Features of injury
If a closed injury occurs in the area of the left side of the chest, then the possibility of heart contusion cannot be ruled out. This problem has such features that it is not always possible to guess about it; cardiac contusion is determined by examination. It occurs as a result of the application of mechanical force to the chest, which is transmitted to the heart.
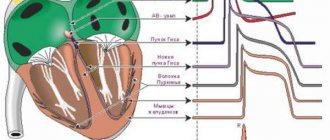
The heart is an organ in which there is a continuous circulation of blood flows, coordinated operation of the valves, and a functioning conduction system that transmits impulses from pacemakers to the chambers. The consequences of a traumatic blow depend on:
- from the force of this action,
- what phase of heart activity was at that moment,
- direction of impact.
The disease code according to the international classification scale (ICD-10) is designated S26 (heart injury).
In some chambers, movement may be slowed down or even stopped during a sudden mechanical impact. During this time, blood flow continues to the heart. The blood in the chambers of the heart responds to a sudden impact with a hydrodynamic phenomenon, which can create a danger to the health of the heart.
The following reactions to impact are possible:
- overcrowding of cells,
- their overload
- stretching of cavities and changing their sizes,
- compression of departments,
- damage to the heart by the ribs,
- blood flow dissociation,
- heart displacement,
- sharp functional disorders can provoke mechanical damage to the heart: myocardial damage,
- valve damage.
Spasm of coronary vessels and organ bruise - differences
The clinical picture of the bruise resembles a heart spasm (suddenly occurring coronary insufficiency). Treatment of pathologies is different, so differential diagnosis is necessary. Reliable results are provided by diagnosis, but before it is carried out, a drug test can be carried out - nitroglycerin reduces or completely relieves pain during spasm of the coronary vessels, whereas in case of a bruise, the painful sensations do not go away.
It is also necessary to find out from the patient the entire history of the disease. If in the days preceding the deterioration of health there were blows to the chest, then only a doctor can rule out a bruise.
Classification and forms
Experts identify two types of clinical manifestations that can be caused by a blow to the heart:
- angina pectoris,
- infarct-like.
Determining which clinical type the symptoms of a particular patient can be attributed to immediately gives a hint about treatment tactics. To exclude the possibility of developing heart failure in a heart attack-like case of contusion, the amount of therapy performed by infusion is limited. In the first case, such a restriction is not provided.
Heart contusion can be divided into components:
- contusion of the heart muscles,
- contusion of coronary vessels,
- bruised valves
- combined bruise.
What it is
A contusion of the heart muscle occurs when there is intense impact on the human chest. Such an injury is classified as closed, so the victim may not always suspect the presence of any violations. In many cases, over time, symptoms develop that indicate the presence of negative changes in the functioning of the cardiovascular system.
With a minor injury, undesirable consequences may not be observed at all, and the human body recovers on its own without external intervention.
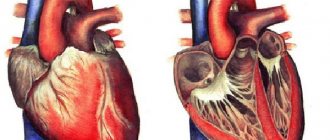
Depending on the damaged area of the heart, the classification of such injuries includes the following diagnoses:
- Traumatization of valves. It is characterized by lightning-fast development of negative symptoms; a common consequence is pulmonary edema, which threatens the patient’s life.
- Concomitant damage to the coronary vessels. In especially severe cases, detachment of the inner layer of the arteries occurs, thrombosis, and myocardial infarction.
- Myocardial contusion. One of the most dangerous injuries, which is explained by the development of negative symptoms only after some time. After myocardial damage, the conduction system of the heart is disrupted, which leads to changes in metabolic processes in tissues.
- Combined bruise. Combines signs of injury to different parts of the cardiovascular system. Most often it is severe and requires special treatment.
In accordance with the developing symptoms, heart contusions are usually divided into two large groups:
- Angina pectoris. They are accompanied by minimal pain, complications are rare, treatment is easy and does not take much time.
- Heart attack-like. Such bruises occur after a strong blow and are accompanied by severe pain and increased body temperature. They require special treatment due to the high risk of developing heart failure.
Causes
A cardiac contusion can occur if there is a blow to the chest in the area where the heart is projected. This action is possible:
- in case of an accident: falling from a height,
- shock wave,
- in an emergency - hitting the steering wheel with your chest;
- in production - when working with heavy objects, when a tool kicks back or another unforeseen situation occurs;
- hydrotrauma,
- hit with a stone
- kicking the ball in a football game,
Next, we will talk to you about the symptoms and treatment of heart contusion.
Diseases as consequences of a constantly high heart rate
A pulse of 70 beats per minute is absolutely normal for any person. But having the ability to constantly and quickly rise is not the norm. It is likely that you have a genetic or acquired heart disease. The most terrible and common disease is ischemic syndrome. It affects the functioning of the thyroid gland and heart rate. Common diseases in which the pulse actively increases include:
- Tachycardia. A sharp increase in heart rate contractions, from 90 beats and above.
- Hypertension. Increased blood pressure from 140 to 90 and above.
- Hyperthyroidism. Hormonal disease of the thyroid gland, in which the pulse quickens.
Symptoms
Heart contusion can manifest itself with the following symptoms:
- interruptions in cardiac activity,
- pain in the chest area,
- heartbeat,
- shortness of breath, in some cases suffocation;
- arrhythmias,
- cyanosis,
- pain similar to angina pectoris;
- expanding the boundaries of the heart,
- the pain factor manifests itself either immediately after the injury or several hours later;
- the appearance of uncharacteristic noises, dull tones are heard;
- decrease in blood pressure over the course of a week,
- if there is a violation of the papillary muscle, for example, its rupture, then a rough systolic murmur will be heard;
- loss of consciousness,
- with serious damage to the heart from a stroke, heart failure with congestion may develop.
Violations may occur:
- thrombosis of cardiac vessels,
- spasm of the coronary arteries,
- hemorrhages in the muscles of the heart,
- rhythm disturbances,
- myocardial infarction,
- for minor injuries: microhemorrhages, hematomas;
- when a traumatic blow of great force is possible: ruptures of valve elements,
- damage to the heart muscles.
There may be signs:
- cold sweat,
- anxiety,
- loss of mind,
- swelling in the heart area,
- causeless horror
- tingling feeling in the fingertips,
- pulsation of large veins.
We will tell you further about ECG and other methods for diagnosing cardiac contusion.
Prevention
To avoid heart contusion, it is necessary to prevent injury to the chest by any means.
This can be done by following simple rules:
- Drivers and passengers must always wear seat belts while driving vehicles..
- When performing installation work at height, builders are required to use special insurance, which prevents them from falling.
- During active sports, it is necessary to protect the heart area from shock.
Diagnostics
The specialist listens to complaints and uses a stethoscope to dry the heart. To clarify, do research:
- An electrocardiogram reflects the electrical impulses of the heart. If the results of this method show a normal result, then you can be sure that there are no serious negative consequences of the bruise.
- Echocardiography is indicated in cases where there are signs of hemodynamic compromise. In situations of bruise, transesophageal examination is used.
- Holter observation – recording of heart impulses throughout the day. Makes it possible to understand what factors are associated with possible deviations from normal readings. The patient wears a portable sensor attached to the body and keeps a chronological record of activities, loads, and mood.
- Laboratory research. Conduct tests for the content of substances that may indicate that the myocardium is damaged: MB isoenzyme,
- troponin.
Diagnosis
The doctor makes a diagnosis based on the medical history, the victim’s complaints, palpation and listens to the work of the heart. If the doctor has doubts about the prescription of treatment, then an additional examination is prescribed:
- An EEG shows the electrical signals of the heart. If the result is positive and the normative indicators are normal, the absence of a bruise and complications after it is diagnosed.
- Echocardiography is used in cases of suspected blood flow abnormalities.
- Holter monitoring – recording the dynamics of the heart rhythm for 24 hours. The method assumes the ability to understand what causes errors in standard indicators. An autonomous device is attached to the patient’s body, which records changes in indicators during exercise over a daily period of time.
- clinical researches. An analysis is performed indicating myocardial damage.
Treatment
To provide assistance to a patient with a heart contusion, he is admitted to a hospital. Treatment takes place in intensive care units, unless urgent surgery is required. The treatment program is carried out under close monitoring of changes in the patient's condition.
Therapeutic
If necessary, the following activities are carried out:
- to restore the ability of the myocardium to contract,
- treatment of hemodynamic disorders,
- antiarrhythmic therapy,
- improvement of metabolism,
- rehabilitation measures.
Medication
Depending on what disorders occurred as a result of the injury, specialists may prescribe:
- drugs that relieve heart pain, these can be: droperidol (with saline solution),
- fentanyl (with saline solution),
- omnopod,
- morphine,
- isoptin,
- diuretics,
Operation
- If mechanical damage to the walls or valve elements occurs in the heart, the patient will need urgent surgical assistance.
- In case of transverse blockade (complete), measures are taken for electrical cardiac stimulation.
Folk remedies
For bruises, traditional methods are successfully used. A heart bruise can pose serious threats, so self-medication is unacceptable.
With the permission of a specialist, you can use:
- Cold and rest help the bruised area.
- Applying plantain helps relieve the effects of a bruise.
- The same thing, only crushed wormwood is applied.
- Make a solution with laundry soap, apply a bandage soaked in this solution to the bruise.
The following video will tell you about the potato method of folk treatment for heart contusion:
First aid
To avoid the serious consequences of a heart contusion, it is important to competently provide assistance to the injured person. Before providing assistance, it is important:
- assess whether the patient is breathing and with what frequency of inhalation and exhalation;
- determine whether the victim is conscious;
- check vital signs, including blood oxygen levels;
- examine the injured area;
- determine what complaints the patient has.
First aid for heart injury includes:
- open the windows to allow enough air to flow in;
- pay attention to the state of cardiac function;
- place the victim in a horizontal position to make it easier for the person to breathe;
- remove clothing from the person that is constricting the chest area;
- do not disturb the victim and ensure peace;
- turn the person's head to the side to prevent asphyxia;
- soak a cotton pad with ammonia and bring it to your nose if the person has lost consciousness;
- talk to minimize fear;
- do not give the patient anything to drink.
After this, the person is given painkillers, anticoagulants, and antiarrhythmics. Then wait for the ambulance to arrive.
Complications and consequences of heart contusion
A heart bruise is a severe stress for the body. This causes a significant blow to various systems. The consequence of injury may be symptoms of post-traumatic myocardial dystrophy.
After a bruise, the following complications may occur:
- ventricular fibrillation,
- atrial fibrillation,
- extrasystole,
- atrial flutter,
- ventricular tachycardia,
- paroxysmal tachycardia,
- conduction disturbance – atrioventricular block (complete or incomplete);
- rhythm disturbances can occur of several types at the same time.
Read last about the prognosis for blunt cardiac trauma.
Structure of the heart
The heart is a hollow muscular organ consisting of 4 sections - 2 ventricles and 2 atria. The main function is “pumping”. The 4 valves of the heart muscle are necessary to ensure normal blood flow. There is an autonomous system for conducting impulses through cardiomyocytes - the muscle itself sets the strength and frequency of contractions. This is a living pump with a complex “electrical circuit” inside. Any mechanical impact may cause malfunction.
Forecast
If the blow was of small force, then the activity of the heart will return to normal after some time. Experts may determine that treatment may not be necessary.
Often, when a serious injury occurs, it is the heart contusion that causes death, although it may be undetected. This situation occurs in three-quarters of fatal injuries . After treatment in a hospital, when surgical intervention was required, if there was circulatory arrest, the probability of death is high, up to 88%.
Is heart rate 84 normal or too much?
The normal human heart rate ranges from 60 to 90 beats at rest. But for many people a heart rate of 81 is normal, for others it is not. And if your blood pressure readings begin to rise sharply, first of all, don’t be alarmed. A high pulse is not always the cause of serious illnesses. Various factors could have influenced its rise:
- Stress.
- Fright.
- Temperature.
- Lots of physical activity during the day.
- Drinking alcohol or energy drinks.
What should you do if your normal heart rate is 60-70 beats, but has now begun to actively increase:
- Start breathing deeply while sitting or lying down. Deep breathing can bring a person to a calmer state. Ease the speed of strikes.
- Lie on your back and close your eyes. This will make it possible for the body to understand that no physical activity should be expected.
- Wash yourself. Cold water also helps calm internal processes.
- Call your GP for advice if the steps above do not help. Your doctor will be able to advise you on medications that will lower your blood pressure.
- Try taking anti-anxiety medications. They can cause weakness and drowsiness, so after taking them, go to rest.
Strong heartbeats in endocrinology
Inflammation or pathology of the thyroid gland disrupts the balance of hormones necessary to maintain processes in the body. A characteristic symptom is strong heartbeats at rest. When a hormonal imbalance occurs, a person notes:
- increased sweating;
- fatigue;
- forgetfulness;
- depression;
- weight gain;
- skin rashes, sagging and dryness.
With hypothyroidism, arrhythmia appears, the heart beats faster. A person cannot work fully, play sports, or devote time to family. Treatment consists of normalizing hormonal levels and stopping the cause of the disease. The endocrinologist selects artificial analogues of hormones in the required volume. When taken for a long time, they help level out the condition and normalize well-being.
Chest bruise: first aid, treatment, consequences | mrikrnts.rf
In medical practice, bruises are common occurrences. The vast majority of injuries occur to the extremities, but cases of chest contusion are not so common.
The danger of injury is that internal organs may be bruised. In this case, injuries that are incompatible with life occur. But dangerous injuries account for a small percentage of bruises.
Such injuries are common in road accidents and natural disasters.
Trauma code according to ICD 10
Superficial cell damage in adults is indicated by the ICD 10 code - S20.2. Frequently encountered injuries are bruises of the anterior chest wall; they are assigned code S20.3.
A separate group of injuries according to the international classification includes superficial injuries of the mammary gland - S20.0 and S20.1.
In case of contusion of the soft tissues of the chest of an unspecified nature, according to ICD 10, codes S20.7 and S20.8 are assigned.
Causes
Chest contusions occur in 10% of all injuries. This is a small percentage of injuries, but such injuries are often accompanied by serious complications and therefore require increased attention.
Most blows to the sternum occur as a result of accidents. In such a situation, there are usually other injuries: dislocations, fractures, hemorrhages.
If the hands were in motion during the impact, then joint deformations are possible.
The causes of a bruise can be:
- fights - random attacks or unsuccessful training with a sparring partner,
- falls from a height - if a person falls from a height of height, then the injury caused by a bruise is minimal; a blow to the surface of the earth from a great height can cause instant death,
- sports – cyclists are more likely to experience sternum injuries when they hit the handlebars.
The danger is posed by compression injury, which can lead to poor circulation and rupture of organs. Chest trauma in children most often occurs due to a fall.
If the baby falls off the horizontal bar or falls down the stairs, bone tissue may be damaged as a result of the injury. In children, injuries are usually associated with negligence.
Minor bruises do not cause concern, but strong blows to the sternum provoke other health problems, mainly from the lungs and heart.
In women, the mammary glands may be injured as a result of the blow. After consulting a traumatologist, it is necessary to be examined by a mammologist to avoid complications.
First aid
A fracture of the sternum may be hidden under the bruise, so all medical procedures are carried out with caution. A bruise of the chest on the left, where the heart is located, is especially dangerous.
To prevent swelling and spread of hemorrhage, apply a pressure bandage. Cold helps relieve pain and swelling. First aid for a chest injury should be provided immediately after the injury.
There is no delay in calling a doctor, and before the ambulance arrives, the patient is offered painkillers - analgesics.
If the pleura of the lungs is damaged, breathing problems arise, even stopping. The victim needs to clear his mouth of mucus and foreign elements and pull out his tongue. Damage to the lungs and pleura is the most dangerous, and any delay is fraught with irreversible consequences. If breathing stops, artificial ventilation is performed.
A blow to the sternum can cause penetrating injuries. In the case of a closed injury to the chest organs, a contusion of the heart is possible - this type of injury often becomes fatal.
Less dramatic is the contusion of the chest on the right. But even with such a wound, anesthesia and cooling are immediately carried out and the victim is taken to the hospital.
What to do if you are injured
What to do at home if you have a chest contusion? For severe pain, non-narcotic analgesics are given. Painkillers are offered in a standard dose, usually an analgin tablet is given.
What to do if organs are compressed due to a chest bruise? In this case, the patient is not offered food or drink, as vomiting may occur. Unbutton clothes and provide fresh air.
How to treat a bruise
At home, treatment of a chest contusion involves the use of pharmaceutical tinctures. For medicinal purposes, tinctures of violet, wild rosemary, and birch buds are indicated. They are used for compresses, which are made at night for 10-14 days.
Compresses and physiotherapy are considered the main methods of treatment after discharge. It will be possible to cure the consequences of injury much faster using folk remedies. So, in case of light damage, it is useful to take equal proportions of alder, hemlock and St. John's wort bark. For 500 ml of vodka take 60 g of raw materials.
Leave for 3 days. The resulting composition is used for compresses daily.
Heparin ointment will ease the condition. It normalizes capillary blood circulation, but it is also not used in the heart area. Your therapist will provide more detailed information on how to treat a bruise at home.
After an injury, it is recommended to sleep on a hard surface exclusively on your back. If complications arise, the specialist asks in what position the patient is resting. “Yes, I sleep mostly on my back,” patients say, but by “mostly” they mean “as needed.” Quite often, it is failure to comply with doctor’s instructions that leads to complications of injury.
Rehabilitation
In case of chest contusion, it is recommended to undergo a course of medicinal electrophoresis and magnetic therapy. All possible loads are permissible only a month after the incident. If the general condition is good, exercise therapy and breathing exercises are indicated. They can be started after 2-3 weeks, but only in case of uncomplicated damage.
Breathing exercises include:
- blowing up balloons,
- inhale for 4 counts, exhale for 8 counts,
- exhaling with resistance, making the sound “sh-sh-sh”.
All exercises are performed without discomfort or pain. During the rehabilitation period, they try to avoid sudden movements, but there should be no stagnation at the site of injury, so adequate gymnastics will be beneficial.
Complications and consequences
A severe chest contusion implies lung damage. Possible complications of such an injury include hemothorax and pneumothorax.
Serious disorders occur due to the formation of air cavities in the subcutaneous tissue. Due to chest trauma, which leads to rupture of intercostal vessels and damage to lung tissue, subcutaneous emphysema develops.
In case of such complications, cardiac activity worsens and anemia develops.
It will be possible to prevent negative consequences if the victim is delivered to a medical aid station in a timely manner. Chest trauma remains one of the most dangerous disorders requiring emergency medical intervention.
(2 5,00 of 5) Loading...
Source: https://xn--h1aeegmc7b.xn--p1ai/pervaya-pomoshh/ushibyi/ushib-grudnoy-kletki
How to measure
The traditional method of measuring pulse is to place two fingers on a person's neck or wrist. It is worth understanding that for various problems, the pulse can appear in unexpected and varied places. So, if a person has aortic valve insufficiency - this is a situation when the valve leaflets do not close completely - the pulse can be viewed through the pupils of the eyes. If there are problems with blood vessels, if there is a failure in the communication between veins and arteries, the veins may pulsate. If blood pressure increases, you can feel the pulse in the abdomen.
You can also feel the pulse in the foot, groin, armpit and forearm. Learning to feel your pulse yourself is not that difficult. This can help save a person’s life, because you can describe to the doctor the strength and speed of heart contractions even at the stage of calling an ambulance. Naturally, if a person has problems with the pulse, he should not expect that the problem will solve itself, and there is also no need to practice self-medication. In such a situation, you should consult a doctor as soon as possible to determine the source of the problem and cope with the situation.
| Person's age | Average heart rate (beats per minute) | Minimum allowable heart rate (beats per minute) | Maximum allowable heart rate (beats per minute) |
| Newborn babies up to 1 month of age | 140 | 110 | 170 |
| Children from 1 month to one year | 132 | 102 | 162 |
| Children 1-2 years old | 124 | 94 | 154 |
| Children 4-6 years old | 106 | 86 | 126 |
| Children 6-8 years old | 98 | 78 | 118 |
| Children 8-10 years old | 88 | 68 | 108 |
| Children 10-12 years old | 80 | 60 | 100 |
| Teenagers 12-15 years old | 75 | 55 | 95 |
| 15-50 years | 70 | 60 | 80 |
| 50-60 years | 74 | 64 | 84 |
| 60-80 years | 79 | 69 | 89 |
prokrasotu.info
Hello, Mikhail Valentinovich! Thank you very much for the consultation!
Mikhail Valentinovich, I’m at a dead end... I went through many tests, MRI of the brain and MRI of the cervical spine, X-rays of the spine, twice Holter ECG monitoring (I do all the tests in private clinics, there is no possibility in the clinic) - there are no diagnoses and no treatment...
For the second time in 2 years I am undergoing Holter ECG monitoring, but there are attacks (increased heartbeat (intermittent), dizziness, compression in the heart and thyroid gland, increased blood pressure, feeling of lack of air, cold sweat, during the day - unsteadiness when walking and weakness in the legs ) cannot be caught. These attacks happen 2-3 times a month (maybe during the day, maybe at night, unexpectedly).
Monitoring was carried out by Holter SDM3 (3-channel, with 3 leads) - this is the best that is available in our regional center in private clinics. And the interpretation of the monitoring is different... What are the characteristics of this Holter ECG model? What are "unusable QRS"? Does Holter SDM3 determine the nature of arrhythmia?
For the second time, Holter monitoring reveals “During the day, regardless of the frequency of sinus rhythm, the different amplitudes and polymorphism of the T wave are recorded. Against the background of sinus tachycardia, ST segment depression of 0.5-1 mm is recorded.” Is this ischemia? Or is it related to long-standing persistent hypertension?
Previously, my thyroid hormone T4 sometimes increased. In 2004, T4 was elevated = 16.3 dl/ml (normal 4.2 - 12.0 dl/ml) - taken to the endocrinology clinic. Anaprilin and several other dietary supplements were prescribed (the diagnosis was not indicated on the card... all prescriptions were written on pieces of paper). Then I took Mercazolil (maintenance dosage), but I cannot tolerate a higher dosage due to severe dizziness and unsteadiness when walking. In 2006 (after taking medications) I took a test at a private medical facility. center: T4 is normal, although the symptoms of hyperthyroidism remain (accelerated heartbeat, increased blood pressure, a feeling of compression in the heart and in the thyroid gland (diffuse goiter), emotionality, increased sweating, shine in the eyes, gastrointestinal disorders). These symptoms have accompanied me from the age of 22 until today (I am now 46). With the advent of menopause, the symptoms doubled. In 2020, she took tests for thyroid hormones + parathyroid hormone (surprisingly, T4 was normal, but parathyroid hormone was elevated (?)): 07/04/2015 thyroid hormones: free T4 (FT4) - 15.02 pmol/l (normal 9.0 - 20.0 pmol/l); Free T3 (FT3) - 4.42 pmol/l (normal 4 - 8.3 pmol/l); antibodies to thyropyroxidase - 6.5 lU/ml (normal up to 50 lU/ml); TSH - 1.63 mIU/ml (normal 0.25 - 5.0 mIU/ml) December 7, 2015 (parathyroid hormone - elevated) - 74.8 pg/ml (normal 15.0 - 65.0 pg/ml) (!)
Why, despite normal T4 levels, do I still have symptoms accompanying hyperthyroidism? Can continuous use of beta blockers (since 2001) affect the result of a thyroid hormone test? What could be associated with such a symptom as lack of air (the feeling that breathing and heartbeat are out of tune) - with hypertension or ischemia? Compressive pain in the heart area (no more than 15 minutes) what can be associated with? Is it from high blood pressure, from an accelerated heartbeat, or ischemia? I used Nitroglycerin a couple of times, it was easier, but a severe headache appeared... The clinic told me to be careful, not to experiment, because of the presence of cerebrovascular insufficiency in the IVB...
How to take Bisoprolol correctly according to Holter ECG data (I publish the data from the previous consultation below)? I have been taking Lozap 50 since 2010, and for more than 6 months now I have been coughing (especially if I rest my back against the back of a chair) - could this be related to taking Lozap, or something else? Do I need to be tested for lipoproteins in fractions? What laboratory tests should I undergo?
I would be grateful for your advice!
PREVIOUS CONSULTATION: October 17, 2020 Natalya asks: Good afternoon! Please advise based on Holter data in combination with symptoms and other examination data. Woman 46 years old. There are attacks: increased heartbeat (intermittently), dizziness, compression in the heart area, increased blood pressure, feeling of lack of air, cold sweat, during the day - unsteadiness when walking. I take it with Bisoprolol. I also take Lozap 50 (hypertensive treatment, level 2), but it causes a cough. What can be replaced? Sometimes the legs and feet swell (mainly in the summer). What is this connected with? In September, I underwent Holter ECG monitoring (Holter was installed at home; there were no pronounced attacks of palpitations; I performed a moderate exercise, which can be performed if coordination is impaired; the following symptoms were noted - at times, imbalance and short-term (but frequent) dizziness, a feeling of pressure in the heart area, persistent increase in blood pressure (after physical activity there is a sharp increase in blood pressure), a feeling of lack of air, unsteadiness when walking (after moderate physical activity) and loss of coordination).
Data from Holter ECG monitoring on September 12-13, 2016: Average heart rate 80/min. Sleep 6 hours 50 minutes Heart rate during sleep is 69/min., while awake 85/min. Circadian index 1.24. Rhythm: Tachycardia >110 00:28:07 maximum heart rate 125/min. (09/12/16 21:51:51) Arrhythmia 00:00:17 Bradycardia (QRS: total 102330, ventricular (V) 234, supraventricular (S) 481, unfit (A) 462. Minimum RR 200 (09/13/16 02: 50:54) Minimum RR(NN) 232 (09/13/16 10:24:38) Maximum RR 2317 (09/13/16 02:02:35) Maximum RR(NN) 1190 09/13/16 10:55:51) During 24-hour monitoring records sinus rhythm with a frequency of 60 at night, during the day up to 64 to 112 beats. per minute The tendency of sinus rhythm to normosystole during the day, insufficient decrease in frequency at night, with a moderate increase in rhythm frequency during physical and emotional stress. In the evening, rare single atrial extrasystoles were recorded, and at night, rare single ventricular extrasystoles occurred. Throughout the day, regardless of the frequency of sinus rhythm, the different amplitudes and polymorphism of the T wave are recorded. Against the background of sinus tachycardia, ST segment depression of 0.5-1 mm is recorded.
The Holter monitoring report is accompanied by 8-page cardiograms.
I didn’t even suspect that I could have a pulse below 60 beats/min. (perhaps this is due to the rather long-term use of beta blockers)… Maximum heart rate 125 beats/min. It was precisely in a state of rest - while watching TV. Now I don’t know how to take Bisoprolol, because there can be both tachycardia (more than 120 beats/min) and 56 beats/min. Therefore, I decided to take Bisoprolol in emergency cases...
And this Holter shows the same thing: “During the day, regardless of the frequency of sinus rhythm, the different amplitudes and polymorphism of the T wave are recorded. Against the background of sinus tachycardia, ST segment depression of 0.5-1 mm is recorded.” Is this ischemia? Or is it related to long-standing hypertension? Or with concomitant diseases: tendency to hypocalcemia; insufficiency of cerebral circulation in the VBB against the background of osteochondrosis of the cervical (4 protrusions, deforming arthrosis, straightened lordosis, osteophytes, dehydration) and thoracic (except for osteochondrosis and osteophytes, deformation of the Th8 vertebral body (probably due to hypocalcemia)) parts of the spine. Previously, the T4 hormone sometimes increased (the thyroid gland is enlarged), but now the cardiac, stomach, and neurological symptoms are the same (weight is normal), and the T4 hormone is normal. Can chronic long-term use of beta blockers “mask” the test result? Do beta blockers reduce metabolism? In addition, on MRI of the brain: Ventricular system - moderate deformation of the anterior horns of the sides of the bodies S = 4.7 mm, D = 4.2 mm. Brain substance: Pronounced focal changes in both hemispheres are detected, expressed somewhat more subcortically. There is a slight deformation of the corpus callosum. Convexital subarachnoid spaces are slightly expanded in the projection of the poles of the heights of the lobes. On MR angiograms (without IV contrast enhancement): ICA on the right = 3.6 mm, on the left = 3.5 mm; vertebral artery right = 2.2 mm, left = 2.2 mm, basilar artery = 2.5 mm. Uneven narrowing (spasm) of the branches of the SMA.
What are the above symptoms associated with (increased heartbeat (intermittently), dizziness, compression in the heart area, increased blood pressure, feeling of lack of air, cold sweat, during the day - unsteadiness when walking + loss of coordination of movements) - are they cardiological, neurological, or endocrinological? violations? These symptoms have been “haunting me” since I was about 19 years old... An ECHO CG (done about 9 years ago) revealed only a slight thickening of the interventricular septum and thickening of the anterior leaflet of the mitral valve and a stroke volume of 45 ml.
And one more thing... In 2001, I had to get very nervous (they brought it up), after which a long-term increase in blood pressure appeared to 175/110 mm Hg. with tachycardia, dizziness, weakness in the legs; astringency, mainly in the left hand; pain in the cervicothoracic spine. Without X-rays and other types of examination (MRI in 2001 was unrealistic), a diagnosis of VSD was made; were prescribed Corvitol, Barboval, Laminaria due to an enlarged thyroid gland...
In July 2020, I became nervous, and my blood pressure rose to 198/103 mm Hg. Art., it was shaking terribly and there was pressure in the chest (I took 25 mg of Lozap and 0.5 tablets of Bisoprolol, lowered the blood pressure to 158/98 mm Hg, the pulse returned to normal; it was possible to bring it closer to normal after another 25 mg of Lozap "Please tell me, is it harmful to increase blood pressure above 180 mm Hg systolic in case of cerebrovascular insufficiency?
I would be very grateful for your advice!
November 07, 2020 Mikhail Valentinovich Bugaev answers: Cardiac surgeon of the highest category information about the consultant Hello. First of all, you still need to try to record an ECG (using Holter monitoring) during attacks, only then can we talk about proper treatment. Moreover, you say that they are frequent, but during the monitoring they were not present. Frequent dizziness is usually associated with brain problems; also see a neurologist. Drugs to control hypertension, such as bisoprolol, are taken not when blood pressure increases, but regularly, daily, in order to prevent its increase.
www.health-ua.org
Unstable blood pressure
With a sharp decrease in pressure, the blood circulation slows down. To normalize the flow of oxygen, the brain commands the heart to work harder, pumping increased volumes. A person feels strong heartbeats against the background of a normal pulse, and feels pulsation in the ears. The following conditions may be the cause:
- dehydration;
- excessive blood loss;
- vegetative-vascular dystonia;
- allergic reaction.
The increased heart rate is accompanied by nausea and loss of appetite, which lead to weakness and drowsiness. Treatment is to maintain blood pressure at the correct range of 120/70 or 130/80 depending on age. If necessary, review the diet, try to consume more protein, clean water, and fruits.
This phenomenon often occurs during pregnancy. A woman in this position experiences strong heartbeats and may lose consciousness. In most cases, this is a consequence of anemia - a lack of hemoglobin, which carries oxygen in the body. The problem should be solved by taking special medications containing iron and vitamins in an easily digestible form.
If the tests do not provide an answer to why the pressure changes sharply and a strong heartbeat occurs, you need to take care of your health:
- devote time to sports, physical therapy, swimming or dancing;
- regularly take mild medications with a sedative effect (Persen, Sedaphyton, valerian extract);
- walk daily for at least 1–2 hours;
- choose a complex from yoga breathing practice;
- do not use debilitating diets.
An active life combined with good nutrition helps strengthen the heart muscle. Gradually, attacks of strong heartbeat disappear: the body copes with stress and does not react to weather changes. Every year you should visit a therapist to get tested for hemoglobin and potassium levels, and monitor your weight.
In most cases, following simple recommendations from a cardiologist, it is possible to completely overcome the problem and prevent its recurrence. But doctors warn that there are a number of symptoms that indicate serious heart disease that requires immediate treatment:
- strong heart beats at night;
- the appearance of panic fear of sudden death;
- the beating is accompanied by pain in the sternum, burning, tingling;
- the skin becomes pale or very red;
- hand tremors are observed;
- the heart skips beats.
If such violations occur, it is necessary to urgently seek qualified diagnostics. It includes: ultrasound of the heart and digestive organs, liver, kidneys, electrocardiogram, a number of tests for hormones, proteins, hemoglobin. In severe situations, the patient is recommended to undergo a full computer examination that can identify neoplasms, cancer, and lung damage.
A strong heartbeat often occurs in a pre-infarction state, with a stroke, or coronary artery disease. These are dangerous pathologies that threaten the life of the patient. To eliminate the painful problem, you should take a number of medications:
- cardiac glycolysides (Digoxin, Korglykon, Novodigal);
- beta blockers (Atenolol, Metoprolol, Bisoprolol);
- sedative complexes (Sedaphyton, motherwort or peony tincture);
- special antioxidants (Preductal, Triducard).
If an attack of rapid heartbeat occurs at night, a person may wake up with a panic attack, be afraid of sudden heartbeats and pain. Urgent measures need to be taken:
- Wash with cool water, rinse your hands up to the elbows.
- Drink a few sips of sweet tea or ice water.
- Walk around the room, try to cough to stimulate blood movement.
- Take Valocordin, Corvalol, valerian extract.
Traditional recipes help relieve unpleasant symptoms and strengthen the heart muscle. For 10–14 days, you can take a decoction of St. John's wort mixed with hawthorn, rose hips, and dry motherwort. This tea is drunk several times a day, adding a little honey. Melissa, valerian root, and chamomile provide a mild sedative effect.
Doctors warn that strong heartbeats are a dangerous symptom, so you should not self-medicate or take potent drugs on the recommendation of friends or neighbors. Ignoring the problem often leads to the development of necrosis of individual parts of the heart sac, coronary disease, and ends in incurable complications.
Strong heartbeats at rest can also occur with unstable blood pressure. With a sharp decrease in blood circulation, the blood circulation quickly slows down. To re-normalize the flow of oxygen to the organs, the brain forces the heart to work harder. As a result, a person notices stronger beats while maintaining a normal pulse. This may also be accompanied by a feeling of ringing in the ears.
What causes the jump in blood pressure itself? Among the main factors are:
- Copious blood loss.
- Dehydration of the body.
- Allergic reactions.
- Vegetative-vascular dystonia.
Periodic strong heartbeats are subsequently accompanied by the following:
- Decreased appetite.
- Nausea.
- Drowsy state.
- General weakness.
You need to see a therapist or cardiologist. Treatment here is aimed at normalizing blood pressure, maintaining it within working limits with the help of medications. A review of the patient's diet is also required - he needs to consume more protein foods, fruits, and clean water.
Is a heart rate of 69 beats per minute low or normal for the average person?
A low pulse, like a high one, is not necessarily a factor of some kind of disease. Most often it occurs due to overwork, severe nervous breakdown, or devastation of a person. A low pulse is also considered when hemoglobin drops after heavy physical activity. It is accompanied by symptoms of dizziness, loss of consciousness, severe weakness, and chills. If low blood pressure is not typical for you, you should take the necessary steps at home.
- Stop being nervous if your pulse drops due to a nervous breakdown. Do not try to drink a sedative; it will only increase the effect of a drop in heart rate. Revive yourself by washing with cold water.
- If you feel like you are losing consciousness, lie down on the floor or any covering and raise your legs. This is done so that blood flow to the brain faster.
- Drink strong, sweet, warm tea.
- Contact your doctor if your condition does not change.
How to treat tachycardia
Doctors explain: it is not tachycardia that needs to be treated, but the disease that causes it. We must also remember about its physiological form, which is a natural reaction of the body. In general, therapy includes:
- identification and treatment of the underlying disease;
- rejection of bad habits;
- taking sedatives for frequent stress;
- moderate physical activity;
- weight control;
- taking medications such as Digoxin, Reserpine, Verapamil, Pulsnorma, Atenolol or Isoptin.
sovets.net
Folk remedies
Proven folk remedies can also be used as an auxiliary therapy. But only with the permission of your attending physician. For example, the following:
- Remedies that help combat the unpleasant symptom of strong heartbeat, strengthening the myocardium. This is a decoction of the following herbs: St. John's wort, rose hips, motherwort, hawthorn. The course of treatment here is 10-14 days. The decoction is drunk several times a day. You can sweeten it slightly with honey.
- Mild sedative effect. Refer to decoctions of valerian root, chamomile, and lemon balm.