Pulmonary artery stenosis (PAS) in newborns is a narrowing of the lumen of the outflow tract of the right ventricle. Pathological changes affect the pulmonary valve or part of the vessel in the valve area.
According to statistics, various forms of isolated PLA account for about 10% of cases of congenital heart pathologies. Most often, valvular stenosis is detected, often aggravated by concomitant heart defects.
Causes
The etiology of congenital heart defects has not been fully elucidated. The causes of the development of congenital heart pathologies, including SPA, may be :
- Burdened heredity. The risk of having a child with congenital SLA is higher if any of the parents, immediate family members, or other children in the family have been diagnosed with a heart defect.
- The presence of systemic or metabolic diseases in the mother.
- Infectious diseases suffered by the mother in the early stages of pregnancy, in particular viral ones.
- Taking certain medications that have teratogenic side effects.
- First birth at the age of over 38 years.
- Multiple pregnancy.
- Extracardiac fetal anomalies.
- Chromosomal diseases.
- Disorders of fetoplacental blood flow.
- Fetal heart rhythm disturbances, including episodic ones.
Risk factors include the presence of other hereditary diseases.
Diagnosis and treatment of pulmonary artery stenosis in children
The narrowing is detected after an ECG. This examination determines the high and moderate degree of narrowing of the artery. With minor pathology, an electrocardiogram will not reveal any abnormalities.
To detect a low degree of stenosis, echocardiography is prescribed.
Treatment is required if the lumen of the artery is so small that it impedes the blood circulation process. The situation is corrected surgically. The operation can be performed as early as the 2nd day of a newborn’s life, if the narrowing is severe and poses a danger to the child’s life. During surgery, excess vessel tissue is removed, thereby clearing the way for blood flow.
If the pathology does not threaten the baby’s life, then it is better to postpone the operation until a later date, when he is at least 5 years old. All this time, the child must be registered with a cardiologist and undergo regular examinations.
Congenital heart defects are anomalies in the structure of large vessels and the heart that form between 2 and 8 weeks of pregnancy. According to statistics, one child out of a thousand is diagnosed with this pathology, and in one or two of them this diagnosis can be fatal. Thanks to the achievements of modern medicine, detection of heart defects in newborns has become possible even at the stage of perinatal development or immediately after birth (in the maternity hospital), but in some cases (in 25% of children with heart defects), these pathologies remain unrecognized due to the peculiarities of the child’s physiology or diagnostic difficulties. In the CIS countries and Europe they are present in 0.8-1% of children. It is extremely important for parents to remember this fact and carefully monitor the child’s condition: this tactic helps to identify the presence of a defect in the early stages and carry out its timely treatment.
In 90% of cases, congenital heart disease in a newborn develops due to exposure to unfavorable environmental factors. The reasons for the development of this pathology include:
- genetic factor;
- intrauterine infection;
- age of parents (mother over 35 years old, father over 50 years old);
- environmental factor (radiation, mutagenic substances, soil and water pollution);
- toxic effects (heavy metals, alcohol, acids and alcohols, contact with paints and varnishes);
- taking certain medications (antibiotics, barbiturates, narcotic analgesics, hormonal contraceptives, lithium preparations, quinine, papaverine, etc.);
- maternal diseases (severe toxicosis during pregnancy, diabetes mellitus, metabolic disorders, rubella, etc.).
Children at risk for developing congenital heart defects include:
- with genetic diseases and Down syndrome;
- premature;
- with other developmental defects (i.e., with disturbances in the functioning and structure of other organs).
Classification
Depending on the location of the narrowing of the vessel, supravalvular, valvular, and subvalvular pulmonary artery stenosis in a newborn is distinguished. In cases of a combination of two types of PAS or pulmonary artery stenosis with other heart pathologies, the form of the disease is defined as combined.
The valvular form of the pathology is diagnosed in approximately 90% of patients . The pulmonary valve in patients with valvular pathology may have an abnormal structure (unicuspid or bicuspid valves). A characteristic anatomical feature of the pathology is post-stenotic dilatation of the arterial trunk.
A characteristic anatomical feature of subvalvular stenosis is a funnel-shaped narrowing of the vessel or an abnormal location of the muscle bundle, which makes it difficult for the ejection of blood into the pulmonary circulation. Isolated subvalvular pulmonary artery stenosis is often accompanied by a ventricular septal defect in a newborn.
Supravalvular stenosis often occurs in association with Williams and Noman syndromes. This pathology occurs in the form of multiple peripheral narrowings, membranes, localized narrowing or diffuse hypoplasia.
The dimensions of the right ventricle and tricuspid valve in patients with SLA are usually within normal limits. The narrowing of the lumen of the pulmonary artery impedes blood flow, as a result of which the pressure gradient between the right ventricle and the pulmonary circulation increases . The pathological structure of the outflow tract is the cause of systolic overload of the myocardium.
Systolic overload of the right ventricle over time leads to myocardial hypertrophy and right ventricular failure.
Manifestations of SLA depend on the severity of the narrowing . With minimally expressed pathology, accompanied by a pressure gradient of up to 40 mm Hg. Art., the disease can be asymptomatic. The average degree of stenosis is determined by a pressure difference of 40-70 mm Hg. Art., accompanied by increased fatigue and shortness of breath during physical exertion.
With a pressure gradient above 70 mm Hg. Art. talk about critical stenosis. Against the background of a critical form of the disease, newborns exhibit symptoms of heart failure, as well as bluish skin caused by right-to-left shunting of blood through the oval window.
What manifestations are characteristic of Eisenmenger syndrome and what can it develop from? All details are in a separate article. Find out in what cases aortic valve insufficiency may occur with stenosis from this material.
Read about the features of the congenital defect - Ebstein's anomaly - in another publication.
Development mechanism
The course of congenital heart disease in a newborn is divided into three phases:
- Phase I (adaptation): in the child’s body there is a process of adaptation and compensation to hemodynamic disturbances caused by heart disease; in case of severe circulatory disorders, significant hyperfunction of the heart muscle is observed, turning into decompensation;
- Phase II (compensation): temporary compensation occurs, which is characterized by improvements in the motor functions and physical condition of the child;
- Phase III (terminal): develops with the exhaustion of compensatory reserves of the myocardium and the development of degenerative, sclerotic and dystrophic changes in the structure of the heart and parenchymal organs.
During the compensation phase, the child develops capillary-trophic insufficiency syndrome, which gradually leads to the development of metabolic disorders, as well as sclerotic, atrophic and dystrophic changes in the internal organs.
The main signs of congenital heart disease may include the following symptoms:
- cyanosis or pallor of the outer skin (usually in the area of the nasolabial triangle, on the fingers and toes), which is especially pronounced during breastfeeding, crying and straining;
- lethargy or restlessness when attaching to the breast;
- slow weight gain;
- frequent regurgitation during breastfeeding;
- causeless screaming;
- attacks of shortness of breath (sometimes combined with cyanosis) or constantly rapid and difficult breathing;
- causeless tachycardia or bradycardia;
- sweating;
- swelling of the limbs;
- bulging in the area of the heart.
If such signs are detected, the child’s parents should immediately consult a doctor to have the child examined. During the examination, the pediatrician can detect heart murmurs and recommend further treatment by a cardiologist.
Symptoms
A mild form of congenital SLA may not appear for long . An indirect indication of the probable presence of pathologies of the pulmonary circulation in infants may be a lag in physical development, frequent colds with complications such as pneumonia.
The most characteristic symptom of moderate and critical stenosis is cyanotic coloration of the nasolabial triangle, lips and nail holes . The critical stage of the pathology is accompanied by symptoms of progressive right ventricular heart failure. Shortness of breath develops during physical exertion.
Percussion reveals a shift of the borders of the heart to the right . When listening to heart sounds, a characteristic rough noise is heard during systole, the intensity of which is proportional to the degree of narrowing of the vessel. The second tone above the pulmonary artery is greatly weakened or absent. Above the area of projection of the valves, the second tone is bifurcated, and ejection sounds can be heard.
Severe forms of SLA appear in the first days and hours of life. Newborns with symptoms of heart disease are examined by a cardiologist, or in severe cases by a cardiac surgeon.
Degrees
At different stages of aortic narrowing in children, various symptoms are present and treatment methods also vary. There are five stages in the development of stenosis:
- Full compensation. In the first degree of the disease, the aortic passage is narrowed slightly and the left ventricle fully copes with its functions.
- Hidden heart failure. During the second stage, children already experience shortness of breath, dizziness, and the child gets tired faster. The doctor prescribes diagnostics and possibly surgery.
- Relative coronary insufficiency. Here dizziness develops into fainting, shortness of breath intensifies, and angina pectoris appears. At this stage it is necessary to perform surgery.
- Severe heart failure. The fourth degree is characterized by nocturnal asthma attacks, even at rest there is shortness of breath. Some operations are already prohibited, so only cardiac surgery is performed.
- Terminal stage during which the disease actively progresses. Surgical intervention is prohibited, so short-term improvements are achieved through medication.
If you do not consult a specialist in time and ignore treatment, then serious complications cannot be avoided. Complications of aortic stenosis are represented by acute and chronic forms of cardiac dysfunction:
- Ischemia;
- Arrhythmia;
- Gastrointestinal bleeding;
- Myocardial infarction;
- AV block;
- Sudden death.
Diagnostics
To confirm the preliminary diagnosis made according to a general examination, an instrumental examination is required . Typically used in practice:
- X-ray examination;
- ECG;
- Echocardiography;
- Doppler.
The x-ray shows a narrowing of the pulmonary artery orifice and expanded borders of the heart . The image of the lungs is often poor.
With minor stenosis, the patient’s electrocardiogram may have a normal appearance;
with more severe forms of pathology, characteristic changes appear , indicating:
- Right ventricular hypertrophy;
- Hypertrophy of the atrial septum.
Some newborn patients with critical stenosis show signs of right ventricular hypertrophy on the ECG. This effect is explained by its relatively large size against the background of a hypoplastic left ventricle.
Echocardiographic examination makes it possible to identify abnormal expansion of the pulmonary artery trunk in the area located directly behind the site of narrowing, narrow arterial branches, pathological structure of the valve, hypertrophic changes in the myocardium of the right ventricle and some other pathological features of the anatomy of the heart.
An echocardiogram also reveals changes in the pressure gradient between the right ventricle and the pulmonary circulation, corresponding to the clinical picture of moderate and critical pathology.
In some cases, Doppler ultrasound is used to assess the difference in pressure in the ventricle and arterial bed.
If SPA is suspected, differential diagnosis with other heart defects is required, in particular, ventricular septal defect, triad and tetralogy of Fallot in children, etc.
Causes and treatments for left atrium enlargement
Hypertrophy or enlargement of the left atrium only sounds like a disease, but in fact, it is an alarming signal about problems in the functioning of the cardiovascular system. An increase in cells in the heart tissue most often occurs on the left side of the heart muscle. To avoid the dangerous development of the disease, you need to consult a doctor in a timely manner, but not everyone knows how to determine the pathology, what it means, and for what reason it appears, although they have probably heard about this disease.
Causes
Why the left atrium enlarges is still not known exactly, but there are many reasons for this pathology. Although heart disease is more common in older people, trends are changing every year, and diseases are becoming younger.
The most common causes of hypertrophy include heredity, high blood pressure and excess weight. The problem of obesity is not new in the modern world, so atrial enlargement is no longer a rare symptom, and such a sign is often found in young people and even children.
If we look at the reasons better, we can understand why such a pathology occurs and how to deal with it.
Hypertension
Most often, hypertrophy occurs in hypertensive patients; high blood pressure increases the load on the heart and impairs blood flow. In the chronic form, even with treatment, blood pressure is far from normal, and constant stress on the muscle leads to swelling and hypertrophy.
Mitral valve stenosis
Enlargement of the left atrium occurs as a result of a narrowing of the opening that regulates blood flow between the left side and the ventricle. At the same time, the load on the heart muscle increases, blood is retained in the left atrium more than expected, and it accordingly stretches and also increases in size.
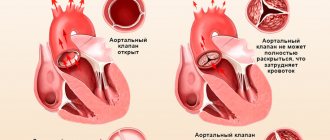
Aortic valve stenosis
Despite the distance of this section from the atrium, with pathology in the areas between the ventricle and the aorta, blood circulation is disrupted, and known disorders of the left atrium occur.
Mitral and aortic valve insufficiency
Not only the narrowing leads to pathology, the blood supply is affected by the operation of these valves. If one of the valves does not close tightly or the frequency of contractions does not correspond to the rhythm, then the outflow of blood occurs in the opposite direction, which inevitably leads to an inflammatory process in the cavity of the heart and the left atrium. As a result of these disorders and the inflammatory process, hypertrophy develops.
Myocarditis and other inflammatory processes
Myocardial inflammation has a negative effect on the contractile function of the heart muscle. Diseases of the respiratory system can also disrupt the functioning of the left atrium; lack of oxygen and heart rhythm disturbances lead to hypertrophic changes. The process is long, so a common cold cannot lead to such consequences. The cause can only be advanced and chronic diseases that systematically disrupt the functioning of the heart.
Congenital pathology
Left atrium hypertrophy is caused by a gene mutation of chromosomes, which results in hypertrophic cardiomyopathy. Pathological compaction of the walls of the ventricle leads to a load on the lower parts of the heart, and increased blood flow enlarges the cavities of the organ.
Nervous system disorders
Not the least of the causes of atrium enlargement are stress and nervous tension. They are the culprits of high blood pressure, which leads to hypertrophic changes.
Symptoms
The process of changes in the left atrium occurs slowly, and symptoms do not appear immediately. It all starts with chest pain, which is not perceived as a serious sign of impairment. Over time, fatigue appears, first during physical activity, later at rest. Feeling worsens as the disease progresses.
The symptoms of enlargement largely depend on the causes of the development of the pathology. If the problem arose due to mitral valve stenosis, in addition to pain, severe swelling of the lower extremities and severe cough with hemoptysis are observed.
With mitral or aortic valve insufficiency, a person complains of the following symptoms:
- cardiopalmus;
- heart rhythm disturbances;
- dyspnea;
- general weakness;
- excessive fatigue;
- pain during exercise.
If there are several reasons, then the symptoms appear gradually in different order. External factors have a great influence on symptoms. Lifestyle, bad habits, heavy physical work and individual characteristics can change symptoms and manifest themselves in different ways.
Diagnostics
Slow damage and enlargement of the left atrium does not allow pathology to be diagnosed based on symptoms, but there are methods by which hypertrophy can be detected at the initial stage.
The first method for diagnosing disturbances in the functioning of the heart muscle and enlargement of the atrium includes auscultation. It does not require special equipment, just a stethoscope and the professionalism of a doctor. This study is based on listening and evaluating the sounds of the heart. The appearance of murmurs and short sharp sounds indicates valve pathology, which allows for atrial hypertrophy.
The performance of the valves can be assessed and abnormalities in their operation can be detected using ultrasound diagnostics. Echocardiography and ultrasound allow you to examine the tissue of the heart muscle, assess the size and thickness of the walls of the heart. Monitoring blood flow in parts of the heart muscle makes it possible to detect pathological changes even before hypertrophy is visible.
X-ray examination is less informative, but is an indispensable diagnostic method for congenital disorders. In addition to the condition of the heart muscle, the X-ray also evaluates the potential of the lungs and their function.
Since contraction disturbances are observed quite often during hypertrophy, an electrocardiogram is one of the methods for examining the heart. One of the methods may not be a way to accurately diagnose. To establish the causes and degree of neglect of the disease, a full range of examinations are carried out.
Treatment methods
Since atrium enlargement is not a separate disease, but a symptom, treatment is based on eliminating the causes that led to hypertrophy and treating the underlying disease. The effectiveness of treatment depends on identifying the exact causes of atrial hypertrophy. Mistakes here are unacceptable and can be fraught with serious consequences.
If the enlargement of the left atrium occurs due to an infectious lesion, antiviral or antibacterial therapy is prescribed. Maintenance therapy is prescribed to support the heart and restore the normal size of the atrium.
In case of hypertension and high blood pressure, to eliminate unpleasant consequences, an important part of therapy remains normalizing the pressure and keeping it within normal limits. Antihypertensive drugs are used for treatment.
If the problem lies in the insufficiency or malfunction of the valves, restorative therapy is carried out, but if time is lost and the stenosis is irreversible, surgical intervention is performed to restore the functionality of the valve and eliminate pathological processes. If during an examination or during surgery it is discovered that the valve cannot be restored, it is replaced with an artificial one.
In addition to drug treatment and surgical intervention, for a speedy recovery, it is recommended to reconsider your lifestyle, follow a diet for some time and give up bad habits, first for the duration of treatment, and then forever.
Prognosis for recovery
How effective the treatment will be depends on how quickly the pathology was identified, the state of the cardiovascular system and the body as a whole, and how severely the heart and left atrium were affected. Timely diagnosis and correct treatment allow you to get rid of a dangerous symptom and return to your normal life without fear for your health.
It is important to remember that the reasons that led to hypertrophy could cause damage not only to the atrium, but also to the vessels, aorta or ventricle. These points must be taken into account during examination and therapy. Left atrial hypertrophy is a dangerous symptom, which, in addition to serious consequences, can also cause life-threatening complications. A missed moment, ineffective treatment, or incorrectly identified causes can lead to disability or death.
But timely diagnosis and proper treatment, even for congenital defects, gives a good prognosis for recovery. After drug treatment and surgical intervention, a person can return to his normal life without limiting himself due to illness.
The prognosis for recovery is favorable; the main thing is not to delay seeing a doctor. When the first signs appear, you should immediately go to the clinic. Mild malaise and barely noticeable pain cannot be an accident; this is the body signaling the occurrence of problems in the functioning of the cardiovascular system. The sooner they are identified, the faster the recovery will be.
Each organism is individual and the approach to treatment should also be based on the results of tests and studies, as well as on the general condition of the patient. It is also important to take into account that the symptoms of pathology are different for everyone and there are also many reasons for the occurrence of hypertrophy.
Source: porok.lechenie-gipertoniya.ru
Manifestations will largely be related to the degree of narrowing of the opening and the severity of stenosis. In the initial stages of the defect, children may feel quite normal, and parents do not notice any deviations in health and development without consulting a doctor. If the diameter of the hole in the aorta becomes less than 0.5 cm, then unpleasant symptoms will begin to appear in the form of pale skin, and there will be a blue discoloration near the nose and around the lips, on the fingertips and wrists. Children exhibit shortness of breath, more than 30 breaths per minute, as well as sudden weight loss, decreased sucking force and strong, constant regurgitation.
In children over three years of age, the defect manifests itself similarly to adults in the form of shortness of breath with increased fatigue after normal exercise; physical exercise can lead to fainting. Stitching pain and compression in the chest area, dizziness, a feeling of the “heart jumping out of the chest,” sudden attacks of anxiety, and moodiness may occur. Coarse heart murmurs audible with a stethoscope, vibration in the chest and arrhythmias are detected.
Depending on the degree to which the narrowing of the aortic valve has reached, various symptoms may occur, and the methods of treating the defect differ:
- With full compensation of the narrowing, the narrowing of the aortic passage is insignificant, the heart, and especially the left ventricle, can fully cope with the loads.
- At the second stage, with the formation of hidden heart failure, children experience periodic shortness of breath, attacks of dizziness and frequent fatigue. With the development of relative coronary insufficiency, dizziness turns into fainting attacks, shortness of breath increases with the addition of angina pectoris, chest pain.
- With severe heart failure, nocturnal attacks of cardiac asthma occur, children experience shortness of breath even at rest and during sleep, and the condition worsens sharply.
- The transition to the terminal stage leads to a sharp progression of the disease and a serious condition; symptoms are relieved only for a short time.
Diagnosis of aortic valve stenosis in a child
The basis of diagnosis is listening to rough organic murmurs in the heart, conducting tests and a full instrumental examination. The following will also be shown:
- ECG with the study of the conductivity of the heart muscle, heart rhythm, and its reactions to stress.
- X-ray of the chest organs with darkening in the lungs due to congestive processes, enlargement of the left side of the heart.
- Ultrasound of the heart (EchoCG) with visual identification of the defect and determination of the degree of narrowing of the opening.
- conducting stress tests, identifying heart function under stress.
- catheterization of the cardiac cavities under general anesthesia with the introduction of a contrast agent into the cardiac cavities through the vessels. Using this method, the pressure inside the heart chamber is determined, especially in its left half.
If necessary, consultations with specialists (rheumatologist, cardiac surgeon) and additional diagnostic methods in the form of MRI or CT of the heart will be prescribed.
Source: DetStrana.ru
Treatment
The only effective treatment for SLA is surgery to eliminate the narrowing . The operation is indicated for patients with moderate and critical SLA. Minimal narrowing of the vessel does not require surgical intervention and in some cases may go away spontaneously.
The type of operation is selected depending on the severity of the patient's condition. In severe cases, surgery is performed in the first months of life. The average degree of stenosis is subject to surgical correction after the patient reaches the age of 5-10 years .
For isolated valvular SPA, different variations of valvuloplasty .
In most cases, endovascular balloon valvuloplasty . The essence of the method is to introduce an inflatable balloon into the stenotic area, into which air is pumped through a catheter. The expanding balloon mechanically pushes the narrowed area apart.
Less commonly used is open valvuloplasty , in which the surgeon dissects the fused commissures. Typically, open surgery is performed when balloon valvuloplasty is ineffective. Sometimes patients with a critical stage of pathology undergo balloon atrioseptostomy. Some forms of SPA require surgical correction in the form of systemic pulmonary bypass.
For supravalvular stenosis, reconstruction is performed in the area of narrowing using a patch from the patient’s own tissue or installing a xenopericardial prosthesis. The treatment strategy for subvalvular stenosis involves removing the narrowed section of the artery.
In the absence of postoperative complications, the prognosis is favorable.
Stages of narrowing of the larynx
There are 4 stages of narrowing of the larynx:
Compensated
Laryngeal stenosis still allows the amount of air necessary for a calm state to pass through. Physical activity and emotional arousal lead to an increase in blood flow, requiring more oxygen. Breathing quickens and becomes a little noisy. When crying and screaming, the baby develops shortness of breath, which is pronounced when inhaling. There are no signs of oxygen starvation yet. This condition can last up to 2 days.
Subcompensated
It manifests itself as moderately rapid, noisy breathing, shortness of breath is observed even in a calm state. The child feels discomfort, does not understand what is happening, and shows signs of anxiety and is agitated.
An additional symptom may appear: retracted intercostal spaces, abdomen, dimples above the collarbones. The skin around the lips and near the nose turns pale or acquires a bluish tint, and the heart rate increases. The 2nd stage can last up to 5 days; with additional irritants, the symptoms are more pronounced, and hospital treatment is necessary.
Decompensated
Vivid signs of oxygen starvation appear: the skin is pale, the lips and fingertips are bluish, the heart beats very quickly. The rhythm of breathing becomes disturbed, it becomes shallow, and it is difficult for the baby to breathe in a lying position. The child's behavior changes sharply from increased excitement to drowsiness, he sharply sucks in his stomach. Failure to provide assistance in a timely manner may result in suffocation.
Thermal
The child loses consciousness, breathing is shallow and intermittent. Heart rate slows down. The skin is clearly bluish and convulsions are possible.
With acute stenosis, a change in all stages is possible within a few hours; often the attack begins in the evening, the third stage can occur at night.
Forecast and preventive measures
Among the most important measures to prevent SLA in newborns is ensuring conditions for the normal course of pregnancy . Expectant mothers at risk should especially carefully follow the doctor's recommendations.
Modern diagnostic methods make it possible to identify disturbances in the formation of the fetal cardiovascular system, which makes it possible to prescribe treatment aimed at eliminating the disease that is their cause.
Minimal narrowing of the pulmonary artery in newborns does not affect the duration and quality of life . Patients with identified abnormalities are recommended to be monitored by a cardiologist and cardiac surgeon, as well as prevention of infective endocarditis.
Aortic stenosis in a child: symptoms
Cardiologists divide this pathology into three types: valvular stenosis or aortic valve stenosis (it is recorded more often than others), supravalvular and subvalvular.
In most cases, with moderate severity of the disease, newborn babies feel normal. But stage 3 disease, when the aorta diameter is less than 5 millimeters, is severe. The baby’s blood circulation is significantly impaired, and as a result, little oxygen reaches the internal organs. So they suffer from hypoxia. With third-degree pathology, the newborn’s condition rapidly deteriorates. This is manifested by constant, profuse regurgitation, shortness of breath, a weak sucking reflex, pale skin and cyanosis of the nasolabial triangle, and weight loss.
Possible complications
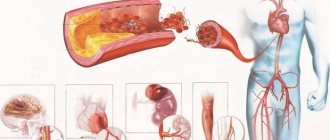
If atherosclerosis is not treated, the consequences can be very serious. When blood vessels narrow, the blood supply to the brain is disrupted, which can lead to the following complications:
- ischemic stroke of the brain, in which vision is impaired or completely lost, speech is completely or partially lost, sensitivity of half the body is lost, disability and even death are possible; dyscirculatory encephalopathy - characterized by mood swings, severe headaches, irritability, dizziness, decreased intelligence, memory impairment, mental disorders, and loss of ability to work.
Life forecast
The prognosis for pulmonary artery stenosis in children and adults, if all the instructions of the attending physician are followed, is favorable. The minimum risk of complications is observed in situations where surgical treatment was performed in childhood. But the lack of timely treatment is very dangerous; serious consequences and the likelihood of death increase by 4-5 times.
The average life expectancy with narrowing of the mouth of the pulmonary trunk depends on the characteristics of the development and course of pathological processes. On average it is 30-40 years. If the attending physician's instructions are not followed, the patient does not live more than 5 years.
With minimal congenital forms of stenosis, the patient’s quality of life and life expectancy do not decrease. Such patients are observed by a cardiologist and in most cases do not have a disability group. After surgical manipulations using stents, the average life expectancy of patients in 91% of cases is more than 5 years.
General description of the pathology
Before looking at the causes, symptoms and effective treatments, it is worth reviewing general information about stenosis. The pulmonary arteries are paired, fairly large branches of the pulmonary trunk that arise from the right ventricle.
The main function of this vessel is to transport venous (oxygen-poor) blood from the right atrium to the capillary system of the lungs, where gas exchange occurs and the blood is saturated with oxygen. In fact, this is where the pulmonary circulation begins. At the point where the pulmonary trunk exits the right atrium there is a tricuspid valve, which regulates blood flow.
Pulmonary artery stenosis is said to occur if there is a narrowing of the vessel itself or a malfunction of the valve (for example, if the valve leaflets are fused at the edges, then blood cannot circulate normally). Impaired blood flow negatively affects the condition of the entire body. First of all, the heart suffers - the right parts of the myocardium often hypertrophy in order to compensate for problems with blood ejection and cope with increased pressure in the right ventricle.
As statistics show, this pathology in most cases is congenital. Timely diagnosis and properly administered therapy help avoid possible complications.
Why is narrowing of the blood vessels in the head dangerous, and how to get rid of it?
Constriction of blood vessels in the brain is a fairly common phenomenon that leads to poor circulation. As a result of insufficient blood supply to tissues, not only does general health deteriorate and unpleasant symptoms appear, but there is also a risk of developing severe and life-threatening complications.
Most often, doctors identify two causes of cerebral vasoconstriction: atherosclerosis and arterial hypertension.
Atherosclerosis
This common vascular disease is one of the most common causes of vasoconstriction. Even at a young age, cholesterol begins to deposit on the walls of the arteries. This occurs due to not eating enough fiber-rich foods and eating too many fatty foods. As a result, deposits grow very quickly, the lumen of the vessels becomes narrower, blood circulation is difficult, the arteries lose their elasticity and cracks appear on their walls. Gradually, cholesterol plaques in the vessels become larger and can completely close the lumen. With atherosclerosis of cerebral vessels, important arteries are affected - the vertebral and carotid.
Arterial hypertension
In the chronic form of the disease, as a rule, deformation of blood vessels and a decrease in their lumen occurs. With severe hypertension, there is a deterioration in blood microcirculation; with sudden surges in pressure, small vessels are destroyed.
Surgery
Today, surgery is considered the most effective treatment option for this type of heart defect. Cardiac surgery uses more modern and effective methods every year. It is advisable to perform the operation only at the second or third stage. If the patient has moderate stenosis, he should be observed, but surgical intervention is postponed.
Stenosis is eliminated through surgery
Today, the following methods of eliminating the defect are used in surgery:
- Pulmonary valvuloplasty, which is performed in a closed manner, is very popular. More recently, it was used to eliminate a large number of defects and stenoses. Surgery is performed on the left side. The path to the heart is obtained through incision in the fourth intercostal space. The operation is performed using a valvulot - an instrument through which the necessary manipulations are performed on the walls of the valve.
- It is possible to perform the operation using catheterization. It is called pulmonary valvotomy. To do this, you need to insert a special probe, at the end of which there are special knives and a balloon.
- The operation can also be performed openly. Before it begins, the patient is connected to a machine with artificial blood circulation. Thanks to this, it is possible to gain access to the heart. The surgeon can visually monitor the process, so the defect is eliminated within a short time.