Acrocyanosis is the name by which in medicine we mean a change in color (blue discoloration) of the skin of the hands, feet, ears, tip of the nose and lips in humans. Often, bluish skin is not dangerous to health and is considered a normal physiological reaction of the body - for example, to cold. But acrocyanosis can also be a symptom of serious respiratory and circulatory diseases.
What is acrocyanosis?
Acrocyanosis is a microcirculatory disorder characterized by persistent bluish discoloration of the extremities of the body. Acrocyanosis is caused by spasm of small vessels of the capillary circle in response to cold and is not associated with occlusive arterial disease (there is no ischemic phase).
Acrocyanosis occurs symmetrically, especially in the arms, legs and distal parts of the face. Often the extremities of the body are cold, they sweat a lot and may become swollen. Unlike Raynaud's syndrome, acrocyanosis is not easily reversible, there is no pain, no trophic changes or ulcerations occur, and the peripheral arterial pulse is normal.
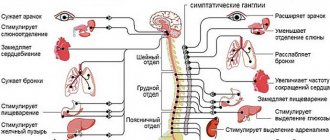
Diseases that cause acrocyanosis
Permanent or temporary blue discoloration of the skin can be caused by a number of diseases.
And even in the absence of chronic diseases, a person sometimes develops an acute form of cyanosis, which occurs suddenly, with rapidly increasing bluishness of the skin. This condition requires emergency care and hospitalization to find out the causes of poor health.
Chronic acrocyanosis and cyanosis can continue for a long time, while the bluish color of the skin changes from faint to clearly noticeable.
List of diseases in which this condition may develop:
- bronchial asthma;
- acute bronchitis or pneumonia;
- pulmonary embolism (PE);
- pulmonary tuberculosis;
- lung cancer;
- pulmonary infarction;
- Congenital heart defect;
- vegetative-vascular dystonia;
- anxiety and depressive disorders;
- inflammatory diseases of arteries and veins;
- chronic obstructive pulmonary disease;
- scleroderma;
- chronic cardiac or respiratory failure.
Also, cyanosis of the hands and face occurs when poisoned by poisons and certain medications , under the influence of which hemoglobin derivatives accumulate in the blood and are unable to transport oxygen to the body’s tissues.
The blood becomes thicker and darker, peripheral circulation is disrupted, causing the fingers and nasolabial triangle to turn blue.
Causes
The exact etiology of acrocyanosis is unknown. Side effects from medications and other substances have sometimes been reported. Some epidemiological evidence suggests that cold climates, occupational causes and low body mass index (BMI) are risk factors.
Additionally, acrocyanosis is common in young women (under 30 years of age) and often resolves completely after menopause. Therefore, it is believed that vasospasm is associated with neurohormonal abnormalities.
Acrocyanosis occurs where there is a change in central temperature control. Apparently, affected subjects are particularly sensitive to temperature fluctuations, with hypersensitivity to cold being more pronounced.
Reasons for appearance
There are several types of this disease:
- Essential. It is observed in teenage girls during puberty.
- Anesthetic. Occurs due to cold irritation on the surface of the skin.
Acrocyanosis indicates heart failure. It can also occur due to poisoning with any poisons or medications that are aimed at the formation of methemoglobin or sulfhemoglobin. “The bluest skin” is observed with heart defects. The appearance of the disease is usually associated with an increased concentration of hemoglobin against the background of excess oxygen consumption by tissues and other structures.
Often the disease is associated with an increase in hemoglobin concentration in the blood
The most common is central cyanosis, which occurs due to oxygen starvation, which is associated with a low degree of oxygen saturation in the blood.
Primary acrocyanosis
Essential (or primary) acrocyanosis is a benign condition sometimes associated with a neurohormonal disorder. In general, it tends to regress spontaneously and does not require special treatment. On the other hand, emergency medical intervention may be required if the extremities are exposed to extreme cold for a long time.
Symptoms
Symptoms of acrocyanosis are:
- the appearance of painful cyanosis on the feet and downturned hands at low ambient temperatures;
- bluish tint of the nose, lips and ears;
- increased cyanosis under the influence of cold (possibly in the presence of physical and mental stress) and its disappearance in warmth and when lifting the limbs upward;
- pastiness (slight swelling) of the hands, feet and fingers;
- increased sweating of the extremities, which accompanies cyanosis that occurs with heart disease.
Skin with acrocyanosis is always cold to the touch and may lose elasticity.
The essential type of acrocyanosis is usually accompanied by paralytic dilation of the venules and subcapillary venous plexus.
With acrocyanosis, which developed as a result of Raynaud's disease, attacks of pallor and cyanosis of the fingers are accompanied by the appearance of pain and the subsequent development of necrosis of the tissue of the acral parts. When exposed to cold and strong emotions, spasms of the arteries of the fingers, dilation of the capillaries and peripheral stagnation of blood are observed.
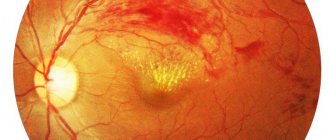
The central type of acrocyanosis, resulting from damage to the heart, is distinguished by a dark red-blue-violet skin tone, and when it is pulmonary in origin, the skin color becomes ash-gray.
Secondary acrocyanosis
Acrocyanosis may also be associated with a more serious health problem that should be looked for during diagnostic testing. Causal conditions include: connective tissue disorders, neurological disorders, vasculitis, problems leading to central cyanosis, antiphospholipid antibody syndrome (APS), cryoglobulinemia, infections, toxicosis and neoplasms.
In these cases, the skin changes observed are known as “secondary acrocyanosis.” They may have a less symmetrical distribution, express themselves later in life, and may cause pain and tissue damage. In general, proper treatment of the underlying condition can reduce the secondary symptoms of acrocyanosis.
Diagnosis of acrocyanosis
To determine the cause of acrocyanosis, the patient is prescribed a number of examinations, including:
- general and biochemical blood tests
- ECG
- pulse oximetry (determining blood oxygen saturation using a sensor that is worn on the finger)
- chest x-ray
The doctor will definitely find out from the patient when the blueness of the skin appeared, how its shade changes during the day, whether physical activity and other irritants provoke increased cyanosis, whether the limbs turn blue at rest and during sleep.
To differentiate acrocyanosis from angioneurosis, a test with raising an arm is used - the patient is asked to raise one arm up and hold it in this position for about 30 seconds. In this case, the bluishness of the skin caused by acrocyanosis (especially in adolescence) immediately disappears.
If necessary, the patient is prescribed specific tests:
- determination of blood gas composition;
- measurement of blood flow speed;
- CT or MRI of the chest;
- ultrasound and Doppler, Holter monitoring.
Signs and symptoms
Acrocyanosis is a condition characterized by persistent, symmetrical, uniform and painless peripheral cyanosis (see photo above). The extremities are often cold and the skin may be swollen. Hands and feet suffer from palmoplantar hyperhidrosis.
Unlike the closely related Raynaud's syndrome, cyanosis is persistent. In addition, there are usually no trophic changes in the skin, localized pain or ulceration.
Features of the flow
As a rule, with acrocyanosis a person does not feel any pain in the affected areas, but some patients experience frequent attacks of muscle spasms. Cramps are usually accompanied by pain. Raynaud's syndrome may stimulate the visual symptoms of acrocyanosis.
Thus, acrocyanosis mainly occurs in people with diseases in the cardiovascular system. These patients also experience swelling of the distal extremities. In other words, people with problems in the heart and blood vessels will have acrocyanosis with an additional symptom.
This condition is difficult to confuse with any other skin disease, since acrocyanosis has a unique list of symptoms specific to it. But to be completely sure of the diagnosis, a test is performed using a cold stimulus.
Acrocyanosis is almost always a symptom of a diseased heart.
If there is acrocyanosis, then when exposed to the skin, rapid bluing of the skin in the affected area is observed. When the test ends, the patient's skin returns to its normal shade.
Diagnostics
Acrocyanosis is diagnosed based on medical history and physical examination.
Pulse oximetry shows normal oxygen saturation. Capillaroscopy and other laboratory techniques may be useful, but only to complete the clinical diagnosis in doubtful cases, especially when concomitant pathology is suspected. With acrocyanosis, the pulse of the peripheral arteries is normal, in rhythm and quality: this allows us to exclude occlusive disease of the peripheral arteries.
Diagnostic methods
At the first symptoms, and as a rule, patients first complain about a change in the shade of the skin, you need to contact a cardiologist. Acrocyanosis can be one of the manifestations of heart failure.
To diagnose this disease, use:
- ECG.
- EchoCG or ultrasound of the heart.
One of the recommended diagnostic methods is echocardiography
When the problem does not lie in the functioning of the cardiovascular system, then the condition of the lungs and liver is analyzed. Laboratory blood tests are indicated.
Treatment
There is no specific treatment for acrocyanosis, and pharmacological approaches are usually not helpful. Some α-adrenergic and calcium channel blockers are mentioned among treatment options. In extreme cases, surgery called sympathectomy is recommended (rarely performed). Protection from cold is the most effective measure to avoid the occurrence of the disorder.
Apart from skin discoloration, there are no other symptoms and no loss of functionality, so patients with acrocyanosis can lead a normal life.
Important! Certain medications should be avoided for this disorder, such as dihydroergotamine (present in many medications used for headaches), beta blockers (used for hypertension or certain forms of altered heart rhythm). Keep in mind that excessive weight loss may aggravate or cause forms of acrocyanosis in susceptible subjects.
Acrocyanosis in newborns
Very often, acrocyanosis is observed in newborns. Such babies have a bluish tint on their limbs and lips. This is due to the physiological characteristics of infants, whose bodies begin to adapt to a new environment saturated with oxygen. Also, a baby's skin may turn blue when he cries or screams. Acrocyanosis in these cases goes away within a few days, when the child’s body is reconstructed after the embryonic type of blood circulation.
Blueness of the nasolabial triangle in a newborn with a heart defect
Constant acrocyanosis in a child means oxygen starvation of the body’s tissues, and therefore the brain. This sign can have serious consequences in the future and therefore requires consultation with a doctor. Often, the symptom of blue skin can help detect congenital heart defects in children or other diseases of the cardiovascular system.
Forecast
Primary acrocyanosis is a rare and benign condition with a good prognosis. Some treatments are available that can reduce symptoms in severe cases.
In newborns, acrocyanosis also has a favorable prognosis and goes away on its own.
Secondary acrocyanosis can be serious, depending on the underlying disease. Contact your doctor if you have symptoms of acrocyanosis. They can determine if there is an underlying condition that needs treatment.
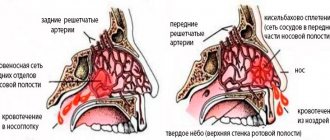
Symptoms of acrocyanosis
The most important symptom of acrocyanosis is a change in skin color. The severity of this symptom depends on the individual characteristics of the patient’s skin, its transparency and density. Vascular walls also affect the “cyanosis”; in this case, the “brightness” of the color depends on their condition. When a patient has acrocyanosis, the initial lesion area is the lips, in other words, in the initial stages, it is the mouth area that most often turns blue. The change in color is very easy to notice, since the “blue” contrasts strongly against the background of the usual shade of the mucous membranes. In second place in the list of the most common sites of injury are the distal extremities. Along with these areas, the nail plates on the fingers also turn blue. Less often, the initial affected area is the chin or nose. With a very small chance, acrocyanosis can appear on the skin of the ears.
But blue skin is not the only symptom that can occur with acrocyanosis. With this disease, the skin temperature in the affected areas decreases, the skin becomes susceptible to temperature irritants.
The skin doesn’t just turn blue, it becomes cold in the affected areas
Characteristic symptoms
The disease can manifest itself either as a slight bluish tint to the skin and mucous membranes, or as a pronounced dark color. It depends on the following factors:
- Severity of the disease - with “blue” congenital defects and severe heart failure, the symptoms are most pronounced.
- Thickness of the skin - the thicker it is, the less pronounced this symptom is.
- Skin pigmentation – in people with dark skin, bluish discoloration is more difficult to detect and may only be noticeable on the lips and nail beds.
- The number of small blood vessels in the skin. This is an individual feature. The more of them, the more pronounced acrocyanosis.
The color depends on the type of disease: with heart defects and heart failure, the skin acquires a dark blue-violet-red hue, and with lung diseases - ash-blue-gray.
Additional symptoms of acrocyanosis caused by heart disease include increased sweating of the extremities and swelling of the affected areas.
Acrocyanosis
Acrocyanosis is a bluish discoloration of the skin that occurs as a result of insufficient blood supply to small capillaries. It is most pronounced in areas of the body furthest from the heart: fingers, lips, tip of the nose and ears.
ICD-10ICD-9DiseasesDB
| I73.8 |
| 443.89 |
| 29444 |
Leave a request and within a few minutes we will find you a trusted doctor and help you make an appointment with him. Or select a doctor yourself by clicking on the “Find a Doctor” button. Find a doctor
- General information
- Forms
- Reasons for development
- Pathogenesis
- Symptoms
- Diagnostics
- Treatment
The term “acrocyanosis” was first used in 1896 by J. B. Crocq, who described a primary disorder of peripheral vascular tone and named one of its forms.
This disorder is not an independent disease, since it always occurs as a result of some disturbance in the body.
Acrocyanosis in newborns is not always a sign of the presence of pathology - it is often detected in the area of the feet, hands and nasolabial triangle in children born prematurely. Signs of acrocyanosis in infants become more pronounced with hypothermia, crying and severe anxiety.
Based on the cause of acrocyanosis, there are several types:
- Anesthetic, which occurs as a reaction when cold is applied to the surface of the skin. Slightly expressed cyanosis is a physiological phenomenon that develops when the skin temperature drops to 15 - 20 ° C.
- Essential or idiopathic. This form of acrocyanosis, caused by spasm of small arteries, is manifested by a persistent bluish tint of the lips, hands and other acral parts of the face in physically healthy females during puberty. It is observed even in warm conditions and at rest, intensifying during physical activity or under the influence of cold.
- Central or diffuse, which is caused by a sharp decrease in oxygen levels in the pulmonary circulation. Occurs with a marked increase in the content of reduced hemoglobin in venous blood (5.2 g%) as a result of impaired blood oxygenation in the lungs.
- Spasmodic, which develops as a result of spasm of small vessels in response to any irritants. It is detected in adolescence in persons with astheno-neurotic syndrome.
The occurrence of acrocyanosis is associated with increased oxygen utilization by peripheral tissues or with a slow linear blood flow velocity, which causes an increase in reduced hemoglobin (deoxyhemoglobin) in the venous blood.
The anesthetic form of acrocyanosis develops due to increased utilization of oxygen by the body in the process of maintaining the necessary heat exchange. In addition, when the body cools, some healthy individuals experience intravascular autoagglutination (sticking together) of red blood cells, which impedes peripheral blood circulation.
Cold agglutinins (antibodies that, when exposed to low temperatures, cause the formation of red blood cell conglomerates) can also be formed in infectious mononucleosis, atypical pneumonia, infectious hepatitis, cirrhosis of the liver, leukemia and some chronic infections.
The cause of essential acrocyanosis remains unclear. It is assumed that acrocyanosis of the hands and acral parts of the face in this case occurs as a result of spasm of arterioles and dilation of skin capillaries and venules (for example, a persistent cyanotic tint to the face is observed in persons regularly exposed to weather and associated vasodilation).
With a pronounced increase in the level of deoxyhemoglobin, a central or diffuse type of acrocyanosis develops.
The cause of central acrocyanosis may be:
- respiratory failure arising from bronchopulmonary pathology;
- pulmonary stenosis;
- pulmonary embolism;
- heart failure;
- venous-arterial shunt (ventricular septal defect, in which a significant amount of venous blood is discharged into the adjacent aorta), drainage of the vena cava into the left atrium and some other heart defects.
Acrocyanosis can also occur with:
- poisoning with poisons or medications, the use of which produces sulfhemoglobin or methemoglobin (a derivative of hemoglobin that is not capable of carrying oxygen);
- Raynaud's disease (a vasospastic disease in which small arteries and arterioles are damaged);
- Buerger's disease, which is an immunopathological inflammatory disease of arteries and veins (in most cases of small and medium diameter);
- syndrome of the scalene muscle, which is a complication of radiculitis of the cervical spine;
- cervical rib syndrome (presence of an additional small fibrous formation);
- scleroderma (systemic sclerosis, which is characterized by a violation of vascular innervation);
- Sudek's syndrome (pain syndrome that occurs after injury to the limbs and is accompanied by long-term trophic and vasomotor disorders);
- varicose veins.
Acrocyanosis is caused by an increased concentration of reduced hemoglobin in the capillary blood with sharply slowed blood flow.
The severity of acrocyanosis depends on the amount of reduced hemoglobin and a number of minor factors that do not cause cyanosis, but contribute to its occurrence. These factors include:
- Skin thickness.
- The amount of pigment in the skin (normal or pathological). With significant skin pigmentation (gypsies, etc.), with jaundice or Addison's disease, cyanosis can be detected only on the mucous membranes or on the nail bed.
- Concentration of oxyhemoglobin in the blood.
- The size, location and number of blood-filled, functioning capillaries and venules that are located in a given area of the skin (including the veins of the subpapillary layer). Cyanosis is always more pronounced on thin, poorly pigmented skin, equipped with a large number of blood vessels.
- Effect of ambient temperature on bare skin.
- Increased venous peripheral pressure.
The development of acrocyanosis is possible with:
- Insufficient oxidation of blood in the lungs. It occurs when the partial pressure of oxygen in the inhaled air decreases, tracheal stenosis, aspiration of foreign bodies that impede the flow of air into the alveoli, with prolonged pulmonary congestion, chronic obstructive pulmonary emphysema and disturbances in the respiratory dynamics of the lungs.
- Increased utilization of oxygen in tissues, which may be a consequence of slowing blood flow due to venous stagnation (local or cardiac origin) or insufficient blood supply (ischemia). Ischemia develops when the stroke volume of the left ventricle decreases and the blood pressure decreases (during collapse, cooling, etc.).
- When a significant amount of venous blood is mixed with arterial blood (when it enters directly through venous-arterial shunts or when blood flows through the pulmonary bed without the oxidation process in infiltrated or collapsed areas of the lungs). For cyanosis to develop, a third of the blood volume must flow from the venous to the arterial without oxidation.
Acrocyanosis cannot always be detected under resting conditions; it often manifests itself only when, during physical activity, oxygen consumption increases simultaneously with an increase in the level of reduced hemoglobin in capillary blood above a critical value.
Symptoms of acrocyanosis are:
- the appearance of painful cyanosis on the feet and downturned hands at low ambient temperatures;
- bluish tint of the nose, lips and ears;
- increased cyanosis under the influence of cold (possibly in the presence of physical and mental stress) and its disappearance in warmth and when lifting the limbs upward;
- pastiness (slight swelling) of the hands, feet and fingers;
- increased sweating of the extremities, which accompanies cyanosis that occurs with heart disease.
Skin with acrocyanosis is always cold to the touch and may lose elasticity.
The essential type of acrocyanosis is usually accompanied by paralytic dilation of the venules and subcapillary venous plexus.
With acrocyanosis, which developed as a result of Raynaud's disease, attacks of pallor and cyanosis of the fingers are accompanied by the appearance of pain and the subsequent development of necrosis of the tissue of the acral parts. When exposed to cold and strong emotions, spasms of the arteries of the fingers, dilation of the capillaries and peripheral stagnation of blood are observed.
The central type of acrocyanosis, resulting from damage to the heart, is distinguished by a dark red-blue-violet skin tone, and when it is pulmonary in origin, the skin color becomes ash-gray.
Acrocyanosis is diagnosed based on the following data:
- medical history;
- general and biochemical blood test;
- ECG.
The differential diagnostic difference between acrocyanosis and angiotrophoneurosis and other angioneuroses is a test with raising the limbs, in which the bluish tint in the presence of acrocyanosis quickly disappears.
Cyanosis of central origin is characterized by normal skin temperature (with acrocyanosis it is lowered and acquires a bright red color after pressure) and a persistent bluish tint.
Treatment of acrocyanosis is aimed at eliminating the cause of the disease. Treatment includes:
- taking vasodilators;
- vitamin therapy;
- physical therapy;
- diet therapy;
- massage;
- physiotherapy.
Found a mistake? Select it and press Ctrl + Enter
Paget-Schroetter syndrome is an acute thrombosis of the deep brachial veins, which is often observed in the axillary or subclavian veins.
Orthostatic collapse (orthostatic hypotension) is a human condition in which a sudden transition of the body from a horizontal to a vertical position or prolonged standing causes a decrease in blood pressure as a result of insufficient blood flow to the brain or a delayed reaction of the heart to a change in body position. Orthostatic hypotension is accompanied by dizziness and darkening of the eyes, after which fainting may develop.
Wolff-Parkinson-White syndrome (WPW syndrome) is an electrocardiographic syndrome that is associated with preexcitation of the ventricles of the heart resulting from the presence of an additional (abnormal) atrioventricular junction (AVJ).
Pre-excitation of the ventricles provokes the development of various arrhythmias, so the patient may experience supraventricular tachycardia, atrial fibrillation or flutter, atrial and ventricular extrasystole and corresponding subjective symptoms - palpitations, shortness of breath, hypotension, dizziness, fainting, chest pain.
Bradycardia is a decrease in heart rate, which is caused by a decrease in the function of the sinus node (the first order pacemaker) or a blockade of the conduction of electrical impulses between the nodes of the heart. The heart rate during bradycardia decreases to less than 60 beats per minute in adults, 70-80 beats in children and adolescents, and less than 100 in infants.
Tetralogy of Fallot is a “blue” heart defect that combines, as defined by a French pathologist named Fallot, four anomalies: stenosis, high ventricular septal defect, aortic dextraposition, right ventricular hypertrophy.
Source: https://liqmed.ru/disease/akrocianoz/
Treatment of the disease
Therapy for such diseases is aimed at eliminating the underlying cause:
- surgical operations are performed if congenital or acquired heart defects are detected;
- prescribe the use of medications for blood pressure;
- use drugs to maintain heart function;
- they use medications to strengthen blood vessels - they will help prevent their expansion.
You can use camphor oil to rub the affected areas. To relieve arteriole spasms, you can use decoctions of medicinal herbs, but before using home treatments, you should consult a doctor.
Classification
Central cyanosis is diffuse and of maximum severity. It develops with weak arterialization of the blood, leading to hypoxia. Gas exchange is disrupted in the lungs, excess carbon dioxide accumulates in the arterial blood, which is clinically manifested by blueness of the conjunctiva of the eyes, palate, tongue, mucous membranes of the lips and cheeks, and facial skin. Qualitative and quantitative changes in hemoglobin in the blood lead to disruption of its transport function and hypoxia.
manifestations of cyanosis in adults and children
Acrocyanosis is localized on the feet, hands, tip of the nose, ears, lips. Peripheral cyanosis is considered a normal variant in the first days of a newborn’s life. Its origin can be easily explained by the incompletely eliminated germinal type of blood circulation, especially in premature infants. Blueness of the skin increases with swaddling, feeding, crying, and anxiety. When the infant fully adapts to the outside world, cyanosis will disappear.
Acrocyanosis in adults is a sign of varicose veins, thrombophlebitis, vegetative-vascular dystonia, atherosclerosis, arteritis.
Cyanosis occurs:
- Permanent and transient, occurring with low blood glucose levels or inflammation of the meninges,
- Total or general
- Regional or local: perioral, distal,
- Isolated.
Local cyanosis develops in places with the largest number of blood vessels, perioral - around the mouth, periorbital - around the eyes. Blueness of any part of the human body can appear due to pulmonary and cardiac pathology.
There are several types of cyanosis based on origin:
- The respiratory type is caused by an insufficient volume of oxygen in the lungs and a disruption in the transport chain of its supply to cells and tissues. It develops when there is a complete or partial disruption to the movement of air along the respiratory tract.
- Cardiac type - insufficient blood supply to organs and tissues leads to oxygen deficiency and bluish skin.
- The cerebral type develops when the blood loses its ability to attach oxygen to hemoglobin and deliver it to brain cells.
- The metabolic type develops when the absorption of oxygen by tissues is impaired.
Respiratory cyanosis disappears 10 minutes after oxygen therapy; all other types persist for a long time. Massaging the earlobe helps get rid of acrocyanosis.