Angina pectoris
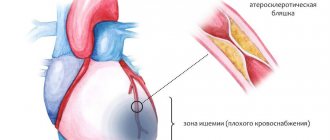
Angina pectoris (from the Latin stenocardia - compression of the heart, angina pectoris - angina pectoris) is one of the main forms of coronary artery disease and is characterized by paroxysmal pain in the chest or in the region of the heart. The occurrence of painful (anginal) attacks is determined by the established relationship of two main factors: anatomical and functional. It has been proven that in the vast majority of cases with typical angina, we are talking about atherosclerosis of the coronary arteries, leading to a narrowing of their lumen and the development of coronary insufficiency. An attack of angina occurs as a result of a discrepancy between the need of the heart muscle for oxygen and the ability of the vessels feeding it to deliver the required amount. The result is ischemia, manifested by pain. Pain syndrome is a signal of trouble, a “cry” of the heart for help. As atherosclerosis of the coronary arteries progresses, attacks of angina pectoris become more frequent. Angina pectoris is the most common form of angina pectoris, it can be: new, stable and progressive. Effortful angina, new-onset New-onset angina includes angina that lasts up to 1 month from the moment of onset. The clinical symptoms of new-onset angina pectoris are similar to the symptoms of stable angina described below, but, unlike it, it is very diverse in its course and prognosis. For the first time, exertional angina can become stable, take a progressive course, and even lead to the development of myocardial infarction. In some cases, regression of clinical symptoms may be observed. Considering this variability in the course of new-onset angina, it is proposed to classify it as unstable angina until it stabilizes. Stable angina pectoris Stable angina pectoris is angina that exists for more than 1 month and is characterized by stereotypical (similar to each other) attacks of pain or discomfort in the heart in response to the same load. The stable form of angina pectoris is currently divided into 4 FCs. — Class I stable angina includes cases when attacks occur only during high-intensity loads performed quickly and for a long time. This type of angina is called latent angina. — FC II angina is characterized by attacks that occur when walking quickly, climbing a hill or stairs above the 1st floor, or walking at a normal pace over a long distance; there is some limitation of usual physical activity. This is a mild degree of angina. — Angina pectoris of FC III is classified as moderate in severity. It appears during normal walking, going up to the 1st floor, and attacks of pain may appear at rest. Ordinary physical activity is noticeably limited. — IV angina pectoris is severe angina pectoris. Attacks occur with any physical activity, as well as at rest. “Thus, determining the functional class of a patient with stable angina is the most important indicator of the severity of the disease and helps to predict its course, and also makes it possible to choose the optimal treatment.
Clinical picture of an angina attack
- Pain (squeezing, pressing, burning, aching) or a feeling of heaviness behind the sternum, in the heart area, radiating to the left shoulder, shoulder blade, arm and even wrist and fingers. - There is a feeling of fear of death. — The occurrence of pain is usually associated with physical activity or emotional experiences. — Angina attacks appear when blood pressure rises, during sleep, when going out into the cold, after a heavy meal, alcohol and smoking. — Pain, as a rule, goes away within 1-5 minutes after stopping the exercise and taking nitroglycerin. The clinical picture of an attack of angina pectoris was first described by the English physician W. Heberden in 1768. Currently, the criteria for angina pectoris developed by the American Heart Association are used, determined during a survey of patients. According to these criteria, typical exertional angina is characterized by the presence of three signs: - pain (or discomfort) behind the sternum; - connection of this pain with physical or emotional stress; - disappearance of pain after stopping exercise or taking nitroglycerin. The presence of only two of the three listed signs indicates atypical (possible) angina, and the presence of only one sign does not provide grounds for establishing a diagnosis of angina. The main symptom of angina is a sudden onset of pain, which in a few seconds reaches a certain intensity that does not change throughout the attack. Most often the pain is localized behind the sternum or in the heart area, much less often in the epigastric region. By its nature, the pain, as a rule, is compressive, less often - pulling, pressing, or is felt by the patient in the form of a burning sensation. Irradiation of pain to the left arm (ulnar part of the left arm), the area of the left shoulder blade and shoulder is considered typical. In some cases, pain is felt in the neck and lower jaw, rarely in the right shoulder, right shoulder blade and even in the lumbar region. Some patients note a feeling of numbness or coldness in the area of pain irradiation. The area of pain irradiation to a certain extent depends on the severity of the angina attack: the more severe it is, the wider the area of irradiation, although this pattern is not always observed. Sometimes during an attack of angina, no pronounced pain syndrome occurs, but a vague feeling of tightness, awkwardness, and heaviness behind the sternum appears. These sensations sometimes cannot be clearly defined verbally, and the patient, instead of describing them verbally, places his hand on the sternum area. In some cases, patients are bothered by pain only under the left shoulder blade, in the shoulder, lower jaw or in the epigastric region. In some cases, pain during angina pectoris may not be localized behind the sternum, but only or predominantly in an atypical area, for example, only in places of irradiation or in the right half of the chest. Atypically localized pain should be properly assessed. If it occurs at the height of the load, goes away at rest, after taking nitroglycerin, it is necessary to assume angina and conduct an appropriate instrumental study to confirm the diagnosis. In some patients, angina pectoris may manifest itself as an attack of suffocation, caused by a decrease in the contractile function of the heart resulting from coronary insufficiency and the development of blood stagnation in the pulmonary circulation. Many patients experience a connection between angina attacks and the unfavorable effects of cold, head winds, and large meals. Severe anginal attacks can be provoked by smoking, especially against the background of intense mental work. According to statistical studies, smokers develop angina 10-12 times more often than non-smokers. An important circumstance of diagnostic significance is the connection of attacks with physical or psycho-emotional stress. Since physical activity causes and intensifies pain, the patient tries not to move during an attack. Factors that provoke an attack of angina pectoris can also be sexual intercourse and tachycardia of any origin (fever, thyrotoxicosis, etc.). As a rule, the pain syndrome lasts from a few seconds to 1 - 5 minutes, extremely rarely - up to 10 minutes and disappears as suddenly as it appears. In stable angina, the pain is stereotypical: it occurs in response to certain loads and is identical in intensity, duration and zones of irradiation. The course of angina pectoris in many patients is wave-like: periods of rare occurrence of pain alternate with their frequency and increased intensity of the attack. A change in the nature of the pain syndrome may indicate progression, severity of the disease, and its transition to an unstable form. In this case, attacks occur with less stress than before, become more frequent and severe, the intensity of pain and its duration increase, and the area of irradiation of pain becomes larger. In addition to pain, an attack of angina may be accompanied by general weakness, weakness, a feeling of melancholy or a feeling of fear of death. The skin is often pale, sometimes showing redness and moderate sweating. Palpitations often occur, pulse quickens, and blood pressure rises moderately. At the end of the attack, a feeling of weakness remains, and sometimes an increased amount of light-colored urine is released. Unstable angina is a reason to assume the possibility of developing myocardial infarction. Such patients are subject to hospitalization. Of particular importance in recognizing an attack of angina has long been attached to the assessment of the effect of nitroglycerin, after taking which the pain usually disappears after 1-3 minutes, and its effect lasts for at least 15-25 minutes. A more severe form of angina pectoris is resting angina. The addition of pain that occurs at rest, often at night during sleep, to angina pectoris is an unfavorable sign indicating the progression of stenosis of the coronary arteries and deterioration of the blood supply to the heart muscle. This form of angina pectoris is more common in old age, in people who also suffer from hypertension. Pain attacks that occur at rest are more painful and last longer. Relieving pain requires more intensive therapy, because taking nitroglycerin does not always completely relieve it. Rest angina is an extreme variant of progressive, unstable angina. Despite the various “masks” of an angina attack, almost all of its manifestations are paroxysmal. Spontaneous angina (Prinzmetal's angina) Some patients with coronary artery disease experience episodes of local spasm of the coronary arteries in the absence of obvious atherosclerotic lesions. This pain syndrome is called variant angina, or Prinzmetal's angina. In this case, oxygen delivery to the myocardium is reduced due to intense spasm, the mechanism of which is currently unknown. The pain syndrome is often intense and prolonged and occurs at rest. Relatively low effectiveness of nitroglycerin was noted. Emergency hospitalization is indicated. The prognosis is serious, there is a high probability of developing myocardial infarction and SCD. Silent (painless, asymptomatic) form of coronary heart disease. A fairly significant proportion of episodes of myocardial ischemia can occur without symptoms of angina pectoris or its equivalents until the development of IBS. According to the Framingham study, up to 25% of myocardial infarctions are first diagnosed only by retrospective analysis of a series of ECGs, and in half of the cases they are completely asymptomatic. Severe atherosclerosis of the coronary arteries can be asymptomatic and is detected only at autopsy in people who died suddenly. With a high degree of probability, the presence of BBIM can be assumed in individuals without clinical signs of IHD, but with several CVD risk factors. In case of multiple risk factors, it is recommended to have a SM ECG, and if BBIM is detected, an in-depth examination including coronary angiography (CAG). In some cases, exercise testing and stress echocardiography are indicated. IHD often manifests itself only as cardiac arrhythmias without pain. In these cases, one should first assume BBIM, immediately take an ECG and hospitalize the patient in a specialized cardiology department. Emergency care for angina pectoris If a patient experiences pain in the heart area, you should immediately call a doctor, before whose arrival the nurse should provide first aid.
Tactics of the nurse before the doctor arrives:
- reassure the patient, measure blood pressure, count and evaluate the nature of the pulse; - help to take a semi-sitting position or lay the patient down, ensuring him complete physical and mental rest; - give the patient nitroglycerin (1 tablet - 5 mg or 1 drop of a 1% alcohol solution on a piece of sugar, or a validol tablet under the tongue); - place mustard plasters on the heart area and on the sternum; in case of a prolonged attack, leeches on the heart area are indicated; — take Corvalol (or Valocordin) 30-35 drops orally; - Before the doctor arrives, carefully monitor the patient’s condition. The nurse should know the mechanism of action of nitroglycerin, which is still the drug of choice for attacks of angina pectoris. The sooner a patient with an attack of angina takes nitroglycerin, the easier the pain is relieved. Therefore, you should not hesitate to use it or refuse to prescribe the drug due to the possible occurrence of headache, dizziness, noise and a feeling of fullness in the head. The patient should be convinced to take the drug and, at the same time, an analgesic for headaches can be given orally. Due to the significant peripheral vasodilating effect of nitroglycerin, in some cases the development of fainting and very rarely collapse is possible, especially if the patient suddenly stood up and assumed a vertical position. The effect of nitroglycerin occurs quickly, after 1-3 minutes. If there is no effect 5 minutes after a single dose of the drug, it should be re-administered at the same dose. For pain that is not relieved by two doses of nitroglycerin, further use is useless and unsafe. In these cases, one must think about the development of a pre-infarction condition or myocardial infarction, which requires the use of stronger medications prescribed by a doctor. The emotional stress that caused the attack and accompanied it can be eliminated by the use of sedatives. A nurse in critical situations for a patient must show restraint, work quickly, confidently, without excessive haste and fussiness. It must be remembered that patients, especially those with diseases of the circulatory system, are suspicious, therefore communication with the patient should be very delicate, careful, tactful, as a real professional nurse should be. The effect of treatment, and sometimes the life of the patient, depends on how competently the nurse is able to recognize the nature of pain in the heart area.
Nursing process for angina pectoris
Patient's problems Present: - complaints of pain in the heart area (behind the sternum), compressive, occurring during physical activity and after excitement, and sometimes at rest. The pain is relieved by taking nitroglycerin (after 2-4 minutes), but after the attack there is a headache; - pain in the heart area is sometimes accompanied by short-term interruptions in the heart area; - shortness of breath on exertion. Physiological: - difficulties with defecation. Psychological: - the patient is very worried about the unexpectedness of his illness, which has disrupted his life plans and also reduced his quality of life. Priority: - shortness of breath on exertion. Potential: - pain in the heart area, which occurs at rest, indicates the progression of the disease, myocardial infarction may develop. Lack of knowledge: - about the causes of the disease; - about the prognosis of the disease; - the need to take prescribed treatment; — about risk factors; - about proper nutrition; - about self-care. Actions of the nurse Carrying out general care for the patient: - changing underwear and bed linen, feeding the patient according to the prescribed diet, ventilating the room (make sure there are no drafts); — fulfillment of all doctor’s prescriptions; — preparing the patient for diagnostic studies. Teaching the patient and his relatives how to properly take nitroglycerin during an attack of pain. Teaching the patient and his relatives to keep an observation diary Conducting conversations: - consolidate in the patient’s mind the fact that during an attack of angina, myocardial infarction can develop, and in the absence of careful attitude to one’s health, the attack can end in death; — convince the patient of the need to systematically take antianginal and lipid-lowering medications; - the need to change your diet; - about the need to constantly monitor your condition. Conversation with relatives regarding the need to follow a diet and monitor the timely intake of medications. Motivate the patient to change lifestyle (reduce risk factors). Counsel patient/family on prevention. Complications of angina: - acute myocardial infarction; — acute rhythm and conduction disturbances (up to SCD); - acute heart failure. Indications for hospitalization: - new-onset angina pectoris; - progressive angina pectoris; - angina pectoris that first appeared at rest; - spontaneous (vasospastic) angina. All patients with the above types of angina should be urgently hospitalized in specialized cardiology departments.
Principles of diagnosing ischemic heart disease
Diagnosis of angina pectoris during a painful attack The diagnosis of angina pectoris is often based on the following main signs: - the nature of the pain - compressive; - localization of pain - usually behind the sternum; - irradiation of pain - to the left shoulder girdle, to the lower jaw; - conditions of occurrence - physical stress, psycho-emotional arousal, exposure to cold; - the attack may be accompanied by tachycardia, moderate hypertension; - the temperature is normal; — clinical blood test is unchanged; - pain goes away after taking nitroglycerin or with rest. Primary assessment of the patient's condition The clinical diagnosis of angina is made on the basis of a detailed qualified survey of the patient, a thorough study of his complaints and a careful study of the anamnesis. All other research methods are used to confirm or exclude the diagnosis and clarify the severity of the disease - prognosis. Although in many cases the diagnosis can be made based on complaints, it should be borne in mind that the patient does not always accurately describe his feelings. Therefore, recently attempts have been made to create a so-called standardized questionnaire for patients suffering from angina (of course, its full use is possible in the interictal period). During the initial examination, before obtaining the results of an objective examination, it is necessary to carefully evaluate the patient’s complaints. Pain in the chest can be classified depending on the location, provoking and relieving factors: typical angina, probable (atypical) angina, cardialgia (non-coronary chest pain). With atypical angina, of the three main characteristics (all signs of pain, connection with physical activity, pain-relieving factors), two of them are present. With non-coronary chest pain, only one of the three characteristics occurs or they are absent altogether. For a correct diagnosis, the patient's habitus is important. When examining a patient during an attack of angina, a frightened facial expression, dilated pupils, perspiration on the forehead, somewhat rapid breathing, pale skin. The patient is restless and cannot lie still. There is an increase in heart rate and often an increase in blood pressure, and various heart rhythm disturbances are possible. In many patients, hypertension may have existed before the onset of angina, and an additional increase in blood pressure can only increase clinical symptoms. On auscultation, as a rule, tachycardia (rarely bradycardia) and muffled tones are noted.
Additional research methods for ischemic heart disease
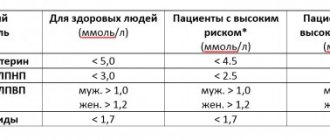
Laboratory tests: - clinical blood test; - biochemical blood test: determination of total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, hemoglobin, glucose, AST, ALT in the blood. Instrumental diagnosis of myocardial ischemia: - recording ECG at rest; — ECG registration during an attack; — stress ECG tests (VEM, treadmill test); — EchoCG and stress echocardiography; — Holter 24-hour ECG monitoring (with MECG); — myocardial scintigraphy; — MRI; — KAG. Differential diagnosis with Cardiac neurosis Osteochondrosis Diaphragmatic hernia High gastric ulcer Angina pectoris must also be differentiated from syphilitic aortitis. Pain in the chest also occurs with other diseases, which should be remembered in case of atypical variants of coronary artery disease. Cardiovascular: - dissecting aortic aneurysm; - pericarditis; - pulmonary embolism. Pulmonary: - pleurisy; - pneumothorax; - lung cancer. Gastrointestinal: - esophagitis; - spasm of the esophagus; - reflux esophagitis; - intestinal colic. — Psychoneurological: — state of anxiety; - the heat of passion. Associated with the chest: - fibrositis; - injuries to the ribs and sternum; - intercostal neuralgia; - herpes zoster (before the rash stage). A separate category is reflex angina, which occurs due to pathology of nearby organs: peptic ulcer, cholecystitis, renal colic, etc. Prognosis of the course of coronary artery disease The quality and life expectancy of a patient with angina depends on: - early detection of the disease; — compliance with the regimen of taking prescribed medications; — lifestyle changes and elimination of risk factors. In other words, if you make certain changes in your lifestyle and take recommended medications, you can continue to live a full life. The main conditions for this are an understanding of the essence of the condition and the patient’s willingness to cooperate with medical personnel. Treatment and treatment goals : - improve the prognosis and prevent the occurrence of myocardial infarction or SCD and accordingly increase life expectancy; - reduce the frequency and intensity of angina attacks in order to improve the quality of life. The choice of treatment method depends on the response to initial drug therapy, although some patients immediately prefer and insist on surgical treatment - TKA, CABG. In the selection process, the patient’s opinion is taken into account, as well as the ratio of price and effectiveness of the proposed treatment. Non-drug treatment of angina pectoris includes: lifestyle changes and counteracting risk factors for coronary artery disease. Drug treatment of angina pectoris 1. Antianginal (anti-ischemic) therapy This treatment is prescribed to patients with attacks of angina or when diagnosing episodes of myocardial ischemia using instrumental methods. Antianginal drugs include: - beta blockers; - calcium antagonists; - nitrates; - nitrate-like drugs; — myocardial cytoprotectors. It is recommended that these classes of drugs be prescribed in this order for the treatment of stable angina, and that they be used in various combinations. Drugs that are not recommended to be prescribed to patients for the treatment of angina pectoris: vitamins and antioxidants, female sex hormones, riboxin, adenosine triphosphate (ATP), cocarboxylase. 2. Medicines that improve the prognosis in patients with angina pectoris. They are recommended for all patients diagnosed with angina pectoris in the absence of contraindications. Antiplatelet drugs, more correctly called antiplatelet agents (acetylsalicylic acid - ASA, clopidogrel) are mandatory treatments for stable angina. All patients after myocardial infarction are recommended to be prescribed a BB without internal sympathomimetic activity: metoprolol, bisoprolol, propranolol, atenolol. Lipid-lowering drugs Beta-blockers (selective action) - Metoprolol (betaloc ZOK, Corvitol, Egilok, Emzok) 50-200 mg 2 times a day. — Atenolol (atenolan, tenormin) 50-200 mg 1-2 times a day. — Bisoprolol (bisogamma, concor, concor cor) 10 mg/day. — Betaxolol (betak) 10-20 mg/day. — Pindolol (Wisken) 2.5-7.5 mg 3 times a day. — Nebivolol (nebilet) 2.5-5 mg/day. - Carvedilol (acridilol, Dilatrend, Cardivas) - 25-50 mg 2 times a day. Calcium antagonists 1. Dihydropyridine - Nifedipine - moderately prolonged (adalat SL, cordaflex retard, corinfar retard) 30-100 mg/day; significantly prolonged (osmo-adalat, cordipin CL, nifecard CL) 30-120 mg/day. — Amlodipine (norvasc, cardlopin, normodipine, kalchek, amlovas, vero-amlodipine) 5-10 mg/day. — Felodipine 5-10 mg/day. — Isradipine 2.5-10 mg 2 times a day. — Lacidipine 2-4 mg/day. 2. Non-dihydropyridine - Diltiazem (diltiazem-Teva, diltiazem Lannacher) 120-320 mg/day. - Verapamil (isoptin, lecoptine, finoptin) - 120-480 mg/day. Nitrates and nitrate-like drugs 1. Nitroglycerin preparations - Short-acting (nitromint, nitrocor, nitrospray) 0.3-1.5 mg sublingually for angina pectoris. — Long-acting (nitrong forte) 6.5-13 mg 2-4 times a day. 2. Preparations of isosorbide dinitrate - Long-term action (cardiquet 40, carditet 60, carditet 120, iso Mac retard) 40-120 mg/day. — Moderate duration of action (isolong, cardiket 20, iso Mak 20, nitrosorbide) 20-80 mg/day. 3. Preparations of isosorbide mononitrate - Moderate action (monosan, monocinque) 40-120 mg/day. - Long-acting (olicard retard, monocinque retard, pectrol, efox long) 40-240 mg/day. 4. Molsidomine preparations - Short-acting (Corvaton, Sidnopharm) 4-12 mg/day. — Moderate duration of action (dilasid) 2-4 mg 2-3 times a day. — Long-acting (dilasidom retard) 8 mg 1-2 times a day. Surgical treatment of coronary artery disease The main indication for surgical treatment of coronary artery disease is the persistence of severe angina (FC III-IV), despite intensive drug treatment. The indications and nature of surgical treatment are specified based on the results of coronary angiography and depend on the degree, prevalence and characteristics of coronary artery lesions. Patients with frequent attacks of angina pectoris and insufficient drug therapy or those with multiple risk factors, including a family history of sudden death, should undergo angiographic examination of the coronary arteries. If narrowing of the main left trunk of the coronary artery and changes in 3 coronary arteries are detected, myocardial revascularization is indicated. Myocardial revascularization includes - Various types of TKA (transcutaneous angioplasty) with the installation of a metal frame - an endoprosthesis (stent), burning out the plaque with a laser, destroying the plaque with a rapidly rotating drill and cutting off the plaque with a special atherotomy catheter. — CABG surgery to create an anastomosis between the aorta and the coronary artery below the site of narrowing to restore effective blood supply to the myocardium. Currently, there is a definite tendency to bypass the maximum possible number of coronary arteries using autoarteries. For this purpose, the internal mammary arteries, radial arteries, right gastroepiploic and inferior epigastric arteries are used. Vein grafts are also used. Despite the quite satisfactory results of CABG, angina returns in 20-25% of patients within 8-10 years. Such patients are considered candidates for reoperation. More often, the return of angina is caused by the progression of coronary atherosclerosis and damage to autovenous shunts, which leads to stenosis and obliteration of their lumen. Shunts are especially susceptible to this process in patients with risk factors: hypertension, diabetes mellitus, dyslipidemia (DLD), smoking, obesity. Medical examination of patients with coronary heart disease Patients with coronary artery disease and various types of angina are subject to medical examination in cardiology centers or cardiology clinics for life.
We recommend reading:
- Nursing process in atherosclerosis
- Nursing process in myocardial infarction
- Nursing process for rheumatism
- Nursing process for pain
- Fifth stage of the nursing process
Contents of the nursing process and its basic principles
Nursing process is a type of medical intervention that meets the needs of certain groups of patients. Its goal is to determine the necessary health measures and select the most effective of them for use in each specific case. In general, the nursing process involves dividing it into three parts - care planning, its implementation and the final assessment of the result.
- systematic and planned;
- individual approach;
- strict adherence to professional standards;
- indispensable participation in the process of the patient himself and his family members.
Today, professional standards require that the nurse not only perform the necessary medical procedures. She must explain to the patient what she is doing and what the goals of her actions are. Currently, in our country, nursing and medical processes are equal in importance to each other and are two interdependent elements of the overall treatment process.
In our country, where heart disease is already epidemic, the role of the nurse is of unprecedented importance. Providing effective assistance to a patient requires knowledge of all the features of the disease. No wonder she is one of the main characters in hospitals. It is the sister who treats the patient - gives injections, IVs, performs care procedures and monitors his condition.
- 1 FC – latent angina, when an attack is a consequence of strong and short-term physical activity;
- FC 2 – mild degree, when pain appears with slight excess of normal physical activity;
- 3 FC – angina pectoris of moderate severity, which occurs even with little physical activity;
- 4 FC – severe angina that occurs even at rest.
If a nurse provides patronage to a patient at home, she must keep a special diary in which the patient’s condition, his complaints, medication intake and all nursing care actions are recorded.
To correctly assess the patient’s condition, the nurse must be able to differentiate the clinical symptoms of angina:
- determine the location of pain;
- assess the patient’s appearance – skin color, facial expression, presence of perspiration, condition of the pupils, posture, ability to communicate;
- conduct a survey to determine the intensity of pain and its nature.
Based on the patient’s complaints, the further process of providing nursing pre-hospital care is built. Also, the observations of a nurse will help the doctor when making a diagnosis and prescribing treatment.