Medical editor: Strokina O.A. - therapist, functional diagnostics doctor. September, 2020.
ICD-10 code: I31.1.
Constrictive pericarditis is compression of the heart by the yielding pericardium (outer lining of the heart). Symptoms include increased fatigue, a feeling of lack of air, swelling in the legs, bloating, and a decrease in the difference between systolic and diastolic pressure. Diagnosis is based on pericardial visualization methods: Echo-CS, MRI, CT. Laboratory tests are necessary to determine the cause of constrictive pericarditis. The complication can only be treated surgically, but drug support (aspirin, NSAIDs, colchicine, diuretics and others) is also possible if surgical intervention is not possible.
Constrictive pericarditis is a serious complication of acute fibrinous, serous-fibrinous and chronic exudative pericarditis. With its development, compression of the heart by the pericardium itself occurs due to the growth of coarse scar tissue in it. It restricts the natural movement of the heart in the pericardial cavity, preventing the ventricles from filling with blood, which leads to symptoms similar to cardiac tamponade.
What it is?
The pericardium is the outer cardiac membrane made of connective tissue, separated from the epicardium of the heart by a cavity filled with serous fluid. Essentially, it is a cardiac sac in the form of a thin-walled, dense sac. Inflammation of this membrane is called pericarditis.
This disease is classified according to etiological and clinical characteristics and has several characteristic varieties. One of the most severe forms is constrictive pericarditis , which is a chronic form of the adhesive type.
Constrictive pericarditis develops as a result of infection or is a consequence of a number of diseases, incl. other types of pericarditis, for example, fibrinous.
ICD-10 code
ICD-10 code: I31.1 - chronic constrictive pericarditis (Concretio cordis, pericardial calcification).
Does it occur in children?
Constrictive pericarditis can also develop in childhood.
It is found even in newborns. The etiology of the disease may be infectious in nature or based on an autoimmune, allergic or rheumatoid mechanism. Symptoms of childhood pathology are practically no different from its manifestations in adults. Important! In infants, the reaction to pain may be anxiety and crying.
Little older children try to take a semi-sitting position with their heads tilted forward. Read more about pericarditis in children and their frequency here.
FAQ
- What does the word “constrictive” mean in the name of the diagnosis?
The term “constrictive” indicates the compressive nature of the effect (“contsrictio” is translated from Latin as “compression”) on the heart, so this type of disease is sometimes called constrictive pericarditis. - How is it different from exudative?
Constrictive pericarditis (CP) is fundamentally different from another characteristic type - exudative pericarditis. Compression of the epicardium occurs as a result of thickening of the visceral layers or “shrinking” of the sac during fusion of the layers, loss of elasticity and calcification. Exudative pericarditis is characterized by the accumulation of effusion (exudate) in the pericardial cavity, released during an inflammatory reaction. - Can it occur as a result of a heart attack and why?
Myocardial infarction can provoke this pathology. In this case, sections of the muscle die, and as a result of oxygen starvation, the replacement of muscle tissue with rough, connective tissue begins. - Does heart failure develop against the background of constrictive pericarditis?
As constrictive pericarditis progresses, heart failure appears. The hardened pericardium compresses the heart, disrupting the diastolic filling of the ventricles, which does not allow the organ to function fully. Developing heart failure impairs blood supply to all body systems, which affects the general condition of a person.
Gradually, it becomes irreversible (untreatable) with an increase in ascid and the appearance of trophic disorders.
Prevention
Prevention of the development of constrictive pericarditis can be considered treatment of the underlying disease, which leads to the formation of effusion in the pericardial cavity. If the necessary therapeutic measures are taken at this stage, the formation of adhesions and fusion of the cavity of the pericardial sac can be avoided.
Did you like the article? Save it!
Still have questions? Ask them in the comments! Cardiologist Mariam Harutyunyan will answer them.
Mariam Harutyunyan
Graduated from Yerevan State Medical University. M. Heratsi. Cardiologist
Causes and risk factors
Constrictive pericarditis occurs due to:
- deep and penetrating wounds in the area of the heart and sternum;
- closed chest injuries;
- previous myocardial infarction or other heart diseases.
- infectious diseases, against the background of tuberculosis, rheumatism.
The occurrence of this pathology is also influenced by diseases that cause metabolic disorders in the body (gout, kidney or liver failure, etc.).
The risk group for this type of pericarditis includes people:
- have undergone various heart surgeries;
- those who have been in car accidents, fallen from a great height, or received any blunt chest injuries;
- patients with tuberculosis (a risk group that makes up the largest percentage of cases);
- those suffering from autoimmune diseases (in the case when the body rejects its own tissues, considering them foreign);
- those who have undergone radiation therapy due to cancer;
- having increased sensitivity to medications and substances in their composition.
It is impossible to clearly formulate the exact number of reasons due to which constrictive pericarditis develops. Sometimes its causes remain unclear (that is, the disease is considered idiopathic); cases of congenital pathology are less common.
Most often, the course of this disease has a cycle . Symptoms appear and disappear, becoming more pronounced only in the almost terminal stage.
Find out what disruption of repolarization processes looks like on an ECG in adults. This information will be useful for deciphering the cardiogram.
Is a sharp deviation of the electrical axis of the heart to the left dangerous? Find out all about the features of this condition and what it means.
How to determine diffuse changes in the myocardium on an ECG? A detailed explanation is in this material.
Symptoms
Constrictive pericarditis is a progressive disease. Its development is indicated by four periods with corresponding symptoms.
Hidden
During this period of time, the disease has no obvious symptoms. If the pathology accompanies previously suffered pericarditis in acute or primary chronic forms, then light adhesions may form in the pericardial area. Their appearance does not in any way affect the functions of the cardiovascular system.
Elementary
Symptoms accompanying the initial period of constrictive pericarditis are expressed:
You can also read:What is effusion pericarditis
- Weakness.
- Shortness of breath.
- Swelling of the face and lower extremities.
- Increased venous pressure.
- Tachycardia.
- Bloating with general exhaustion.
The course of the disease during this period is due to fibrous compression of the heart and impaired hemodynamics.
Expressed clinical manifestations
The period of pronounced clinical manifestations is marked by severe weakness and a progressive rise in central venous pressure. The level of the latter exceeds 300 mm. water Art. At the same time, swelling noticeably increases. Cyanosis of the face and cervical region increases, and ascites develops.
Dystrophic
The dystrophic period of constrictive pericarditis is expressed by a general deterioration in health and exhaustion. At this time, degenerative changes begin in the patient’s organs. The liver stops functioning normally. The whole body undergoes edema, asthenic syndrome manifests itself. Skeletal muscles gradually atrophy, trophic ulcers appear and the heart rhythm is disturbed.
Constrictive pericarditis can be complicated by myocardial failure, atrial fibrillation, cardiac cirrhosis, exudative enteropathy and nephrotic syndrome.
Clinical picture that suggests the development of
At the onset of the disease, signs such as shortness of breath worsening with exertion, weakness and fatigue, loss of appetite and weight loss are noted. As heart failure develops (usually of the right ventricular type), pain occurs in the hypochondrium on the right side, ascites and local swelling.
The progression of constrictive pericarditis leads to a characteristic set of symptoms:
- enlarged belly against the background of general weight loss;
- enlarged neck veins (Kussmaul's sign), when they swell noticeably during inspiration;
- swelling of the lower extremities;
- dilated veins in the abdominal area;
- high blood pressure.
Many patients have a paradoxical pulse with subsidence on inspiration. Upon palpation, an increase in the size of the spleen and liver can be detected. During auscultation of the heart, a characteristic pericardial click is detected.
Changes in symptoms by stage
The clinical picture of constrictive pericarditis varies according to stages. The following main symptoms are distinguished depending on the period of development of the disease:
- Initial stage. At this stage, constrictive pericarditis is characterized by cicatricial compression, leading to shortness of breath during exercise and prolonged walking. After physical activity, there is puffiness on the face, expansion of the neck veins, and increased venous pressure. Signs of the onset of the disease are detected only after exercise, and the manifestation depends on their intensity and duration.
- Expressed stage. At this stage of the disease, stable venous hypertension appears, leading to puffiness of the face, cyanosis of the face, ears and hands, and enlargement of the neck veins. Ascites appears. Shortness of breath becomes sensitive and manifests itself at the slightest exertion. Possibly causing liver problems.
- Dystrophic stage. This is an advanced stage of the disease, when swelling occurs in the lower extremities and parts of the body, and then in the arms and face. Liver functions are impaired. Blood coagulation activity decreases significantly, hypoprothrombinemia and hyperfibrinogenemia occur. Trophic ulcers and joint contracture may appear.
Important! Constrictive pericarditis tends to progress rapidly. The onset of the dystrophic phase depends on the degree of compression and the nature of hemodynamic disturbances.
Shell heart
A neglected CP can develop into the form of calcified pericarditis. It is characterized by the formation of a “shell heart”, which is a heart sandwiched by a tough, hard shell, compacted with calcium deposits.
Unlike a typical KP, when the organ is compressed by connective tissue (fused sheets), the “armored heart” is compressed by granulation tissue, in which adhesions are strengthened with calcium salts.
The organ is firmly blocked by the shell and does not have the ability to fully expand when the ventricle is filled with blood.
What is the cause of the “shell heart”? It is generated by calcification of the pericardium . At the initial stage, foci of calcification appear due to the deposition of salts from hemorrhagic fluid appearing in the pericardial cavity. Such lesions can also appear in the connective tissue itself when its blood supply is disrupted.
As the disease progresses, a large amount of salts accumulates, which can first form a stripe and then cover the entire pericardium.
Symptoms of calcified pericarditis correspond to an advanced stage of KP and indicate the development of heart failure . The patient complains of shortness of breath, pain in the chest and right hypochondrium. His belly is enlarged and his legs are noticeably swollen. Pseudocirrhosis of the liver develops, as evidenced by an increase in its size.
Erythrocyte sedimentation rate is increased - what does this mean? Features and a number of factors that influence this indicator are discussed in our article.
This material will tell you what a blood test for a coagulogram shows, how the results are interpreted and what they should be normally.
Do you know why rheovasography of the upper and lower extremities is needed? These studies are described here.
Symptoms of constrictive pericarditis
The clinical picture of constrictive pericarditis can develop over months, and sometimes years, and is associated with impaired blood supply to the ventricles of the heart due to their gradual compression. The right ventricle begins to suffer most quickly with the development of stagnation in the systemic circulation. Then the clinic is joined by left ventricular failure (shortness of breath, suffocation, cough) and failure of other internal organs, in particular the liver.
Patients diagnosed with “constrictive pericarditis” complain:
- increased fatigue;
- peripheral edema (legs, arms);
- lack of air;
- bloating;
- decreased appetite;
- swelling of the neck veins;
- decrease in pulse blood pressure - the difference between systolic and diastolic blood pressure;
- paradoxical pulsus (decrease in systolic blood pressure by more than 10% during inspiration during quiet breathing) in 30% of cases.
Some of the listed symptoms indicate stagnation of blood in the systemic circulation due to the development of right ventricular failure - ascites (fluid in the abdominal cavity), accumulation of effusion in the pleural cavity, enlargement of the liver, venous stagnation in the veins of the lower extremities.
Diagnostics
The disease can be diagnosed or prevented by taking into account the following factors:
- previous heart surgeries, injuries, bad habits;
- presence of autoimmune diseases;
- data obtained as a result of electrocardiography;
- general examination of the patient and identification of pathological signs;
- the presence of light spots in the heart area on a chest x-ray.
Very often, constrictive pericarditis is discovered completely by accident : after assessing the results of a puncture or the results of an x-ray (the heart, which is “imprisoned” by calcified tissue, in the picture has the same white color as bone tissue).
Diagnostics includes:
- X-ray examinations;
- computed tomography;
- electrocardiogram and echocardiography;
- cardiac catheterization;
- laboratory research.
The patient's medical history is of greatest importance in making a diagnosis.
Since constrictive pericarditis is often a consequence of past infectious diseases, it is necessary to know which diseases preceded the onset of at least some of the symptoms. Heart murmurs are also a sign of pathology : they are created by the petals of the pericardium rubbing against each other. However, if fluid accumulates between the pericardium and the heart, that is, a very advanced case occurs, then instead of noise, moist rales may be heard in the lungs.
We talked about methods for diagnosing pericarditis here.
EchoCG signs
Echocardiography (EchoCG) is extremely important for identifying KP. With this pathology, thickening of the pericardial layers is detected (most noticeable during transedible echocardiography), displacement of the interventricular septa in the posterior direction during inspiration, enlargement of the inferior vena cava and hepatic vein, and dilatation of the atria.
An increase in pericardial thickness is determined by 2 signals directed from the visceral and parietal layers. They reveal the fusion of leaves. The nature of the signals makes it possible to identify blocking of the mobility of the left ventricular posterior wall and the zone of calcification as the pathology progresses.
Characteristic echocardiographic signs
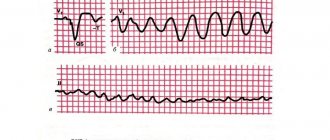
ECG signs
An electrocardiogram (ECG) reveals abnormal heartbeats. The most typical symptoms of constrictive pericarditis
- low voltage (amplitude) of the ventricular QRS complex;
- high, widened P wave, double-humped;
- flattening and inversion of the T wave.
In almost half of the cases of KP, the presence of atrial fibrillation is determined. At an advanced stage, it is possible to reach the connective tissue of the myocardium, which affects conductivity. The ECG records bundle branch block, indicating a violation of intraventricular conduction, as well as AV block, characteristic of a violation of atrioventricular conduction.
What will be seen on the ECG
Differential diagnosis
A diagnosis is made through an external examination, laboratory and instrumental studies. However, when diagnosing KP, it is important to differentiate it from similar diseases that lead to heart failure. Among such pathologies, myocardial lesions, heart defects, and other types of pericarditis stand out.
An important distinguishing feature is the expansion of the veins during inspiration and a sharp increase in venous pressure.
Radiography plays an important role in differential diagnosis. Unlike some heart defects that have similar manifestations, there are no auscultatory symptoms with KP . With pericarditis of the exudative type, an increase in the size of the heart is detected, which does not occur with KP. In addition to cardiac diseases, pericarditis should be separated from liver pathologies, in particular cirrhosis.
Differences from cardiac tamponade
What happens to the heart during constrictive pericarditis?
Constrictive pericarditis is an advanced chronic stage of pericarditis. What is characteristic of constrictive pericarditis is that when it is present, the body loses the ability to remove fluid in the required volume, which begins to accumulate between the lobes of the pericardium and put pressure on the heart, preventing it from contracting and pumping blood normally. Under these conditions, the “motor” of the body is constantly working under overload.
Over time, the fluid may resolve, and the pericardial walls will become denser and stiffer due to their calcification. Therefore, there is a direct connection between constrictive pericarditis and the “shell heart”, which is no longer able to fill with blood to the required extent and pump it in sufficient quantities to other organs. As a result, from constant overload, the myocardium itself is destroyed, the period of its normal functioning is sharply reduced, at the same time, all other organs experience a lack of nutrition and oxygen, which is also fraught with serious illnesses.
According to statistics, constrictive pericarditis is not a common disease; many sources claim that it most often affects men. Although women suffer from it quite often.
Treatment
Depending on the stage of the disease, treatment is prescribed. If a diagnosis of KP is made, then you can try to eliminate the problem with therapeutic methods. Sometimes it is possible to slow down the course of the disease or completely stop it by taking antibiotics, glucocorticosteroids and NSAIDs. Diuretics are helpful. They reduce the likelihood of ascites and edema. If atrial fibrillation is present, Digoxin sometimes helps.
Therapy prescribed by a doctor for 2.5-4 months can significantly improve the general condition of a sick person.
The only effective way to combat advanced forms of constrictive pericarditis and “shell heart” is considered to be surgery . As a rule, it involves a surgical operation - pericardiectomy. It is prescribed when blood pressure in the jugular veins rises to more than 75-85 mm H2O.
Severe heart failure with circulatory disorders also becomes an indication. The operation involves excision of scar bridges, and, if necessary, partial or complete removal of the pericardium with the release of veins from the connective tissue.
Another surgical treatment option is pericardiocentesis. It represents a puncture of the pericardium. This operation is performed during cardiac tamponade to pump out fluid from the pericardial cavity. The most commonly used extrapleural approach is when the needle is inserted into the area between the urinary process and the left costal arch.
After surgery, the rehabilitation process takes a relatively short time: as a rule, after 2.5 - 3 months after the operation, the patient can already return to his usual lifestyle . In the first months after treatment, which is accompanied by positive dynamics, you should avoid excessive physical stress on the heart, and also be under the constant supervision of your doctor. Further, all procedures will be aimed at preventing the disease.
The treatment tactics for all types of pericarditis are described in this material.
Duplex scanning of the brachiocephalic arteries - what is it, why is it prescribed and how does it affect the diagnosis? Find out everything!
Why do you need a blood test for ferritin, how to take it correctly and interpret the results? All details are described here.
Alkaline phosphatase in the blood - what is it, what is it responsible for and does it fit into the norm? We'll tell you!
Treatment of constrictive pericarditis
Despite the fact that the basis of treatment for constrictive pericarditis is surgical methods, conservative treatment can also affect its course.
Drug therapy
Etiotropic therapy refers to the treatment of the identified cause of the disease, which helps prevent relapses. An example is tuberculous pericarditis. Antibacterial drugs aimed at combating tubercle bacilli can reduce the risk of developing constriction from 80% to 10%.
Resolution of the transient version of the constriction when it is “cured”, but after a few months it returns. For this purpose, standard anti-inflammatory therapy is usually used - aspirin or NSAIDs (non-steroidal anti-inflammatory drugs - indomethacin, ibuprofen).
Maintenance drug therapy (mainly diuretics) to reduce signs of blood stasis in cases where it is impossible to use surgical techniques - contraindications or high risk of surgery.
Surgery
Speaking about the surgical treatment of constrictive pericarditis, it is worth mentioning that there are several specific forms of it, which imply different tactics for managing patients:
The transient variant is treated with anti-inflammatory drugs and resolves within a few weeks. Constriction occurs precisely due to inflammation of the pericardial layers with their thickening. Accordingly, when inflammation passes, constriction also passes. Therefore, in the absence of data on a chronic process, a patient with newly diagnosed constrictive pericarditis is recommended to first undergo 2-3 weeks of conservative therapy before resorting to surgical methods.
Effusion-constrictive pericarditis is treated with pericardectomy (excision) of the visceral layer (closest to the heart).
Chronic constrictive pericarditis is treated only with pericardiectomy. The operation must be treated very carefully, especially in patients with the last stage of development of constriction. Since surgery itself will not greatly improve their quality of life, and the risk of death is very high and amounts to 6-12%.
Immediate and long-term complications, prognosis
Compression of the heart by the affected pericardium interferes with the filling of the ventricles, blocking their expansion. As a result, hypertension occurs in the systemic veins and right ventricular failure develops. The immediate complication of the pathology is cardiac arrhythmia, gradual atrophy of the heart muscle and a decrease in cardiac mass.
With a long course of the disease, long-term complications can be expected in the form of accumulation of calcium deposits (calcification) and the formation of a hard “shell” around the heart (“armored heart”). Progressive PC spreads sclerotic lesions to surrounding tissues (pleura, diaphragm, coronary arteries).
Diffuse type myofibrosis and coronary insufficiency develop. The proliferation of connective tissue can reach the capsule of the liver and spleen, causing their damage and functional impairment.
In its advanced stage, the disease has a poor prognosis . Impaired blood supply causes tissue atrophy, which leads to irreversible consequences. Surgical treatment can prolong the patient’s life, but disability is difficult to avoid.
If treatment is insufficient or ineffective, the prognosis is unfavorable, but if the disease is diagnosed in time, then one can hope for a successful resolution of the problem.
Prognosis, complications and consequences
Typically, patients face bad news if they do not receive timely therapy, are not allowed to undergo surgery, or do not respond to pericardiectomy. Most often, operations prolong the life of patients by 10 to 15 years. Under certain conditions, you can adhere to certain liberties during this time:
- If there is no decompensation, you can give physical stress to the body during this period.
- If residual nuances in the form of heart failure are observed, a disability group should be obtained.
If timely diagnosis and therapy are not carried out, the patient will face the following complications:
- Arrhythmia appears. We have already discussed what it entails in one of the previous articles.
- Armored heart syndrome. This disorder occurs as a result of the accumulation and deposition of calcium in the place where the pericardium becomes inflamed. Thus, a shell-like plaque forms around the main muscle, which makes it difficult to work.
- Ascites. It is an accumulation of fluid in the abdominal area. Its quantity in the cavity can reach 25 liters.
What does a “shell heart” look like in cross section?
- Cardiac tamponade. In this case, the heart is compressed by the fluid around it as a result of a problem with the pericardium.
- Heart failure. It develops quite often if you do not follow the basic rules of health care. If there is insufficiency, the muscle cannot fully perform its functions.
Prevention recommendations
There are no specific preventive measures for KP. To reduce the risk of the disease, it is necessary to promptly and effectively combat infections, as well as other diseases that can provoke pericarditis. Chest injuries should not be allowed. If signs of the disease appear, you should immediately consult a doctor.
Measures to prevent constrictive pericarditis include:
- quick and timely treatment of infectious, fungal and purulent diseases;
- eliminating foci of possible infection;
- systematic examination by specialists, and conducting timely research when symptoms appear;
- prevention of sternum injuries;
- maintenance treatment for chronic diseases;
- balanced diet;
- rejection of bad habits.
Constrictive pericarditis is a dangerous cardiac problem that can lead to serious consequences. It requires mandatory treatment, and the only effective method is surgery. In the absence of timely, adequate treatment, the prognosis for survival is unfavorable.
Types of disease
Based on the cause of constrictive pericarditis, the following types of disease are distinguished:
- Infectious, caused by infection, possible inflammation of the pericardial sac.
- rheumatic – caused by streptococcus, a microorganism that causes rheumatic diseases;
- bacterial – appearing due to numerous bacteria (with pneumonia, sepsis, anthrax and other infections);
- tuberculous – is a complication of tuberculosis;
- protozoal – caused by simple microorganisms;
- fungal – appears when the body is exposed to a fungus;
- viral – occurs during viral infections.
- Aseptic (occurs due to inflammation that is not associated with infection).
- allergic – caused by manifestations of an allergic reaction;
- caused by blood diseases (poor blood clotting due to changes in the composition of platelets responsible for this process);
- constrictive pericarditis caused by connective tissue diseases due to systemic diseases that spread to all organs and disrupt the structure of tissues with supporting function;
- caused by malignant tumors or blood diseases;
- traumatic - pericarditis caused by injuries after damage or injury to the heart muscle, blunt or closed trauma to the heart;
- caused by metabolic disorders, for example, after uremia, a disease that promotes the accumulation of uric acid in the blood after problems with the kidneys.
- radiation – resulting from damage received from radiation;
- caused by long-term use of drugs, after which changes in the heart began; may occur after incorrect intake or use of: corticosteroids - substances used to reduce inflammation from rheumatism, which appears as a complication after scarlet fever or tonsillitis, during which damage occurs in the heart muscle; after bronchial asthma (in case of malfunction of the bronchial tubes) or other similar diseases;
- medicines for tumors or the effects of chemotherapy;
- vaccinations in the presence of intolerance to one of the components.
- Idiopathic pericarditis. Occurs for no apparent reason.
Complications
Constrictive pericarditis is especially dangerous because it is difficult to detect in time. The symptoms accompanying it at the initial stage are often associated with a common loss of strength, a general deterioration in health, stress, and vitamin deficiency. When this disease is not treated, it can lead to unpleasant and even serious complications:
- arrhythmia;
- pulmonary edema;
- enlargement of the collar zone due to highly swollen veins;
- ascites - a huge, fluid-filled (up to 20 l) abdomen;
- heart failure;
- the ongoing calcification of the tissues surrounding the heart first leads to its dysfunction, and then the process can reach a complete stop.
The type of complications also depends on the type of constrictive pericarditis. If it is accompanied by the accumulation of exudate, then the latter puts increasing pressure on the myocardium. If this situation was not detected in a timely manner, the likelihood of death increases sharply.