central venous or pulmonary artery catheterization provides valuable information on the filling pressure of the cardiac chambers, after which cardiac output can be easily calculated.
Treatment
Treatment is symptomatic and aimed at stopping attacks and its most obvious manifestations. For example, for uncontrolled motor agitation, tranquilizers are prescribed, and for suicide attempts, antidepressants are prescribed. And almost all patients are given sedatives.
However, it is worth remembering that treatment must be prescribed by a psychiatrist. He can involve other specialists for the necessary consultations: psychologists, neurologists, cardiologists and many others.
Therefore, self-medication at home may not only not help, but also aggravate the situation. Moreover, the previously prescribed treatment regimen should also be reviewed in case of clear signs of such a violation.
Lapshun Galina Nikolaevna, Master of Psychology, psychologist I category
Decompensation of psychopathy
The signs of decompensation of psychopathy are particularly diverse due to the large variability of symptoms within this group of diseases. Each clinical case has basic symptoms, which are used to determine the clinical type of decompensation of psychopathy. There are three basic types:
- neurotic type,
- affective type,
- abnormal personality type.
The neurotic type of decompensation of psychopathy can occur in the following scenarios:
Asthenization - fatigue, feeling of weakness, inability to concentrate, headaches, autonomic disorders (sweating, palpitations, indigestion and salivation), decreased motor activity, sharpening of personality traits.
Hypochondriacal syndrome is a belief in the presence of a serious or fatal illness, fixation on the state of health and tracking of all its manifestations, the use of an imaginary or existing illness to manipulate others.
Obsessive-phobic syndrome - repeated fears and obsessive thoughts, painful, exhausting, leading to constant monitoring and double-checking of actions. Usually there is a noticeable connection with the situation that caused the decompensation.
Hysteroneurotic type – demonstrative, exaggerated manifestation of symptoms with not so significant severity, autonomic disorders, tendency to hysteria.
The affective type of decompensation of psychopathy includes several syndromes:
- Affective instability is a constant change in mood, variability in the manifestation of affective disorders, their frequent change.
- Explosive-dysphoric syndrome - reduced mood, gloominess, irritability, anger, gloominess, tendency to conflict, excitability.
- Subdepressive type - the general background of mood is low for a long time, there are no aspirations and desires, sleep is disturbed, expressed dissatisfaction with everything around, gloominess, anxiety.
Compensation
Almost any organ or organ system has compensation
, ensuring the adaptation of organs and systems to changing conditions (changes in the external environment, changes in the body’s lifestyle, exposure to pathogenic factors). If we consider the normal state of the body in a normal external environment as equilibrium, then the influence of external and internal factors puts the body or its individual organs out of balance, and compensation mechanisms restore balance by introducing certain changes in the functioning of the organs or changing them themselves. So, for example, with heart defects or with constant significant physical activity (in athletes), hypertrophy of the heart muscle occurs (in the first case it compensates for the defects, in the second it provides more powerful blood flow for frequent work at increased load).
Pathogenesis
There are tens of millions of patients worldwide who suffer from heart failure. This figure is growing every year. The most common cause is a narrowing of the lumen of the coronary arteries that supply the myocardium. Despite the fact that vascular pathology develops at a relatively young age, congestive heart failure is most often observed in older people.
10 out of 1000 patients over 70 years of age have signs of heart failure. Pathology is most often observed in women. This phenomenon is explained by the high mortality rate in the male half. In women, heart disease leads to heart failure, and in men, coronary disease occurs with complications and more often ends in death. The development of heart failure is provoked by:
- changes in the valvular apparatus of the heart;
- arterial hypertension;
- thyroid diseases;
- drug and alcohol addiction;
- myocarditis and other inflammatory diseases of the heart muscle.
Decompensation using the example of cirrhosis
Cirrhosis is the replacement of functioning liver tissue with scar tissue as a result of the hepatitis C virus, alcohol intoxication, and fatty degeneration. Decompensation means that the body's resource has been exhausted. In compensated cirrhosis, the function of the affected areas of the liver is performed by its healthy parts.
Fibrosis of the liver impairs blood flow, portal hypertension develops, which leads to many complications:
- ascites, or fluid accumulation in the abdomen;
- stretching of the veins of the stomach, intestines, varicose veins;
- itching due to decreased bile flow;
- muscle atrophy and bone loss due to decreased synthesis of substances;
- increased risk of bacterial infections, bleeding and decreased immunity.
An examination is carried out to determine the stage. A blood test shows an increase in ESR and leukocytes, and a decrease in iron levels. Protein and red blood cells, leukocytes and casts are detected in the urine. A biochemical blood test reflects global changes. Bilirubin, alkaline phosphatase, gamma-glutamyl transpeptidase, liver enzymes, and globulins increase. Cholesterol, protein, albumin and urea are reduced.
Cirrhosis in the decompensation stage is confirmed by histological examination and can only be treated with a liver transplant.