0
Author of the article: Marina Dmitrievna
2017.06.19
2 224
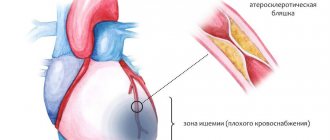
Ischemia
Diagnosis of coronary heart disease (CHD) is a series of medical studies aimed at detecting coronary heart disease in a patient and determining the nature and stage of development of the disease. The examination is carried out as prescribed by a doctor or at the request of the patient for prevention.
History taking
First of all, the doctor finds out what the patient is complaining about.
With typical angina, the patient is bothered by chest pain, which has characteristic features. It is pressing, squeezing, burning, and always occurs in the same place at the same level of load. With rest or under the influence of nitroglycerin, such pain quickly passes. It can “give” to the neck, jaw, arm.
It is clarified how long ago the pain began, what treatment the patient took, and whether it was effective. Concomitant diseases that can increase the lack of oxygen in the myocardium are identified. They are divided into 2 groups: increasing the need for oxygen and reducing its supply to the body.
The first group includes non-cardiac conditions such as fever, increased thyroid function (hyperthyroidism), and emotional agitation. Of the heart diseases, hypertrophic cardiomyopathy, tachycardia and aortic heart disease increase the oxygen consumption of the heart.
Reduce the supply of oxygen to the body:
- anemia of various origins;
- pneumonia - pneumonia;
- chronic pulmonary diseases;
- increased pressure in the pulmonary artery - pulmonary hypertension;
- sleep apnea syndrome;
- leukemia, increased blood clotting.
Among heart diseases, it is important to note heart defects and circulatory failure.
The doctor finds out some circumstances of the patient’s life - smoking, drinking alcohol, professional route, past illnesses. He clarifies whether there are cases of cardiac pathology in the family.
For information about the risk factors for coronary artery disease and for which complaints you should consult a cardiologist, watch this video:
Causes
IHD occurs as a result of atherosclerosis of large (epicardial) coronary (heart) arteries of varying degrees: from a slight narrowing of the lumen in the vessel to its complete blockage by atheroma (cholesterol, fat) masses or a blood clot that has developed at the site of a “vulnerable” (damaged) atherosclerotic plaque (ASP) . Other causes of IHD are spasm of the coronary arteries and damage to the microvasculature in the myocardium. In most cases, they also develop against the background of existing atherosclerosis.
It is possible to identify the population groups most susceptible to the development of coronary artery disease: people suffering from high blood pressure, those addicted to smoking, those suffering from high cholesterol levels, diabetes mellitus, and chronic kidney diseases. . Male gender and old age are also powerful risk factors for the development of coronary artery disease.
Medical examination
During an external examination, body mass index and waist circumference are determined, pulse rate and blood pressure are measured in both arms.
Xanthomas on the eyelids
You can detect external signs of atherosclerosis - xanthomas on the eyelids, clouding of the edge of the cornea, pallor of the extremities and others.
Auscultation does not reveal specific signs of ischemic heart disease. Sometimes the 3rd and 4th heart sounds, noise during systole (contraction) of the heart, pulsation in the pericardial zone, indicating a large aneurysm, are recorded.
Analyzes
Blood tests help identify factors that increase the risk of heart disease and possible causes of the disease.
Tests for coronary artery disease (angina) with a suspected diagnosis:
- general blood test with determination of hemoglobin;
- biochemical analysis with determination of glucose, cholesterol (TC), triglycerides (TG), high-density lipoproteins (HDL) and low-density lipoproteins (LDL), aspartate aminotransferase (AST) and alanine aminotransferase (ALT).
Once the diagnosis is confirmed, all patients are prescribed the following tests:
- lipid spectrum (TC, TG, HDL, LDL);
- glucose level;
- general blood test with determination of hemoglobin and leukemia;
- biochemical analysis for creatinine content.
Lipid spectrum norms depending on concomitant pathology and risk factors
When signs of unstable angina appear, a blood test for troponins, markers of cardiac muscle necrosis, is prescribed for coronary artery disease. If there is a probable pathology of the thyroid gland, its hormones are examined.
Urinalysis reveals no specific changes.
In diagnostically unclear cases, doctors prescribe:
- glucose load test;
- biochemical blood test for ischemic heart disease: C-reactive protein, lipoprotein (a), ApoA, ApoB, terminal fragment of brain natriuretic peptide.
We recommend reading about the troponin test for myocardial infarction. You will learn about what troponin is, about two types of troponin in diagnosing myocardial infarction, reliable and high-quality methods for diagnosing a heart attack. And here is more information about what an ECG looks like during myocardial ischemia.
Treatment of coronary artery disease
Treatment of coronary heart disease is complex and can be either medicinal (conservative and surgical) or non-medicinal.
Non-drug treatment of coronary artery disease includes addressing risk factors: eliminating unhealthy diets, reducing excess body weight, normalizing physical activity and blood pressure, as well as correcting carbohydrate metabolism disorders (diabetes mellitus).
Drug treatment is based on the prescription of various groups of drugs for the most complete and comprehensive treatment. The following main groups of drugs are distinguished:
- Nitrates
- Short-acting - used to relieve an attack and are not suitable for treatment. These include nitroglycerin, the effect of which occurs within a few minutes (from one to five).
- Long-acting - these include isosorbide mono- and dinitrate, used to prevent attacks.
- Beta blockers - to reduce myocardial contractility:
- Selective (block only one type of receptor) - metoprolol and atenolol.
- Non-selective (block all sympathetic receptors that are located both in the heart and in other organs and tissues) - propranolol.
- Antiplatelet agents (aspirin, clopidogrel) - reduce blood clotting by affecting platelet aggregation.
- Statins - simvastatin, nystatin (reduce the concentration of cholesterol in low-density lipoproteins, that is, they affect risk factors).
- Metabolic agents – preductal, increases oxygen delivery to the heart muscle.
- Angiotensin-converting enzyme inhibitors (lisinopril, ramipril) or angiotensin receptor blockers (losartan, valsartan).
It is possible to use combinations of these drugs.
What will electrocardiography and echocardiography show?
At rest, there are most often no changes on the ECG. If a recording can be made during a painful episode, it reveals a horizontal downward displacement of the ST segment. With more severe ischemia, the ST segment rises above the isoline. These changes disappear after the pain stops.
On a resting ECG, traces of myocardial infarction suffered in the past can be detected, and concomitant rhythm disturbances and intracardiac conduction can be identified. This data is important not only for diagnosis, but also for selecting the correct treatment.
Echocardiography (EchoCG) is prescribed to distinguish between ischemic heart disease and other heart diseases. It is performed in the following cases:
- heart murmurs indicating a defect or hypertrophic cardiomyopathy;
- heart failure;
- previous heart attack;
- abnormal resting ECG, such as bundle branch block or abnormal Q wave.
Load tests
ECG changes characteristic of this disease appear only when the heart rate increases. To achieve a rapid pulse, doctors use various loading techniques.
ECG test with physical activity
This test is considered the first step in diagnosing angina pectoris.
It is performed on a stationary exercise bike (bicycle ergometer) or treadmill (treadmill). The load on the patient increases in steps. The doctor monitors the ECG on the monitor. When symptoms of ischemia appear, the test is considered positive.
Such a study detects the disease in 68% of cases. In 23% of cases, a positive test does not mean the presence of coronary artery disease in 23 out of 100 patients. Therefore, the data obtained cannot serve as the basis for a final diagnosis.
Bicycle ergometry or treadmill test should be prescribed to all patients if there are complaints and there are no contraindications.
Transesophageal electrical stimulation
If it is impossible to perform a regular stress test or if it is uninformative, TEES can be used. During the procedure, a thin probe is inserted into the patient's esophagus. Through it, electrical impulses are sent to the heart, increasing the heart rate. When the required heart rate is achieved, the doctor evaluates ischemic changes using an ECG.
Stress EchoCG
The technique is based on the fact that with the development of myocardial ischemia, its contractility first decreases, then ECG changes appear, and only then an attack of pain. Stress echocardiography is more informative than a stress test, but is more technically complex.
First, the patient undergoes a conventional echocardiography. Then the heart rate is increased using a bicycle ergometer, treadmill, TES or medications (dobutamine, dipyridamole, ergonovine, adenosine). Then the echocardiography is repeated and searches for areas of the heart muscle with reduced contractility. This confirms ischemia.
Perfusion scintigraphy with stress
The technique is comparable in value to stress echocardiography and is used when ultrasound of the heart fails to obtain a high-quality image (for example, in obesity).
During the study, a radioactive isotope is injected intravenously, which is distributed in the heart muscle in proportion to the intensity of blood flow. Thus, areas poorly supplied with blood will be clearly visible on the monitor screen. The sensitivity of the method reaches 90%. The last 2 methods are shown in such cases:
- changes in the ECG at rest, preventing the performance of a stress test;
- diagnostic doubts after the remaining studies performed.
They are useful in recognizing CAD in women, as well as in selecting an artery for revascularization.
Prevention
Preventing a disease is much easier than curing it. To maintain healthy arteries and blood vessels, it is necessary to eliminate risk factors that negatively affect your health:
- To give up smoking;
- Monitoring blood pressure levels
- Normalization of the level of “bad” cholesterol (low-density lipoproteins)
- Fighting stress and depression
- Minimize alcohol consumption;
- Refusal of smoked, fatty, fried and salty foods.
Spend more time on an active lifestyle: moderate physical activity, therapeutic exercises, morning exercises, walking, swimming, dancing. Physical activity will help strengthen the walls of blood vessels and maintain normal weight, and if necessary, reduce it.
The most important thing in prevention is timely observation by a specialist. In order not to visit medical institutions several times to undergo all the necessary tests and examinations, contact our cardiology center. Federal Research Center FMBA offers patients several programs for comprehensive heart research. You can find them here.
Multislice computed tomography of the heart and its vessels
The technique is based on an x-ray examination of the heart using special equipment. It is indicated for the following patients:
- men over 45 years old and women over 55 years old to detect the first signs of coronary artery disease;
- patients under 65 years of age with atypical pain syndrome;
- questionable stress test results in people under 65 years of age;
- the need to exclude myocarditis or cardiomyopathy.
To learn about what multislice cardiac computed tomography (MSCT) is, watch this video:
Coronary angiography
This is the main diagnostic method that allows not only to diagnose coronary artery disease, but also to determine how best to treat the patient - with medications or surgery. It is based on the introduction of an X-ray contrast agent into the bloodstream, which does not pass through the clogged vessels of the heart.
Indications:
- angina pectoris III – IV functional classes (attacks with little exertion and at rest), especially when medications are ineffective;
- previous cardiac arrest;
- dangerous ventricular arrhythmias;
- recurrence of angina after surgical treatment;
- a dubious diagnosis for people in certain professions (drivers, pilots, train drivers).
The arrow indicates partial obstruction of the coronary artery
Why is it worth getting diagnosed with coronary artery disease at the CBCP clinic?
The Circulatory Pathology Center will help you maintain your health thanks to:
- qualified cardiologists - doctors of the highest category with 15-20 years of experience in leading medical institutions of the Russian Federation;
- doctors of functional diagnostics, some of whom underwent specialized training in Frankfurt, training at the Scientific Center for Surgery named after. A.N. Bakuleva;
- premium diagnostic expert equipment of Italian, Japanese, Swiss production;
- the latest diagnostic methods that identify the slightest defects and disturbances in the functioning of the myocardium, which allows timely initiation of effective treatment.
Timely examination for coronary artery disease is the key to your safety and longevity!