Heart problems occur in most people who have crossed the age limit of maturity, and often at a younger age, and even in children.
Traditionally, the doctor prescribes an examination: in some cases, electrocardiography, in others, echography, and often both methods. Which study is preferable? What is better - ultrasound of the heart or ECG? In order to get an answer to this question, which patients often ask, it is necessary to know about the features of each of the methods: to whom they are indicated and to whom they are contraindicated, and what their diagnostic capabilities are.
Indications for cardiac examination
Additional methods of cardiac examination are prescribed for the following purposes:
- conducting primary diagnostics of various diseases;
- monitoring the dynamics of the condition during treatment and after it;
- round-the-clock monitoring of the condition after surgery, severe injuries, after a stroke, heart attack;
- for preventive purposes - during medical examinations in persons over 40 years of age;
- for early detection of pathology in people at risk, whose work is associated with heavy physical and psycho-emotional stress and in the presence of chronic diseases that can affect the condition of the heart.
The “gold standard” of research is 2 main methods: an ECG or ultrasound of the heart is prescribed, the doctor determines what is better and more necessary in each specific case. The choice depends on the age, general condition of the patient, and the purpose of the examination. For preventive examination and initial examination, an ECG is usually used, and echography is indicated for a more in-depth study of identified or existing pathology, if congenital or acquired heart defects are suspected.
For what reasons does the cardiogram worsen?
The main reasons that worsen ECG readings are:
- excessive alcohol consumption, smoking, drug addiction,
- hard physical work before taking data,
- stress,
- blockades of different locations,
- cardiac hypertrophy,
- arrhythmia,
- bradycardia,
- scarring of tissue in the myocardium,
- myocardial infarction,
- inflammation of the membranes, ventricles, atria, etc.
To make a diagnosis, one electrocardiogram is not enough. Cardiologists prescribe diagnostics using echocardiography, Holter monitoring, ultrasound, general blood test, biochemical blood test, and sometimes thyroid hormone testing.
Are there any contraindications to the study?
There are no absolute contraindications to conducting research using these methods. There are limitations when ECG or echocardiography techniques with stress are needed for a functional study, but they are not carried out in severe condition of the patient, when stress is contraindicated.
Also, an obstacle to performing an ECG can be damage to the skin due to injuries or burns, when it is impossible to apply electrodes. However, this is also neglected when the patient’s serious condition requires constant ECG monitoring.
In what cases is an ECG prescribed?
The algorithm for taking an ECG is quite simple. The procedure takes no more than five minutes, the result will be ready immediately. The technique is often used by ambulance or emergency personnel using a portable electrocardiograph. The main advantage of the study is the immediate result.
Indications for ECG:
- hypertension or hypotension;
- suspicion of myocardial infarction;
- angina pectoris;
- heart defect (congenital or acquired);
- cardiac ischemia;
- post-infarction state;
- heart failure;
- pregnancy;
- preparation for surgery.
An ECG is also performed regularly during any heart surgery. The technique may also be prescribed for other diseases, for example, disorders of the endocrine system. There are also certain symptoms that indicate problems in the heart area. This includes fatigue, shortness of breath, and a burning sensation in the stomach.
Features of diagnostics using ECG
The electrocardiogram is the most common method of studying the heart, existing for more than 100 years. It is based on the electrical activity of the heart and the spread of electrical potentials throughout the body. The name of the method literally means recording the electrical activity of the heart.
The diagnostic value of the method lies in the fact that it allows you to record potentials in different parts of the body, and judge the work of the heart by their nature. The areas (leads) to which maximum impulses arrive from certain parts of the heart - the right and left ventricles, and atria - are determined. The electrodes placed on them make it possible to record impulses from different parts of the heart and convert them into a graphic recording or an image on the monitor.
Advantages and disadvantages of ECG
The diagnostic value of the cardiac ECG method is provided by its following capabilities:
- detection of heart rhythm disturbances;
- determination of impulse conduction disturbances (heart block);
- detection of acute pathology in the heart muscle (in case of heart attack, blockage of the pulmonary artery, myocarditis);
- detection of chronic changes in the myocardium (with ischemic disease, chronic pulmonary failure, lack of potassium and calcium, myocardial dystrophy of various etiologies);
- determination of changes in the rhythm and contractility of the heart as a result of treatment, how effective it is.
The disadvantage of an electrocardiographic study is that it provides information only over a short period of time. Cardiac potentials change many times during the day, and their disturbances may not appear constantly, but periodically. Therefore, in modern cardiology, the most reliable method is used - Holter ECG, that is, continuous research and recording throughout the day. At the same time, the patient with the electrodes of the portable device leads his usual lifestyle.
In what cases is electrocardiography prescribed?
An ECG can be prescribed on an emergency or planned basis. Emergency cases include:
- suspicion of myocardial infarction (pain behind the sternum, shortness of breath, severe pain in the abdomen, in the left side of the back, neck, lower jaw, fainting, loss of consciousness);
- feeling of sudden lack of air;
- arrhythmia;
- chest injury;
- a sharp increase or decrease in blood pressure.
The study is routinely carried out before surgery, in pregnant women, in case of obesity, hypertension, rheumatism, diabetes, after a sore throat, other acute infections and poisoning. During routine medical examinations, ECGs are performed on people over 40 years of age and those whose work requires heavy workload (athletes, pilots, drivers, sailors, rescue workers).
Ultrasound of the heart (echocardiography) ecg smad holter
is an ultrasound examination of the heart, which allows you to obtain an image of the heart, its four chambers, valves, all of which can be seen in motion in real time.
The use of a special principle of image analysis - Doppler - allows you to document the movement of blood inside the heart itself and in the vessels.
Thanks to such approaches, cardiac ultrasound allows one to evaluate not only the structure of the heart, but also its functions.
Echocardiography is prescribed for pain in the heart area, for suspected presence of organic changes in the heart, for listening to murmurs, for heart defects, heart failure, hypertension, and cardiac arrhythmias. Ultrasound of the heart and blood vessels is increasingly used for preventive purposes,
since the method allows us to identify the earliest disorders of the heart.
No special preparation is required for this study. You can eat and drink as usual. You can take your usual medications.
When examining the heart, the patient undresses to the waist, the front part of the chest is lubricated with a special gel, the doctor installs an ultrasound sensor in different positions, which allows you to see different parts of the heart and make the necessary measurements.
When examining vessels, the sensor is installed according to their location. The patient experiences virtually no discomfort during ultrasound. The duration of the procedure is within 15 minutes.
Echocardiography allows you to obtain a number of quantitative indicators characterizing the main function of the heart - contractile
. Already in the early stages of a decline in this function, these disorders can be recognized and appropriate treatment carried out.
Repeated studies allow the doctor to evaluate the effectiveness of treatment measures.
Echocardiography makes it possible to accurately recognize diseases of the outer lining of the heart - the pericardium, types of thickening of the pericardial layers, adhesions between them, and the presence of fluid in the pericardial cavity. Heart tumors are clearly identified.
Examination of peripheral vessels reveals mainly a narrowing of their lumen.
Ultrasound of the heart is highly informative (the reliability of the method reaches 90%). Ultrasound of the heart provides very valuable data for assessing its function, due to the fact that it is possible to obtain quantitative expressions of very important indicators and early identify signs of heart failure.
Electrocardiogram - a modern method for diagnosing cardiac activity
An electrocardiogram is the main method for diagnosing the functioning of the heart, providing information about the frequency and regularity of contractions of the heart muscles.
This allows for timely detection of acute or chronic dysfunctions of the myocardium, other pathologies, including a number of non-cardiac diseases (eg.
, thromboembolism of the pulmonary arteries), as well as diagnose metabolic disorders of magnesium and calcium.
An electrocardiogram allows the doctor to analyze the appearance of a curved line, which is a set of points on the electrocardiograph screen that display the dependence of the magnitude of cardiac impulses on time.
These impulses are recorded using electrodes that are attached to the patient’s chest, arms and legs, after which they undergo complex processing on a computer.
The accuracy of the data obtained directly depends on the quality of the equipment used.
We offer a modern electrocardiograph, which makes it possible to quickly and effectively diagnose cardiac activity. The device is capable of synchronously recording 12 generally accepted ECG leads, and the program generates a syndromic conclusion in automatic mode with the possibility of manual correction.
Data via the Internet are sent to the Moscow Regional Research Clinical Institute named after. M.F. Vladimirsky"
Transcript ready in 10 minutes
A holter is attached to the patient, most often on a belt, in a special case and electrodes are applied.
Doctors often use the phrase “hang up the Holter” or “make a Holter”, meaning that the device will be used for 24 hours, on an outpatient basis, in the patient’s usual living conditions - at home, at work, during night sleep. Patients are asked not to wet the device, but otherwise lead their usual lifestyle.
This process of taking readings is called Holter monitoring, named after the American research scientist Norman J. Holter, who first used this technique in 1961.
Why do you need a holter?
It would seem, why do you need a Holter if you can just go to the doctor and take an ECG? Often, people with heart health problems have the following situation: they have complaints, but they arise when it is not possible to immediately see a doctor - in the evening, at night, during some events.
The next day the person goes to the clinic, an ECG is taken, but no abnormalities are found.
Why might this happen? Because a standard electrocardiogram is a record, like a “snapshot,” that records cardiac activity over a short period of time.
A regular ECG records only a few myocardial contractions: from three to twenty, depending on the cardiograph used for this purpose.
Whereas the heart contracts about 100 thousand times per day! Holter records an ECG throughout the day, and not a single heartbeat during this period will go unnoticed by the device, because the electrocardiogram is recorded continuously. Holter makes available for analysis that information about the patient's heart health that cannot be obtained during a short visit to the doctor, and this is the most important diagnostic value of this device.
Then the holter is removed from the patient, and with the help of a special computer program that processes the data obtained, all types of heart rhythm disturbances, painless and painful attacks of myocardial ischemia, etc. are identified and analyzed.
Holter is a device that allows both accurate diagnosis of heart disease and helps to treat cardiovascular diseases - hypertension, atherosclerosis, heart attack, myocarditis - much more effectively.
24-hour monitoring, which Holter proposed, is a procedure that detects almost all possible disorders of cardiac activity that appear during the day, which cannot be done using other methods of cardiac diagnostics currently used. Holter monitoring is a simple and safe procedure.
In order to carry it out, two visits to the doctor will be required. On the first visit, the holter is programmed and installed on the patient; this procedure takes no more than a quarter of an hour. In a day, the holter will need to be removed and its records analyzed. These actions usually take the doctor about half an hour or an hour - in more complex cases.
Modern clinics often offer Holter monitoring at the patient’s home: all necessary visits are made by the doctor himself. This is certainly very convenient, especially if the study is required by an elderly, sedentary person.
How to deceive Holter?
Very often, patients of military age try to deceive the holter by running tirelessly up the stairs and bringing themselves to complete exhaustion, imitating tachycardia. But I hasten to disappoint those who came here in the hope of learning how to deceive Holter - 24-hour blood pressure and ECG monitors are equipped with special sensors that, together with an experienced doctor, always recognize malingerers.
When is a halter needed?
Holter monitoring may be indicated for a patient if:
- there are complaints resulting from heart rhythm disturbances (palpitations, dizziness, loss of consciousness);
- diagnosis of coronary heart disease is required;
- it is necessary to preventively monitor patients with threatening ischemia and arrhythmias;
- it is necessary to evaluate the effectiveness of the treatment;
- white coat hypertension is present;
- arterial hypertension has been detected for the first time, and the heart needs to be examined in order to decide whether to begin drug therapy;
- the fact of chronic constitutional hypotension was revealed;
- Moderate to severe hypertension, resistant to previous treatment, was diagnosed.
In addition, it is advisable to use a Holter if the patient has congenital heart defects, both unoperated and operated, or if he has suffered a myocardial infarction; to evaluate the performance of a pacemaker; in all cases of acute and chronic heart failure. A Holter monitoring procedure would be useful for people who are overweight (obese) or have diseases of the endocrine system.
How to prepare for Holter monitoring?
If the patient is to wear a halter, then during the 24 hours during which the study will be carried out, he must live his normal life - work, rest, meet people, and perform his usual physical activities.
Some doctors, when installing a holter for their patients, ask them to keep an activity diary during the 24-hour examination. This diary should record everything that affects cardiac activity: sleep, medication, movements, etc. This is not always necessary.
Firstly, because constant attention to the process on the part of the patient can affect the reliability of the result (the person will only think about what the Holter shows in the event of one or another action).
And, secondly, a modern holter can have a built-in sensor that records the patient’s physical activity, from which it is possible to determine at what moment the patient was sleeping and at what point, for example, he was running in the park. During the analysis, these points are clarified.
Modern Holter records not only an electrocardiogram, but also performs actigraphy (this is the recording of the patient’s physical activity) and monitors blood pressure.
The software, which is used to analyze the parameters recorded by Holter, allows you to effectively and quickly identify both heart rhythm disturbances and obtain a clear picture of how the autonomic nervous system regulates the functioning of the heart.
During Holter monitoring, no special actions need to be taken. You just need to remember that a holter is a complex, expensive electronic device, and your attitude towards it should be appropriate. This means:
- The halter should not be wet - take a bath, shower, or swim in open water with it;
- Do not expose the holter to low or high temperatures (for example, do not go to the bathhouse on the day of the test);
- The device must be protected from shock and vibration. It is advisable to avoid contact with aggressive household chemicals, especially those containing acids, during Holter monitoring.
In addition, heavy, prolonged physical activity is very undesirable, since, firstly, it can distort the results of the study, and secondly, due to increased sweat, the electrodes may come off.
A patient wearing a halter is advised not to be near transformer booths or powerful power lines. And also come close to working electrical household and medical equipment.
During the examination, it is better to give preference to cotton underwear and avoid wearing clothes made of synthetic and silk fabrics, which can accumulate static electricity.
Holter is a medical device with which 24-hour monitoring of heart activity is carried out - an important and serious study, the relevance of which is undeniable these days.
Features of heart diagnostics using ultrasound
What is ultrasound or cardiac ultrasound and how does it differ from ECG? The differences are fundamental; they lie in the very basis of the method, the technique of its implementation and diagnostic capabilities. Another name for the method is echography, which is its essence. Echo is a reflection of sound, graphy is a recording.
Ultrasound waves are passed through the heart, which are reflected from various structures of the heart, and this is an “echo” - the reflected waves are captured by a sensor and enter a digital analyzer, and are then converted into an image on the screen. The technology is quite accurate, it allows you to study the condition of all elements of the heart - membranes, valves, myocardium, blood vessels, since they reflect ultrasound differently.
In combination with Doppler ultrasound, it is possible to visualize blood flow in the cavities of the heart, large vessels and coronary arteries - a method of color duplex mapping in 3D format.
Advantages and disadvantages of cardiac ultrasound
Cardiac echography is a very informative research method that has the following advantages:
- visualize the shape and size of the heart;
- study the structure of the parts of the heart - membranes, valves, septum, openings, myocardium of the ventricles, atria, incoming and outgoing vessels;
- identify deviations in the structure - scars in the myocardium, degenerative changes, deformation and shortening of the valves, narrowing of the orifices, thickening and adhesions of the cardiac membrane, changes in the amount of fluid in the cavity of the cardiac sac;
- detect blood clots in the cavities of the heart;
- evaluate various parameters of the heartbeat - frequency and strength of contractions, cardiac output and other indicators;
- assess the condition of the coronary vessels, identify sclerotic changes in them;
- identify narrowing, expansion or thinning, aneurysm of the aorta, pulmonary artery.
In addition, the method allows you to examine the heart of a baby and even a fetus in the womb, identify defects, and is absolutely harmless to the body.
The only drawback is the higher cost of the study compared to an ECG.
In what cases is an ultrasound examination of the heart prescribed?
There are certain indications for performing a cardiac ultrasound procedure:
- chest pain, unclear nature, frequent back pain;
- dyspnea;
- attacks of dizziness, fainting;
- pallor and acrocyanosis (blueness of the skin of the nose, ears, hands, feet);
- changes in blood pressure (increase, decrease);
- interruptions in the heart area, arrhythmic pulse;
- murmurs in the heart area, determined by listening;
- systemic diseases - collagenosis (rheumatism, lupus erythematosus, scleroderma);
- delay in the development of the child, the presence of any anomalies;
- condition after heart surgery (bypass surgery, vascular stenting, valve replacement).
Characteristics of echocardiography, indications, limitations
Echocardiography is a study of the heart using ultrasound waves. The technique allows you to measure the size and weight of the heart, determine the size of its chambers (atria and ventricles), look at the condition of the valve systems, identify pathologies of large vessels, heart tumors, and developmental defects. In addition, the study allows you to look at the nature of the hemodynamics of the heart.
| Types of technologies Echo CG | Varieties of holding |
| one-dimensional (flat image) two-dimensional three-dimensional echo CG 4D modeling | transthoracic echo CG transesophageal echo CG stress-echo CG (with load) Echo CG with stress test (administration of Dobutamine or Adenosine, on an exercise bike) intravascular echo CG |
Two-dimensional examination is often carried out with a load (squats, as well as walking on a treadmill). With 3D EchoCG, the doctor can look at the heart in a 3D image and assess the speed of blood flow in the chambers of the heart and large vessels in real time. Arterial and venous blood on the monitor are highlighted in different colors (red, blue). This allows you to evaluate the function of the organ, as well as identify developmental defects and valve pathology. The device detects the backflow of blood (regurgitation) through the shut-off valves when the atria or ventricles contract.
Four-dimensional modeling is carried out after three-dimensional Echo-CG based on the research performed. The doctor analyzes the data obtained, models pathological areas of the heart, and checks the mechanism of operation of the changed element. Such an element could be a valve.
There is no special preparation before performing Echo-CG
Indications for Echo-CG:
- The presence of complaints and clinical manifestations (murmurs, arrhythmias) characterizing heart disease.
- Pathology on the ECG.
- Suspicion of heart defects, tumors, valve damage, aortic aneurysm, heart attack or angina pectoris, as well as other diseases.
- Instability of blood pressure.
- Rheumatic diseases (with suspected rheumatoid heart disease).
- Complicated course of viral and bacterial respiratory infections (Tonsillitis, Influenza).
- The period of gestation.
- Endocrinopathies.
- Varicose veins, increased thrombosis.
Unlike ECG, echocardiography helps to accurately determine organic lesions of the heart. The method allows you to see the area of damage, identify pathological changes in hemodynamics, and accurately determine heart defects, even in utero.
There are almost no restrictions to the research. Transesophageal echo CG is not done for diseases of the esophagus. Intravascular echo CG is not performed in severe condition. Any type of examination is not indicated for chest injuries, severe obesity, or obstructive pulmonary disease.
No specific preparation is required before the test. The patient is placed on a couch during the procedure. The doctor applies a gel for better conductivity of ultrasound rays. The doctor places a sensor on the heart area and begins the study. If an echocardiogram with a load is required, a standard study is performed, after which the patient squats or stands on a treadmill. After the load, the patient is examined again.
What will the results show?
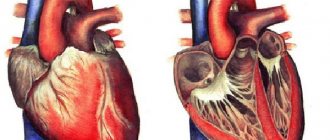
What pathology can be identified during examination - what does an ultrasound of the heart show, and what can an ECG diagnose? Based on the results of electrocardiography, one can judge the work of the heart - its rhythm, the strength of myocardial contractions, and indirectly about the coronary circulation. It is possible to detect heart blockades, extrasystoles, determine their level, identify myocardial hypoxia and disorders of its contractility. Also, the ECG shows specific signs of an acute heart attack and those suffered in the past.
Ultrasound of the heart also determines its functional state, plus deviations from the norm in the structure: various defects, narrowing of the orifices, deformation and insufficiency of the valves, hypertrophy and thinning of the myocardium, the presence of scars, tumors, inflammation, blood clots, atherosclerosis of the coronary vessels, myocardial ischemia, aortic sclerosis , pathology of the pulmonary arteries and veins. In this case, the doctor receives information about the cause of functional disorders.
ECG – electrocardiogram
ECG is an examination method based on the conduction of heart impulses. Previously, 100 years ago, when the Nobel Prize was awarded for the invention of the ECG machine, patients had to immerse their arms and legs in containers of water to record a cardiogram. Currently, science does not stand still and more compact devices have been invented, but the number of wires, electrodes and holders has not decreased.
Taking an ECG
There are only 5 electrodes that are used to record the ECG at rest, but a lead and ground are also present. Each of these elements is important, and the absence of at least one may not only prevent the device from recording a normal cardiogram, but also cause physical harm to the patient.
What will an ECG reveal?
Arrhythmia (a pathology associated with a rhythm disorder, which manifests itself in the form of irregular heartbeats), tachycardia (a disorder associated with an increase in the number of heartbeats), bradycardia (a disorder associated with a decrease in the number of heartbeats), atrial fibrillation, extrasystole (an unusual heartbeat with a long pause after).
Various heart rhythm disturbances
- Disturbances in the trophism of the heart muscle
The phenomenon of insufficient supply of oxygen and nutrients to the muscle, during its increased, intensified or normal work, is called ischemia. Its acute manifestation is myocardial infarction, which in most cases leads to death or serious problems in the future and even disability.
- Impaired conduction of impulses
Disturbances in the conduction of electrical impulses through the conduction system are expressed in blockades, which are clearly visible on the cardiogram. The heart has several nodes that generate an electrical impulse, thanks to which automation occurs (independent contraction). The main one is the atrioventricular one.
A displacement of the axis indicates hypertrophy of some sections and resulting pathologies.
- Thickening of the muscle wall of the components (ventricles or atria)
Hypertrophy of individual components indicates pathologies and problems in the cardiovascular system. Early detection of wall thickening will prevent the development of serious diseases that have not yet manifested themselves clinically.
Increasing the thickness of the heart muscle
Basically, a cardiogram allows you to identify already advanced stages of defects associated with the valve apparatus.
What can't an ECG detect?
- Disturbances in the functioning of the heart that are not currently apparent. For such cases, when failures occur at the time of emotional stress or physical activity, there is Holter or long-term 24-hour monitoring.
- Heart defects, especially the valve apparatus, in the early stages of development.
- Sometimes false positive results are possible and require separate consideration.
ECG is an examination method based on the conduction of heart impulses. Previously, 100 years ago, when the Nobel Prize was awarded for the invention of the ECG machine, patients had to immerse their arms and legs in containers of water to record a cardiogram. Currently, science does not stand still and more compact devices have been invented, but the number of wires, electrodes and holders has not decreased.
Which method should be preferred?
So, what is better - a cardiogram or an ultrasound for various heart diseases? In this regard, you should know that both methods cannot be compared, because they are fundamentally different and complement each other. For example, during a preventive examination, an ECG is sufficient, and if a pathology is detected, then an ultrasound is also prescribed.
In any case, both studies have their own indications, which are determined by a cardiologist or cardiac surgeon. And although the price of the methods differs - for echography it is higher (from 1200 to 3500 rubles), it is still not “exorbitant”, and this study must be completed if necessary. Moreover, it is included in the list of medical services under compulsory medical insurance; if you have a health insurance policy and a referral from a cardiologist, you can receive it for free.
How to improve ECG readings?
Bad heart cardiogram, what to do to improve the result? When a person notices a change in heart rate in everyday life due to stress, then he needs to psychologically prepare for the procedure. Don't worry or be nervous.
Advice! Before the ECG procedure, do not take heart medications so that the result is as reliable and informative as possible.
There are several simple but effective recommendations that can affect the result of the cardiogram:
- If the diagnosis is preventive, then get at least 8 hours of sleep before the ECG.
- Give up morning exercise to keep your heart in a calm state.
- When the procedure is in the morning, it is easy to have breakfast or refuse food. Eat food two hours before the procedure.
- If a person drinks a lot of water, then the day before the cardiogram, reduce the amount of fluid you drink.
- Avoid consuming alcoholic drinks, energy drinks and caffeinated drinks.
- To better attach the electrodes, men with increased chest hair growth can shave the area where the electrodes will be attached.
- To prepare psychologically and be less nervous, it is better to come to the procedure in advance.
These are simple guidelines, but they are important for the correct collection of information.