Myocardial cardiosclerosis is caused by exposure to prolonged hypoxia on the body, which is associated with vascular atherosclerosis and coronary heart disease, as well as exposure to infectious agents and autoimmune processes. In this case, the patient experiences replacement of cardiomyocytes with scar tissue. Cardiac hypertrophy, chest pain, weakness and acute cardiovascular failure develop. Insufficient or untimely treatment can result in death.
A characteristic sign of cardiosclerosis is a weakening of heart sounds and a change in pulse strength.
Reasons for development
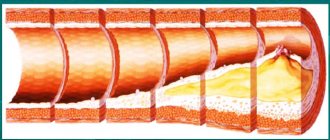
Cardiosclerosis occurs as a result of prolonged hypoxia of myocardial tissue due to blockage of a vessel by an atherosclerotic plaque or thrombus, followed by processes of exudation and proliferation of connective tissues. In this regard, scar tissue or fibrous cords form in place of the cardiomyocytes, which are unable to perform the functions of muscle fibers and contract. As a result of compensatory mechanisms, the heart increases significantly in size, which is associated with hypertrophy of the remaining myocardium, since it bears a significant load. And also these areas of fibrosis provoke the development of arrhythmias, because the conduction of nerve impulses through the heart is disrupted.
An infectious-allergic process and an autoimmune reaction can provoke the replacement of muscle fibers with scars. Myocardial damage is also caused by viruses, bacteria and toxins. The immediate cause of cardiosclerosis is myocardial dystrophy as a result of metabolic disorders or family history.
Stress undoubtedly influences the development of such pathology of the heart muscle in humans.
Myocardial hypoxia due to coronary heart disease and atherosclerosis can be caused by the impact on the human body of factors such as:
- smoking;
- metabolic disease;
- diabetes;
- hypertension;
- hormonal imbalance;
- alcohol consumption;
- obesity;
- inactive lifestyle;
- poor nutrition;
- vitamin deficiency;
- frequent stress.
Cardiosclerosis
Cardiosclerosis is a heart disease in which the formation of connective tissue occurs in its muscle following the partial death of muscle fibers. Cardiosclerosis can be the result of inflammatory, infectious (myocarditis), but more often dystrophic (necrotic) processes. Therefore, there are two forms of cardiosclerosis - myocardial and atherosclerotic.
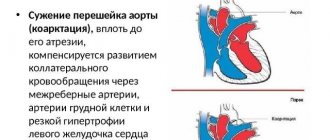
Etiology and pathogenesis Atherosclerotic cardiosclerosis is formed during prolonged myocardial ischemia and as a result of necrosis of the heart muscle. The degree of development of sclerotic changes in the heart muscle depends on the compensatory restructuring of the coronary artery system; in this case, the more poorly developed the collateral network, the more pronounced sclerosis is. Hypoxemia is also important as a factor in the enhanced development of connective tissue in the heart muscle.
Myocardial cardiosclerosis is an outcome of inflammatory, septic, allergic or other nature.
Pathological anatomy Atherosclerotic cardiosclerosis can be limited and diffuse. In the focal form, foci of sclerosis resulting from a heart attack alternate with unchanged areas. With extensive transmural myocardial infarction, a section of the heart muscle wall becomes thinner and is replaced by scar tissue, forming an aneurysm. Diffuse cardiosclerosis is the result of small-focal degenerative-necrobiotic processes in the myocardium due to chronic hypoxia. With myocardial cardiosclerosis, numerous small scars form in the myocardium, which, in the case of rheumatic etiology of cardiosclerosis, are located mainly around the vessels.
Clinical picture of atherosclerosis
Atherosclerotic cardiosclerosis develops in middle and old age, remaining asymptomatic for a long time. Over time, signs of circulatory disorders appear, the contractile function of the myocardium decreases, and disturbances in heart rhythm and conduction occur. Cardiac dullness increases due to cardiac enlargement and myocardial hypertrophy. Heart sounds are muffled, especially the first one. At the apex, a systolic murmur begins to be heard, which is caused by mitral valve insufficiency (relative), as well as a weakening of the tone of the heart muscle.
As the process progresses, signs of heart failure appear - palpitations, shortness of breath, discomfort in the cardiac region with low stress, and sometimes attacks of cardiac asthma; Subsequently, these phenomena also occur at rest. Edema forms, stagnation appears in the small circle, accompanied by an enlargement of the liver and the appearance of ascites. Urine is excreted in very small quantities. Angina attacks are often observed. The electrocardiogram shows a decrease in the S-T interval and a biphasic or negative T wave in a number of leads. Among the rhythm disturbances, extrasystole and often atrial fibrillation are observed, which at first is periodic in nature, and later becomes constant. Atrioventricular block of varying degrees may occur, up to complete block with Morgagni-Edams-Stokes syndrome, intraventricular block of the bundle branches.
Differential diagnosis In patients with myocardial cardiosclerosis, there is a history of rheumatism (often repeated exacerbations), scarlet fever, and diphtheria. With atherosclerotic cardiosclerosis, attacks of angina pectoris and a history of myocardial infarction are observed. The age of patients is older than with myocardial cardiosclerosis. In the presence of atrial fibrillation, mitral heart disease and diffuse toxic goiter should be excluded. The course is often complicated by atrial fibrillation. The presence of presystolic murmur speaks in favor of mitral disease. The characteristic x-ray picture provides significant assistance in the diagnosis of mitral disease.
The prognosis depends on the degree and severity of changes in the heart muscle and coronary arteries.
Prevention and treatment
Prevention is the same as for diseases that cause cardiosclerosis, i.e. for rheumatism, atherosclerosis, etc.
Treatment is aimed at eliminating the causes that caused cardiosclerosis, as well as restoring impaired blood circulation and heart rhythm. It is necessary to combat the progression of cardiosclerosis, and in the case of rheumatic etiology of cardiosclerosis, to prevent repeated outbreaks of rheumatism. In order to productively restore impaired blood circulation, bed rest and a moderate milk-vegetable diet are prescribed, the intake of liquid and table salt is sharply limited. Mandatory consultation with a specialist is required.
The recommended medications are corglycone or strophanthin. It is better not to use Digitalis for angina pectoris and myocardial infarction. To eliminate atrial fibrillation, quinidine, novocainamide, and inderal are used; in some cases, electrical defibrillation is used. For atherosclerotic cardiosclerosis, iodine preparations, aminophylline, and vitamins are prescribed. B, methionine.
Main symptoms
This disease is characterized by the appearance of a cough in a person when he assumes a horizontal position.
Myocardial cardiosclerosis causes the patient to develop the following characteristic clinical signs:
- recurrent acute chest pain;
- feeling of a lump behind the sternum;
- fast fatiguability;
- severe weakness and weakness;
- increased heart rate;
- exercise intolerance;
- impairment of cognitive functions and mental activity;
- ascites;
- accumulation of fluid in the pleural cavity;
- cough that worsens when lying down;
- episodes of loss of consciousness;
- dilation of veins on the surface of the abdominal wall.
Clinical picture
At the initial stages, symptoms directly indicating cardiosclerosis are usually absent, especially when the pathology progresses slowly. Therefore, it is useful for people who are predisposed to cardiac disorders to know about this disease: what signs indicate the presence of this disease, what cardiosclerosis is in general and how to treat it.
Manifestations are often not observed in focal and moderate diffuse forms, but without treatment the symptoms become more noticeable. This or that sign of cardiosclerosis increases gradually as the disease tends to progress.
Shortness of breath and cough
Rapid and heavy breathing indicates the presence of heart failure accompanying cardiosclerosis. The occurrence of the symptom is explained by a violation of the pumping function of the heart, thus the blood is not able to circulate normally, stagnation and impaired gas exchange in the lungs occur. The patient begins to feel rapid fatigue during physical and mental stress.
Since changes in the myocardium are irreversible, shortness of breath worries patients constantly. Initially, it is provoked by heavy loads, and then appears even during rest.
Loss of myocardial strength causes shortness of breath.
Cough is the result of fluid overflowing the walls of the bronchi and irritation of the cough receptors. Usually not accompanied by sputum production.
Rhythm disturbances and increased heartbeat
If necrosis affects the conductive impulses of the fiber, arrhythmia occurs, which impairs blood circulation and increases the risk of thrombosis.
The development of cardiosclerosis may be accompanied by:
- tachycardia;
- bradycardia;
- extrasystole.
Attacks of increased heart rate negatively affect the functioning of the heart, causing oxygen deficiency and contributing to the wear and tear of the heart muscle. Tachycardia can cause loss of consciousness.
Edema and dizziness
Swelling in the area of the feet and ankles is not immediately observed and indicates stagnation of blood in the systemic circulation. The formation of swelling is typical in places where there is low pressure and slow blood flow.
Read also: Cardiosclerosis of the interventricular septum
If you feel dizzy, it means there is acute oxygen starvation of the brain. It is caused by severe arrhythmia or a sharp decrease in blood pressure. Occasional fainting may occur due to dizziness. This is a kind of protective reaction that allows the heart to function normally with the available amount of oxygen.
Why is it dangerous?
Myocardial cardiosclerosis with disturbances in the rhythm of the heart can provoke the development of the following complications in the patient:
A severe complication of this pathology is the development of a vascular aneurysm.
- aneurysm;
- rupture of the heart muscle and internal bleeding;
- atrial fibrillation;
- cardiovascular failure;
- fibrillation;
- death.
Necessary diagnostics
It is quite difficult to detect the beginning replacement of cardiomyocytes with fibrous tissue, especially since patients often do not seek help in the early stages of the disease. There is a greater chance of detecting pathology after myocarditis or a heart attack, since the death of heart muscle cells is quite expected.
The list of diagnostic measures is presented:
- Examination of the patient. The cardiologist or therapist resorts to questioning the patient, visual examination, palpation of the chest, percussion and auscultation.
- Echocardiography (ultrasound of the heart). The goal of the painless and non-invasive technique is to determine how well the organ copes with its functions and what condition the myocardium is in.
- Electrocardiography. Helps evaluate the bioelectrical activity of the heart. The method is used not only to make a diagnosis, but also during treatment, which allows the treatment regimen to be adjusted as necessary.
- X-ray. Such a study, due to its ineffectiveness, is considered unnecessary. However, sometimes it can be used to make a preliminary diagnosis. If the pathology is in advanced stages, the image will show an enlarged organ. In some cases, x-rays reveal the presence of aneurysms.
- CT and MRI. These methods are highly informative and can detect foci of necrosis.
- Scintigraphy. Involves the introduction of radioactive isotopes into the bloodstream in order to detect unwanted changes in the myocardium. If cells are damaged, isotopes accumulate in them in small quantities. When a person is healthy, the substances are distributed evenly throughout the muscle.
In addition to the listed methods, morphometric ones are used. In particular, to confirm cardiosclerosis, a myocardial biopsy is performed followed by microscopic examination.
Blood and urine tests are also required to determine the root cause of the disease. In addition, laboratory tests make it possible to monitor the effectiveness of treatment.
Features of treatment
Therapy for myocardial cardiosclerosis should be comprehensive and include the use of drugs that eliminate the immediate cause of the disease. For this, statins and liberin are used, which normalize cholesterol levels in the blood and reduce the amount of LDL. In addition, it is important to cure chronic infectious pathologies that cause severe allergization of the body and lead to myocardial damage. Antihistamines and antiallergic drugs are indicated. For high blood pressure, it is recommended to take ACE inhibitors and beta blockers. It is also important to use angioprotectors that improve the condition of the vascular wall. Nitroglycerin and cardiac glycosides will be useful, as they dilate blood vessels and reduce the load on the heart.
Fibrinous pericarditis (dry): description, symptoms and treatment, macroscopic specimen and microscopic specimen
Pericarditis is a large group of inflammatory diseases of the pericardium of primary and secondary origin.
Among all types of pericarditis, the dry form is the most common. The uniqueness of the clinical manifestations makes it possible to suspect inflammation of the pericardial sac in time and seek medical help.
The article discusses the causes, signs and distinctive features of dry pericarditis, as well as methods of diagnosis and treatment.
Dry pericarditis - what is it?
Fibrinous pericarditis (ICD-10 code: I30) is an inflammatory disease of the outer and inner layers of the heart sac, accompanied by the deposition of the inflammatory protein fibrin between them.
The incidence is 0.1% of all cardiac pathologies.
Has the following characteristics:
- Local swelling;
- Local increase in temperature and dilation of blood vessels;
- Pain syndrome;
- Dysfunction of the cardiac membrane.
Fibrinous inflammation may be an early stage of other types of pericarditis. In response to the action of the etiological factor, a specific protein, fibrin, falls out on the pericardial layers. Fibrin deposits are white sticky thread-like masses. Their massive deposits lead to adhesion and destruction of the cardiac membrane.
Causes and mechanism of development
Dry pericarditis can be primary or secondary. Primary develops without a previous disease, secondary - after it. Among the main etiological factors are:
- Microbial agents;
- Hypothermia;
- Systemic autoimmune diseases;
- Metabolic pathology.
The most common causes of dry pericarditis are viral infections of the respiratory tract and intestines, pneumonia, and influenza.
At the first stage, blood cells are attracted to the site of inflammation. Edema, local fever, and infiltration of platelets and leukocytes develop. During the second stage, the level of fibrinogen, the precursor protein of fibrin, increases in the blood. In the third stage, the accumulation of fibrin leads to the adhesion of the pericardial layers to each other.
Symptoms and signs by stage
Along the way, three forms of the disease are distinguished:
- Acute (up to 2 weeks);
- Subacute (2 weeks – 6 months);
- Chronic (more than 6 months).
Acute dry pericarditis is characterized by vivid symptoms and severe pain . The pain develops gradually, over the course of a day, and is stabbing, cutting or squeezing in nature. There is an increase in pain when bending the body, coughing, eating and at the height of inspiration. Pain syndrome is accompanied by:
- Fever;
- Muscle weakness;
- Drowsiness;
- Redness of the skin of the face and chest.
The patient notes a feeling of uneven, loud heartbeat, interruptions in heart function. Characterized by self-limitation in food and physical activity, shortness of breath. The disease is accompanied by insomnia due to deterioration in the lying position.
The subacute form is transitional between acute and chronic and does not always develop . It is most typical for elderly patients with late or irrational treatment. A distinctive characteristic of this form is the reduction of pain and normalization of body temperature. Patients complain of palpitations, shortness of breath, and dizziness.
The chronic form is characterized by a successive change of remission and exacerbation . During the period of exacerbation, the clinical picture corresponds to the symptoms of acute fibrinous pericarditis; during remission, patients feel satisfactory. Exacerbations occur during the cold season or after the action of a provoking factor (infection). Fever rarely develops.
What happens to the cardiovascular system?
With a small lesion, fibrin resorption occurs quickly. In view of this, cardiac damage is minimal in the form of tachycardia and a decrease in stroke force. With massive protein deposits, an irreversible adhesive process develops.
Organic changes in the pericardium complicate ventricular contractions and lead to the development of extrasystoles, arrhythmias and blockades. Cardiac tamponade does not develop.
Establishing diagnosis
Diagnostic triad of fibrous pericarditis:
- ECG changes;
- Pain in the precordial region;
- Pericardial murmur.
The diagnostic algorithm includes examination, objective examination, laboratory and instrumental methods.
- Inspection. The forced position of the patient with a forward bend is revealed.
- Palpation. Local pain and swelling behind the sternum and to the left of it are determined. No displacement of the apical impulse is observed.
- Percussion. If dry pericarditis turns into exudative, a shift in the boundaries of relative cardiac dullness of the heart to the left, right and down is noted. In other cases, the boundaries are not changed.
- Auscultation. With dry pericarditis, a continuous pericardial murmur is detected by auscultation, which does not disappear after coughing and is not carried to the vessels of the neck. The noise intensifies when the stethoscope is pressed against the skin and is squeaky or “crunchy” in nature.
- Laboratory data. An increase in ESR, CRP and fibrinogen levels in the blood serum is detected. Viral etiology is characterized by an increase in lymphocytes of more than 40%. PCR is performed to determine virus antigens.
- ECG. Changes in dry pericarditis are more striking and specific than in exudative pericarditis. The following signs are revealed: Decrease in the ST segment by 5-10 mm below the isoline;
- The amplitude of the T wave is twice normal;
- In lead aVL the PR interval is shortened;
- The length of the ST segment exceeds the length of the T wave by 25% or more.
Differential diagnosis
Dry pericarditis is differentiated from:
- Exudative (by increasing the cardiac boundaries);
- Pneumonia (fluid level on x-ray, cough with purulent sputum);
- Myocardial infarction (a Q wave appears on the ECG, the pain is not relieved by analgesics);
- Tumors and injuries of the chest (detected using x-rays).
Symptoms of dry pericarditis allow one to suspect a number of diseases of other organs and systems:
- To exclude tuberculosis, a Mantoux test is performed;
- To exclude uremia, the level of creatinine and uric acid in the blood is determined;
- Autoimmune diseases are identified by the presence of rheumatoid factor, LE cells, ASL-O, and autoantibodies in the serum;
- To exclude thyroid diseases, T3 and T4 levels are examined.
All patients are tested for HIV infection and syphilis.
Pathanatomy: description of macroscopic and microscopic specimens
Fibrin accumulations are deposited between the epicardium and the inner layer of the pericardium, which form thread-like deposits. When the leaves come apart, the pathological areas are easily wounded and have a striped appearance. In this regard, the macropreparation is called “hairy heart”.
The pericardial cells are stretched and partially destroyed. Between them, accumulations of fibrin and cells are found - neutrophils, lymphocytes, platelets and fibroblasts. This phenomenon is called “cellular lymphocytic infiltration” and is characteristic of the acute stage of inflammation. In the chronic stage, connective tissue fibers, calcium deposits, and microthrombosis are found in the microslide.
Possible complications and consequences
Outcomes of dry pericarditis without therapy:
Adverse effects after therapy are extremely rare. In cases where treatment was started at the wrong time, accidental injury to the heart is possible when trying to remove adhesions surgically.
Fibrinous pericarditis in children
Occupies 5% of all pediatric cardiac pathology. In 60% of cases, the disease has a viral etiology and develops in the cold season. Children experience long-term general symptoms (fever, intoxication), as well as dyspepsia (vomiting, diarrhea). In some cases, this lengthens the duration of therapy, but the prognosis remains relatively favorable. Mortality rate is less than 0.1%.
Find out in more detail about pericarditis in childhood from a separate material.
Treatment tactics are the same as for adults. Doses of drugs are calculated based on the age and weight of the child. For young children, it is preferable to use drugs in the form of suppositories.
Choice of treatment tactics
The goal of therapy is to reduce pain and eliminate the causative factor. Indication for treatment is diagnosis of “Dry pericarditis”.
Indications for hospitalization:
- Pregnancy;
- Childhood;
- Fever;
- Severe pain syndrome;
- Persistent tachycardia;
- Rhythm disturbances.
The following groups of drugs are used in therapy:
- Anti-inflammatory drugs (NSAIDs) - diclofenac, ibuprofen, aspirin, ketorol, indomethacin. If they are ineffective, they are replaced with colchicine or used in combination with NSAIDs;
- If colchicine is ineffective, hormones (prednisolone) are added to therapy;
- Auxiliary agents – interferon, cycloferon, anaferon, viferon.
Invasive treatment is rarely performed. The indication for this is long-term resorption of fibrin deposits. To remove them, a puncture of the pericardium is performed, during which its cavity is cleared of fibrin and washed with antiseptic solutions.
Treatment table No. 10 is assigned. The diet is aimed at reducing the consumption of salt and animal fats, as well as replenishing protein deficiency. The daily calorie content of food is 2500 kcal.
Bed rest. Children and pregnant women are treated in a hospital until complete recovery. The remaining patients, with clinical improvement, switch to outpatient treatment.
Lifestyle does not change after suffering from the disease. Working capacity is rarely reduced, only in the case of secondary complications.
Clinical guidelines
If you have characteristic symptoms, you should not resort to self-medication. It is necessary to seek help as early as possible and conduct a comprehensive examination. In the treatment of dry pericarditis, the following rules should be followed:
- The drugs of choice are NSAIDs and antivirals;
- Antibiotics are prescribed only when effusion occurs;
- The patient is provided with physical and emotional peace;
- Until the patient's condition improves, he remains on bed rest.
The ESC clinical guidelines for the diagnosis and management of patients with pericardial disease, approved in 2020, provide clear answers on how to treat pericarditis. It can be downloaded here.
Prevention measures
Timely abandonment of bad habits will protect a person from this disease.
Myocardial cardiosclerosis can be prevented by leading a healthy lifestyle, avoiding stress and getting rid of bad habits. A balanced diet is also recommended, so fatty, fried and spicy foods should be excluded from the diet. Preference should be given to steamed food, vegetables and fruits. Adequate sleep and sufficient rest are important.
Cardiosclerosis of the myocardium occurs more often in men, and both young and elderly people can get sick.
Prevention and nutritional advice
Compliance with preventive measures plays a huge role in the treatment process. In other words, the use of medications will be ineffective if you do not reconsider your lifestyle.
Read also: Diagnosis of atherosclerotic cardiosclerosis
You can speed up recovery and maintain normal heart function by:
- Quitting smoking and alcoholic beverages.
- Moderate physical activity.
- Regular examinations by a cardiologist, regardless of how you feel.
- Maintaining inner peace.
Infections and other pathologies that can cause necrosis of cardiomyocytes should be treated promptly.
A separate topic is a nutritious diet for cardiosclerosis. First of all, the ban is imposed on foods that increase cholesterol. It is also necessary to reduce salt and fluid intake. This will reduce the volume of circulating blood, which will relieve excessive stress on the heart.
Patients with cardiosclerosis should eat within the framework of dietary table No. 10.
The menu should not include:
- smoked meats;
- pickles;
- animal fats;
- coffee, strong tea;
- chocolate.
Doctors advise eating cereals, boiled lean meats, fruits and vegetables. It is worth leaning on foods containing large amounts of potassium (dried fruits, raisins, bananas).
Diet correction is possible if you are overweight or excessively exhausted. The issue of diet should be discussed with your doctor.
Cardiosclerosis usually develops as a complication of cardiac pathologies or other disorders that negatively affect the functioning of an important organ. Myocardial cells affected by necrosis cannot be restored, but the process can be prevented or slowed down. The main thing is not to ignore the first manifestations and refrain from self-medication.