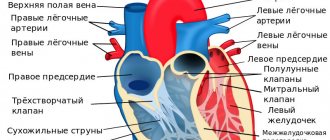
Structure of the heart: valves
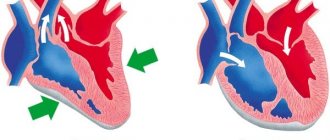
The heart is a hollow organ that consists of 4 chambers. The left and right halves are separated by septa, in which there are no formations, however, between the atrium and ventricle of each side there is an opening equipped with a valve. These formations allow you to regulate blood circulation, preventing regurgitation, that is, backflow.
On the left there is the mitral valve, consisting of two leaflets, and on the right - the tricuspid valve, it has three leaflets. The valves are equipped with tendon threads, which ensures that they open only in one direction. This prevents blood from flowing back into the atria. At the junction of the left ventricle and the aorta there is an aortic valve. Its function is to ensure unilateral movement of blood into the aorta. There is also a pulmonary valve on the right side. Both formations are called “crescentic”; they have three valves. Any pathology, for example, calcification of the aortic valve leaflets, leads to disruption of blood movement. Acquired defects are usually associated with some disease. Therefore, people with so-called risk factors should undergo regular examinations: mainly an echocardiogram.
Structure
The aortic valve is a special type of septum that consists of connective tissue.
It is located on the border between the left ventricle and the aorta. Its main purpose is to prevent the process of regurgitation.
The aortic valve apparatus consists of the following components:
- the annulus fibrosus, which is the base of the valve. It is the fibrous ring that separates the left ventricle and the aorta;
- doors The AC consists of 3 leaflets, which have a semilunar shape and are attached to the fibrous ring. When they close together, the lumen of the aorta closes tightly. Each of the valves has the following parts: body, surface and base. In addition, the valves consist of several layers: aortic, ventricular and spongy. The upper part of the halves is covered with a layer of endothelium. On the aortic side, the valves are covered with elastin fibers;
- 3 sinuses of Valsava, which are also known as sinuses. They are located behind the semilunar recesses.
Aortic valves, like the other three types of valves, are formed during embryonic development from the mesenchymal type of tissue of embryonic primordia.
Mechanism of operation of the aortic valve
The aortic valve plays a significant role in blood circulation. The valves are compacted or shortened - this is one of the main pathologies. It causes hemodynamic disturbances. The function of this part of the organ is to ensure the movement of blood from the left atrium into the ventricle, preventing regurgitation. The valves open during atrial systole, at which time blood is directed through the aortic valve into the ventricle. Next, the flaps are closed to prevent backflow.
Congenital and acquired aortic valve defects
If problems arise with the aortic valve during the baby’s intrauterine development, it is difficult to notice. Usually the defect is noticed after birth, since the baby’s blood bypasses the valve, directly into the aorta through the open ductus arteriosus. Deviations in heart development can be noticed only through echocardiography, and only from 6 months.
The most common valve abnormality is the development of 2 leaflets instead of 3. This heart defect is called a bicuspid aortic valve. The anomaly is not in any danger to the child. But 2 sashes wear out faster. And by adulthood, maintenance therapy or surgery is sometimes needed. Less commonly, a defect such as a single-leaf valve occurs. Then the valve wears out even faster.
Another anomaly is congenital aortic valve stenosis. The semilunar valves either fuse together, or the valvular fibrous ring itself, to which they are attached, is excessively narrow. Then the pressure between the aorta and the ventricle differs. Over time, the stenosis intensifies. And interruptions in the work of the heart prevent the child from fully developing; it is difficult for him to exercise even in the school gym. Severe disruption of blood flow through the aorta may at some point lead to sudden death of the child.
Acquired defects are a consequence of smoking, excessive eating, sedentary and stressful lifestyle. Since everything in the body is connected, after 45–50 years all minor ailments usually develop into diseases. The aortic valve of the heart gradually wears out in old age, as it works constantly. Exploitation of your body's resources and lack of sleep wear out these important parts of the heart faster.
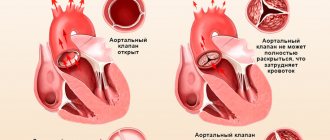
Aortic valve stenosis
Pathology implies a narrowing of the transition of the left ventricle into the aorta - the valve leaflets and surrounding tissues are affected. This disease, according to statistics, is more common in men. Hardening of the aortic walls and aortic valve leaflets is usually associated with rheumatic and degenerative lesions. Endocarditis and rheumatoid arthritis can also act as etiological factors. These diseases lead to fusion of the leaflets, as a result of which their mobility decreases, and the valve cannot fully open during left ventricular systole. In old age, the cause of the lesion is often atherosclerosis and calcification of the aortic valve cusps.
As a result of narrowing of the aortic opening, significant changes in hemodynamics occur. They are observed when the stenosis is severe - a decrease in the tract by more than 50%. This leads to the fact that the pressure gradient of the aortic valve changes - in the aorta the pressure remains normal, but in the left ventricle it increases. Increased impact on the wall of the left ventricle leads to the development of compensatory hypertrophy, that is, to its thickening. Subsequently, diastolic function is also impaired, which causes an increase in pressure in the left atrium. Hypertrophy leads to an increase in oxygen demand, however, the increased myocardial mass accounts for the same blood supply, and with concomitant pathologies, even a reduced one. This leads to the development of heart failure.
Hemodynamics
The structure of the aortic valve is quite simple, but despite this, the efficiency of the heart depends on the normal functioning of the aortic valve.
The closing and opening of the valve halves is passive and depends on the direction of blood flow, as well as on the blood pressure in the cavities of the heart. The valve operation phase can be divided into the following stages:
- Opening. This stage begins in the diastole phase. There are different pressure levels in the cavity of the aorta and left ventricle, which leads to the formation of a certain tension in the valves. As a result, the aortic root contracts and its diameter decreases. The left ventricle fills with blood. Approximately 25–35 ms before the moment of complete opening of the AC valves, its root expands by 12–15%. Further, the pressure in the left ventricle gradually increases, and the aortic root expands. At the end of this stage, the valves open completely, and the level of resistance to blood flow becomes minimal.
- Closing. This stage is also known as the Vortex theory. This is due to the fact that the process of pushing out blood takes the form of small vortices, which is associated with a slowdown in the speed of blood movement. Along the inside of the aortic wall, these vortices are directed to the root of the base, where the base of the left ventricle and the aortic root connect, heading towards the sinuses of Valsalva. At the end of this stage, the blood is completely pushed out, and the valve flaps close together. A distinctive feature of the stage is its duration, which does not exceed 30 ms.
- Rheology. The blood moves in a pulsating stream. The specific position of the AC valves helps to minimize the level of turbulence. This became possible due to the normalization of the diameter of the aortic root and the aorta itself.
All stages can be conditionally attributed to damper-type mechanisms, which lead to a decrease in the possibility of deformation, as well as the tension of the valve flaps.
Clinic
In the early stages, the affected aortic valve may not manifest itself in any way. Clinical changes occur when the hole narrows by 2/3 of normal. With severe physical activity, patients begin to experience pain localized behind the sternum. Pain syndrome in rare cases can be combined with loss of consciousness due to systemic vasodilation. The formation of pulmonary hypertension leads to shortness of breath, which at first worries only during exertion, but then appears at rest. The prolonged course of the disease causes chronic heart failure. The pathology requires surgical treatment, as there is a risk of deterioration and sudden cardiac death.
Causes and risk factors
The development of aortic valve disease pathology can be congenital or acquired.
Note. Congenital disorders occur during embryogenesis if a pregnant woman has suffered a long-term infectious disease or received a large dose of x-ray radiation.
It can also be embedded in the genetic code if relatives have such a pathology. Hereditary developmental anomalies manifest themselves as asymmetry of the valves (absence or different sizes). The most common type in children is the bicuspid valve. Does not require surgical intervention, if there are no clinical symptoms, the body decompensates for the deficiency on its own. A very rare phenomenon is a four-leaf valve type. The valve may be stretched or larger than the other two; there may be a hole in the semilunae.
Acquired aortic insufficiency is divided into:
- Functional - caused by the formation of an enlargement of the aorta or left ventricle.
- Organic pathology - arose due to damage to the valve tissue.
An acquired defect can be caused by the following factors:
- As a consequence of an infectious disease (for example, pneumonia, sepsis, syphilis). When, in severe cases, pathogenic microflora affects the endocardial tissue, forming colonies on them (endocarditis). Subsequently, it becomes covered with protein, overgrows and prevents complete closure of the valve.
- Adverse reaction after autoimmune inflammatory diseases (rheumatism, lupus erythematosus). Which also causes thickening of the valves and their wrinkling, due to the proliferation of connective tissue.
- Hypertension.
- Left ventricular aneurysm.
- Enlarged aortic valve.
- Aortic dissection as a complication of atherosclerosis of the heart vessels and a sharp increase in pressure. The condition is dangerous and can result in death for the patient.
- Atherosclerosis.
- A strong blow to the heart area.
- Elderly age. The elasticity of the walls of blood vessels wears out over the years and is more often damaged.
- The formation of a layer of calcium deposits on the walls of the aorta (the cause of pathology of hormones and vital organs, as well as tumors).
- Systemic connective tissue disease (Marfan syndrome).
- Malignant neoplasms.
Diagnostics
On examination, patients exhibit characteristic pallor associated with decreased cardiac output. The pulse in the radial arteries is difficult to palpate - it is rare and weak. On auscultation, a weakening of the 2nd tone or its splitting is observed. The ECG is not informative enough - signs of hypertrophy are determined only with severe stenosis. The most revealing is echocardiography, which allows one to evaluate the aortic valve. The valves are compacted and thickened, the opening is narrowed - these are the main diagnostic criteria that this study helps to detect. The degree of stenosis and pressure gradient can be effectively determined by catheterization of cavities.
Treatment
With mild and moderate degrees of stenosis, only lifestyle correction is required - avoidance of excessive physical exertion, treatment of concomitant pathologies. For increased contractions, adrenergic blockers are prescribed, and for heart failure, diuretics and cardiac glycosides are effective. Severe thickening of the aortic walls and aortic valve leaflets requires surgical treatment. Typically, prosthetics or balloon dilatation are performed.
Aortic valve disease: features of its course and treatment
According to statistics, disorders of the cardiovascular system have become increasingly observed in people over 30 years of age. There are many reasons that provoke pathologies. If some diseases are treatable and, by removing provoking factors, one can achieve normalization of health, then others accompany the patient throughout his life and can significantly shorten his life.
Aortic valve disease is a serious pathology. More often requires surgical intervention. It can be congenital or acquired. Appears as a result of narrowing of the aortic mouth or incomplete closure of its valve.
Causes and symptoms
There are no exact statistics on the prevalence of the disease by age group and gender, but cardiologists note that it is detected several times more often in women than in men. The peak number of patients is observed among people of older retirement age. The main reasons may be:
- leaflet calcification;
- progression of rheumatism;
- idiopathic dilatation of the aorta;
- arterial hypertension and endocarditis;
- aneurysm;
- congenital defect of the aortic valve.
Chest trauma, arthritis, syphilis and some pathologies that develop in a person over a long period of time can also give impetus to the appearance or progression of disruption of the normal functioning of the organ.
8
24/7
Degrees
The risk to the patient's health and the need for surgery depends on the degree of aortic regurgitation.
| Stage | Amount of thrown blood, % | Prosthetics |
| First, full compensation | no more than 15 | Not required |
| Second, hidden CH | from 15 to 30 | Required under certain conditions |
| Third, relative coronary insufficiency | up to 50 | |
| Fourth, severe left ventricular failure | more than 50 | |
| The issue is resolved individually | Not required due to its uselessness. |
Depending on the degree, the valves are deformed and the quantitative volume of blood entering the heart through the aorta changes. The initial, first stage of the disease is virtually impossible to determine. The patient’s symptoms are completely absent or feel like side effects of other diseases. This occurs because the heart adjusts to the change in volume and compensates for it.
Symptoms
As the pathology develops, the organ ceases to cope with its functions, and symptoms characteristic of aortic valve disease appear:
- tinnitus and dizziness when moving or changing position;
- increased heartbeat, pronounced pulsation in the blood vessels;
- shortness of breath, fatigue, fainting and pre-fainting states, nausea;
- a pressing feeling of heaviness in the right hypochondrium, as well as swelling of the lower extremities;
- coughing attacks when lying down, standing, feeling of constant weakness.
Due to a lack of oxygen, a person’s complexion becomes pale gray, a bluish tint to the lips is observed, and typical circles appear under the eyes. Also, when examining a patient, the cardiologist examines the presence and severity of symptoms:
- the difference between the upper and lower blood pressure readings;
- pulsation on the carotid arteries, uvula and tonsils;
- reaction of the pupils to heart contractions, heart murmurs;
- changes in the size of the organ, protrusion in the chest area.
Diagnostics
Accurate diagnosis of the disease can only be made on the basis of objective data, a complete cardiac examination, biochemical blood test and a number of other tests.
Based on the presence of clinical symptoms, the severity of the defect, and the severity of aortic insufficiency, a decision about surgery is made. In elderly patients, due to the low contractility of the organ, the functional impairment is almost invisible. The severity of the pathology can be determined after studying the area of the hole in relation to the blood flow. Arterial insufficiency is determined by the indicator of reverse blood flow.
By listening, a cardiologist can determine the onset of development of bicuspid aortic valve disease:
- with stenosis, a systolic murmur is characteristic with a weakening of the 2nd tone in the aorta;
- Insufficiency is indicated by a murmur during diastole.
It is necessary to study the functioning of the heart by:
- ECG;
- X-ray examination;
- MRI to exclude coronary insufficiency and other pathologies.
However, the basis for choosing treatment is echocardiography.
When diagnosing, an accurate description of the patient’s feelings is of great importance, so before the appointment, you can write down all the complaints and let the doctor read them.
8
24/7
Treatment at different stages
Depending on the cause, extent, stage of aortic valve disease and other factors, different treatment methods may be used. The patient must be regularly observed by a specialist and undergo the examinations prescribed by him. In the absence of obvious symptoms:
- mild defect – once every 3 years;
- moderate form – once every 24 months;
- severe degree - annually, sometimes more often.
The following medications are prescribed:
- rheumatic nature of the disease - antibiotics;
- arterial hypertension - to normalize blood pressure.
Surgical intervention is not required, only constant monitoring by the attending physician is required.
If clinical complaints appear, to alleviate the patient’s condition in the preoperative period or if surgery is impossible, the following is prescribed:
- inhibitors, diuretics, nitrates;
- vasodilators and beta blockers;
- drugs that improve blood circulation.
A timely operation can help completely get rid of aortic valve disease. When blood reflux in an amount not exceeding 30% and slight deformation of the valves, intra-aortic balloon counterpulsation is recommended. In case of severe structural changes that allow more than 30% blood flow, implantation is required.
Surgery
In a person with heart disease, the bicuspid aortic valve requires replacement or replacement in several cases.
| Diagnosis | Cause |
| Severe stenosis | Complaints of severe pain and worsening condition. |
| Associated ischemia requiring coronary artery bypass grafting. | |
| Additional pathological changes in the organ requiring surgical intervention. | |
| The ejection fraction with cardiac contractility is below 50%. | |
| Severe valvular insufficiency | Clinical manifestations of the disease. |
| Surgery is required for other diseases of the organ. | |
| A decrease in ejection fraction in the absence of complaints from the patient. | |
| Too much enlargement of the ventricles. |
Surgical intervention is mainly performed after 30-35 years, but with the accelerated development of the disease it can take place at any time. The number of contraindications to prosthetics is minimal. They are:
- decompensated diabetes;
- oncological diseases;
- post-stroke condition;
- exhaustion and anemia.
For each patient, his condition is predicted at the time of the operation and during the rehabilitation period. Depending on this, a conclusion is given about the possibility of returning to normal life.
Forecast
The construction of treatment plans for the disease and the choice of methods occurs after diagnosis and identification of the severity of the aortic valve defect.
Mild hypertrophy with strong obstruction of blood flow leads to a decrease in the number of heart contractions and, accordingly, gradually reduces the therapeutic effect of surgery.
The process of hypertrophy allows, at a certain stage of the disease, to stabilize the functioning of the heart, but at the same time it can cause the development of angina pectoris and increase the likelihood of a heart attack.
If aortic heart valve disease developed asymptomatically, and then its rapid progression began, then the subsequent life expectancy of a person is no more than 3 years.
Risk factors and disease prevention
Aortic valve defects can be divided into 2 groups.
| View | Development time | Cause |
| Congenital | During intrauterine development of the fetus at 2-8 weeks of formation. | Genetic predisposition. Radiation exposure, rubella and other viral infections. Smoking, alcohol and drug addiction of the mother. |
| The defect becomes noticeable as the child grows. | The presence of a muscle cushion above the AC. The valve design is two- or single-leaf rather than three-leaf. Under the valve there is a membrane with a hole. | |
| Acquired | Any age | Infectious diseases that lead to microorganisms entering the organ. The subsequent appearance of a colony of connective tissue at the site of localization leads to deformation of the valves. |
| Autoimmune diseases become an impetus for the fusion of pouches and changes in the aortic mouth. | ||
| Age-related disorders, mainly calcification of the edges of the valves and the growth of fatty plaques, lead to closure of the lumen. |
There are no preventive measures that guarantee complete protection against the disease, but the following help reduce the risk:
- timely treatment of streptococcal infections;
- if you have rheumatism, constant monitoring by a specialist;
- taking certain groups of antibiotics and other drugs prescribed by a cardiologist;
- complete exclusion of alcohol, drugs and smoking;
- engaging in acceptable forms of exercise.
Aortic valve disease needs to be treated using scientific methods of therapy. Traditional methods do not have the desired effect and can lead to missed deadlines when the disease can be cured. Therefore, in case of any deviations, medical attention is needed.
8
24/7
Aortic valve insufficiency
This name was given to a pathology characterized by non-closure of the valves. This phenomenon leads to the backflow of blood into the left ventricle, which occurs during diastole. The defect is usually a complication of infective endocarditis and rheumatic lesions. Less commonly, it is caused by syphilis, aortic aneurysm, aortitis, arterial hypertension, Marfan syndrome, and systemic lupus erythematosus.
The aortic valve plays an important role in blood circulation. Incomplete closure of its valves causes regurgitation, that is, the backflow of blood into the left ventricle. As a result, there is an excessive amount of blood in its cavity, which leads to overload and stretching. Systolic function is impaired, and increased pressure leads to the development of hypertrophy. The pressure in the pulmonary circle increases retrogradely - pulmonary hypertension is formed.
Possible pathologies
The aortic valve, like others, may have some pathologies. Among the most common are the following:
- Aortic insufficiency. As a rule, this type of pathology develops predominantly in men. Its essence lies in the partial closure of the valve leaflets, which leads to the return of blood to the left ventricle and its increase in size. Such processes after some time lead to rapid wear of the valve, as well as the development of hemodynamic disorders of the heart.
When assessing the degree of aortic valve insufficiency, the amount of blood that returns is taken into account. There are 4 degrees of deficiency:
- 1st degree – the level of regurgitation does not exceed 15%;
- 2nd degree – returns within 15–30% of the pumped blood;
- Grade 3 – approximately 50% of the blood returns back to the left ventricle;
- Grade 4 – the level of regurgitation exceeds 50%.
The aortic valve has the same level of regurgitation as the degree of deformation of its leaflets.
This pathology can be either congenital or acquired. Congenital AA deficiency develops during the period of intrauterine development of the fetus. VNAK manifests itself as asymmetry of the aortic valve leaflets (absence of the third leaflet, violation of the size of one of the leaflets, etc.).
If we talk about acquired deficiency, it may be caused by the fact that the patient has suffered any infectious or autoimmune diseases. In addition to the above reasons for the development of aortic valve insufficiency, one can also name high blood pressure, atherosclerosis of the aorta, and the formation of a calcium layer on the walls of the aorta.
Deficiency is manifested by the following symptoms:
- pale skin;
- strong pulsation of the arteries;
- tachycardia;
- development of the cardiac hump, increase in heart volume, etc.
In the first stages of pathology development, the patient may not experience any symptoms.
- AC stenosis. According to statistics, this type of defect, which affects the aortic valve, occurs in every ninth patient whose age exceeds 65 years. The essence of stenosis is that the lumen of the aorta narrows, causing disruption of the circulatory process.
With aortic valve stenosis, blood does not have time to pump from the left ventricle to the artery. As a result of this, the heart increases in size, and the pressure in all its parts increases.
With normal functioning of the heart and all its parts, the total area of the opening between the leaflets of the aortic valve is approximately 2.5 cm2. When classifying the degree of stenosis, the area of the orifice between the leaflets is assessed:
- light – 1.5 cm2;
- moderate – in the range of 1.5 – 1 cm2;
- heavy – 1 cm2 or less.
The intensity of symptoms of stenosis is directly dependent on the degree of complexity of the pathology.
CA stenosis can develop during the period of intrauterine development of the child. In the first years of a baby’s life, the symptoms of stenosis manifest themselves weakly or not at all. But with age, the intensity gradually increases.
PSAC can develop as a result of the patient suffering from infectious or autoimmune diseases. In addition, age-related changes (atherosclerosis, sedimentation of calcium salts, plaque formation, etc.) are also factors that provoke stenosis of the aortic heart valve.
Among the most pronounced symptoms are the following:
- fast fatiguability;
- pallor of the skin;
- bradycardia;
- listening to a fuzzy sound that occurs when the aortic valve flaps close;
- cough;
- swelling of the limbs, etc.
Since the aortic valve is of decisive importance in the process of hemodynamics, it is important to determine the presence of pathology as early as possible.
Clinic
As with stenosis, the pathology makes itself felt only with a pronounced degree of insufficiency. Shortness of breath occurs during physical exertion and is associated with pulmonary hypertension. Pain occurs only in 20% of cases. In this case, auscultatory and external manifestations of pathology are expressed:
- Pulsation of the carotid arteries.
- Durosier's sign or the appearance of a systolic murmur in the femoral artery. It occurs when it is pinched closer to the listening position.
- Quincke's symptom is a change in the color of the lips and nails in accordance with the pulsation of arterioles.
- Double Traube sounds, loud, “cannonball”, which arise over the femoral artery.
- De Musset's sign, manifested by shaking of the head.
- Diastolic murmur after the 2nd tone, occurring during auscultation of the heart, as well as weakening of the 1st tone.
Danger and complications
Untimely medical care can prolong the pathological process. As a result, serious complications arise. First of all there are:
- various failures of the cardiac system;
- extrasystole of the atria or ventricle;
- atrial fibrillation or ventricular fibrillation.
Attention! Thromboembolism may develop when the resulting blood clots block the lumen of the vessels of the lungs, brain or heart. This leads to a serious condition - stroke or heart attack.
Symptoms become apparent at stage 2 insufficiency, when a third of the blood flow returns from the aorta to the left ventricle. At the same time, a person feels and hears:
- increased heart rate (tachycardia);
- pain in the sternum (angina);
- shortness of breath during light physical exertion;
- headache and dizziness with a sudden change in body location.
Fainting is possible. With further progression of the disease, swelling and heaviness appear under the ribs on the right side (the phenomenon of stagnation of blood in the liver).
Characterized by pronounced pallor of the skin and protrusion of the chest, due to the expansion of the cavity of the heart chambers. The pulsation of blood through the cervical artery is visible. Systolic pressure is too high, and diastolic pressure is less than normal.
Can be classified according to developmental stages. But this is an approximate plan; the nature of the course of the disease is individual for each person:
- Stage 1 – asymptomatic, slight enlargement of the heart walls and moderate enlargement of the left ventricular cavity;
- Stage 2 – latent decompensation without obvious symptoms;
- Stage 3 – coronary insufficiency is formed, part of the blood; returns back to the ventricle. there is pain in the heart area;
- Stage 4 - the ventricle contracts weaker due to overfilling with excess blood volume, shortness of breath, pulmonary edema, heart failure, and lack of air appear;
- Stage 5 – critical, close to death, heart contractions are less, blood stagnation forms in the organs.
Treatment
Severe insufficiency with a large volume of regurgitation and intense clinical manifestations requires surgical treatment. The optimal solution is artificial aortic valves, which allow the heart to function again. If necessary, symptomatic drug therapy is prescribed.
Aortic valve stenosis and insufficiency are the most common heart defects, which, as a rule, are the result of some local or systemic disease. The pathology progresses quite slowly, which allows it to be diagnosed in time. Modern treatment methods help restore the function of the valve and improve the patient’s condition.
Causes of cardiac fibrosis
the mitral valve is most commonly affected . In second place in frequency is the aortic valve . Infection, inflammation, calcium deposition, congenital features, etc. can lead to the replacement of normal valve tissue with fibrous tissue.
Most often, fibrosis of the heart valves is caused by the following conditions and diseases:
- Age-related changes in valve leaflets. Thus, in patients over 60 years of age, due to age-related changes in collagen and elastic fibers, the number of vessels feeding the latter decreases. As a result, the fibers in the heart valves acquire a coarse fibrous structure, which affects the function of the valves.
- Previous acute rheumatic fever, especially with repeated attacks (previously called rheumatism). When the valve is affected by bacteria (usually streptococci, hemolytic, viridans, etc.), infective endocarditis develops with an inflammatory process on the valves. When the valve is influenced by antibodies to this group of bacteria (usually GABHS - group A beta-hemolytic streptococcus), an inflammatory process on the valve is also formed, but of an autoimmune nature. People most often affected by rheumatism are those who often suffer from sore throats, tonsillitis, caries, chronic diseases of the ENT organs and those who have had scarlet fever. Infective endocarditis also develops in this category of patients, but it is more common in injection drug users.
rheumatic vegetations on the mitral valve
- Congenital features, for example, connective tissue dysplasia, Marfan syndrome, mitral valve prolapse. With these anomalies, initially the connective tissue in other organs differs from normal, and often leads to loss of function by the organ. For example, with Marfan syndrome, there is a disturbance in the anatomical and functional structure of other internal organs, including the heart. Mitral valve prolapse causes the leaflets to “sag” into the lumen of the heart chamber, and if linear fibrosis develops on such leaflets, the patient is likely to experience disturbances in intracardiac hemodynamics.
- Atherosclerosis of the aorta. The deposition of cholesterol plaques, in addition to harm to the coronary arteries and, in connection with this, a high risk of myocardial infarction, poses another danger. This is a lesion of the aortic root with subsequent deposition of calcium in the plaque. In addition to the wall of the aorta itself, its valves are affected, and aortic fibrosis develops.
- Previous myocardial infarction and acute inflammation of the heart muscle (myocarditis). Necrosis (cell death) or inflammation near the valve ring leads to the proliferation of sclerotic tissue in place of dead cardiomyocytes - a “scar on the heart” is formed. If in place of this tissue there were tiny vessels feeding the valve leaflets, naturally, they can no longer perform their function. Due to chronic hypoxia, fibrous tissue forms directly in the valve leaflets.