Local expansion of the vascular wall due to its stretching and thinning is called an aneurysm. The disease is typical for people of any age and can develop primarily or secondary.
Aneurysms of the heart and blood vessels in children most often have an infectious and traumatic etiology, and in 20% of cases they are large and gigantic in size. Pathology is 2-3 times more common in boys.
Causes in newborns and older children
Frequency of occurrence per 100,000 children:
- Among newborns – from 3.5 to 5.7;
- Among children – 2.0-2.2;
- Among teenagers – 1.0-1.4.
According to the mechanism of development, true aneurysms predominate (consisting of all layers of the vascular wall), and according to their shape, saccular aneurysms (80%). Most of the diagnosed pathology occurs in the cerebral vessels (23-29%), aorta (12-20%) and heart (40-42%).
Causes of development in newborns:
- Genetic abnormalities of structural proteins;
- Hypoplasia of the heart and blood vessels;
- Congenital defects;
- Pathology of pregnancy in the mother;
- Pathology of the ovum and chorion in the fetus;
- Placental insufficiency and placental abruption in the 1st-2nd trimester of pregnancy;
- Fetal hypoxia.
Causes in children:
- Marfan syndrome;
- Viral and bacterial myocarditis;
- Injuries;
- Heart diverticulum;
- Streptococcal infection;
- Endocarditis;
- Arteritis.
Children at risk are:
- Having a weight at the time of birth of more than 4200 g;
- Premature (less than 37 weeks of intrauterine development);
- Suffering from malnutrition or dystrophy;
- Born with critically low body weight (500 g);
- Susceptible to injury;
- Children with low weight gain, chronic vitamin deficiencies, and micronutrient deficiencies.
Symptoms and signs of aneurysms by location
Aorta
Symptoms in newborns:
- Visible pulsation of the anterior abdominal wall;
- Crying, breast refusal;
- Insomnia;
- Dyspnea;
- Screaming during a massage of the abdomen or back;
- Lack of stool or urine;
- Pale skin;
- Coldness of hands and feet.
The clinic may simulate a picture of an acute abdomen or intestinal colic, accompanied by fever.
Symptoms of aortic aneurysm in children:
- Pulsation of the anterior abdominal wall;
- Exercise intolerance;
- Local or diffuse swelling of the lumbar region;
- Decreased amount of urine;
- Symptoms of compression of the mediastinal organs (pain when eating, cough, shortness of breath);
- Rapid heartbeat and shortness of breath at rest.
Aortic aneurysm is dangerous because it can occur without any symptoms at all. And the first signs can be noticed only when the dilated vessel begins to compress neighboring organs. We suggest you learn even more information about this dangerous disease:
- Stratification of this formation.
- Aneurysm of the aortic arch.
- Aneurysm of the ascending, descending and thoracic region.
- Abdominal aortic aneurysm and possible rupture.
Heart
In newborns, cardiac aneurysms are often combined with other congenital anomalies. In this case, the symptoms are determined by a heart defect. Clinic for isolated lesion:
- Cyanosis of lips, fingers, tip of nose;
- Drowsiness;
- Blueness and coldness of the skin;
- Rapid breathing;
- Slow weight gain;
- Breast refusal.
Aneurysms up to 3 mm have no clinical manifestations.
Symptoms in children and adolescents:
- Dyspnea-cyanotic syndrome;
- Tendency to faint;
- Weakness;
- Frequent heartbeat;
- Insomnia;
- Worsening of the condition when lying down and during physical activity;
- Pain and feeling of heaviness behind the sternum.
Brain vessels
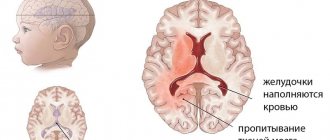
Clinic of cerebral aneurysm in newborns:
- Cry;
- Closing your eyes and throwing your head back (a sign of concomitant meningitis);
- Purple bluishness of the face and neck;
- Hydrocephalus (enlargement of the head due to the accumulation of cerebrospinal fluid).
Often there are no clinical manifestations.
Symptoms of cerebral aneurysm in children and adolescents:
- Headache;
- Dizziness;
- Tearfulness;
- Loss of consciousness;
- Throwing back the head;
- Rarely – strabismus, decreased vision and hearing.
You can read more about the classification, diagnosis and treatment of cerebral aneurysms in separate materials on the pages of our portal. There we will also talk about the causes and consequences of the rupture of such a formation and what a saccular aneurysm of a cerebral artery is.
Can an aneurysm be congenital?
Congenital aneurysms develop in 7-9% of cases. The reasons for the formation are the adverse effects of external and internal factors on the fetus’s body:
- Bad habits of the mother (alcoholism, smoking);
- Ionizing radiation;
- Intrauterine infections (rubella, fetal syphilis);
- Impact of external factors on the mother’s body (vibration, contact with metals, chemical compounds).
Most often (up to 80% of cases) congenital cardiac aneurysms are diagnosed, combined with other developmental defects.
Damage to cerebral vessels occurs in 3-5% of cases, aorta - 7-10%, peripheral and visceral arteries - in 1-3% of patients. Methods for confirming the diagnosis:
- Triple ultrasound of the fetus (in the 1st, 2nd and 3rd trimester; according to indications, the method can be used more often);
- Genetic counseling;
- Study of amniotic fluid and chorionic villi to identify genetic abnormalities.
Forecast
To prevent the disease from progressing to a more severe form, your baby should be regularly examined by a local pediatrician and cardiologist. It is also necessary to periodically do an ultrasound and perform an ECG. Such measures will allow you to monitor the dynamics of the disease and take timely actions to minimize possible complications.
In general, the prognosis for such an anomaly is favorable. The pathology does not affect the baby’s development and rarely causes discomfort. Aneurysm rupture is diagnosed in 10% of patients. Moreover, the survival rate after the operation is about 80%.
Many parents who are faced with this problem are concerned about their child’s attendance at physical education classes and sports clubs. Permission for this type of training must be given by a cardiologist. The specialist makes a decision based on the examination results, taking into account the size of the anomaly and accompanying changes in the functioning of the heart.
Prevention is relevant only at the time of planning and bearing a child. The expectant mother must monitor her health, undergo the necessary examinations and take appropriate tests to detect infections. This should be taken especially seriously by those who have relatives suffering from heart disease. During pregnancy, it is important to undergo fetal ultrasound several times. You also need to forget about bad habits such as smoking and drinking alcoholic beverages. In the first trimester, you should do everything possible to avoid infectious diseases (ARVI or influenza). To do this, it is important to eat right, take a walk every day, and minimize the time you spend in crowded places.
The following sources of information were used to prepare the material.
A protrusion of the septum separating the right and left atrium (where it is thinnest) by more than one centimeter is called an aneurysm, but in cardiological practice, smaller deformations are often also classified as a disease, especially if this causes negative manifestations. Curvature of the sac is not life-threatening, so it is classified as a minor cardiac anomaly. In most cases, patients are monitored dynamically, but some have to undergo surgical treatment.
Danger and possible consequences
Aneurysms larger than 5 mm are susceptible to rupture with profuse arterial bleeding. The complication is accompanied by ischemia of internal organs, collapse, shock and poses an immediate threat to life. Other complications:
- Thrombosis and thromboembolism;
- Intracerebral hemorrhage (including in the cerebral ventricle);
- Hydrocephalus;
- Fibrillation and flutter of the ventricles or atria.
Long-term consequences:
- Heart failure;
- Edema;
- Cardiac ischemia;
- Arrhythmia;
- Kidney failure;
- Decrease in intelligence;
- Violation of physical and intellectual development.
Disease detection
Aneurysm of the interatrial septum is most often diagnosed using ultrasound (ultrasound); specialists also use electrocardiography, computed tomography and nuclear magnetic resonance imaging. This disease can be diagnosed in newborns using ultrasound examination of the heart, but a definitive diagnosis is made only in case of differential examination of the foramen ovale in the interventricular septum.
Computed tomography in the case of diagnosing an aneurysm of the interventricular septum allows one to be informed regarding the current size and location of the protrusion in the area of thinned tissues.
Doctors prescribe a subsequent heart examination if there are suspicions of other possible heart diseases and pathologies.
In adult patients, an atrial septal aneurysm forms after a heart attack. In this regard, pathology is divided into the types listed below.
It is detected 3-6 weeks after a heart attack. Develops due to improper formation of a scar in the area of infarction. This type of aneurysm is manifested by shortness of breath, increased fatigue, and increased heart rate.
Diagnostics
The diagnosis is confirmed using objective and instrumental examination:
- Questioning and inspection are rarely effective . Children complain of pain, weakness, dizziness. The child’s parents may indicate tearfulness and the connection of complaints with body position and food intake.
- Objective examination . Pathological pulsation, swelling and tension of the skin over the projection of the aneurysm, enlargement of the head, and local pulsating protrusion in the lesion are detected.
- X-ray data - an increase in the cardiac shadow, pallor or abrasion of the roots of the lungs, smoothing of the cardiac arches.
- ECG – displacement of the cardiac axis, signs of ischemia (ST segment displacement, deep T wave), arrhythmias. X-rays and ECGs are effective in diagnosing cardiac aneurysms.
- Ultrasound . The method is effective for identifying aneurysms of any location except intracranial. The pathology is represented by a saccular pulsating expansion associated with the vascular wall.
- Angiography is a method of confirming the diagnosis at any location. Angiography involves contouring the walls of blood vessels by injecting inert dyes into the blood. Angiograms reveal a local protrusion associated with the vascular wall.
- CT and MRI are effective for detecting cerebral aneurysms, allowing one to differentiate pathology from tumors and cysts, and diagnose local tissue edema and hydrocephalus.
You will find all the detailed information about vascular diagnostics in a separate material.
What it is?
Aneurysm of the interatrial septum is a dangerous pathology that can lead to rapid death.
That is why a child who has been diagnosed with a disease must be constantly monitored by a cardiologist. After the patient reaches the age of 1 year, the pathology is eliminated surgically. Atrial septal aneurysm is a minor cardiac anomaly. This pathology causes a change in the structure of the walls of a large vessel, against which a protrusion of a separate section of the heart is formed. Protrusion is observed from the right or left atrium.
Medicine has not yet established the exact causes of the disease. One of the main assumptions regarding the development of this abnormality in the functioning of the heart is the incorrect formation of connective tissues in a child during its intrauterine development, caused by infection. In addition to this version, doctors do not exclude a hereditary factor in the transmission of the disease.
Aneurysm of the interatrial septum in children almost never causes heart failure. This is due to the fact that during the disease there are no serious disruptions in the blood supply system through the heart arteries. The aneurysm is connected to the left ventricle of the heart via a small muscular reservoir. That is why there are no visual disturbances in the child’s condition, he does not experience pain or discomfort.
But over time, the pathological protrusion becomes thinner and can lead to rupture. Exacerbation of the situation can be provoked by heavy physical activity, poor nutrition, and stressful situations. After a rupture of an aneurysm of the interatrial septum, heart failure occurs, which leads to the death of the child.
The disease can manifest itself as follows:
- Pathological pulsation in the third intercostal space. If you listen to a child in a supine position, the pulsation will resemble the sound of a rocking wave. You can determine it even without listening. By feeling the heart area with your fingers, you can detect pathological tremors caused by an aneurysm in a small patient.
- Parietal blood clots that occur as a result of impaired blood circulation. Their formation leads to the disappearance of pathological pulsation.
- Heart rhythm disturbances. This manifestation is most often observed in adolescents who actively engage in sports or lead an unhealthy lifestyle, smoking and drinking alcohol.
Currently, there are three forms of aneurysm. The most common is represented by protrusion of the vessel wall from the left to the right atrium. The second form of pathology is less common and manifests itself in the form of bulging walls from right to left. The third has an S-shape.
Choice of treatment tactics
Therapy can be conservative and surgical. Indications for a particular method are determined individually for each child.
General indications for conservative treatment:
- Neonatal period and infancy (up to 1 year);
- No complaints;
- Infectious diseases;
- Exacerbation of chronic diseases;
- Satisfactory general condition;
- Signs of calcification according to ultrasound and CT.
Drug therapy:
- Antihypertensive drugs;
- Beta blockers;
- Multivitamin complexes;
- Cardioprotectors;
- Symptomatic remedies.
Other methods of conservative therapy:
- Physiotherapy;
- Mud and hydrotherapy;
- Electrophoresis of vitamins, antioxidants;
- Spa treatment.
General indications for surgical treatment:
- Medium, large and giant aneurysms;
- Deterioration of general condition;
- Pain syndrome;
- Frequent loss of consciousness and constant shortness of breath;
- Swelling of the legs and enlargement of the abdomen;
- Arterial hypotension;
- Threat of rupture and bleeding;
- Pulmonary hypertension.
If there is a threat of rupture, surgery is indicated for children regardless of age.
Surgical intervention is aimed at eliminating the protrusion and restoring the integrity of the vessel. Types of operations:
- Clipping;
- Vessel resection;
- Suturing the vascular wall.
Heart operations are often accompanied by the elimination of concomitant congenital defects.
Therapy
Before treating a child, he must undergo certain diagnostic procedures:
- Auscultation is listening to the heart using a stethoscope. This device will allow you to hear noises if there is a possibility of an anomaly;
- ECG. Performed to check the functioning of the heart, it makes it possible to identify rhythm disturbances;
- Ultrasound. This diagnostic method is safe and quite informative. It allows you to detect bulging of the interatrial septum, as well as determine fluctuations in the cardiac cycle.
Treatment depends on the growth rate and increase in the size of the formation. As the disease progresses, the patient is indicated for surgical intervention, which involves replacing the damaged area of the vessel with an artificial graft.
Small aneurysms rarely lead to rupture of a heart vessel, so they can be treated with medications. Drug therapy includes antihypertensive drugs, which are also used to stabilize blood pressure. Therapeutic measures should be aimed at normalizing the functioning of the heart muscle, adjusting the rhythm, and improving metabolic processes in the myocardium.
Treatment is not complete without magnesium supplements. The role of this microelement in the formation of collagen fibers is difficult to overestimate. Magnesium has an antiarrhythmic effect, promotes contraction and relaxation of heart cells. That is why it is included in complex therapy for rhythm disturbances.
Treatment with magnesium preparations consists of taking Magnerot three times at a dosage of 0.5 g at a time. The duration of such therapy is 1 week. After this, take 25 g of this drug for 5 weeks. The use of Magne B6 is also required. The course of treatment is 1.5-2 months. The dosage depends on the child’s weight.
For antioxidant protection and membrane-stabilizing effect, L-carnitine, Cyto-Mac, and Coenzyme Q10 are used. Metabolic therapy can last about 1.5 months. Moreover, it must be repeated several times a year, as a rule, two or three are enough.
To improve metabolism, it is recommended to take PP and B vitamins. Vitamin therapy is carried out over a two-month course, repeated up to 3 times a year.
It is also possible to use beta blockers, glycosides and anticoagulants. The former help reduce heart rate. Glycosides and anticoagulants can be prescribed at the preoperative stage.
Additionally, you should adhere to non-drug treatment, the essence of which is as follows:
- It is necessary to properly organize the child’s daily routine, ensure normal sleep, walks in the fresh air, and proper rest.
- Particular attention should be paid to the baby’s nutrition; it should be balanced and as healthy as possible.
- It will be useful to carry out hydrotherapy or balneotherapy.
- Different types of massage have a very good effect.
- Physiotherapy will also be beneficial, especially if we are talking about electrophoresis using magnesium.
Small aneurysms can be treated with folk remedies. But they should only be used under the supervision of a physician. Under no circumstances should you conduct experiments on your own, especially if the pathological formation has reached a large size.
https://www.youtube.com/watch?v=cosamomglavnom
Among traditional medicine recipes, a collection of herbs such as rose hips, valerian officinalis, hawthorn and calamus has proven itself to be excellent. To prepare the product you need to take 1 tbsp. spoon of each component, and pour boiling water (0.5 l) over the raw materials. After the infusion has stood for 2-3 hours, it is filtered and 1 teaspoon of the decoction is diluted in a glass of water. Treatment is carried out three times a day.
False aneurysms in children
False aneurysms develop extremely rarely in children (less than 1% of cases) .
The formation is represented by an accumulation of blood limited to scar tissue or the pericardium (if localized in the heart). False aneurysms are of traumatic origin (open wounds, rib fractures, falls from great heights, concussions and brain contusions). Characterized by rapid calcification.
The clinical picture is often absent. With large sizes, the following symptoms are observed:
- Pain;
- Tension and bluishness of the skin over the protrusion (with a superficial location);
- When localized in the brain - headaches, hydrocephalus.
The danger of the disease lies in the possibility of thromboembolism and rupture.
The diagnostic algorithm is the same as for true forms. For small sizes (up to 5 mm), dynamic observation is carried out; for large sizes, excision and suturing of the vessel (heart) wall are performed.
We wrote in more detail about false and true aneurysms in another article.
Practical recommendations for parents
Observation and care of a sick child include:
- Exclusion of professional sports and injuries;
- Attentive attitude to complaints and general condition;
- Prevention of infectious diseases common to children (meningococcal, adenovirus infections, chickenpox, measles, scarlet fever);
- Determination of feasible physical activity (walking, swimming, gymnastics);
- Periodic observation by a cardiologist, pediatrician, surgeon;
- Monitoring the dynamics of the process (ultrasound, MRI).
Aneurysms in children are a rare cardiovascular pathology of a congenital or acquired nature. The disease is most typical for children who have experienced intrauterine infection, trauma, or infectious myocarditis. Early detection and rational treatment of pathology can prevent possible complications. Prevention is based on proper management of pregnancy and childbirth, careful attention to the health of the child and medical examinations.