The essence of the pathology, the mechanism of its development
Chronic heart failure can develop over months. This process is divided into several main stages:
- Due to heart disease or organ overload, the integrity of the myocardium is compromised.
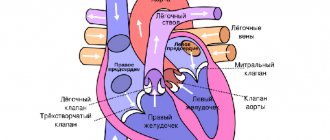
- The left ventricle contracts incorrectly, that is, weakly, which is why not enough blood enters the heart vessels.
- Compensation mechanism. It is triggered when the normal functioning of the heart muscle is necessary under difficult conditions. The layer on the left side of the organ thickens and hypertrophies, and the body releases more adrenaline. The heart begins to contract faster and stronger, and the pituitary gland produces a hormone, due to which the amount of water in the blood increases significantly.
- When the heart is no longer able to supply organs and tissues with oxygen, the body's reserves are exhausted. Oxygen starvation of cells occurs.
- Due to serious circulatory disorders, decompensation develops. The heart beats slowly and weakly.
- Heart failure occurs - the inability of the organ to supply the body with oxygen and nutrients.
ICD 10 code anasarca
Edema syndrome is an excessive accumulation of fluid in the tissues of the body and serous cavities, manifested by an increase in tissue volume and a change in the capacity of the serous cavity, a change in the physical properties and dysfunction of edematous organs and tissues.
A distinction is made between local (localized) edema, associated with fluid retention in a limited area of tissue of the body or organ, and general (generalized) - a manifestation of the positive water balance of the body as a whole.
Generalized edema includes edema due to heart failure, cirrhosis of the liver, nephrotic and nephritic, dropsy in pregnancy, cachectic and idiopathic, as well as as a result of chronic loss of potassium by the body due to the abuse of laxatives.
The following can contribute to the appearance of edema or accelerate their development: finylbutazone, pyrozolone derivatives, mineralocorticoids, androgens, estrogens, licorice root preparations. Localized edema includes: cerebral edema, pulmonary edema, edema of the extremities.
Local edema develops in the absence of general disturbances in water-eletrolyte metabolism and is associated with the presence of local disorders of hemo- and lymphodynamics, capillary permeability and metabolism. If, after pressing with a finger on the swollen skin, no pit remains, then the swelling can be classified as false. Such swelling occurs with myxedema, scleroderma, and obesity.
To differentiate edema of the lower extremities in venous insufficiency from edema caused by heart failure, venous pressure in the ulnar vein should be measured. Swelling of veins is mild or moderate in density, swollen skin is warm. With lymphostasis, irreversible subcutaneous thickening often occurs.
To recognize hydrothorax and ascites, both basic and additional examination methods may be needed (x-ray, laboratory analysis of intracavitary fluid, etc.).
During an objective examination, hydrothorax is characterized by limited mobility of the chest during breathing, weakened tremors, a dull percussion sound above the fluid, and a dull tympanic sound above its upper border.
Breathing above the area of dullness is weakened or absent; bronchial breathing may be heard above the upper border of dullness due to compression of the lung. X-ray with hydrothorax reveals a homogeneous characteristic darkening in the lower part of the pulmonary field.
During a test pleural puncture, we obtain a transudate, which is characterized by a low specific gravity (less than 1015), a protein content of less than 3%, and a poor cellular composition. In the presence of fluid in the abdominal cavity, the abdomen is convex, sags somewhat when the patient is standing and expands in the lateral sections when the patient is lying down (frog belly).
The navel area protrudes, the skin of the abdominal wall is smooth, shiny, sometimes with pink stripes. When percussing the abdomen with the patient in the supine position, a dull sound is detected in the lateral parts of the abdomen.
When the body position changes, the localization of dullness changes: if the patient is on the right side - dullness only on the right, if the patient is standing - dullness in the lower abdomen. Perquetometer determination of ascites is possible with the accumulation of at least 1.5 - 2 liters of fluid.
When there is a small amount of fluid, it is sometimes possible to obtain a dull sound in the navel area if you percussion from below along the anterior abdominal wall in the patient’s knee-elbow position.
With ascites of inflammatory origin, the characteristic distribution of percussion sound, as well as its change, with a change in body position, may not be observed due to the fusion of the loops of the intestine with each other and with the mesentery and the encystation of fluid.
The diagnosis of ascites is facilitated by the appearance of fluctuations: when you apply your hand to one side of the abdomen and tap on the abdominal wall on the arched side, vibrations are felt (fluid fluctuation). To eliminate vibration of the abdominal wall, the assistant places the palm of the elbow along the midline of the abdomen. Nephrotic edema is characterized by a gradual onset.
Swelling is localized not only on the face, especially in the eyelid area (swelling of the face is more pronounced in the morning), but also on the legs, lower back, genitals, and anterior abdominal wall. The swelling shifts quite quickly when changing body positions. Edema skin is dryish, soft, pale, sometimes shiny. Ascites often occurs, and hydrothorax occurs less frequently. Shortness of breath, as a rule, does not occur.
With nephritic edema, rapid (early) onset. Edema skin is pale, dense, at normal temperature. Edema is localized mainly on the face, as well as on the upper and lower extremities. Sometimes hydrothorax, hydropericardium. Edema in liver cirrhosis usually occurs in the late stages of the disease.
They manifest themselves predominantly as ascites, which is more pronounced than swelling in the legs. Sometimes hydrothorax is detected (usually right-sided). Edema skin is dense and warm. During the examination, clinical and laboratory signs of the underlying disease are revealed. Kachyktic edema - occurs with general starvation or a sharp lack of protein in food, as well as with diseases accompanied by loss of protein through the intestines (exudative forms of gastroentritis, ulcerative colitis, lymphangiectasia in intestinal tumors). Severe vitamin deficiencies, alcoholism. The swelling is usually small, localized on the legs and feet, and is often accompanied by puffiness of the face. If the whole body is swollen, then it is very mobile. Swelling skin, doughy consistency, dry. Characterized by general exhaustion, hypoglycemia, hypocholesterolemia, severe hypoproteinemia, hypoalbuminemia. Edema in pregnant women can be caused by heart failure, exacerbation of chronic glomerulonephritis, late toxicosis of a pregnant woman. Hydrops of pregnancy is detected after the 30th week, rarely after the 25th week of pregnancy. Edema skin is soft and moist. Swelling first appears on the legs, then on the external genitalia, anterior abdominal wall, anterior chest wall, lower back, back, face. Ascites and hemothorax are rarely found. Idiopathic edema. It is observed mainly in women of childbearing age who are prone to obesity and vegetative disorders. It rarely occurs in men. Sometimes after mental trauma and neuroinfections. The swelling is mild, localized mainly on the legs, and increases during the day and in the hot season. Swelling is often found on the eyelids and fingers. The skin on the legs is often cyanotic. Skin hyperesthesia is sometimes observed.
Nephrotic syndrome is characterized by low protein levels in the blood serum, prytheinuria, increased levels of lipids in the blood, and edema. The pathological process is based on dystrophic, degenerative processes in the kidneys. Nephrotic syndrome develops secondarily, being an integral part of many kidney diseases that occur with damage to the glomeruli.
These include chronic glomerulonephritis, glomerulonephritis in systemic connective tissue diseases, amyloidosis, diabetes mellitus, kidney damage due to sensitization by allergens. Patients with nephrotic syndrome are referred due to the appearance of edema; in the absence of edema, nephrotic syndrome can be detected by significant proteinuria.
The swelling gradually increases, affecting the subcutaneous tissue of the entire body (anasarca). Fluid can accumulate in the pleura, pericardium, and abdominal cavity. Urine is a small amount, sometimes up to 300 ml/day, sometimes dark, cloudy, specific gravity - 1030 - 1040, protein 3-5 g/day. The urine sediment contains renal epithelial cells, hyaline, granular, waxy casts, and leukocytes.
In the blood, protein is reduced, the amount of cholesterol is increased, and ESR is accelerated.
Source: https://phoenix-pharma.su/kod-po-mkb-10-anasarka/
Classification
According to ICD-10, CHF is divided into three stages depending on the course of the disease:
- First. Clinical manifestations occur in humans only after physical exertion, and there are no signs of stagnation in the blood circulation.
- Second. In one or two circles of the blood flow there are signs of stagnation.
- Third. Persistent disorders and irreversible processes in the body are observed.
Depending on the condition of the left ventricle, there are two types of CHF:
- systolic function of the left lower chamber of the heart is preserved,
- left ventricular dysfunction is observed.
Chronic heart failure is also divided into functional classes:
- I – ordinary physical activity does not provoke any clinical signs.
- II – during physical activity, symptoms of heart failure appear, so a person is forced to limit himself in work.
- III – the clinic is clearly expressed even with minor loads.
- IV – complaints arise in the patient at rest.
Emergency care for cardiac asthma.
Protocol code: E-014
The goal of the stage: restoration of the function of all vital systems and organs.
ICD-10 code(s):
I50.1 Left ventricular failure
Definition: Acute left ventricular failure (ALF) and its main manifestations - cardiac asthma and pulmonary edema - are a pathological condition caused by profuse sweating of the liquid part of the blood into the interstitial tissue of the lungs, and then into the alveoli, which is clinically manifested by severe suffocation, cyanosis and bubbling breathing .
Classification:
1. Congestive type: left ventricular acute heart failure (cardiac asthma, pulmonary edema); right ventricular acute heart failure (venous congestion in the systemic circulation).
2. Hypokinetic type . cardiogenic shock.
Cardiac asthma occurs more often in the presence of organic changes in the cardiovascular system, leading to a weakening of the contractility of the left ventricle (hypertension, acute myocardial infarction, cardiosclerosis, stenosis of the left venous orifice, aortic heart defects, diffuse glomerulonephritis, etc.).
Emergency aid tactics:
Algorithm for providing emergency care for ALV:
1. Inhalation of alcohol vapor through a nasal catheter (anti-foaming).
The initial rate of oxygen introduction (through 96°C ethyl alcohol) is 2-3 l/min, for several (up to 10) minutes. When the mucous membranes get used to the irritating effect of the gas, the speed is increased to 9-10 l/min. Inhalation is continued for 30-40 minutes with 10-15 minute breaks.
2. Relieving “respiratory panic” with narcotic analgesics . morphine
Dilute 1.0 ml of a 1% solution in 20 ml of a 0.9% sodium chloride solution and administer intravenously in fractional doses of 4-10 ml (or 2-5 mg) every 5-15 minutes until pain and shortness of breath are eliminated.
3. Heparin 5000 units intravenously.
POINTS 1-3 ARE MANDATORY!
4. With normal blood pressure:
— sit the patient down with the lower limbs lowered;
- sublingual nitroglycerin in tablets (0.5-1 mg), or aerosol, or spray (0.4-
0.8 mg or 1-2 doses); or intravenously 0.1% alcohol solution up to 10 mg in 100 ml of isotonic sodium chloride solution dropwise, increase the rate of administration from
25 mcg/min until effect is achieved under blood pressure control until effect is achieved;
- furosemide 40-80 mg intravenous bolus;
- diazepam intravenously in fractional doses until the effect is achieved or a total dose of 10 mg is reached.
5. For arterial hypertension :
- sit the patient down with the lower limbs lowered;
- nitroglycerin tablets (preferably aerosol) 0.4-0.5 mg sublingually, once;
- furosemide 40-80 mg intravenous bolus;
- nitroglycerin intravenously 0.1% alcohol solution up to 10 mg in 100 ml
isotonic sodium chloride solution drip, increasing the rate of administration from 25 mcg/min until the effect is achieved under the control of blood pressure until the effect is achieved, or sodium nitroprusside 30 mg in 300 ml of 5% dextrose solution intravenously drip, gradually increasing the rate of infusion of the drug from 0.3 mcg/ (kghmin) until the effect is achieved, controlling blood pressure;
- diazepam intravenously in fractional doses until the effect is achieved or a total dose of 10 mg is reached.
6. For moderate hypotension (systolic pressure 75 – 90 mmHg):
- lay the patient down, raising the head of the bed;
- dopamine 250 mg in 250 ml of isotonic sodium chloride solution, increasing the infusion rate from 5 mcg/(kghmin) until blood pressure is stabilized at the lowest possible level;
- furosemide 40-80 mg intravenously.
7. In case of severe arterial hypotension:
- lay the patient down, raising the head of the bed;
- dopamine 200 mg in 400 ml of 5% dextrose solution intravenously, increasing the infusion rate from 5 mcg/(kgmin) until blood pressure is stabilized at the lowest possible level;
- with increased blood pressure, accompanied by increasing edema
lungs, - additionally nitroglycerin intravenously drip 1% alcohol solution until
10 mg in 100 ml isotonic sodium chloride solution, increase speed
administration from 25 mcg/min until effect under blood pressure control until effect is achieved;
- furosemide 40-80 mg intravenously only after stabilization of blood pressure.
8. Monitoring vital functions of the body (cardiac monitor,
pulse oximeter).
Indications for emergency hospitalization: In case of severe pulmonary edema, hospitalization is possible after its relief or by specialized emergency medical teams. The patient is transported in a sitting position.
Causes
The ICD code for CHF is I50. This syndrome, in fact, is an unfavorable outcome of most heart diseases, and especially coronary artery disease and hypertension (up to 85% of cases). A quarter of cases of CHF can be caused by the following reasons:
- myocarditis,
- cardiomyopathy,
- endocarditis,
- heart muscle defects.
Very rarely, factors such as:
- arrhythmia,
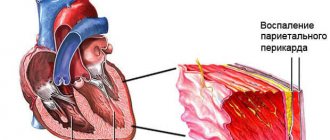
- pericarditis,
- rheumatism,
- diabetes,
- excess weight,
- metabolic disease,
- anemia,
- heart tumors,
- chemotherapy,
- pregnancy.
In any case, if a person suffers from any of the above-mentioned disorders, his heart gradually becomes weaker and its pumping function deteriorates.
Other forms of acute coronary heart disease (I24)
Excluded:
- angina (I20.-)
- transient neonatal myocardial ischemia (P29.4)
Coronary (artery) (vein):
- embolism
- occlusion
- thromboembolism
https://www.youtube.com/watch?v=ytcopyrightru
not leading to myocardial infarction
Excluded: chronic coronary thrombosis or an established duration of more than 4 weeks (more than 28 days) from onset (I25.8)
Coronary:
- failure
- inferiority
Excludes: coronary heart disease (chronic) NOS (I25.9)
In Russia, the International Classification of Diseases, 10th revision (ICD-10) has been adopted as a single normative document for recording morbidity, reasons for the population's visits to medical institutions of all departments, and causes of death.
ICD-10 was introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997. No. 170
The release of a new revision (ICD-11) is planned by WHO in 2017-2018.
With changes and additions from WHO.
The acute form of coronary vascular insufficiency syndrome (ACS) can develop into a complicated form of pathology and appear with the following consequences:
- Heart muscle rhythm disorders - arrhythmia;
- Transition of pathology into an acute form of failure with a fatal outcome;
- Inflammation of the cardiac pericardium - pericarditis;
- The disease is an aortic aneurysm;
- Coronary artery rupture in ACS.
In order to prevent the transition of coronary insufficiency (ACS) to a complicated form of pathology, it is necessary to strictly follow all the recommendations of the treating doctor.
Clinical picture
Signs of chronic heart failure depend on the severity of the disease and accompanying disorders in the body. Typical complaints of patients with CHF are:
- development of shortness of breath. First, rapid breathing appears due to physical activity, later – even at rest;
- night suffocation is a phenomenon when the patient wakes up from the fact that he cannot breathe and feels the need to get out of bed;
- shortness of breath in an upright position (it happens that the patient has difficulty breathing while standing or sitting, but when he lies on his back, the breathing rate normalizes);
- general weakness and fatigue;
- dry cough resulting from stagnation of blood in the lungs;
- nocturnal diuresis prevails over daytime diuresis (frequent urination at night);
- swelling of the legs (first the feet and legs swell symmetrically, then the thighs);
- development of ascites (fluid accumulation in the abdomen).
Another pronounced sign of chronic heart failure is orthopnea - a forced position of the patient in which he lies with his head elevated, otherwise he will experience shortness of breath and a dry cough.
What are the features
The syndrome is manifested by a fairly large list of signs that indicate the patient’s development of myocardial infarction in the acute stage of development. Experts note that this condition does not appear as a separate disease, but only as a syndrome.
https://www.youtube.com/watch?v=https:accounts.google.comServiceLogin
In some cases, coronary heart disease and ACS are identified. But that's not true. With ischemic heart disease, a small section of the mitral valve dies, which is accompanied by the manifestation of one or more symptoms.
Whereas with the syndrome, almost all signs of ischemia or angina appear.
If the signs that appear in a patient during an attack of acute coronary syndrome primarily indicate the development of cardiac ischemia, he needs urgent medical care. Otherwise, death is possible. If the suspicion falls on unstable angina, the patient’s condition is not so serious.
But this in no way means that there is no need to conduct a thorough examination of the person’s condition.
No one can be absolutely sure how ACS may end: ischemic heart disease or angina pectoris. This means that at the slightest suspicion you should immediately contact a specialist.
Diagnostic measures
When diagnosing a patient, one cannot do without a visual examination, during which the doctor will clearly see the typical symptoms of CHF - swelling, pulsation and swelling of the veins, enlarged abdomen. On palpation, “splashing noises” are detected, which confirm the presence of free fluid in the peritoneum.
Auscultation can reveal fluid accumulation in the lungs (moist rales). The patient's heart and liver are enlarged in size.
To clarify the diagnosis, the doctor prescribes a number of hardware tests:
- electrocardiogram - reveals changes inherent in diseases that led to chronic heart failure;
- Ultrasound of the heart - allows you to detect expansion of the organ cavities, signs of regurgitation (reflux of blood from the ventricles back into the atria), and also study the contractility of the ventricles;
- Chest x-ray - helps to determine the size of the heart, as well as detect congestion in the lungs.
Symptoms
The picture of vertebrobasilar insufficiency is extremely diverse. One of the most common manifestations of vertebrobasilar insufficiency is sudden onset of dizziness. The frequency of this symptom may be due to the characteristics of the blood supply to the vestibular apparatus, which is very sensitive to insufficient blood supply. In most patients with vertebrobasilar insufficiency, dizziness manifests itself in the form of a sensation of rotation or linear movement of surrounding objects or one’s own body. Dizziness usually occurs quickly and lasts from a few minutes to hours. As a rule, it is accompanied by disorders such as nausea, vomiting, sweating, changes in heart rate and blood pressure. In some cases, the patient experiences a feeling of sinking, motion sickness, and unsteadiness of the surrounding space. Motor disorders in patients with circulatory disorders in the vertebrobasilar system consist in the development of weakness and clumsiness in the limbs. A common manifestation is unilateral hearing loss - sensorineural hearing loss. Tremor.
Treatment
The main principle of treatment for chronic heart failure is to slow the progression of the disease as well as relieve symptoms. Conservative therapy involves lifelong use of heart medications and other medications that improve the patient’s quality of life.
The drugs prescribed by the doctor for CHF include:
- ACE inhibitors, which lower the level of pressure inside blood vessels;
- beta blockers, which reduce heart rate and overall vascular resistance, allowing blood to move freely through the arteries;
- cardiac glycosides, which increase the contractility of the heart muscle while reducing the contraction frequency;
- anticoagulants that prevent thrombosis;
- calcium channel antagonists, which relax blood vessels and help lower blood pressure;
- nitrates, which reduce blood flow to the heart muscle;
- diuretics - prescribed to relieve congestion in organs and reduce swelling.
Diagnostics
A full diagnostic program is carried out only after the patient’s condition has been stabilized. Be sure to notify the doctor about what medications were given to the patient as first aid.
General analysis of blood and urine;
Biochemical blood test - the level of cholesterol, sugar and triglycerides is determined;
Coagulogram – to determine the level of blood clotting;.
ECG is a mandatory method of instrumental diagnostics for ACS;
Coronary angiography - to determine the location and degree of narrowing of the coronary artery.
https://www.youtube.com/watch?v=ytpressru
To make an accurate diagnosis, it is necessary to go through the following stages of examination:
- Primary medical history of the patient. In this case, the doctor listens to all the patient’s complaints and conducts auscultation. An extremely important point at this stage is familiarization with the patient’s working and living conditions, as well as with the presence of various diseases in close relatives.
- Laboratory examination:
- general blood analysis;
- analysis to determine the level of two types of cholesterol;
- blood biochemistry;
- determination of blood sugar levels;
- study of blood clotting rate;
- OA of urine.
- Electrocardiogram. This method is considered the most effective. Especially if the results are taken during the attack and after it. This will make it possible to determine how the heart rate or the volume of its cavities changes under different conditions.
- Ultrasound examination of the heart. This type of examination makes it possible to determine the size and structure of the heart parts, examine the characteristics of blood flow, assess the level of development of atherosclerosis of blood vessels and heart valves, and detect the presence of a violation of the heart rate.
- Coronary angiography. It is one of the types of x-ray examination of the heart, which helps to obtain information about the localization and degree of development of narrowing of the coronary arteries.
If such a need arises, you will have to resort to the help of specialized specialists or more complex examination methods.
Consequences
If the patient takes a responsible approach to his health and does not delay his visit to the doctor, and then follows all the appointments, then, most likely, the course of the disease will be favorable until complete recovery.
If these conditions are not met, the disease will progress, TIA may be complicated, and chronic and acute (stroke) circulatory disorders in the brain will occur. Such consequences of vertebrobasilar insufficiency can have a very serious impact on later life and health.
Source
Prevention
For patients who suspect that they may develop vertebrobasilar insufficiency, it is recommended for prevention:
- Proper nutrition with plenty of vegetables, fruits, foods rich in vitamin C, seafood, low-fat dairy products and limiting flour products, salty and fatty foods;
- Quitting nicotine and alcoholic beverages;
- Limiting table salt;
- Light exercise, as described above or otherwise;
- Treatment of hypertension;
- If possible, avoid a sedentary lifestyle;
- Use of orthopedic pillows and beds;
- Avoiding nervous overload;
- Walk outdoors;
- Swimming and water aerobics in natural reservoirs or a pool;
- Observation by a neurologist.