The term “Coronary heart disease” includes a group of diseases:
- myocardial infarction
- atherosclerotic cardiosclerosis
- angina pectoris.
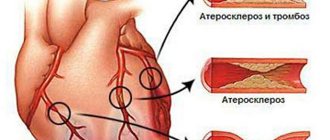
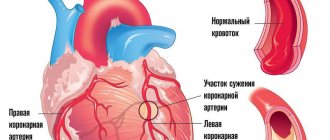
Angina pectoris (synonymous with angina pectoris) is characterized by attacks of sharp chest pain and discomfort in the chest due to lack of blood supply to a certain area of the heart. The severity of the attacks varies, and in rare cases it ends in death. The main cause of the disease is atherosclerosis of the coronary arteries of the heart.
To make an accurate diagnosis, a number of other diseases that may manifest as pain in the heart area should be excluded: spinal osteochondrosis, herpes zoster, diseases of the esophagus and stomach, lung diseases, cardioneurosis, pericarditis.
Types of angina
There are the following types of disease, which depend on the clinical picture:
Angina pectoris
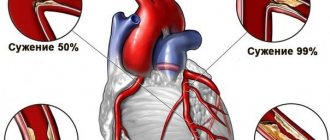
One of the main manifestations of IHD. As a result of a discrepancy between the myocardial need for oxygen and its delivery through arteries narrowed due to atherosclerosis, myocardial ischemia occurs, which is manifested by chest pain or shortness of breath and severe fatigue during exercise.
Stable exertional angina is divided into four functional classes. Functional classes of angina are designed for accurate diagnosis and include a wide variety of clinical information (eg, easy walking on level ground and brisk climbing of stairs).
Variant (spontaneous) angina
Characterized by unpredictable appearance, i.e. pain may also occur at rest. It does not occur as a response of the heart to emotional and physical stress and differs from angina pectoris in that it is usually based on spasm of the coronary arteries of the heart, and not just atherosclerotic damage.
Unstable angina
Requires immediate hospitalization, there is a high probability of developing myocardial infarction.
Non-drug treatment
If a patient has angina pectoris infrequently, the attack is easily stopped by taking Nitroglycerin, and diffuse changes have not begun, then treatment should begin with the following:
- balance your daily routine. Sleep for 6–7 hours, take breaks after physical activity, minimize nervous stress;
- diet therapy. You should reduce the amount of food per day, since overeating can trigger an angina attack. Meals should be taken in the morning, at lunch and three to four hours before bedtime; if desired, lunch and dinner can be divided into several parts. Food should be low-fat, with a minimum amount of animal fat (cholesterol);
- dosed physical activity. If possible, you should increase the amount of physical activity, walk more in the fresh air (but not cold air, cold air can cause an attack of angina), walking up the stairs - preferably down. Physical activity is necessary to prevent the formation of blood clots in the coronary vessels and heart;
- refusal to take nicotine in any form (cigarettes, cigars, pipes, hookah, vape), nicotine increases blood pressure and causes spasm of the coronary and pulmonary vessels. Avoiding alcohol is necessary due to its toxic effects on the heart muscle.
If the results of non-drug treatment are poor or if angina is severe, you should switch to medications (conservative treatment).
Nutrition for angina
Cardiologists recommend the following drug regimen for the treatment of angina pectoris:
- acetylsalicylic acid. The drug has a very strong antiplatelet effect on human platelets. When taking the drug, the ability of platelets to stick together disappears forever. To prevent the formation of blood clots, acetylsalicylic acid is used daily at a dose of 75–150 mg, once a day after dinner. If you are intolerant to acetylsalicylic acid, use Clopidogrel in the same dosage. A side effect of these drugs is disruption of the regeneration of the epithelium of the gastrointestinal tract;
- statins. The most popular representative of statins is Atorvastatin. The drug is taken to lower cholesterol levels. It is effective for the prevention of atherosclerosis and ischemic heart disease. The dosage of the drug is 10–20 mg for one day, the dose is selected by the attending physician. Side effects may include muscle pain and allergic reactions;
- "Nitroglycerine". It is used directly during an attack or to prevent angina pectoris. During an attack of angina, you should put a Nitroglycerin tablet (drop a drop if it is a drop form) under your tongue. After ten minutes, you can take another tablet, but no more than three tablets at a time. If the pain does not disappear after 20–30 minutes while taking Nitroglycerin, it is necessary to suspect myocardial infarction and take the patient to the cardiology department. There are also inhaled forms of Nitroglycerin, which are also very effective and convenient. Side effects of the drug may include headache and nausea;
- beta blockers. There are two types of such drugs, selective and non-selective blockers. Now cardiologists prefer only selective ones due to fewer side effects from the lungs. The main representatives are “Bisoprolol” and “Metoprolol”; the dosage of the drugs is selected individually by titration and heart rate monitoring. The drugs protect the heart from lack of oxygen and trigger the processes of remodeling of hypertrophied myocardium;
Medicines are necessary to reduce the frequency of attacks, reduce their duration and prevent the development of myocardial infarction
- calcium channel blockers. These include Amlodipine and Nifedipine. The advantage of this group of drugs is that they have a very small number of negative effects, act quickly and are quickly eliminated from the body. "Amlodipine" has a prolonged effect and is used for permanent treatment, "Nifedipine" has a short effect and is used exclusively during an attack of angina pectoris;
- ACE inhibitors. Used to reduce blood pressure and normalize metabolism in the myocardium. The main representatives are “Lisinopril” - 10 mg once a day in the morning (the dose may vary), “Pirindopril”, “Enalapril”, “Captopril” - the latter is used to relieve hypertensive crises and angina pectoris.
Unfortunately, angina cannot be cured; medication must be taken for life. But the treatment regimen is constantly changing, some drugs are replaced by others or their pharmacological groups are changed.
For stable angina, treatment can be done without surgery. But if a patient experiences unstable angina or angina at rest, surgery should be considered.
Symptoms
Main symptoms include:
- acute chest pain radiating from the left (or right) side to the lower jaw, arm, shoulder blade
- shortness of breath
- feeling of suffocation and lack of air
- feeling of fear, anxiety
- increased pain in the left chest area when trying to take a deep breath
- increased sweating
- tachycardia
- deviation of blood pressure from normal (low or high).
The main factors in the development of the disease that cause symptoms of angina pectoris include
- age (usually after 40 years)
- gender (men develop CHD on average 10 years earlier than women)
- hereditary factor.
An important role in the formation of the disease is played by excess body weight, a history of diseases such as diabetes, arterial hypertension, increased blood clotting, metabolic syndrome, emotional lability, lack of physical activity, smoking and alcoholism.
How to treat angina
In the cardiology center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, advanced methods of treating angina pectoris are successfully used:
- Optimal drug treatment. It can be performed on an outpatient basis or as an inpatient basis in the cardiology department. Treatment involves taking medications - B-blockers, antiplatelet agents, statins, nitrates, etc.;
- Surgical intervention:
- Coronary artery bypass grafting is an operation that allows you to bypass the site of damage (narrowing) of a vessel using shunts (vascular prostheses), creating a parallel channel for blood flow to the myocardium;
Stenting of the coronary arteries is a low-traumatic treatment method in which a stent (spacer) mounted on a balloon is placed through a miniature catheter to the narrowed section of the coronary artery. The balloon is inflated with liquid, the stent expands, squeezing out the plaque that narrows the lumen of the artery, the balloon is quickly deflated and removed. The stent, like a spacer, remains in the lumen of the artery, preventing re-narrowing and ensuring normal blood flow.
Our clinic performs unique minimally invasive surgeries, as well as high-quality diagnostics of various heart diseases. Specialists of the cardiology center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency successfully use advanced European treatment methods in their work. They constantly improve their skills and exchange experiences at international conferences.
Diagnostics
In diagnosing angina, a balanced and competent approach is necessary, because with unstable angina, the patient's condition may worsen until the development of myocardial infarction. Each study must be substantiated.
- ECG
- 24-hour ECG monitoring
- bicycle ergometry or treadmill (stress test with simultaneous ECG recording)
- EchoCG
- stress echocardiography
- coronary angiography
- myocardial scintigraphy
At the EXPERT Clinic, cardiologists are also functional diagnostics doctors. They will weigh all the risks before conducting the examination.
3. Coronary heart disease, angina and rules of life
Usually a well-functioning heart is practically undisturbed, but there may come a time when the heart suddenly makes itself felt.
Most often this is associated with the development of a serious disease – coronary heart disease.
What is coronary heart disease?
IHD - coronary heart disease (angina pectoris, unstable angina, myocardial infarction) - is a consequence of narrowing and blockage of the main arteries of the heart with atherosclerotic plaques. Over time, there are more and more of them, and when the lumen of the vessel is blocked by 50% or more, difficulty in blood flow occurs. As a result, the delivery of oxygen and nutrients to the heart muscle decreases, oxygen starvation (hypoxia) develops, which leads to myocardial ischemia. The larger the size of the atherosclerotic plaque, the smaller the lumen of the vessel and the less blood flows through it, the more pronounced the myocardial hypoxia, which means the more pronounced ischemia (angina).
If, due to physical activity or emotional stress, you experience pain or a feeling of pressure or heaviness behind the sternum, you have a high probability of having angina pectoris (formerly called angina pectoris).
It is strongly recommended that you be examined by a cardiologist or physician.
Know that an attack of angina can be triggered by exercise, emotional stress, cold air and smoking.
Under the influence of these external influences, the pulse (heart rate) increases and blood pressure (BP) increases, which entails an increase in the myocardial oxygen demand against the background of a decrease in its delivery to the heart cells, thus developing myocardial ischemia, which the patient feels as angina pectoris.
How to diagnose angina?
The diagnosis of coronary artery disease and angina is made on the basis of a thorough survey and complaints.
To confirm the diagnosis and clarify the severity of the disease, additional methods are needed:
— taking an electrocardiogram (ECG) at rest and at the height of an attack
— carrying out stress tests (treadle test or test on a bicycle ergometer)
— according to indications (in case of high pulse, abnormal heart rhythm), 24-hour ECG recording is performed (Holter ECG monitoring)
— Sometimes coronary angiography (contrast study of the arteries of the heart) is required.
Warning signs of angina development:
— sudden discomfort, pain, or burning sensation;
— Pain can be triggered by walking, any physical activity, anxiety, emotional stress, cold air, smoking, less often pain appears at rest;
— pain most often occurs behind the sternum, but can radiate (radiate) to the left arm, left half of the lower jaw, teeth, shoulder, back or upper abdomen;
— pain occurs predominantly in the form of mild attacks (3-5 minutes), attacks can be repeated with varying frequency;
— usually the pain disappears 2-3 minutes after stopping walking or other physical activity, or taking nitroglycerin;
— attacks of angina may intensify with increased blood pressure, smoking, late intake or withdrawal of medications.
Types of angina:
V If your attacks appear during the day after the same load, with the same frequency and are of the same type, then you have stable angina.
V If your attacks become more frequent, occur with less stress and even at rest, become stronger, more severe and last longer, and are poorly controlled by the usual dose of nitroglycerin, then you should suspect unstable angina .
You need urgent medical consultation.
V If the pain becomes more intense and lasts for more than 15 minutes, repeats in waves at rest and does not go away after taking three nitroglycerin tablets, there is severe weakness and a feeling of fear, blood pressure and pulse fluctuate sharply, then you should suspect myocardial infarction. In this situation, urgent consultation with a doctor and immediate call for emergency medical assistance is necessary!
To improve your well-being and prevent the development or further progression of IHD, determine whether you have risk factors.
Factors that increase your risk of developing CHD
(check your risk factors):
Factors you cannot control
[] age/gender: men over 45 years old, women over 55 years old
[] early development of IHD in close relatives: - in men under 55 years of age, - in women under 65 years of age
Factors you can control
[] elevated blood pressure
[] smoking
[] elevated blood cholesterol levels
[] elevated blood glucose levels (diabetes)
[] excessive alcohol consumption
[] passive lifestyle
[] overweight
[] stressful situations
Inform your doctor about the risk factors you have identified and ask for advice on what you should do to correct them and subsequently control them well.
Treatment of coronary artery disease and angina has two goals:
the first is to improve the prognosis and prevent the occurrence of serious complications - myocardial infarction, sudden death - and prolong life;
the second is to reduce the severity of clinical symptoms - the frequency and intensity of angina attacks and, thus, improve the quality of life.
You should:
* learn to stop an attack of angina:
— interrupt the load, stop,
— take nitroglycerin under the tongue;
* be informed:
— about the potential undesirable effects of nitrates,
— about the possibility of developing hypotension after taking nitroglycerin;
— about the need to immediately call an ambulance if an angina attack persists at rest and/or is not relieved by nitroglycerin for more than 15-20 minutes;
— about the nature of angina, the mechanism of its development and the significance of this disease in the prognosis of life and recommended methods of treatment and prevention,
* to prevent an attack of angina, take nitrates (nitroglycerin) before exercise, which usually leads to angina.
How can you reduce the high likelihood of progression of coronary artery disease, angina,
as well as the development of serious cardiovascular complications
(myocardial infarction, unstable angina, sudden death, heart failure, cerebral stroke)?
STEP 1 relieving an attack of angina
If you have an angina attack:
V stop physical activity, stop walking, sit down, calm down and relax,
V put one nitroglycerin tablet under the tongue or use nitroglycerin in the form of a spray,
V Before taking nitroglycerin, you should sit down, because the drug may cause dizziness or decreased blood pressure,
V crush the nitroglycerin tablet and let the tablet dissolve completely; if the pain does not stop, then after 3-5 minutes repeat taking nitroglycerin either in the form of a tablet (up to 3 tablets) or in the form of a spray (spraying into the mouth up to 3 times)
V If an attack of angina cannot be relieved within 15 minutes after taking 3 tablets of nitroglycerin, you should immediately seek emergency medical help, and immediately chew 1 tablet of aspirin with water (aspirin prevents the formation of a blood clot). You may be developing a myocardial infarction!
REMEMBER!
You should always have a sufficient number of nitroglycerin tablets with you and they should always be at hand, no matter where you are at the moment!
STEP 2 regular blood pressure checks
People with elevated blood pressure levels and untreated developed myocardial infarction in 68 out of 100 cases and cerebral stroke in 75 out of 100 cases.
Monitor blood pressure levels carefully:
* at least once a year – with a single unstable increase in blood pressure discovered by chance;
* at least once a month - if you feel well, but have a tendency to frequently increase blood pressure;
* at least 2 times a day – in case of exacerbation, poor health, stable increase in blood pressure
Aim for a blood pressure level below 140/90 mmHg.
If you have suffered a myocardial infarction, suffer from angina pectoris, intermittent claudication, then strive for a lower blood pressure level - below 130/80 mm Hg.
In people with good blood pressure control:
* 42% fewer brain strokes;
* 20% less lethal and other serious cardiovascular complications (myocardial infarction, unstable angina, sudden death);
* 50% less heart failure;
* 14% fewer deaths from any other non-cardiac cause.
STEP 3 regular monitoring of cholesterol levels in the blood
Check your blood cholesterol levels and, if they are elevated, discuss with your doctor the possibility of taking cholesterol-lowering medications.
Criteria for optimal lipid levels in the majority of patients with coronary artery disease, patients who have had myocardial infarction, or surgery on the vessels of the heart, carotid arteries or arteries of the lower extremities:
* Total cholesterol - less than 4.0 mmol/l
* LDL cholesterol – less than 1.8 mmol/l
* Triglycerides – less than 1.7 mmol/l
* HDL cholesterol – for Men – 1.0 mmol/l or more
* HDL cholesterol - for Women - 1.2 mmol/l or more
STEP 4 heart rate control
In case of coronary artery disease, angina pectoris, or after a myocardial infarction, it is very important to control the pulse rate (heartbeat).
The optimal heart rate should be between 55-60 beats per minute.
This optimal heart rate is usually maintained with special medications prescribed by the attending physician.
STEP 5 proper nutrition
Change your eating pattern: eat healthy foods with less animal fat (60-105 g/day for men and 45-75 g/day for women) and rich in vegetables, fruits, complex carbohydrates, dietary fiber, fish.
Exclude from the diet: fatty meats, strong meat broths, any fat, sausages (even the so-called doctor's ones!), sausages, ready-made dumplings, canned meat, mayonnaise, internal organs of animals, brains, caviar, butter, hard margarine, fatty cottage cheese , cream cakes, creamy ice cream.
STEP 6 more movements
Move more and be physically active (at least 30 minutes of moderate exercise on most days of the week). If you have heart problems and are taking medications, talk to your doctor before changing your level of physical activity.
If you have been physically inactive for a long time, or if you are over 40 years old, or have angina pectoris, then the mode and level of physical activity should be determined by your doctor or physical therapy specialist, determining the pulse safety zone.
Physical activity is useful: aerobic, dynamic and moderate intensity - cycling, measured walking, swimming, team sports (football, volleyball), etc.
Optimal training walking tempo (number of steps per minute) depending on physical load tolerance (according to a load test on a bicycle ergometer)
Amount of load performed
during bicycle ergometer test, W 50 75 100 125
Function class
angina III II II I
Optimal pace
number of steps per minute 99-102 105-108 111-114 118-121
(or average) or 100 or 105 or 110 or 120
STEP 7 monitor the status of other risk factors
> Monitor your weight and measure your waist circumference (a waist circumference greater than 102 cm for men and greater than 88 cm for women indicates abdominal obesity, which is associated with a risk of cardiovascular complications).
> Stop smoking.
> Learn to control your psycho-emotional stress (avoid conflict situations, devote time to auto-training and relaxation methods).
> Maintain normal blood glucose levels: < 6 mmol/L (110 mg/dL)
STEP 8 Take medications prescribed by your doctor regularly
Today, the doctor has at his disposal a sufficient number of highly effective and safe drugs to reduce high blood pressure, prevent angina pectoris and prevent the development of serious cardiovascular complications.
REMEMBER!
Interruptions in taking medications reduce the effectiveness of preventing the development of myocardial infarction, unstable angina, and heart failure.
For the treatment of coronary artery disease and angina pectoris, different classes of medications are used today, the action of which is aimed at preventing the development of myocardial ischemia and angina attacks, vascular thrombosis, preventing the progression of atherosclerosis, reducing blood pressure and pulse rate (heart rate).
Take medication as directed by your doctor!
If the disease, despite active drug therapy, progresses, it is necessary to use modern interventional and surgical methods to restore blood supply to the myocardium:
V balloon angioplasty – expansion of the vessel at the site of stenosis by inflating the balloon
V stenting of the coronary arteries - installation of a special stent (tube) that allows for a long time to expand the artery of the heart and ensure normal blood flow
V coronary artery bypass grafting is used for a certain localization of atheromatous plaque and significant and multiple narrowing of the coronary vessel, when the first two methods are not effective
MAIN!
Treatment of coronary heart disease through lifestyle changes and highly effective medications prescribed by a doctor must be constant, long-term and daily.
STEP 9 keep a self-monitoring diary
A self-monitoring diary must be kept in order to promptly notice negative changes in the course of the disease and immediately contact your doctor.
The diary should record: blood pressure level, pulse rate, number of angina attacks, amount of nitroglycerin in the form of tablets or spray inhalations that were taken to relieve (relieve) an angina attack or prophylactically, for example, before physical activity, going outside to prevent it development.
The diary will allow you and your attending physician to evaluate the effectiveness of treatment, prevent exacerbation of the disease and, if necessary, correct therapy.
IF YOU FOLLOW THESE RULES AND MANAGE YOUR LIFE SMARTLY, YOUR ILLNESS WILL ALWAYS BE UNDER GOOD CONTROL!
________________________________
As part of the Educational Project for Patients “Be Healthy!” For more information, read other brochures from the Patient Library:
1. “Arterial hypertension and control rules”
2. “Arterial hypertension, physical activity, stress”
3. “Coronary heart disease, angina and rules of life”
4. “Smoking: from habit to arterial hypertension and atherosclerosis”
5. “Arterial hypertension and nutrition rules”
6. “Caution: cholesterol!”
7. “Brain stroke: how to avoid it?”
8. “Arterial hypertension, metabolic syndrome, diabetes mellitus”
9. “Atherosclerosis: from vascular disease to possibilities of prevention”
Russian Society of Cardiosomatic Rehabilitation and Secondary Prevention (RosOKR).
Go to the “School for Patients” page
Treatment
The goals of treatment are to improve the prognosis (prevent heart attack) and eliminate symptoms of the disease. Non-medicinal (sports, diet), medicinal (tablets and drip infusions) and surgical treatment methods are used.
At the EXPERT Clinic, patients have the opportunity to receive a full consultation with a cardiologist on lifestyle changes and modification of risk factors. If necessary, treatment in a day hospital under the supervision of experienced medical personnel is possible.
Treatment methods
By the term treatment of angina pectoris, cardiologists mean treatment of the original disease, which led to myocardial ischemia and the development of pain.
In first place among diseases that can lead to angina pectoris is atherosclerosis of the coronary arteries, leading to myocardial ischemia.
The following methods are used to treat coronary heart disease:
- non-drug treatment (diet, regimen, dosed exercise, giving up bad habits);
- medicinal or conservative (use of drugs that help improve blood circulation in the heart);
- surgical treatment (stent placement or coronary artery bypass grafting).
Like any disease associated with a disruption in the functioning of the cardiovascular system, angina pectoris is treated with several types of drugs at once
Recommendations
To prevent angina attacks you must:
- quit smoking
- control cholesterol levels, if necessary, eat a low-fat diet
- perform a dosed and doctor-selected set of physical exercises
- avoid stress
- lead a healthy lifestyle
A balanced diet, dosed physical activity and regular monitoring by a qualified doctor can save a patient with angina pectoris from heart surgery.
Angina pectoris (angina pectoris): causes, types, risk factors
- Obesity. This is the first factor in the development of diseases of the cardiac system, vascular system and pathologies in internal organs. People who are overweight have a high cholesterol ratio in their blood, and this leads to the formation of atherosclerotic plaques and poor blood flow in the artery system;
- Sedentary lifestyle. This factor is observed in people who do not engage in physical recreation, have given up walks, outdoor games and devote all their free time to watching television films or spend a long time at the computer;
- Tobacco smoking. Smoking, like obesity, is the first among the provocateurs of IHD. The fight against smoking has an international level. Cardiologists say that passive smoking is also dangerous for the cardiac system and the entire body. If a person has suffered a heart attack, then smoking is a deadly action for him;
- Alcohol addiction. This is a threat not only to the heart and arteries, but to the entire body;
- Diseases that accompany ischemic heart disease. Diabetes mellitus, like a disruption in the endocrine system, hypertension, and gallstones, provoke disruptions in the functioning of the heart muscle and vascular system. IHD develops.
- Pathology of peripheral vessels. This disease manifests itself when the vessels of the extremities are clogged with atherosclerotic plaques.
- Vitamin deficiency is directly related to coronary artery disease. Lack of vitamins B6, B9, B12 provokes heart pathologies. With a deficiency of vitamins, the level of homocysteine in the blood increases, which increases the risk of heart attack and stroke;
- Inflammation of the lungs (pneumonia) and infectious inflammations. Infections and viruses have a destructive effect on arteries. Coccal and chlamydial infections can settle on plaques in the arteries and heart muscle;
- Night snoring. Apnea (stopping breathing) provokes heart disease, since snoring causes a temporary stop in air flow and the myocardium suffers from this condition. Severe apnea provokes a heart attack and coronary artery disease;
- Inflammation of periodontal disease causes a heart attack;
- Age factor. With age, vascular tone is lost, which provokes ischemic heart disease;
- Gender of the patient. Men more often suffer from heart pathologies and at an earlier age. Women suffer from coronary artery disease after menopause;
- Heredity. If relatives have diabetes or hypertension, then the risk of coronary artery disease increases several times;
- Race. The highest percentage of heart disease is in the African-American race;
- Depressive state. Depression increases the risk of heart attacks;
We invite you to familiarize yourself with: IHD angina pectoris fc 2 operation
IHD is the most common cardiac pathology on the planet today. Ischemia is not completely cured. Maintenance treatment is long and complex.
The disease can be prevented with a balanced diet, lifestyle and moderate exercise.
FAQ
How to avoid angina pectoris?
To avoid angina pectoris, it is necessary to prevent the development of atherosclerosis if possible, because in the vast majority of cases it is the cause of angina. As is known, many factors directly influence the formation of atherosclerotic plaques. Gender, age, heredity are predisposing factors that cannot be changed, but other factors can be controlled and even prevented:
- high blood pressure
- smoking
- high cholesterol
- overweight
- diabetes
- low physical activity
- stress
Changing these factors is in your hands!
Is it possible to completely recover from angina?
Angina pectoris, as a rule, occurs as a result of damage to the coronary arteries supplying blood to the myocardium by atherosclerosis, and this is a chronic incurable process. However, with a properly selected treatment regimen, it is possible to ensure that long-term remission occurs and angina attacks will not bother you. Also, at present, if necessary, it is possible to install a stent into the narrowed lumen of the vessel to restore blood circulation, or MCS/CABG surgery is a surgical intervention that restores the blood flow of the heart below the site of the narrowing of the vessel. In this surgical procedure, another path for blood flow is created around the narrowing site to the part of the heart that is not supplied with blood.
Where does it hurt during an angina attack?
Characteristic of angina is paroxysmal pain behind the sternum, in the center of the chest. The pain is of a compressive, pressing nature, more often associated with physical or psycho-emotional stress and goes away when it stops. The pain may radiate to the left arm, shoulder blade, lower jaw and collarbone. If nitrates are used, the effect on angina is not delayed, it develops immediately, within 1-2 minutes.
Are there ways to cope with an angina attack without medications?
Since many people experience angina attacks during physical activity, sometimes simply stopping the activity (walking, etc.) and resting can lead to the cessation of pain. However, people suffering from angina pectoris should always have nitroglycerin or nitrospray with them in order to relieve an attack of pain within one to two minutes. You should not delay the time before taking nitroglycerin, since pain is a manifestation of myocardial ischemia (insufficient blood supply), and if it persists, then foci of necrosis may occur in the myocardium (myocardial cells may die). If angina attacks become more frequent, you should urgently consult a cardiologist.
What medications will help with an attack of angina?
An attack of angina must be stopped as soon as possible from the moment of its occurrence, because prolonged ischemia will lead to the development of necrosis, i.e. myocardial infarction. If an attack occurs for the first time in your life, call an ambulance. You can take a nitroglycerin tablet on your own or use a nitro spray under the tongue. The effect will occur within 1-2 minutes and does not last long, 10-15 minutes. It is better to take the drug while sitting or lying down, as a short-term decrease in blood pressure, dizziness, headache, tinnitus may occur - these symptoms are safe and are a consequence of the action of nitroglycerin. If pain returns, you can take nitroglycerin again, because it does not accumulate in the body; multiple doses of the drug are possible during the day (up to 6 tablets per day). If your blood pressure is high, you need to lower it to normal levels.
All patients who have suffered an attack of angina pectoris need to have an ECG performed and a decision by a cardiologist on hospitalization.
Why is it necessary to quit smoking? How does smoking worsen angina?
If you smoke and have angina, the best thing you can do to help your heart is to quit smoking!
Studies have shown that the mortality rate in those patients with angina who quit smoking decreased by 2 times compared to those who continued to smoke. Why? Angina is based on a lack of oxygen in the heart muscle, and smoking increases the level of carbon dioxide in the blood, and it displaces oxygen in the blood. This leads to oxygen starvation of the heart muscle. Smoking also increases blood viscosity. Smoking increases the frequency and aggravation of angina attacks and greatly increases the risk of myocardial infarction. Quitting smoking eliminates the adverse effects of nicotine on the coronary arteries, and angina attacks disappear or become less frequent.
Important: replacing cigarettes with cigars and pipe tobacco, switching to cigarettes with less tar and nicotine do not reduce cardiovascular risk!
Contrary to popular belief, abruptly quitting smoking is not harmful; overcoming this bad habit has an undeniable positive effect, regardless of smoking experience.
You need to be prepared for the fact that sometimes depression and irritability occur when quitting smoking, in which case you can seek help from a psychotherapist.
I suffer from angina pectoris, but I dream of losing excess weight. What physical activities are acceptable for people with such problems?
For people suffering from angina, 30–45 minutes of physical activity per day is recommended. The best choice is walking (preferably at a brisk pace) or Nordic walking with ski poles, cycling, swimming. It is important that the exercises do not cause pain, palpitations, or shortness of breath. When practicing swimming or water aerobics, you should remember that cold water can provoke angina attacks, so the water temperature in the pool should be comfortable for you. It is better to do water aerobics under the supervision of a trainer and according to a program specially adapted for people with cardiac problems. In this case, the loads should increase very gradually. However, to lose weight, you need not only physical activity, but also proper nutrition; a nutritionist will help you choose the right menu during your consultation.
Can you have angina if there is no pain?
Unfortunately yes. For example, with diabetes mellitus, diabetic polyneuropathy develops, and the patient may not feel pain, this is the so-called silent ischemia. This condition is dangerous because the patient does not take action in time, and myocardial infarction will develop. In some cases, shortness of breath during exercise can be considered equivalent to pain, so you can suspect the presence of angina pectoris and come for examination to a cardiologist.
Prevention of angina
Angina pectoris is a chronic heart disease that reduces performance and quality of life and can develop into myocardial infarction. Prevention is aimed at treating and monitoring the course of the disease, preventing the development of coronary artery disease. Therefore, it is important to adhere to the recommendations of your doctor and follow all his instructions.
Additional preventive measures include:
- weight control and weight loss, if necessary;
- blood pressure control;
- lifestyle changes: quitting smoking and drinking alcohol;
- diet – give up salty, fatty, spicy, smoked foods;
- stabilization of psycho-emotional state;
- treatment of concomitant diseases - diabetes, obesity;
- physiotherapy.
To prevent the onset of angina, it is important to periodically see a cardiologist. At our center, Federal Scientific and Clinical Center of Federal Medical and Biological Agency, you can undergo a comprehensive heart examination in order to take timely measures to prevent or treat the disease.
Treatment history
Case No. 1
Kirill, 57 years old. Experienced smoker, hypertensive (“working” pressure 150/95 mmHg). Five years ago, according to the patient, he had problems with his heart and blood pressure, was examined, took prescribed medications for six months, then stopped taking them on his own. During the visit to the clinic, attacks of chest pain appeared during physical activity, which went away when the exercise stopped. At the doctor’s appointment, blood pressure is 170/100 mmHg, rapid pulse is 90 beats per minute. The patient was examined - an increase in the level of “bad” cholesterol was detected, ECG and ultrasound of the heart without signs of ischemia, and ischemia was recorded on the 24-hour ECG monitor at the time of significant physical activity, i.e. there is angina pectoris. The patient was given a treatment regimen for angina pectoris, which resulted in normalization of blood pressure and cholesterol levels within 3 months, and a significant increase in exercise tolerance. With the help of a psychotherapist, the patient decided to quit smoking and took up Nordic walking with a gradual increase in loads under the supervision of a cardiologist. Over the past year, angina attacks have not bothered me. It is recommended to continue taking medications and undergo regular preventive examinations.
Thanks to cooperation with doctors and the desire to feel better, the patient was able to change his lifestyle, prevent complications of the disease and prolong his life for many years.
Surgical treatment of angina pectoris
Considering that the main cause of angina is a problem with the diameter of the vessel, surgical treatment is aimed at expanding the latter or creating bypass paths.
Types of operations
- minimally invasive intervention followed by placement of an intravascular stent. The operation is performed using special equipment under constant X-ray control. This operation allows you to cure angina pectoris, which was caused by a narrowing of the coronary vessels;
- coronary artery bypass grafting. With this type of surgical intervention, a path is created to bypass the affected coronary vessels. The operation is complex and expensive, but if possible and indicated, it should not be postponed.
People wondering whether angina can be cured need to know that, unfortunately, it is impossible to completely cure angina, but doctors can improve and prolong your life. The earlier treatment begins, the better the outcome.
Treatment of coronary artery disease and angina pectoris
Treatment is divided depending on the method of exposure to the body. Only a specialist can select a specific method, the optimal drug from the group and the dosage for its use.
Most often the choice is between:
- drugs that dilate blood vessels: nitrates - “Isoket”, “Nitro-mic”, “Nitroglycerin”;
- B-blockers – “Bisoprolol”, “Corvazan”, “Metoprolol”;
- calcium duct blockers - “Corinfar”, “Nifedipine”.
- anticoagulants – “Warfarin”, “Heparin”;
- vitamin complexes – “Thiamin”, “ATP”, “Pyridoxine”;
Drugs for restoring lipid metabolism are mainly statins. The best medications of the group: Lovastatin, Atorvastatin, Atoris.
In acute and severe forms of the pathology, surgical intervention is often prescribed. Mainly consists of bypass surgery of the aortic and coronary vessels. An alternative surgical method is endovascular stenting.
To improve the prognosis for recovery, you should definitely pay attention to pain in the heart area. With a timely visit to a specialist and an accurate description of the symptoms, there is a high probability of eliminating the pathology and preventing the progression of the disease and the onset of a heart attack.
Types of IHD
IHD - exertional angina - is divided into subtypes. Classification is an important procedure, as it allows you to adjust the tactics of treating the disorder, characterize the level of reversibility and the type of course of the pathology.
Angina can be divided according to the condition in the myocardium. With the appearance of necrosis, which characterizes the destruction of an organ, various types of infarction may appear: superficial, widespread and transmural forms.
What is angina
If the myocardium is affected by ischemia and is not destroyed, the pathology has a different course and form. By the nature of their appearance they are defined as:
- angina pectoris - pain occurs during activities associated with physical activity. Additionally, stable and unstable forms are distinguished;
- Angina at rest is characterized by the appearance of symptoms in a state without exercise. There is an additional division into vasospastic angina and Prinzmetal's angina.
Angina pectoris
IHD with exertional angina is characterized by the appearance of compressive pain during physical exertion. The period of time from the start of exercise to the onset of angina determines the severity and intensity of pain. Depending on the severity of the disorder, treatment differs.
Mostly the patient detects characteristic sensations in the area of the heart muscle when walking or climbing, as well as doing work at home. The pain syndrome tends to radiate to the adjacent shoulder, the area under the shoulder blade, the cervical spine or the pharynx. This condition forces you to stop performing any actions that led to the onset of angina. The pain goes away on its own after a short time, and to speed up the relief of symptoms, taking nitrates is indicated.
Risk of death with unstable angina
The disease is further divided into classes depending on the level of tolerance to physical stress. There are 4 main functional classes (FC):
- Good load tolerance. Pain occurs only with a significant increase in load from the usual level for a person. Increasing the duration of the run, the severity of the work, or the duration of the climb helps provoke angina.
- Angina pectoris FC 2 is characterized by average tolerability. The onset of an attack can be caused by a standard load. Angina pectoris 2 FC can be provoked by walking short distances of more than 500 m, climbing several floors, as well as a sharp change in weather conditions.
- Noticeable load limitation. Pain syndrome can occur even when moving from 100 to 500 m or climbing one floor.
- Significant reduction in permissible loads. Even slight effort provokes angina pectoris. Sometimes it occurs in a calm state.
If the condition persists for a long time, when approximately the same intensity of exercise leads to an attack, a diagnosis of a stable form of angina is made. This condition is described as positive, as it indicates the absence of progression of ischemic processes. For some cases, stable angina is the result of treatment measures. The stable form has a relatively positive prognosis and rarely provokes a heart attack. As the pathology progresses, the heart adapts to this condition. If the strength of the pain syndrome or the rate of onset of angina changes, a diagnosis of unstable form is made.
Progressive angina, which occurs with coronary artery disease, is a particularly dangerous disease, since the patient’s condition worsens over time. In the future, the appearance of angina pectoris may occur even in the absence of loads or their insignificant amount.
Stable angina with ischemic heart disease
Angina at rest
The pathological state of pain tends to occur when the body is completely calm. The sensation can appear due to two main reasons:
- The formation of an instant spasm in the arteries, this leads to the rapid onset of ischemia.
- A specific form of Prinzmetal's angina. It is characterized by a rapid appearance, similar to the previous pathology, but the cause of this condition differs - a detached or torn plaque. An atherosclerotic plaque is attached to a vessel on one side, while the other can move freely and at certain stages of time blocks the blood flow. The pathology is extremely dangerous and often leads to a heart attack.
Angina at rest is a dangerous form of pathology, as it occurs as a result of spontaneous changes in the lumen in the vessel. A blocked artery can appear instantly and disappear just as quickly. The condition can resolve on its own or cause a heart attack.
Unstable angina
Doctors can diagnose an unstable form in each of the listed cases, subject to a progressive course or changeable nature of the pathology. This condition is separately identified due to the high risk and danger.
When pain occurs due to physical activity that has not previously provoked an attack, doctors recognize that angina is getting out of control. Relieving symptoms with nitrates does not completely cure the disease. This level of lack of control is typical for the first case of angina.
Rest angina symptoms and treatment
In an unstable form, the patient and the doctor must perform all necessary procedures to find the true cause of the pathology and eliminate the source.
Beta blockers
Beta blockers
– reduce the heart rate (pulse), thereby reducing the work performed by the heart and the need of the heart muscle (myocardium) for oxygen, improving blood supply to the heart, reducing the number of
angina attacks
and increasing exercise tolerance.
Beta blockers prevent and treat abnormal heart rhythms (arrhythmias). This is especially important after a myocardial infarction
, when the arrhythmia often becomes life-threatening.
Regular use of beta blockers can prevent the death of patients who have had a heart attack by up to 40% (in every 40 people out of 100!). Therefore, they are recommended to be prescribed to all patients after a heart attack
, in the absence of contraindications.
Beta blockers normalize blood pressure. In most patients, angina is combined with arterial hypertension
, in this case, taking a beta blocker “kills two birds with one stone” -
we treat hypertension and angina
at the same time. Some beta blockers have been shown to prevent the development of heart failure. These include metaprolol succinate (BetalokZOK), bisoprolol (Concor), nebivalol (Nebilet), carvedilol (Dilatrend). This effect, just like all of the above, is possible only with regular long-term use of the drug.
How to take beta blockers
Take a beta blocker daily, in the morning (long-acting drugs, about 24 hours) or twice a day (morning and evening). The dose of the beta blocker is selected individually. The dose is considered effective if your resting heart rate is 50-60 beats per minute while taking the drug. In this case, all the therapeutic effects of the drug are manifested. You should not suddenly stop taking the beta blocker - in the first days, your pulse may reflexively increase sharply and your health will worsen. In those patients with angina
who take a beta blocker to maintain the correct rhythm and prevent arrhythmia, after discontinuation, interruptions in heart function may resume. Undesirable effects of beta blockers are characteristic mainly of non-cardioselective drugs (for example, decreased potency), and in modern highly cardioselective drugs they occur rarely, usually with increasing doses. It is undesirable to prescribe beta blockers to patients with bronchial asthma and chronic obstructive pulmonary disease COPD), atherosclerotic lesions of the arteries of the lower extremities (atherosclerosis obliterans).
Symptoms and signs of angina
Symptoms of angina pectoris are pronounced during a heart attack:
- Pain behind the chest. Angina pectoris manifests itself as compressive pain after physical exertion, and lasts from 2 5 minutes to 30 minutes. You need to lie down in a horizontal position, calm down and wait in a relaxed state for this pain to subside. If there was a load on the body before the attack, then this pain signals that stable angina is developing. If pain appears in the chest suddenly and without reason, then this is an unstable form of the disease;
- An increased heart rate after physical activity signals the first signs of angina pectoris. If there is an increased heartbeat without obvious reasons, then this is a sign of the development of failure and heart attack;
- Compression in the chest occurs with angina pectoris. The pain radiates to the left side of the body, aching pain in the limbs and neck;
- Depressive state. Unreasonable feelings of anxiety, irritability and restlessness. During an attack of depression, shortness of breath, heart palpitations and panic occur.
Women may experience pain in the lower abdomen, nausea, which can lead to vomiting, and fatigue throughout the body.
The main symptoms of angina are:
- various types of discomfort in the heart (pain, burning, feeling of heaviness, pressure, compression);
- feeling of suffocation or severe pain.
The pain is localized mainly in the epigastrium, back, jaw, and shoulders. The pain syndrome disappears if the patient is given an injection of nitroglycerin or given rest for 5 minutes.
Additional symptoms of angina:
- cough accompanied by intense chest pain;
- pain during physical activity, eating, exposure to cold or emotional stress;
- an attack of angina may also occur in a lying position;
- profuse sweating;
- feeling tired;
- nausea.
Symptomatic manifestations of stable angina are usually temporary and last about 15 minutes. This is its main difference from unstable angina, the symptoms of which may not go away within a day and can be very intense.
Diagnosis of the disease
Patient complaints are very important to make a correct diagnosis. The doctor will need information about:
- the location of pain and irradiation of pain to other parts of the body;
- frequency of angina attacks, their duration and strength.
- whether physical activity provokes attacks;
- how the patient manages to relieve pain.
Laboratory tests include a blood test to check for the development of atherosclerosis, as the main possible cause of vascular damage. To make a correct diagnosis, instrumental examinations are also carried out:
- Electrocardiogram as the main way to obtain information about cardiac disorders;
- Daily Holter monitoring to track the dynamics of changes during each attack of angina;
- An echocardiogram, which allows you to see the changes that have occurred during the development of coronary artery disease;
- Velgoergometry, which allows you to determine the maximum physical activity that a patient can endure without the threat of developing coronary artery disease.
- Diagnostic coronography, which allows you to assess the condition of the heart arteries.