What is arrhythmia?
Arrhythmia refers to various changes in the heart rhythm. These types of disorders occur due to diseases of the cardiovascular system, endocrine system or metabolic disorders in both men and women. Quite often, arrhythmia can be observed in women during pregnancy, when the body of the expectant mother rearranges its work.
Normally, the human heart beats about 70 times per minute. If a person has an arrhythmia, then the rhythm of his heart contractions will be different.
Heart arrhythmia in the morning
Interruptions in the functioning of the heart are called arrhythmia.
This is any pathological change in the frequency of beats. Sometimes similar disruptions occur after sleep. Both the strength of contractions and their frequency are impaired. In a state of calm, heart rate fluctuates between 60-80 beats. With physical activity or diseases of the cardiovascular system, heart function worsens. If such a phenomenon often occurs in the morning, you must definitely visit a doctor and find out the factors that could trigger the appearance of morning arrhythmia.
Causes of pathology
High blood pressure in the morning can occur even in healthy people.
This is due to the fact that the body is just recovering from sleep. In this case, the heart muscle begins to work intermittently, either increasing the rhythm or slowing it down. So, normal indicators increase to 110 beats and above.
The development of sinus arrhythmia in the morning is associated with deterioration in the functioning of the respiratory tract. Often the cause of arrhythmia is snoring at night. Because of it, the airways narrow and the load on the main organ increases. In this case, bradycardia develops.
Chronic runny nose or nasal septum disorders also lead to arrhythmia in the morning. The following reasons are also identified:
- necrosis of cardiac muscle tissue;
- Karyomyopathy;
- ischemia;
- circulatory disorders of the heart muscle;
- predisposition to arrhythmia (problems with the structure of the coronary vessels or myocardium).
Symptoms of the disease
A heartbeat accelerated to 90 beats per minute indicates the development of tachycardia.
Arrhythmia is divided into 5 types. Each of them has its own characteristics. With tachycardia, the beats accelerate to 90 per minute.
Bradycardia, on the contrary, is characterized by the fact that the heart rate drops below 60 beats per minute. With atrial fibrillation, the patient feels painful spasms near the heart with each beat.
If the patient feels an additional contraction, then this is a clear symptom of extrasystole. When blocked, the pulse slows down, which leads to death.
Patients sometimes complain not only of chest pain, but also of cramps. When the heart rate decreases, it is not always possible to find a person’s pulse. There are often complaints of dizziness or loss of consciousness.
Complications
A neglected condition leads to serious consequences. Without treatment, the disease causes the development of ischemia and blood clots in the vessels. It also risks a heart attack or even death from a heart attack. If morning arrhythmia appears due to oxygen starvation, then as a result, brain function is disrupted. As a result, the patient's memory deteriorates or a stroke may occur.
Diagnostics
If a person notices any symptoms of the disease, then he needs to visit a doctor.
It is better to consult a doctor with the first signs of the disease and not ignore the problem. Electrocardiography (ECG) is prescribed for the study, which helps to identify pathologies.
But they also perform an ultrasound examination to determine the size of the heart valves and the general condition of the organ. A daily Holter test helps to make the diagnosis as accurately as possible.
In rare cases, additional exercise tests may need to be performed.
Treatment of morning arrhythmia
Drug treatment is prescribed. Patients most often use beta blockers of sodium, potassium and calcium channels. Be sure to prescribe a course of vitamins (potassium and magnesium) to maintain health. Another method is electropulse treatment.
It is designed to restore the rhythm of the organ in a short time. Rarely resort to surgical intervention. Doctors recommend a diet that excludes all trans fats, alcohol and flour. Vegetables, fruits, and lean meats are best steamed or stewed.
As a treatment for morning arrhythmias, they resort to simple physical exercises. They strengthen the body and stimulate the functioning of the main organ. It is necessary to exclude running, lifting weights and intense training in the gym. But walks in the fresh air, exercise and yoga will only bring benefits.
Traditional methods are often used to treat morning sickness. The most common method is an infusion or decoction of valerian. In the first case, the root of the plant is poured with boiling water and infused for about 10 hours. Then take 3 teaspoons per day. A decoction is prepared using 2 tablespoons of solution and 100 milliliters of water.
Boil for 15 minutes. Take 4 spoons per day.
Symptoms
Symptoms will help you immediately notice health problems, which means starting treatment for the disease right away. Symptoms of arrhythmia depend solely on the type of arrhythmia, and also vary slightly depending on age - the manifestations of the disorder in a child may not coincide with the manifestations in old age. But there are common signs of heart rhythm disturbances:
- heartache;
- abnormal pulse;
- dizziness;
- fainting;
- weakness.
Important! If these signs are detected, you should immediately go to a cardiologist and do an ECG, which will determine the condition of the heart. You can often notice a change in the heart rate on the cardiogram during deep breaths - in this case they speak of respiratory arrhythmia.
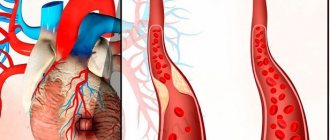
Causes of arrhythmia after a heart attack, stenting
The first hours after an acute disturbance of coronary circulation are accompanied by all sorts of disturbances in the formation of impulses and their conduction through the myocardium. One type of arrhythmia replaces another, they disappear and recur. This is due to the following factors:
- decreased blood flow to heart cells - ischemia, hypoxia, metabolic disorders;
- destruction of myocardiocytes with their loss of potassium and an increase in its content in the extracellular space;
- change in the ratio of basic electrolytes, acid-base balance;
- excess stress hormones in the blood;
- damaging effects of free radicals.
The variety of rhythm disturbances is caused by the fact that different parts of the myocardium experience different pathological influences. Therefore, even neighboring zones have different properties - some cells are already leaving the stage of refractoriness (inability to respond to a signal), while others cannot yet change the polarity of the membrane.
As a result, the myocardium becomes mosaic, foci are formed along which impulses move in a circle, unable to move further. This is how extrasystoles and ventricular tachycardia, flutter and fibrillation are formed.
A separate group is reperfusion (reperfusion - resumption of blood supply) rhythm disturbances. They appear during the dissolution of a blood clot, stenting or bypass surgery of the coronary arteries. Arrhythmias in this case arise due to a sharp influx of blood into the ischemic zone and the surrounding stunned myocardium.
Spasm of small arterioles and widespread disruption of microcirculation cause a malfunction of excitability and conductivity functions, suppress the processes of restoration of cell polarity and stimulate the formation of many loops of recirculation of signals. Paradoxical myocardial dysfunction occurs with improved cell nutrition, which reduces the effectiveness of the operation. Reperfusion may help:
- expansion of the zone of destruction of the heart muscle;
- decreased contractility of the left ventricular myocardium;
- electrical instability leading to various types of ventricular arrhythmias.
We recommend reading the article about arrhythmia after a stroke. From it you will learn about the causes of arrhythmia after a stroke, the diagnosis of arrhythmia and treatment methods. Read more about the complications of myocardial infarction here.
Classification according to ICD-10
By duration:
- first detected - a single attack;
- paroxysm of atrial fibrillation – when it lasts about two days;
- persistent – about one week;
- long-persistent – lasts up to one year;
- permanent – lasts more than one year.
For symptoms that can interfere with a normal lifestyle:
- asymptomatic – occurs without visible signs;
- mild – symptoms are minor and do not interfere with a person’s normal lifestyle;
- severe – signs do not allow you to lead a normal life;
- severe – the symptoms are so serious that the person cannot live independently without the help of other people.
According to the location of the violation, they are distinguished:
- atrial (supraventricular);
- ventricular;
- sinus;
- atrioventricular.
Reference! For young people of military age, it may be interesting whether they are accepted into the army with arrhythmia, what indicators influence the determination of the fitness category and what you need to know in order not to end up in the army.
Mechanical damage
Complications of myocardial infarction caused by mechanical causes include a number of serious lesions:
- heart failure;
- dysfunction of the left ventricle;
- cardiogenic shock (a complex symptom associated with damage to the heart, kidneys and brain);
- rupture of the ventricular wall or septum between the ventricles;
- aneurysms and false aneurysms;
- right ventricular failure;
- mitral valve damage.
After a heart attack, left ventricular dysfunction or heart failure may occur. Severe heart failure after cardiac rupture indicates a poor prognosis.
Heart failure occurs due to damage to the myocardium itself during a heart attack, but can be caused by arrhythmia or mechanical complications, such as mitral valve or ventricular septal defects. The severity of heart failure depends on the extent of the heart attack and the presence of any other complications.
Another mechanical complication of acute illness is cardiogenic shock. It occurs in 5-20% of patients suffering from cardiac rupture. Its severity is determined by discernible wheezing in the pulmonary fields and the audibility of heart sounds.
Read also: Cardiac arrhythmia symptoms and treatment
Heart failure generally responds well to oxygen, diuretics, and intravenous nitrates. Patients with clinical signs of heart failure and diabetes should receive Eplerenone or Spironolactone, the second drug is cheaper but has more side effects. Patients receive supplemental oxygen, and very severe heart failure may require surgery. If it is impossible, then the probability of death is more than 70%.
Another mechanical complication is rupture of the interventricular septum or ventricular wall. This event occurs infrequently, but is life-threatening. Risk factors for this complication: old age, female gender. This complication often occurs when the heart rate is elevated on admission or when blood pressure is elevated.
This complication can develop as early as 24 hours after myocardial infarction, but often occurs 2-7 days after it. The mortality rate exceeds 90%.
Post-infarction rupture of the interventricular septum occurs. Patients may initially have no significant cardiopulmonary symptoms, but then quickly develop angina, shock, or pulmonary edema and other symptoms. A sign of a ventricular septal rupture may be hard sounds at the left lower edge of the sternum. The echocardiogram shows an increase in oxygen saturation of the right ventricle. Post-infarction ventricular septal defect requires urgent surgical intervention. When the wall ruptures, bleeding occurs into the pericardium, which leads to blockage of the heart with progression of the lack of cardiac function. Deaths are common. With this complication, the only hope is surgery.
Sometimes false aneurysms of the left ventricular wall occur. They may remain clinically undetected and only detected by routine testing, but in some patients the consequence is heart failure and arrhythmia. The diagnosis is confirmed using echocardiography, MRI or CT. Spontaneous rupture of the false aneurysm may occur in about a third of cases, so surgery is recommended for all patients.
Mitral valve damage may be due to ischemia, necrosis, or rupture. Mitral valve defects after myocardial infarction carry a poor prognosis, but are often temporary and asymptomatic. Echocardiography should be performed to confirm the diagnosis, especially if it is necessary to distinguish it from a ventricular septal rupture, and to assess the severity of the injury. Sometimes a rupture requires replacement of the mitral valve. Before surgery, coronary angiography is performed.
Some patients experience post-infarction left ventricular aneurysm. The frequency of such events is 2-15%. Five-year survival rate is observed in 10-25% of cases. An x-ray may show an abnormal bulge on the left border of the heart, but definitive diagnosis is made by echocardiography, MRI, and CT. With an aneurysm, congestive heart failure may occur. Patients receive ACE inhibitors, digoxin and diuretics. In the case of wall thrombi, anticoagulation with warfarin is indicated.
Severe heart failure and ventricular arrhythmias in patients with aneurysms are indications for surgery.
Complications after a heart attack in many cases lead to right ventricular failure. This disorder manifests as low blood pressure, venous distension with clear lungs and absence of shortness of breath. A severe form can lead to mental changes. Diagnosis is made using echocardiography. Nitrates, diuretics and similar drugs should be avoided. Treatment is limited to supporting the filling of the ventricles with fluid; inotropes, such as dobutamine, are prescribed. In most patients after acute injury, the condition of the right ventricle improves within 2-3 days.
Obstruction of the left ventricular outflow tract can occur for various reasons: due to left ventricular hypertrophy, bleeding, dehydration, mitral valve defects, stress, anxiety, medications. This is a rare complication. Diagnostic test - echocardiography.
A life-threatening arrhythmia (eg, ventricular tachycardia or systemic block) may be the first manifestation of ischemia. Arrhythmia leads to many reported cases of sudden cardiac death. Heart rhythm disturbances that occur in the first 2 days after a heart attack do not depend on its degree. Late arrhythmias that occur on the third day and later depend on the degree of ventricular damage. The risk of death from arrhythmia is highest during the first 6 months after myocardial infarction and remains high for the next 2 years.
Arrhythmias can be caused by the heart attack itself, toxic products, or metabolic disorders (especially potassium or magnesium imbalance). Some cases of arrhythmia (eg, ventricular tachycardia) do not require treatment. Minor arrhythmias should not be treated. But serious disorders, especially in older patients, cannot be missed. Their symptoms are pain, acidosis, hypoxia.
Early treatment of arrhythmias can prevent cardiogenic shock, which leads to irreversible myocardial damage.
Heart block and conduction disturbances are often temporary. Sinus tachycardia can occur due to pain, anxiety, or medications.
For ventricular arrhythmia, patients are prescribed intravenous epinephrine, amiodarone or beta blockers, and magnesium.
Reasons for development
There are many reasons that cause such violations. Let's look at the main ones:
- serious diseases of the cardiovascular system (heart disease, heart attack, high/low blood pressure);
- improper functioning of the thyroid gland;
- improper metabolism;
- a large number of energy drinks and caffeine-containing drinks that a person consumes;
- alcohol consumption;
- smoking has a detrimental effect on the functioning of the heart;
- heredity can also increase the risk of arrhythmia;
- nervous stress.
Possible complications of myocardial infarction
Often, patients with myocardial infarction die not from the heart attack itself, but from its complications.
Complications of myocardial infarction include:
- ischemic complications: angina pectoris, recurrent infarction, expansion of the infarction zone;
- mechanical complications: heart failure, cardiogenic shock, mitral valve dysfunction, aneurysms, cardiac rupture;
- arrhythmias - atrial, ventricular and other types;
- thrombosis and embolism;
- inflammatory complications - pericarditis;
- psychosocial complications (including depression).
Mortality after a heart attack remains high, and most often it occurs from arrhythmia. Let's take a closer look at the main types of complications.
Classification
There are several main types of arrhythmia:
- Sinus tachycardia is characterized by an increased heart rate (more than 90 beats per minute). A person feels a constantly high pulse.
- Sinus arrhythmia is an abnormal alternation of contractions. This type of arrhythmia most often occurs in young people and even children. With this type, when inhaling and exhaling, a person’s pulse changes.
- Sinus bradycardia is a slow pulse (less than 55 beats per minute). At rest, many people have a low heart rate, but in normal conditions this indicates problems with the heart.
- With paroxysmal atrial fibrillation, the correct rhythm is observed, but at the same time 240 beats per minute. People with this type of arrhythmia experience pallor and frequent fainting.
- Paroxysmal tachycardia is an increase in heart rate to 140, and sometimes up to 240 beats per minute. Such an increase can appear at any time and also go away unexpectedly.
- Extrasystole is strongly manifested in human sensations. A person feels either tremors in the chest or freezing.
Types of rhythm disturbances
Arrhythmias, which have a significant impact on blood circulation, during myocardial infarction can occur in the form of atrial fibrillation, ventricular extrasystoles, paroxysmal tachycardia and fibrillation.
Atrial fibrillation
Most often occurs in the following pathological conditions:
- severe damage to the anterior wall of the left ventricle;
- circulatory failure; Heart impulses
- activation of sympathetic impulses;
- pulmonary embolism.
It is characterized by a very frequent atrial rhythm (250 - 350 per minute), but not all impulses pass to the ventricles through the atrioventricular node.
If their rhythm is close to normal, then it can be tolerated quite well by patients. With rare contractions, it helps to reduce blood flow into the aorta and the appearance of cardiogenic shock.
An excessive increase in speed aggravates heart failure, since the filling of the ventricles with blood is disrupted due to short diastole, coronary blood flow drops even more, and the high contraction frequency increases the heart's need for oxygen. The consequences of atrial fibrillation are:
- expansion of the infarction zone;
- severe drop in blood pressure;
- acute left ventricular failure, pulmonary edema.
Expansion of the infarction zone
The appearance of this type of arrhythmia is regarded as a complication that poses a threat to life.
Ventricular
The most common extrasystole is of ventricular origin. It is not detected in less than 5% of patients, therefore it is perceived as a sign of a heart attack, and not its complication . In itself, this rhythm disturbance is not so dangerous, especially if the source of excitation is in the sinus node.
But if an extraordinary contraction is superimposed on the T wave of the previous normal complex, then the likelihood of transformation of extrasystole into ventricular fibrillation and sudden death increases.
In addition to extrasystoles R on T (early form), unfavorable options include:
- from several foci (polymorphic);
- double;
- salvo (several in a row).
Paroxysmal tachycardia can be short or long. In the second case, blood circulation is disrupted up to cardiogenic shock, left ventricular failure.
In half of the patients, it turns into the most unfavorable variant of arrhythmia - ventricular fibrillation. With it, muscle fibers contract in an uncoordinated manner, which prevents effective cardiac output. This condition is life-threatening, since without immediate restoration of the rhythm it leads to death.
Fibrillation can be primary, secondary and late. Primary is noted in the first hours or days of a heart attack before other complications. It is a manifestation of instability of the heart muscle, an acute cessation of blood flow to the destruction zone. Often leads to sudden cardiac arrest.
Secondary is associated with pulmonary edema or shock. The time of its detection is 1 - 3 days of the disease. The late form occurs on days 15–45 or even by the end of the second month, more often with anterior localization of necrosis or against the background of another rhythm disturbance.
Ventricular fibrillation is characterized by the sequential appearance of the following symptoms:
- severe weakness, dizziness;
- rapid loss of consciousness;
- convulsive muscle contraction;
- involuntary release of urine and feces;
- dilated pupils;
- wheezing breathing;
- rare and irregular inhalations and exhalations;
- clinical death - no consciousness, breathing, pulse in the carotid artery, pupils do not react to light.
First aid for an attack
First aid often saves the lives of people who are experiencing various attacks. The first minutes are very important - the person who is nearby must know how to behave, not panic, but take decisive and correct actions.
First aid for arrhythmia directly depends on the type of arrhythmia. However, there are several actions that need to be taken during an attack:
- Make sure that fresh air flows freely into the room.
- Release the victim's neck so that he can breathe freely.
- Be sure to measure your pulse and blood pressure to make sure it is an arrhythmia attack.
- Help the person get into a comfortable lying position. If this is bradycardia, then the legs should be slightly higher than the body. This ensures proper blood circulation.
- Give the medicine prescribed by the doctor.
- Wash your face with cool water.
Arrhythmia is a very dangerous disorder; it is not for nothing that cardiovascular diseases are the first cause of death in the population. Therefore, if the attack is severe, call an ambulance immediately.
General information
I want to start with general information, since it is important to understand who most often suffers from an atypical variant. This will allow doctors and the person himself to pay attention to deviations in a timely manner.
Risk group
Manifestations of atypical forms are most often observed in risk groups; I pay special attention to the following categories:
- patients with coronary artery disease and a history of heart attack;
- elderly people;
- patients with diabetes mellitus;
- alcoholics and experienced smokers;
- hypertensive patients and persons with cardiosclerosis of any origin.
Etiology and pathogenesis
An asymptomatic course or manifestations in the form of rhythm disturbances are observed in people who have had diabetes for a long time. This is caused by the fact that when blood sugar rises, nerve fibers atrophy and they cannot transmit impulses to the central nervous system. In this case, deviations become noticeable only after an ECG.
The cerebral form of infarction is typical for people with cerebral circulatory disorders, so the initial picture resembles an ischemic stroke. The abdominal variant manifests itself due to the close proximity of the phrenic nerve and abdominal organs to the posterobasal region of the heart.
General manifestations
Atypical forms of myocardial infarction have features in their manifestation:
- sensations of unexpressed pain or its absence;
- severe pain elsewhere (abdomen, shoulder blade, spine, joints of the upper extremities);
- the duration of such manifestations is 2-3 hours to 1-2 days;
- restoration of the typical picture of myocardial necrosis after some time.
The prognosis for an atypical heart attack is unfavorable, since the patient often presents late.
Time is spent visiting a therapist and getting tests. But in fact, he requires urgent hospitalization in the cardiac intensive care unit.
Treatment methods
If you or your loved ones have already encountered this disease, then you need to find out what treatment methods currently exist. Timely treatment can save you from disastrous consequences. The doctor will tell you which treatment method is right for your case.
If the arrhythmia occurred against the background of another disease, then it will be enough to cure it in order to forget about such heart problems forever. However, if the violations are the most serious, then certain measures must be taken. There are several surest remedies: drug treatment and surgery, used only in extreme cases.
There are several types of medications:
- those that block Ca channels;
- those that block K channels;
- those that block Na channels;
- beta blockers.
Important! As you understand, such medications can only be prescribed by cardiologists.
Under no circumstances should you treat a disease such as arrhythmia on your own. Therefore, when using traditional methods of treatment, be sure to consult with your doctor.
Peripheral forms
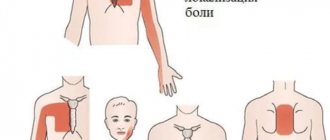
There are also atypical variants of myocardial infarction, when parts of the body and organs located far from the heart hurt.
In my practice and in the experience of my colleagues, the following manifestations of the disease have been encountered:
- nagging pain in the left hand (sometimes in the wrist or even one finger);
- sharp shooting under the left shoulder blade;
- pain in a separate area of the spine, reminiscent of exacerbation of osteochondrosis;
- discomfort in the lower jaw or left side of the head;
- sore throat, similar to a sore throat or inflammation due to a cold.
Prevention
Prevention is the best treatment. One cannot but agree with this statement. It is much easier to prevent a disease than to try to get rid of it later.
- Charger . Physical education and breathing exercises are useful for all people; they keep the body in good physical shape. Improves heart function, because a person is able to overcome serious physical exertion. Sport is the best way to keep your body healthy for many years.
- Avoid alcohol and tobacco products . Bad habits can completely destroy a person’s health. Such habits have a particularly harmful effect on the cardiovascular system.
- Proper nutrition and diet . You need to give up junk food, which has a bad effect on all organs and systems in the human body. Include more fruits and vegetables in your diet, which contain many vitamins.
- Try to avoid emotional overstrain and severe stress . Stress is the main weapon of any disease.
- Watch your weight , because obesity increases the risk of arrhythmia.
Pericarditis
A complication of a heart attack that affects every tenth patient is the inflammatory heart disease pericarditis. It usually develops on the second to fourth day after a heart attack. Manifests itself as fever with chest pain. On a chest x-ray, you can sometimes see a spherical enlarged heart. Mild pericarditis may be detected by echocardiography.
Pericarditis is treated with anti-inflammatory and painkillers.
Read also: Angina pectoris arrhythmia
Nonsteroidal anti-inflammatory drugs are used initially, and steroids are indicated if signs are severe or re-drainage is required.
Changes in the patient's mental status tend to be present to varying degrees in heart attack patients and reflect poor brain health. This may include fear, irritability and anxiety, sometimes anger, frustration, sadness and hopelessness, 65% of patients have elements of depression, and 20% of patients develop severe depression.
Myocardial infarction increases the risk of suicide. Depression after myocardial infarction worsens the overall prognosis of recovery: patients with depression have a 3.5 times higher risk of death. This factor is often more important than gender, weight, blood pressure and cholesterol. However, depression is diagnosed in only a quarter of patients, since its main symptoms are similar to those of coronary heart disease, and patients in a hospital setting are reluctant to complain about their mental state.
If depression is detected, the use of antidepressants in combination with psychotherapy is recommended.
The incidence of complications of acute myocardial infarction is constantly decreasing, but mortality from the disease remains at a high level. Detailed knowledge of complications and their risks can help to make an early diagnosis, initiate timely therapy or, if necessary, resort to surgery to achieve a favorable outcome.
Treatment of arrhythmia with folk remedies
Important! You cannot prescribe treatment for yourself. Before treatment, be sure to consult your doctor, because... Even folk remedies can harm the body!!!
Read also Dermatosis - symptoms, causes, types and treatment of dermatosis
Valerian infusion. 1 tbsp. Pour a spoonful of crushed valerian root into 1 glass of boiled water (room temperature). Leave in a sealed container for 8-12 hours, strain and take 1 tbsp. spoon 3-4 times a day.
Valerian decoction. Pour 2 teaspoons into 100 ml of water, boil for 15 minutes and take 1 tbsp. spoon 3-4 times a day before meals.
Calendula infusion. Pour 2 teaspoons of calendula flowers with 2 cups of boiling water, let stand for 1 hour and strain. Drink 0.5 glasses 4 times a day.
Melissa infusion. 1 tbsp. Pour 2.5 cups of boiling water over a spoon, let stand for a couple of hours (wrapped up) and strain. Drink 0.5 glasses 3-4 times a day. Take weekly breaks once every 2 months.
Hawthorn tincture. Pour 10 g of dried hawthorn fruit into 100 ml of vodka and leave to brew for 10 days. Strain and take 10 drops with water 3 times a day before meals.
Decoction of hawthorn flowers. Pour 5 g of hawthorn flowers into 1 cup of boiling water, cover with a lid, heat in a water bath for 15 minutes, cool and strain. Drink 0.5 glasses 2-3 times a day 30 minutes before meals.
Radish juice with honey. Mix fresh juice of black radish and honey in a 1:1 ratio. Take 1 tbsp. spoon 2-3 times a day.
Horsetail infusion. 1 tbsp. Pour 400 ml of boiling water over a spoonful of dry crushed horsetail herb, let it brew for 2 hours and strain. Take 1 tbsp. spoon 5-6 times a day.
Snack for arrhythmia. Grate the celery, add parsley, dill, mayonnaise and a little salt. Eat the resulting mixture once a day, before dinner. This delicious medicine can be eaten separately, or spread on bread.
Onion with apple. Chop a small onion and 1 apple. Mix and take between meals 2 times a day for 1 month.