The main cause of such a dangerous disease as atherosclerosis of the heart is damage to the veins and arteries leading to the heart by cholesterol. This pathology is characterized by the complexity of therapy and serious danger in the absence of treatment or non-compliance with the rules of a healthy lifestyle.
The main difficulty of therapy is based on the fact that in order to successfully eliminate it, the disease must be diagnosed as early as possible, and at the initial stage the pathology manifests itself insignificantly. Only with timely treatment can harmful vascular changes be prevented and eliminated and the likelihood of life-threatening complications can be significantly reduced.
The mechanism of development of atherosclerotic plaque in the heart vessels
Atherosclerosis of the heart vessels (symptoms and treatment are interrelated) is a disease that has stages of development.
Stages of development of atherosclerosis of heart vessels
There are the following phases of pathology:
- First . Additional name: initial stage. The speed of blood flow gradually decreases, and small cracks form on the walls of blood vessels. Next, microcracks grow and their size increases. That is, more noticeable and clinically significant defects are formed. Lipid deposits penetrate into the vessels, and fatty spots gradually form.
- Second . Another name is liposclerosis. In the lesion, the infiltration (penetration) of fat cells accumulates and increases. But atherosclerotic plaque is unstable. That is, it can come off, so this stage is characterized by an increased risk of blood clots.
- Third . Another name is atherocalcinosis. The plaques thicken, calcium salts join the growth, and a fibrous layer forms on top. The lumen of the vessels decreases, and the thrombus grows and deforms the artery. At this stage, there is a high probability of occlusion - this is the blocking of the lumen of the vessel by elements of a ruptured plaque, followed by necrosis (death).
Causes, risk factors
Atherosclerosis of the heart vessels can appear for various reasons.
The most common of them:
- infectious lesions - penetration of viruses and bacteria into the body;
- autoimmune pathologies – multiple sclerosis, diabetes mellitus and others;
- congenital defects in the walls of blood vessels;
- chronic pathologies of the heart and blood vessels;
- arterial hypertension - a persistent increase in pressure (more than 140/90 mm Hg).
In addition, the reasons contributing to atherosclerosis of heart vessels include an imbalance of lipoproteins and the accumulation of varieties having low density (LDL), very low density (VLDL), intermediate density (IDL) in the walls of blood vessels.
General classification:
- high-density lipoproteins (HDL) - the smallest particles, contain phospholipids that prevent cholesterol from leaving the bloodstream;
- intermediate density lipoproteins (IDL) - they have a short lifespan in the blood, because normally they should be quickly absorbed by the liver and converted into LDL, but with impaired lipid metabolism, the accumulation of IDL is possible;
- low-density lipoproteins (LDL) – contain a lot of cholesterol and proteins (up to 30%), less triglycerides (up to 10%), transport cholesterol throughout the body;
- very low density lipoproteins (VLDL) are the largest particles, contain a large amount of triglycerides (up to 70%), 10% cholesterol and proteins, VLDL transport triglycerides from the liver to adipose tissue;
- chylomicrons (CM) - deliver fats (from food) to the liver for further breakdown of triglycerides.
LDL, VLDL, LPPP are atherogenic lipoproteins. If the blood contains a large amount of these fractions, cholesterol plaques form, atherosclerosis and other concomitant heart diseases develop.
Cholesterol is divided into the following types:
- good – contains HDL;
- bad – contains LDL, VLDL, LPPP.
The name cholesterol did not appear by chance.
Associated with the following conclusions:
- if the content of LDL, VLDL, or LPPP is increased in the blood, then this negatively affects the cardiovascular system;
- good cholesterol removes bad cholesterol from plaques and transports it to the liver for further breakdown and removal from the body.
In addition to the reasons that can affect atherosclerosis of the heart vessels, there are factors that increase the likelihood of the disease occurring.
Items:
- passive lifestyle;
- excess body weight;
- bad habits – smoking, drinking alcoholic beverages and drugs;
- frequent stress;
- taking medications from the contraceptive group (Klaira, Jess, Yarina);
- taking medications that can increase the level of bad cholesterol - for example, anabolic steroids can increase LDL by 20% and reduce HDL by 20 - 70%;
- increased blood clotting and high probability of thrombosis;
- chronic lack of sleep and lack of rest;
- hormonal imbalances - for example, menopause, pregnancy;
- age category – the likelihood of atherosclerosis increases with age;
- unhealthy diet – predominance of fatty foods;
- gender – men have a greater risk of developing cardiovascular diseases than women;
- living in places with unfavorable ecology.
Clinical picture of the disease
In the early stages, atherosclerosis of the coronary arteries of the heart occurs in a latent form. Typically, the first signs of the disease are observed by middle-aged people.
Therefore, doctors recommend annual examinations for all people who have crossed the 35-year mark. However, smoking, hypertension, and hypercholesterolemia can lead to earlier development of symptoms of coronary artery atherosclerosis.
The first signs of the disease include the following symptoms:
- Pain in the chest area, radiating to the back or left shoulder;
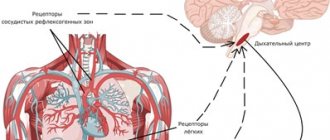
- The appearance of shortness of breath at the onset of pain. Sometimes patients are unable to remain in a horizontal position due to breathing problems;
- Dizziness;
- Nausea and vomiting.
The listed symptoms of atherosclerosis of the coronary arteries are not specific, so they are often confused with other pathologies of the cardiovascular system. This significantly complicates the diagnosis and treatment of the disease.
With further progression, atherosclerosis of the coronary vessels causes the following symptoms:
- Angina pectoris. The condition is characterized by rare pain in the chest, which develops after intense physical exertion or emotional stress;
- Cardiosclerosis. Acute myocardial ischemia leads to the formation of areas of fibrosis throughout the heart muscle. The condition causes disruption of the contractile function of the heart;
- Arrhythmia. The pathology develops as a result of myocardial damage, impaired conduction of impulses;
- Heart attack. If a cholesterol plaque ruptures, a blood clot forms on its surface. This clot interferes with normal blood flow and provokes the development of cardiomyocyte necrosis. Typically, heart attacks develop between 4 and 10 a.m., when adrenaline levels rise in the bloodstream. About 50% note the appearance of warning symptoms before an attack.
Signs of atherosclerosis of the heart
Atherosclerosis of the heart vessels (symptoms and treatment are interrelated factors) is a pathology that has certain signs. At the initial stage of the disease, they may not appear or be present to a small extent.
Symptoms of atherosclerosis of the heart vessels:
- pain in the sternum;
- frequent headache;
- dizziness;
- shortness of breath, which worsens during activity (walking, climbing stairs), then manifests itself at rest;
- rapid fatigue with minimal load;
- reduced performance;
- malaise;
- memory impairment;
- numbness of the legs;
- swelling of the lower extremities;
- pain in the back and limbs;
- impaired speech;
- frequent fainting;
- weight loss;
- nausea and difficulty swallowing food;
- pale skin;
- impaired coordination of movements;
- dry skin;
- pain in the jaw on the right side (rare).
With atherosclerosis of the heart vessels, complete blockage of the artery is possible, which leads to myocardial infarction. Symptoms of the condition are severe and prolonged pain in the middle of the chest, shortness of breath and increased sweating. A heart attack requires immediate medical attention.
Sudden death from atherosclerosis
Atherosclerosis is one of the most common human diseases, which is based on lipid infiltration of arterial walls with the subsequent reactive development of connective tissue thickenings in these places - plaques, which leads to thickening of the walls and narrowing of the lumen of the arteries.
The etiology and pathogenesis of atherosclerosis have not been fully elucidated. Currently, there are a large number of so-called “risk factors” that determine the rate of development of atherosclerosis, among which the most important are hypercholesterolemia, arterial hypertension, prolonged psycho-emotional overload, sedentary lifestyle, excess and poor nutrition, and family history. In addition, there are several dozen more factors that contribute to the occurrence and enhance the development of atherosclerosis. Epidemiological studies conducted in recent years have shown that the incidence of atherosclerosis in many countries of the world is growing, that atherosclerosis has become “younger”. Nowadays, myocardial infarction - the most dangerous complication of atherosclerosis - is not uncommon at the age of 20-30 years, and at the age of 40-50 it has become a common occurrence. It is believed that the reason for this is accelerated urbanization and the ever-increasing intensity of life, i.e. atherosclerosis is a disease of modern civilization.
The most dangerous, from the point of view of sudden death, is atherosclerosis with predominant damage to the coronary arteries of the heart. In this case, atherosclerotic plaques are most often detected in the area of the mouths of the coronary arteries and in places where large branches depart from the main trunks. The favorite localization of single plaques is the upper third of the anterior descending branch of the left coronary artery.
There are three stages of this disease : ischemic, which is characterized by attacks of angina pectoris; thromonecrotic, with its most severe and dangerous complication - myocardial infarction, and fibrous, which is usually referred to as atherosclerotic cardiosclerosis.
Sudden death can occur in any of these three stages of the disease. It is important to note that in most cases, by the time of autopsy, the expert does not have any information about the clinical course of the disease, or this information is scanty, fragmentary, and insufficient. Often, a subsequent survey of the relatives of the deceased also does not provide any data - the deceased did not complain of pain in the heart area, he worked until the last day or hour. The fact that death often occurs in a normal work environment, as well as on the street, in transport, etc., suggests that even shortly before death, those who suddenly died felt practically healthy. This gives reason to believe that among those who died suddenly, many suffered from a painless form of atherosclerosis of the coronary arteries of the heart.
When, during an autopsy, an expert discovers severe stenosing coronary sclerosis, he can easily establish the cause of sudden death and can explain its genesis, which in such cases is associated with an acute violation of the coronary circulation. However, the experience of expert work shows that not in all cases there is a correspondence between the severity of the morphological picture of atherosclerosis and the onset of sudden death. Thus, many people with severe lesions (stenotic atherosclerosis with thrombosis and extensive scars in the myocardium) live to a very old age and die from other diseases or violent death (for example, from a transport injury). At the same time, relatively young people sometimes die suddenly, and at autopsy only initial signs of atherosclerosis of the coronary arteries of the heart can be detected in the form of single plaques. In such cases, the genesis of death can be explained by spasm of the coronary arteries affected by the sclerotic process.
A short-term spasm gives the clinical picture of angina pectoris; prolonged spasm can lead to myocardial infarction or rapid death if the ensuing coronary circulatory disorder cannot be compensated for by the active involvement of anastomoses and collaterals. Namely, at a young age, with relatively mild atherosclerotic lesions and a short duration of coronary artery disease, collateral circulation is insufficient and cannot compensate for the acute disorder of coronary circulation.
The severity of morphological changes in acute coronary insufficiency depends not only on the presence of coronary sclerosis, but also on the speed of dying. With very rapid death, visible foci of necrosis do not have time to form in the myocardium, and only signs of focal circulatory disorder are revealed. Studies in recent years (especially A.V. Smolyannikov et al., A.V. Kapustina et al., etc.) have shown that in cases of death from acute coronary insufficiency, characteristic microscopic changes can often be identified: foci of acute plasmatic impregnation of the intima of the coronary arteries , especially above the plaques, small hemorrhages into the plaques, and on their surface there are fresh parietal thrombi. In the myocardium, against the background of a sharp congestion of the capillaries, perivascular hemorrhages, stromal edema, fragmentation and focal necrosis of muscle fibers are often detected.
If ischemia of the heart muscle lasted more than 3-4 hours, then at autopsy one can detect signs of myocardial infarction. The most common cause of heart attack is stenosing coronary sclerosis with thrombosis of the coronary arteries. Therefore, at autopsy it is necessary to look for blood clots in the coronary arteries.
Macroscopically, a necrotic focus in the heart muscle is clearly visible if at least a day has passed from the moment of disruption of coronary circulation to death. In this case, the area of necrosis appears as a dirty-gray or yellowish-gray area, sometimes sinking, often with bizarre dark red borders (hemorrhage area). Microscopic examination during this period reveals necrosis of muscle fibers and myocardial stroma, as well as a demarcation shaft consisting mainly of leukocytes. Subsequently, the necrotic muscle fibers are resorbed and replaced by granulation tissue, which turns into a dense scar. This entire organizing process lasts from 4 to 8 weeks.
Infarctions are usually localized in the anterior (50-60%), posterior (30-40%) walls of the left ventricle near the apex of the heart and in the interventricular septum (10-12%). With necrosis of the entire thickness of the myocardium (total infarction), cardiac rupture may occur, followed by pericardial tamponade and rapid death.
At autopsy in such cases, a sharply stretched pericardium is revealed, which contains liquid blood and a large blood clot. Upon removal of this bundle, a cardiac rupture becomes visible, which is most often localized in the area of myomalacia of the cardiac muscle, but can also occur at the border of the infarcted and healthy area,
At the end of the 50s, a new nosological form appeared in the practice of clinicians - ischemic or coronary heart disease, which was included in the International Classification of Diseases, Eighth Revision, 1965. This classification was put into effect in our country on January 1, 1970, and from that time on, the diagnosis of “coronary heart disease” became widely accepted in medical practice.
According to the WHO expert group, coronary heart disease (CHD) is an acute or chronic dysfunction that occurs due to a relative or absolute decrease in the supply of arterial blood to the myocardium.
Such dysfunction, according to experts, is most often, although not always, associated with a pathological process in the coronary artery system.
In accordance with this definition, IHD should be considered, first of all, a clinical concept and, secondly, a collective concept, since the cause of myocardial ischemia can be a wide variety of pathological processes: atherosclerotic, microcirculatory, toxic, infectious-allergic, etc. However, the experience of dissection and Expert work indicates that in the vast majority of cases (up to 97-98%), the morphological basis of IHD is atherosclerosis of the coronary arteries of varying degrees of severity.
It would seem that in such cases the expert does not need to begin the forensic diagnosis with the defining concept of “coronary heart disease.” But due to the fact that this diagnosis has widely entered into clinical practice, there is often a need to compare clinical and forensic diagnoses, as well as to unify statistical data, forensic doctors, in appropriate cases, should use the currently generally accepted the wording is “coronary heart disease.”
Presidium of the All-Union Cardiological Society in 1973-1974. held a special meeting to develop recommendations for formulating a diagnosis in cases of coronary artery disease. The meeting considered it advisable to immediately after the general formulation “coronary heart disease” to diagnose in order of priority one of the three main forms of the disease: acute myocardial infarction, acute coronary insufficiency, or angina pectoris, cardiosclerosis. And only after them, the diagnosis should reflect the morphological manifestations of coronary artery disease (atherosclerosis of the coronary arteries, their thrombosis, cardiac aneurysm, cardiac rupture, etc.). Example. Coronary heart disease: acute infarction of the posterior wall of the left ventricle, severe atherosclerosis of the coronary arteries of the heart, thrombosis of the circumflex branch of the left coronary artery.
This construction of the diagnosis does not meet the requirements of the etiopathogenetic principle applied in all other cases, and is an exception to the rules for formulating a medical diagnosis.
Other localizations of atherosclerosis are less likely to cause sudden death. With atherosclerosis of the cerebral arteries, complicated by thrombosis, a focus of ischemic softening of the brain matter or cerebral hemorrhage may develop. Typically, such hemorrhage is a complication of hypertension.
Modern diagnostic methods
If you suspect atherosclerosis of the heart vessels, you should visit a doctor. The disease is within the competence of the cardiologist. If it is impossible to visit this doctor, you can contact a therapist.
Before prescribing a diagnosis, the specialist carries out the following actions:
- survey - the doctor asks various questions that relate to symptoms and concomitant diseases;
- measuring human health indicators (blood pressure, body temperature, pulse);
- examination – a specialist examines the skin and mucous membranes.
Next, an examination is prescribed that allows you to determine atherosclerosis.
Diagnostic methods are listed in the table:
| Name | Description |
| General blood analysis | Using the study, you can determine the value of various indicators (hemoglobin, red blood cells, etc.). For analysis, blood is taken from a vein or finger. The first method is most often used, since the result will be more accurate. |
| General urine analysis | The study allows us to identify abnormalities in the functioning of the cardiovascular, genitourinary and endocrine systems. The result sheet contains the following information:
|
| Determination of glucose | The indicator can be determined in blood or urine. Diabetes mellitus is detected using the analysis. |
| Lipid profile | Screening includes determination of HDL and LDL, total cholesterol. They also include triglycerides (TG). If the profile is extended, then the analysis additionally includes VLDL and apolipoprotein. Based on the results, the risk of atherosclerosis is identified. |
| Angiography | The examination involves studying the blood vessels of any area (heart, head, etc.). Angiography is the use of X-ray radiation. The procedure allows you to determine:
Carrying out the examination:
The procedure makes it possible to determine the prevalence and degree of development of atherosclerosis and other diseases of the cardiovascular system (heart attack, coronary disease). |
| Electrocardiogram (ECG) | Another name is electrocardiography. The procedure involves determining the electrical activity of the heart. Electrodes are used to record biological potentials. The result is displayed in the form of a graph on the device monitor or printed on paper. Using an ECG it is possible to determine:
There are different types of ECG. Namely:
|
| Ultrasound examination (ultrasound) of the heart | Among the types of ultrasound, echocardiography (EchoCG) is used. The procedure allows you to study the structure and functionality of the heart, as well as blood vessels. Among all echocardiography methods, Doppler echocardiography is most often used. During the procedure, it is possible to identify impaired blood flow in the heart and blood vessels. The stages of echocardiography do not differ from conventional ultrasound. If necessary, a contrast agent may be injected before the procedure to improve visualization. Scheme of echocardiography:
|
| Plethysmography | An examination that allows you to record changes in the volume of a separate organ or part of the body. Most often, the procedure is used to determine the tone of small vessels and blood flow in them. The study is used for constant narrowing of blood vessels in different parts of the body. |
| Sphygmography | A procedure that involves measuring arterial pulse and other indicators of the cardiovascular system. A sphygmograph is a device that performs monitoring. As a result of the procedure, a sphygmogram is obtained (a curved line with parts, each of them is responsible for different pressures inside the vessels). Using this examination, it is possible to assess the condition of the blood vessels. The procedure takes 10–15 minutes. A sensor is installed on the skin, which reads all the information and transmits the data to a recording device. |
| Magnetic resonance imaging (MRI) of the heart and blood vessels | The method involves exposure to electromagnetic radiation. Using the procedure, it is possible to identify the following diseases:
Additionally, MRI is performed to evaluate the effectiveness of the operation. For example, with bypass surgery. To improve visualization, a contrast agent may be injected into the person's body before an MRI. The procedure depends on the type of device:
The results of the procedure produce three-dimensional images. MRI takes 40–60 minutes. |
Before conducting a diagnosis, the doctor must tell you about the preparation measures for each study. The cost of the examination may vary. It all depends on the list of procedures, city, organization. Therefore, it is better to find out the price in a specific clinic.
You can get diagnosed for free. To do this, you need to go to a clinic with a compulsory health insurance policy (CHI).
Atherosclerosis of the heart vessels (symptoms include pain in the sternum) is a disease that requires referral to additional specialists.
Before prescribing treatment, a cardiologist or internist may refer the patient for consultation with other doctors.
Most often, it is additionally recommended to contact the following specialists:
- nutritionist – creates a nutrition plan;
- endocrinologist – identifies and treats metabolic disorders (diabetes mellitus and others);
- narcologist – treats drug, alcohol and tobacco addiction;
- psychologist – helps a person normalize emotions;
- hematologist – identifies and treats blood diseases;
- surgeon - performs surgery.
Symptoms and diagnosis
The disease of cardiosclerosis can occur without pronounced symptoms, especially in cases of slow development of the disease.
With a moderate degree of growth of connective tissue, there is no loss of elasticity of the heart muscle, weakening of the force of its contractions, or significant damage to function.
Cardiosclerosis, which is a consequence of a heart attack, may not have pronounced manifestations, especially in cases where there is a superficial location of connective tissue scars and the extent of such areas is small.
Malfunctions of the heart in such situations depend rather on the diseases that resulted in the development of cardiosclerosis.
Characteristic symptoms of cardiosclerosis are:
- Shortness of breath, which increases with the progress of the disease; may occur during physical activity, in a lying position, in stressful situations, and then at rest
- Cough, especially at night
- Increased heart rate
- Arrhythmia of heart contractions, manifested in the form of tachycardia, bradycardia, extrasystole, “ragged” rhythm
- Pain from the heart
- Dizziness
- Swelling, which is one of the late manifestations of the disease
- Fatigue, weakness, tiredness as a result of insufficient functioning of the heart
- Decreased performance
Diagnosing the disease in the early stages of development is difficult.
The following are used as diagnostic methods:
- Methods for collecting and analyzing the patient’s medical history and daily life and work activities
- Methods for collecting and analyzing patient complaints
- Physical examination techniques, including listening to the heart (auscultation), pulse, and checking blood pressure
- Methods of laboratory tests of blood samples (general, biochemical), including cholesterol levels
- Methods of electrocardiography, echocardiography, Holter monitoring of the electrocardiogram, magnetic resonance imaging, myocardial scintigraphy, radiography
Unfortunately, diagnosis of the disease usually takes place at the stages of the disease, when the patient is concerned about serious complications and manifestations of acute heart failure.
Medications. Names and treatment regimens
Medicines are aimed at improving a person’s condition, normalizing lipid metabolism and blood flow. Additionally, atherosclerotic plaques are stabilized.
In case of illness, the following groups of medications can be prescribed:
- hypolipidemic;
- anticoagulants;
- antihypertensive.
Lipid-lowering drugs
Drugs in this group normalize the lipid profile.
Lipid-lowering drugs are prescribed in the following cases:
- angina pectoris;
- atherosclerosis;
- prevention of cardiovascular diseases in the presence of risk factors (smoking, arterial hypertension, etc.);
- increased content of atherogenic lipoproteins;
- secondary prevention of cardiovascular diseases after ischemic disease.
Drugs in this group are divided into the following types:
- Statins (Atoris, Atorvastatin, Crestor). The drugs reduce the concentration of cholesterol in the blood.
- Fibrates (Ciprofibrate, Fenofibrate, Clofibrate). They inhibit the synthesis of VLDL and LDL and can increase the destruction of LDL. When used systemically, the content of atherogenic fractions of lipoproteins decreases and the amount of HDL increases.
- Vitamin PP (Nicotinic acid, vitamin B3). Normalizes the concentration of lipoproteins, reduces the level of LDL, increases the content of HDL.
- Bile acid sequestrants (Guarem, Questran). The drugs bind bile acids that enter the intestines, and the complexes are excreted in the feces. That is, the body synthesizes new bile acids and uses cholesterol as a raw material. Additionally, the amount of LDL and total cholesterol is reduced.
- Cholesterol absorption inhibitors (Ezetrol). The group slows down the absorption of cholesterol, the body breaks down LDL. As a result, fat metabolism is normalized.
- Polyunsaturated fatty acids (Omacor, OmegaTrin, Linetol). The medications have a positive effect on the lipid profile and have a mild effect.
Anticoagulants
The drugs reduce blood clotting, it becomes liquid and passes through the vessels more easily.
Anticoagulants prevent blood clots from forming. Additionally, the drugs reduce the likelihood of a heart attack, stroke, and blood vessel blockage. But blood clots that previously formed do not dissolve under the influence of medications of this group.
Anticoagulants are divided into the following types:
- direct action (Heparin, Sodium citrate, Fraxiparine) – affect coagulation factors directly in the blood;
- indirect action (Warfarin, Sinkumar, Phenilin) - inhibit the synthesis of blood coagulation factors in the liver.
Antihypertensive medications
Drugs in this group are prescribed to people with high blood pressure.
Antihypertensive drugs are divided into the following types:
- angiotensin-converting enzyme or ACE inhibitors (Captopril, Enalapril, Enap) - dilate the lumen of blood vessels, reduce blood pressure without changing heart rate and cardiac output;
- diuretics (Furosemide, Veroshpiron, Spironolactone) – remove excess water from the body, unload the heart and blood vessels;
- angiotensin receptor blockers (Valsartan, Irbesartan, Valsacor) - disrupt the contact of angiotensin with the receptors of cells of internal organs, the vascular wall relaxes, blood pressure decreases;
- adrenergic blockers (Bisoprolol, Betalok, Concor) – block adrenergic receptors, reduce blood pressure and slow down the heart rate;
- calcium antagonists (Verapamil, Diltiazem, Nifedipine) – reduce the penetration of calcium ions into vascular muscle cells, eliminate arterial spasm.
Possible causes of aortic atherosclerosis
The immediate causes of the development of atherosclerotic lesions of the aorta and other vessels have not been identified to this day.
Risk factors for the development of aortosclerosis include the presence of high blood pressure, age over 40 years, and male gender. Atherosclerosis of the aorta and other vessels is more common in people who smoke, are overweight and have a low level of physical activity.
Additional factors that increase the likelihood of developing atherosclerosis include constant nervous tension, the presence of diabetes mellitus, family history, and some psychological characteristics.
The main mechanism for the development of aortosclerosis and other localizations of atherosclerosis is a violation of fat metabolism in the body.
Surgery
If conservative treatments are not effective, your doctor may recommend surgery.
For atherosclerosis, the following types of intervention are used:
- coronary angioplasty;
- coronary artery bypass surgery;
- heart transplantation.
Coronary angioplasty
During the operation, a catheter is inserted into a large artery, at the end of which there is a deflated balloon. The doctor advances the catheter through the vessels until he reaches the area of narrowing. Everything is carried out under the control of equipment. Then the balloon is inflated and deflated several times, the lumen of the vessel expands.
Next you need to consolidate the result. To do this, a stent is installed, which is a small metal frame. It is inserted into the vessel to eliminate its narrowing.
During the operation, the atherosclerotic plaque is not removed.
Coronary artery bypass surgery
It is not always possible to restore blood flow with angioplasty. Therefore, the use of shunting is allowed. The operation is complex. Its goal is to create an escape route bypassing the narrowed vessel. A section of the patient's thoracic artery, radial artery, or saphenous vein is cut out from the patient's leg. Then, an incision is made above the place where the narrowing occurred and a vascular prosthesis is sewn.
Bypass surgery takes 3–4 hours and is also accompanied by long-term rehabilitation. Therefore, this operation is performed only on seriously ill patients. Most often, the intervention is accompanied by the connection of a heart-lung machine.
Heart transplant
If the heart is in poor condition and bypass surgery and angioplasty are unsuccessful, organ transplantation is possible.
The operation requires a highly qualified doctor, modern equipment, and financial investments. Therefore, it is not always possible to intervene.
Is it possible to completely cure the pathology, how long does the therapy last?
Atherosclerosis can be cured only in the early stages. Therapy can last from 5-6 months to 1-2 years. In severe cases, the only thing a doctor can do is to alleviate the symptoms of the disease and stabilize blood cholesterol levels.
After starting to take medications, the effect occurs within 1-2 months, then it is maintained at the same level. If lowering cholesterol is not effective enough, the doctor may increase the dose of the drug or prescribe an additional drug.
Recipes for folk remedies
Atherosclerosis of the heart vessels (symptoms and treatment are related factors) is a disease for which the use of herbal recipes is possible.
Traditional methods are used as part of complex therapy. This way you can achieve maximum effect from use.
Traditional methods allowed for atherosclerosis:
- Garlic tincture. To prepare the recipe, you need to take 250 g of peeled garlic cloves and grind them to a paste. Then pour in 1 liter of purified food alcohol (40 degrees) or vodka. Place in a dark, cool place for 21 days. Squeeze the mixture and filter through cheesecloth. On the first day, take 1 drop of the product, then increase the amount daily. When the indicator is equal to 25, you need to start the countdown. It is better not to drink the drops in their pure form; they must be mixed with water. The recipe is used to cleanse blood vessels, as garlic relaxes the walls of the artery and expands its lumen.
- Thyme. To prepare the recipe, you need to take 1 tbsp. dried herbs and 500 ml hot water. Leave for 60 minutes. in a tightly closed container. Filter through cheesecloth, take 1/3 cup 3 times a day before meals. The recipe relaxes the muscle layer of the vascular walls and has an expanding property. Additionally, the mixture improves blood flow.
- Rose hip. To prepare the recipe, you need to chop 100 g of fresh fruits of the plant, pour purified ethyl alcohol or vodka (400 ml) into the raw materials. Close the container with a lid and put it in a dark and cool place for 15 days. You need to shake the container daily. Take 25 drops per day.
Atherosclerotic cardiosclerosis: causes, treatment, prognosis
Cardiosclerosis is a complication of coronary heart disease (CHD), which is manifested by the replacement of cardiac muscle cells with connective tissue. A decrease in the number of cardiomyocytes reduces the performance of the heart. This is how heart failure develops. Its severe forms are incurable, so the disease quite often causes death in people.
Narrowing of the coronary arteries leads to coronary heart disease, a chronic disease in which the cells of the heart muscle do not receive enough oxygen. Lack of oxygen and nutrients disrupts intracellular metabolism. For some cardiomyocytes, circulatory disorders are fatal. The muscle cells of the heart cannot reproduce, so connective tissue takes the place of the dead. This is how scars appear that are unable to engage in the work of the heart.
Diet
Proper nutrition must be used as part of complex therapy, that is, in conjunction with other methods.
Diet principles:
- eat 5 – 6 times a day;
- do not exceed serving size (150 – 300 g);
- eat every 3 – 4 hours;
- exclude fried, salted, smoked foods;
- exclude sweets, flour, spicy foods;
- add vegetables and fruits to your diet;
- cook food using steam, boiled or bake food in the oven;
- the diet should include vegetable soups, porridge with water or milk;
- replace fatty foods with low-calorie ones - for example, buy chicken or turkey instead of pork;
- exclude strong coffee, black tea, alcohol - it is better to drink compote, green tea, juice;
- do not forget about the drinking regime - at least 1.5 liters of clean still water per day.
Prevention measures
You can prevent atherosclerosis of the pulmonary aorta if you lead a healthy lifestyle, get rid of bad habits and avoid stress. It is important to eat right and exclude fatty, fried and spicy foods from your diet. Preference is given to steamed food, fresh vegetables and fruits. An active lifestyle and swimming or jogging are recommended.
Pulmonary aortosclerosis is a chronic pathology that is characterized by an increase in tissue mass on the walls of the aorta and the formation of cholesterol plaques . Due to this, a narrowing of the artery of the respiratory organ is observed, which leads to a decrease in the supply of oxygen to the body. This leads to serious complications and can even cause death. The disease usually occurs in a very severe form and is almost always accompanied by pulmonary hypertension. Approximately half of the world's population aged about 50 years suffers from this pathology.
Possible complications
Atherosclerosis of the heart vessels is a disease in which complications may develop. Most often, the consequences appear in the absence of treatment for the pathology.
Possible complications:
- myocardial infarction – a form of ischemia that occurs with the development of necrosis;
- angina pectoris is a pathology in which the delivery of oxygen to the myocardium does not meet the need;
- atrial fibrillation - an abnormal heart rhythm, that is, rapid and irregular contraction of the organ;
- death.
A disease called atherosclerosis is a chronic pathology in which cholesterol and lipoprotein fractions are deposited in the walls of blood vessels. As a result, the lumen narrows and complete blockage is possible. If the disease affects the blood vessels of the heart, symptoms include pain in the organ area, shortness of breath, and fatigue.
If signs of pathology appear, you should visit a doctor who will refer the person for examination. After receiving the diagnostic results, treatment is prescribed. Therapy depends on the stage of development of the disease - in phases 1 and 2, medications, proper nutrition and alternative therapy are recommended, and in severe cases, surgery is necessary.
The disease cannot be completely cured. Therefore, it is necessary to consult a specialist in a timely manner and follow all his recommendations in order to reduce the likelihood of further development of the pathology and alleviate the person’s condition.
Forecast
The diffuse form of cardiosclerosis is considered unfavorable in its prognosis. For example, with the formation of connective tissue at the site of a transmural infarction, the risk of developing an aneurysm increases, the rupture of which most often leads to immediate death. In cases where cardiosclerosis arose as a result of natural age-related changes, this course of the disease is usually favorable.
Cardiosclerosis is a common heart pathology, the severity of which depends on the volume of affected tissue and the general condition of the body. If a person notices symptoms of this disease, he should consult a doctor as soon as possible, who will examine him and prescribe therapy.