Reasons for development
As already noted, aortic defects can be congenital or acquired.
As for the first options, it is rarely possible to identify a specific cause for the violation of embryogenesis. However, there are certain risk factors that every pregnant woman should be aware of:
bad habits (smoking, alcoholism);- infectious diseases (including such “harmless” ones as influenza);
- taking medications;
- strong psycho-emotional and physical stress;
- polluted environment;
- X-ray examinations.
The pathogenesis of the disease is as follows:
- one valve may be underdeveloped;
- a hole forms in one of the valves;
- A bicuspid valve is formed instead of a tricuspid valve.
Acquired defects usually develop as a result of previous illnesses.
Infectious diseases (sepsis, tonsillitis, syphilis and other sexually transmitted diseases). In this case, bacteria, entering the endocardium with the bloodstream, damage the structure of the valves
Autoimmune pathologies (rheumatism, systemic lupus erythematosus). The defect is formed due to the fact that immune cells begin to attack their own body, in this case the aortic tissue. As a result, a degenerative process develops and valve damage occurs.
Atherosclerosis. It develops in older people, when calcium salts settle on the valve flaps and plaques form. As a result, their mobility decreases.
Chest injuries. The reason is rare, but still occurs. Valves are deformed due to direct mechanical impact.
It is worth noting that these factors can also cause the development of other defects, such as mitral (bicuspid valve defect) or tricuspid.
Three-valve defect
ICD-10 code: I08.3.
Description
Combination of aortic stenosis with mitral and tricuspid valve insufficiency. Occurrence - 1 case per 100,000 population . The disease is characterized by extremely rapid decompensation (within 1 year).
Both circles of blood circulation are affected. Depending on which half of the heart the predominant lesion is located, the disease will begin with either arterial insufficiency or venous stagnation (compensation), always supplemented by an increase in pressure in the lungs and involvement of neighboring valves in the process (subcompensation). Lung congestion leads to increased pressure in the right ventricle and rapid depletion of the right ventricle, causing blood to pool and veins to dilate throughout the body (decompensation).
The prognosis is unfavorable due to the rapid depletion of myocardial fibers. Distinctive signs are early pulmonary edema, a tendency to pneumonia, weight gain, disorders of consciousness, digestion and urination.
Characteristic signs
- Compensation . Paleness, quickly turning into blueness of the skin. Transient swelling of the legs, shortness of breath, decreased blood pressure.
- Subcompensation . Interruptions in heart function, difficulty walking, shortness of breath at rest, constant headaches, loss of appetite. Worsening at night. The swelling rises to the knees and does not subside.
- Decompensation . Loss of consciousness, decreased amount of urine, thinning and vulnerable skin, stupor, lack of response to any cardiac medications.
Diagnostics
- Inspection . Noisy shortness of breath, difficulty speaking, wheezing, cough streaked with blood.
- Palpation . The skin is warm, the swelling is dense. The liver protrudes from under the edge of the costal arch. A cardiac impulse, a “frog belly”, a decrease in pressure, and a rapid pulse are detected.
- Percussion . Expansion of all boundaries of the heart, dullness of pulmonary sound (pulmonary edema).
- Auscultation . Constant blowing noise superimposed on ri, decreased volume of tones, moist rales.
- ECG . Extrasystoles, atrial fibrillation, signs of ventricular and atrial hypertrophy (bifurcation and increased amplitude of the P and R waves).
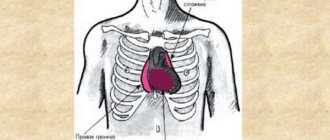
- Radiography . Fluid accumulation in the lungs, spherical heart (cardiomegaly).
- Ultrasound . Method of confirming the diagnosis. Ultrasound reveals the type of combination and the magnitude of the stenosis, as well as the degree of reverse blood flow. Depending on which valve has the greatest backflow, the predominance of the defect is determined.
How are they treated?
The choice of method depends on the complaints and general condition. The disease quickly leads to decompensation, so it is important to detect the patient in an early period. Indication for drug treatment is preparation for surgery, for surgery - subcompensation.
- Conservative therapy is used in stage 1 . It is impossible to cure the defect without surgery. Drugs used: cardiac glycosides (digoxin), diuretics, antiarrhythmics, adrenergic blockers.
- Surgical treatment is indicated in the subcompensated stage and often combines commissurotomy (separation of fused folds), valvuloplasty (valve expansion) and prosthetics, which are performed in several stages.
Classification of violations
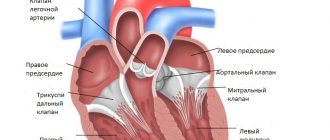
There are two fundamentally different groups of aortic valve defects.
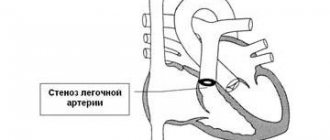
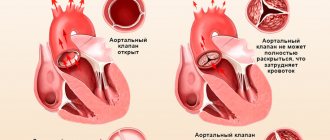
The first is aortic valve stenosis. This term means that the doors have lost their elasticity and cannot open completely. A restriction occurs due to which the ventricles are not able to push all the blood into the aorta.
There is also valve insufficiency. In a normal state, having passed blood into the aorta, the valves close in order to prevent reverse flow into the heart (the so-called regurgitation). In pathology, this mechanism does not work; a small gap remains between the valves and part of the blood returns to the ventricles.
It is important to know that these forms occur both in isolation and as a combined (mitral-aortic) defect. Usually there is a predominance of a defect in one of the structures. Combined aortic heart disease is a simultaneous combination of insufficiency and stenosis.
Failure is classified by the volume of blood that returns to the left ventricle:
- I degree – regurgitation up to 15%;
- II degree – 15-30%;
- III degree – 30-50%;
- IV degree – more than 50%.
Clinical manifestations
Isolated forms may not appear for a long period of time, while combined aortic heart defect gives a pronounced clinical picture.
Also, the symptoms of the disease depend on the type of lesion. The pathogenesis of stenosis is primarily characterized by an increase in resistance to blood flow, which is manifested by the following symptoms:
myocardial ischemia (compressive pain in the heart);- cardiopalmus;
- shortness of breath, cardiac asthma;
- dizziness;
- fainting;
- cyanosis (blue discoloration) of the extremities.
In case of insufficiency, cardiac output is significantly reduced (due to the fact that some of the blood returns back). The following symptoms occur:
- tachycardia;
- pain in the heart like angina pectoris;
- swelling of the neck veins;
- noise in ears;
- dizziness;
- pain and heaviness in the right hypochondrium;
- dyspnea.
Development of rheumatic aortic stenosis
Under the influence of systemic ailments that disrupt the immune system, the development of so-called rheumatic aortic stenosis occurs.
In particular, with rheumatism or lupus erythematosus, connective tissue growths appear at the junction of the aorta and the heart. Because of this, the lumen of the vessel narrows, making it difficult for blood to flow into it from the ventricle. Subsequently, calcium deposition occurs, leading to even greater narrowing and loss of elasticity of the valve.
Regardless of the reasons that led to the pathology in question, the result is always identical: due to impaired blood flow, all organs begin to lack nutrients. This causes the formation of symptoms accompanying aortic stenosis.
Diagnostics
Due to the rather vague picture of the disease, a thorough examination should be carried out to accurately determine the cause of the disease. First of all, the doctor must collect a detailed medical history.
Physical diagnostic methods (auscultation)
Upon examination, pale skin, cyanosis, increased pulsation, and swelling of the veins of the neck are revealed.
Upon palpation (and in some cases visually), a “heart hump” is determined - a protrusion of the chest wall due to cardiac hypertrophy.
A specific symptom of stenosis is “systolic cat purring.” In this case, a trembling of the chest wall is felt in the projection of the left ventricle.
Percussion determines the increase in heart size.
With stenosis, a predominant decrease in systolic pressure is observed, with insufficiency - in diastolic pressure.
Auscultation with stenosis reveals a systolic murmur (due to obstructed blood flow). Failure is characterized by a murmur during diastole (since regurgitation occurs when the ventricles relax.)
Instrumental methods
Identification of the above symptoms requires further examination. The “gold standard” for diagnosing valve defects is ECHO-CG with Dopplerography. This method allows you to study in detail the structure and function of the heart. An electrocardiogram and chest x-ray should be performed.
In rare cases, if the results are inaccurate, additional studies are performed using MRI, CT, and angiography.
Treatment options for a patient with aortic disease
In the absence of symptoms and in mild stages, treatment is usually not prescribed. Patients are recommended to undergo additional examinations every six months.
Drug treatment
Conservative therapy does not ensure complete recovery of patients with aortic defects. The goal of pharmacological treatment is only to improve symptoms and prevent complications. In addition, medications are prescribed in preparation for operations.
The following groups of medications are used:
- calcium antagonists (verapamil, nifedipine) – used for arrhythmias and arterial hypertension;
- diuretics (torasemide, spironolactone) - reduce the load on the heart;
- beta-blockers (atenolol, propranolol) – lower blood pressure, improve hemodynamics;
- ACE inhibitors (enalapril, lisinopril) - have a hypotensive effect.
- antianginal agents (Sustak, Nitrong).
If the disease is caused by an infection or an autoimmune process, drugs are used for etiotropic (i.e., aimed at the cause) therapy:
- antibiotics (penicillins, carbapenems, fluoroquinolones and others) – for infectious diseases;
- glucocorticosteroids (prednisolone, dexamethasone) – for systemic autoimmune diseases such as rheumatism;
- anti-sclerotic drugs (levostatin, atorvastatin).
However, the main method of treating valve defects is still surgery.
Operations are indicated in the following cases:
- severe stage of the defect, which leads to the development of heart failure;
- combined defects;
- the presence of associated factors that can lead to decompensation;
- reduction in ejection fraction even in the absence of complaints.
Contraindications are:
- age over 70 years;
- the presence of severe comorbid pathologies (renal, liver, respiratory failure, diabetes mellitus, etc.)
For congenital anomalies, organ-sparing valvuloplasty is more often used. If you use this method for acquired defects, relapses may occur. The technique involves excision and suturing of valve defects. In some cases, balloon valvuloplasty is used. In this case, the aortic mouth is widened with a special device. An important feature of this operation is its minimally invasive nature.
In case of acquired pathologies, valve replacement is used. Implants are made from both synthetic materials (silicone) and natural ones (bioprostheses from one’s own tissue or from a deceased person).
Treatment
Combined heart disease is a pathology that does not have clear instructions for its elimination. For each case, individual options for eliminating the problem are selected. If there is a narrowing of the valve, then the need for surgical intervention appears in the presence of the slightest symptoms of the disease. Regurition also requires surgical treatment if obvious signs are present.
Also read: Causes of effusion pericarditis
General therapeutic methods
Treatment consists of eliminating the cause of the defect. Usually this is rheumatism or atherosclerosis. The patient, first of all, must follow a diet in which animal fats, salt and a lot of liquid are prohibited.
Physical activity needs to be reduced. If a person is professionally involved in sports, then he should reduce the intensity and duration of training.
Drinking alcoholic beverages and smoking are strictly contraindicated.
Secondary preventive measures against rheumatism include regular administration of the antibacterial drug Bicillin. But it is not always used.
Patients are recommended to undergo complete sanitation of the oral cavity. Before visiting the dentist and if necessary, any procedures that may be accompanied by a violation of the integrity of blood vessels, it is necessary to use antibacterial agents for prevention. This will avoid the development of infective endocarditis.
Drug therapy
If the defect causes problems in the form of atrial fibrillation, then there is a need to use anticoagulants and drugs to make the heart rate slower.
If a combined heart defect has caused the development of a severe form of heart failure, then relief is achieved by:
- angiotensin-converting enzyme inhibitors;
- diuretics;
- angiotensin receptor blockers;
- cardiac glycosides.
There are no indications for the use of beta-blockers.
Surgical techniques
A good effect can only be achieved with the help of surgical treatment methods. The solution to the problem is selected depending on the type:
- For mitral stenosis in combination with aortic insufficiency, surgical treatment is prescribed if the first symptoms of increased pressure in the vessels of the lungs appear. In the initial stages, mitral valvotomy is often performed. An inflatable balloon can also be used, which is placed into the cardiac chambers through the vascular lumen. If there is no effect from such procedures, then the aortic valve is replaced with a mechanical prosthesis.
- For mitral stenosis and tricuspid valve insufficiency, mitral valvotomy is performed. The procedure is prescribed regardless of the manifestations that bother the patient. Surgery is usually sufficient to eliminate swelling of the lower extremities and ascites. If the defects are severe, it is impossible to do without installing prostheses in place of the damaged valves.
- In case of insufficiency of the mitral and aortic valves, plastic surgery of the mitral valve and installation of a prosthesis in place of the aortic valve are prescribed.
- With valve stenosis, there is a need for mitral valvotomy. If it does not produce results, prosthetics are needed.
- For aortic stenosis and mitral insufficiency, both valves are replaced with prostheses. The option of mitral valve restoration and aortic valve replacement is also used. If the stenosis is more developed, then therapy can eliminate the symptoms, and there is no need for mitral valve surgery. A severe form of the disease requires mitral valve replacement. Whether the aortic one needs to be replaced can be determined by additional studies.
Surgical treatment significantly improves the prognosis.
Patient monitoring
Valve defects are a very insidious disease that can hardly manifest itself, and then lead to the development of heart failure. In addition, a blurred clinical picture makes it difficult to make a correct diagnosis.
Auscultation of aortic heart defects is the simplest screening method. If you hear pathological noises, you should immediately send the patient for further examination.
Therefore, if you have been diagnosed with this pathology, you need to take preventive examinations as responsibly as possible. You should undergo echocardiography and other examinations prescribed by your doctor at least once every six months.
Complications of combined aortic-mitral heart disease
Complications are associated with expansion of the heart chambers, impaired conduction and contractility of the myocardium:
- atrial fibrillation with irregular rhythm;
- atrioventricular block, which may require the installation of a pacemaker;
- secondary endocarditis of the affected valves with septic complications;
- left ventricular, less often - right ventricular heart failure;
- pulmonary hypertension.
Atrial fibrillation as a complication of combined aortic-mitral heart disease
conclusions
Aortic valve defects are fairly common diseases that can be either congenital or acquired. Impaired blood flow due to damage to the valves can lead to the development of chronic heart failure.
The symptoms that arise from aortic valve disease are not specific enough, but modern diagnostic methods can easily detect them.
In the absence of significant contraindications, surgical treatment of this disease gives a good result. The prognosis for life and work ability is favorable.