An abnormal heart rate is called arrhythmia. This is a heterogeneous group of pathological processes, they agree on one thing: a change in the nature of the activity of cardiac structures.
There are several variants of dysfunction: tachycardia - acceleration of the rhythm, bradycardia - slowing of the pulse, and uneven intervals and delays between each further heartbeat (fibrillation, flutter, flicker). In the latter case, there is no clear pattern at all.
Normal activity is considered to be a contraction frequency of 60-90 beats or a little more, depending on age and physical fitness, with equal time intervals between systoles and diastoles. All deviations are considered as probable pathology until proven otherwise.
Natural factors in the development of the problem are taken into account later, if there is no evidence of organic pathology.
There are threatening and non-threatening types of heart failure. The former are several times more common, but one can be distinguished from the other only through objective diagnostics (electrocardiography, ultrasound, 24-hour monitoring).
Types of outages
The arrhythmic process has many varieties. Some are more dangerous, others pose less of a threat to life and health.
Non-fatal forms
- Single extrasystoles. They feel like an extra heartbeat and represent functional impairments of a short-term nature. They develop as a result of extraordinary contractions of the heart muscle due to the generation of additional electrical impulses by the atrioventricular node, atria or ventricles. An important distinguishing feature of such interruptions in the heart is the singularity of changes. Moreover, this is not a regular problem. Up to 6-70% of all cores suffer from extrasystole, which makes this form the most common. There are no symptoms at all, so it is almost impossible to determine whether you have a problem. This is a variant of an incidental finding during an ECG.
- A mild form of atrial fibrillation (with a heart rate of up to 110 beats per minute). It is a disruption of the functioning of the entire muscular organ, when an electrical impulse is generated not only by the sinus node, but also by other cardiac structures. The process is noticeable, but does not pose any danger due to good control. Also called atrial fibrillation.
- Conduction disorder of the His bundles. Likewise, it is not characterized by manifestations. Since there are no symptoms, it is impossible to detect the process on your own; diagnostics are required. It is possible to cope with pathological changes using medicinal methods in a short time.
- 1st degree atrioventricular block. It is characterized by a violation of the passage of electrical impulses from the sinoatrial node to the atrioventricular node and further to the ventricles. At an early stage, changes are minimal, so quick correction is possible. There is almost no danger. In the future, there is a threat to life (over the next several weeks or months).
- Sinus tachycardia. Acceleration of cardiac activity due to excessive stimulation of the pacemaker. Develops as a response to internal or external controllable factors. In the early stages it does not require correction at all. It appears brightly, but does not pose a danger to health or life.
- Bradycardia. Reverse process. It also develops due to dysfunction of the sinus node. In 40-50% of cases it is of physiological origin, not associated with pathogenic processes.
Dangerous species
Requires urgent medical attention. It is impossible to predict in advance when a fatal complication will occur. Immediately after identifying the problem, treatment should be prescribed, preferably in an inpatient setting or under the constant supervision of a cardiologist as part of outpatient diagnostics.
- Multiple extrasystoles. Unlike single ones, they are repeated many times, repeatedly. As a result, cardiac structures work chaotically and cannot be coordinated. Possible cardiac arrest. It happens suddenly. Since this type of pathological process almost never makes itself known, it is difficult to identify the problem.
- Ventricular flutter.
- Advanced atrioventricular blockade, complete or 2 degrees. The conductivity of cardiac structures is impaired. In this case, the ventricles are “switched off”, which is fraught with sudden cardiac arrest. It is impossible to restore functional activity even within the framework of emergency resuscitation.
- Paroxysmal tachycardia. It is characterized by an acceleration of the frequency of contractions of the muscular organ, the number of “movements” can reach 150-180 or more, these are full-fledged beats that the patient feels as if the heart is turning over and jumping out of the chest.
Heart rhythm disturbances are the result of a process of cardiac, endocrine or neurological origin. Less commonly, a natural phenomenon occurs that is not related to organic changes.
Types of arrhythmia and their features
Our heart can fail in different ways, so the medical community identifies the following types of arrhythmia:
- Sinus tachycardia: characterized by rapid contraction of the heart, more than 90 beats per minute. Usually provoked by excessive physical or emotional stress, it can be caused by colds;
- Sinus bradycardia: the contraction frequency drops to 55 beats per minute, as a rule, it is provoked by poor thyroid function. With sinus bradycardia, weakness and drowsiness often occur;
- Sinus arrhythmia: the beat frequency is not uniform. This type of arrhythmia most often affects adolescents and children. Often this disease is associated with breathing; such arrhythmia often does not require medical intervention and does not interfere with normal life;
- Atrial fibrillation or atrial fibrillation. It is dangerous because often the patient does not even know about the disease, but sometimes you can feel fluttering in the chest area, as well as pain, and shortness of breath often occurs. People who abuse alcohol and have thyroid disease are at risk. The main symptom is a lack of pulse, that is, the heart rate exceeds the pulse rate when listening;
- Heart block: can be determined because a person periodically loses his pulse altogether. Often, a sick person suffers from fainting, and with a complete blockade, death is possible.
From the descriptions, the main symptoms of arrhythmia can be identified, these include: slow or fast heartbeat, shortness of breath, chest pain and lightheadedness. But the symptoms, for the time being, may manifest themselves mildly and many tend to attribute them to banal fatigue, so be careful and listen to your health.
Development mechanism
There are 4 ways of causing heart failure.
Among the possible options:
- Impaired generation of electrical impulses in the sinus node. The natural pacemaker creates an excessive or, more often, insufficiently strong signal. As a result, the cardiac structures contract evenly, but weakly, which leads to the need to accelerate the rhythm to more quickly “pump” blood and provide tissues with oxygen.
- Advanced contraction of individual areas of the heart. As a result of increased excitability of organ cell bundles.
- Blockade of the atrioventricular node. Impaired tissue conductivity. Formed after suffering functional lesions.
- Propagation of an electrical impulse in certain areas, disruption of the further movement of the signal. Ends with uneven contraction.
Interruptions in the heart are the result of four types of organic abnormalities: tissue conductivity changes or the creation of an electrical impulse. A mixed mechanism is often observed.
Cardiac causes of the development of the pathological process
- Ischemic disease. Deficiency of nutrition (trophism) of the myocardium. The inability to supply the organ itself with blood leads to changes in the cardiac structures. The classic end of the process is a heart attack. The problem manifests itself as shortness of breath and various types of rhythm disturbances. Often the condition cannot be detected.
- Arterial hypertension. Persistent increase in pressure. As a rule, patients with a long history of illness suffer from interruptions in the functioning of the heart; the longer the process lasts, the worse the prognosis. A comprehensive assessment of the entire cardiovascular system is necessary.
- Myocardial infarction. Acute malnutrition of the muscle layer and neurosis of cardiomyocytes (cells). It ends in death in 35-50% of cases, more often in the presence of concomitant diseases or complications.
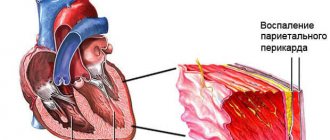
- Cardiosclerosis. Replacement of functional tissue with scar structures. It becomes the result of inflammation or a heart attack.
- Endocarditis. Infectious or autoimmune (less commonly) pathologies of active structures and tissues. In the absence of timely treatment or with an aggressive course of the process, destruction of the atria occurs. Prosthetics will be required.
An uneven pulse is the result of hemodynamic disturbances, stimulation of organ function as a result of functional deviations.
Somersaulting heart - what kind of pathology is this?
Extrasystole is a pathological process in which a change in the normal myocardial rhythm is observed. The pathology is accompanied by extraordinary contractions of an intense nature, both of the entire human organ and of the individual ventricles.
As the disease develops, the release of blood from the myocardium decreases. The process leads to a decrease in coronary blood flow and in the veins supplying the brain.
This condition provokes the formation of angina pectoris, the occurrence of frequent cardiac fainting and paresis. The result of the pathology is the acquisition of atrial fibrillation by a person, as well as the possibility of sudden death.
Doctors say that pain and discomfort in the chest occurs in most people. Isolated manifestations are observed even among young people. In people who have crossed the 50-year mark, pathology is recorded in 65-80% of cases.
Extracardiac causes
- Intense physical activity. As a result of overexertion, the activity of muscle structures accelerates. This occurs due to the need to provide organs and tissues with blood and nutrients, respectively. Trained people are less susceptible to changes in the functional activity of the heart. Usually we are talking about inadequate physical activity.
- Stomach ulcer, problems with the duodenum. Pathologies of the gastrointestinal tract. For the development of interruptions in the functioning of the heart, one condition must be met: the appearance of constant weak bleeding and, accordingly, anemia. Once the condition has stabilized, the cardiac structures resume normal activity.
- Violation of body temperature. Both hypothermia and the opposite phenomenon. Usually occurs when climate conditions change or when you are in an aggressive environment.
- Endocrine pathologies. Including hyperthyroidism (excess thyroid hormones), hypercortisolism (excessive amounts of cortisol and adrenal cortex substances), diabetes mellitus. Accompanied by severe symptoms, it is difficult to confuse the disease with anything else. A competent endocrinologist will immediately determine the presence of a problem.
- Intoxication of the body, poisoning. Nicotine, narcotic substances, caffeine, drugs to lower blood pressure, cardiac glycosides, salts of heavy metals, and other poisons.
- Neurogenic disorders manifested by vegetative-vascular dystonia (VSD is not an independent diagnosis, but a symptom).
- Viral and bacterial infections. Any type. Sinus tachycardia occurs more often, other phenomena occur less frequently.
- Traumatic lesions of cerebral structures and the central nervous system (concussion as a classic variant). The cause of the interruptions is damage to the cortex or trunk, where the center responsible for the normal activity of the muscular organ is located. It is very dangerous.
- Other injuries: electrical injuries, fractures and bruises of the chest.
If the heart beats unevenly, the reason lies in endocrine, cardiovascular, gastrointestinal, and neurogenic pathologies.
The diagnosis is made by exclusion. In the absence of evidence for organic disorders, and if natural factors cannot be identified, they speak of an idiopathic process.
Heart stopping with VSD
With vegetative-vascular dystonia, people may experience interruptions in heart rhythm. A person begins to feel as if his heart stops in his chest for a moment, leading to anxiety and fear of death.
This phenomenon is short-term, but causes sufficient concern.
Disturbances in the functioning of the cardiovascular system can often be observed as one of the symptoms of VSD, which does not always require medical intervention.
If freezing occurs frequently, causes discomfort, and bothers you even during rest, then this is a reason to consult a therapist.
Symptoms
The clinical picture directly depends on the type of violation of the functional activity of the organ.
Averaged complexes can be like this:
- Freezing of the heart. Beats are missed as a result of uneven signal distribution.
- Too frequent contractions and the reverse process.
- Dyspnea. For no apparent reason. Occurs as a consequence of hypoxia of tissue structures.
- Chest pain. Regular.
- Cephalgia. Bales, shoots in the area of the back of the head or crown.
- Vertigo. Up to the complete loss of the ability to navigate in space.
- Fainting, loss of consciousness.
The process can occur on a regular basis. With paroxysmal phenomena, a paroxysmal course occurs. Manifestations are absent in mild or mild forms of pathological processes.
The most serious symptom is if the heart skips beats (intermittent pulse). This is an indication of a disturbance in the distribution of the electrical impulse and a possible blockade of the nodes.
Treatment of the disorder
Treatment of patients with obvious cardiac arrhythmias largely depends on the type and nature of the disease, as well as its degree. As a rule, doctors begin by treating the underlying disease that caused the disease. Most types of rhythm disturbances do not require drug treatment and can be eliminated by simple lifestyle changes. For example, a person should give up caffeine in all its forms, and also quit smoking. It is necessary to drink alcohol wisely and completely avoid stressful situations.
First aid at home
The following drugs are used to stop heart rhythm disturbances:
- Anaprilin (1 tablet) + Carvedilol (1 tablet) + motherwort (2 tablets). With tachycardia.
- Caffeine (1 tablet) + Eleutherococcus tincture (2 tsp) + alcoholic ginseng (20 drops). Against the background of bradycardia.
- Amiodarone (1 tablet) + Verapamil (1-2 tablets). If there is another type of arrhythmia.
You can't overexert yourself physically. You should lie down. As soon as organ dysfunction begins, it is recommended to call an ambulance. Primary measures are aimed at stabilizing the condition, but it is unknown when a relapse will occur and how it will end.
Heart failure - how dangerous can it be?
Oh, it will hurt and it will stop - that’s what many of us say after drinking it, when we are completely tired of taking a validol tablet. No, on the one hand, this approach to life may be good in some ways, it helps not to get upset in vain. But we must understand that problems related to heart health cannot be categorized as trifles. This is serious, and before giving up on the problem, let’s talk about what will happen if you don’t pay attention to the problem at all.
If you do not deal with the problem, then there is a high risk of developing diseases such as:
1. Congestive heart failure - the heart simply does not work efficiently, it wears out, but the body does not receive enough, since the blood moves slowly and nutrients are supplied intermittently;
2. Stroke, or rather ischemic stroke; unfortunately, this disease has a high risk of death.
Diagnostics
It is carried out under the supervision of a cardiologist and related specialists in the endocrine system, central nervous structures, etc. Since the form of the pathological process is not yet clear, it is better to conduct the examination in an inpatient setting. This will simplify information sorting, analysis and speed up the process.
An approximate diagram is as follows:
- Collection of patient complaints and anamnestic data. Bad habits, lifestyle and other important points are taken into account. The function of the patient himself is to talk about his feelings in as much detail as possible.
- Blood pressure measurement. Also heart rates using automatic or mechanical methods.
- Daily tonometry. Allows you to evaluate the dynamics of heart rate in the patient’s usual conditions. It is better to carry it out as part of an outpatient diagnosis. In a hospital setting, information may not be accurate.
- Electrocardiography with or without insertion of a sensor (to check the conductivity of cardiac structures). The most informative technique, it is used first.
- Echocardiography. Ultrasonic method. Allows you to visualize tissues and determine organic changes in structures.
- Load tests. With great care. It is possible to stop working as a result of uneven or inadequate activity.
Diagnosis is required in all cases. Interruptions in the functioning of the heart at rest are an indication of organic disorders of the endocrine, nervous or cardiovascular system. Often in a complex. You will need the help of several specialists.
Therapeutic tactics
Surgical or medical treatment is carried out. Approximate list of drugs:
- Calcium antagonists. Diltiazem and Verapamil. Restores normal vascular tone.
- Beta blockers. Carvedilol, Anaprilin, Metoprolol.
- Drugs for restoring the functional activity of the myocardium: Cordarone and analogues. They normalize the reduction process.
- Khindin, Novocainamide and other antiarrhythmic drugs. Selectively influence the source of the problem, putting the rhythm in order.
- Glycosides: Digoxin, tincture of lily of the valley.
There are many medicines. Since heart failure is varied, tactics will always be different. Specific names are selected by the doctor after a thorough diagnosis. You cannot take anything on your own.
Surgical and minimally invasive care includes electrocardioversion, radiofrequency ablation, and installation of an artificial pacemaker. These are extreme measures.
The use of folk recipes does not make sense. It's a waste of time. But you need to change your lifestyle:
- Quit smoking and alcohol.
- Sleep 8 hours.
- Walk for 2-3 hours a day.
- Taking vitamin-mineral complexes.
- Avoiding stress.
- Correction of the diet (less fatty, fried, smoked, salt up to 7 grams per day, no semi-finished products or canned food, everything else in moderation).
The same recommendations apply as part of prevention.
What is the name of the condition when the heart freezes?
An abnormal heart rhythm (arrhythmia) is called extrasystole. This condition occurs due to excessive excitation of part or all of the myocardium. Such a reduction is provoked by extraordinary impulses. Normally, the impulse comes only from the sinus node.
After untimely contractions, a compensatory pause occurs, which, in turn, can be complete or incomplete. This phenomenon in itself is safe, but if organic heart damage is present, then factors that negatively affect health arise.
The constant alternation of normal contractions and freezing is called bigeminy in medicine. If there are two contractions for one freezing, we speak of trigeminy.
There is also such a thing as quadrigymenia.
Causes and types of heart failure
Depending on the cause, functional and organic extrasystoles are distinguished. The first ones occur in people who do not have heart pathologies. The reasons in this case are hidden in dysfunction of the autonomic nervous system. Smoking, stress, alcohol, coffee, and vitamin deficiency can trigger freezing. In women, this feeling can occur under the influence of hormones.
The second - organic - occur in heart pathologies, for example, ischemia, dystrophy, cardiosclerosis, inflammation, defects, hypertension, cardiomyopathy. This is observed in most people who have suffered a myocardial infarction. In this situation, it is caused by necrosis of areas of the organ.
Extrasystoles are distinguished by the number of impulse foci. They are divided into monotropic (one section) and polytropic (several). Two foci may be observed at once: one is normal, sinus, the other is extrasystolic.
According to the place of occurrence, extrasystoles are divided into atrial, atrioventricular and ventricular.
Symptoms when heart palpitations occur
- With atrial extrasystole, which. It is worth noting that it occurs quite rarely; organic damage to the organ is observed. When the number of its contractions increases, atrial fibrillation and paroxysmal tachycardia may develop. In this case, the sensation of freezing observed most often occurs in a supine position of the body;
- The atrioventricular form is also quite rare. The danger of this phenomenon is that this can lead to reverse flow of blood from the atria into the veins;
- Ventricular extrasystoles are the most common. This phenomenon can progress to ventricular tachycardia. It is also dangerous in case of myocardial infarction, as it can lead to ventricular fibrillation.
Symptoms of pathology, as a rule, are visible only to a cardiologist who interprets the results of the electrocardiogram. But it is worth noting that when deciphering the results of a standard ECG, an error can occur and even a good cardiologist can make the wrong conclusion. Signs of extrasystole can be confused with conduction disturbances and a number of other pathological phenomena. In turn, incorrect diagnosis leads to inadequate treatment.
As for the more obvious symptoms that the patient himself can notice, in most cases these do not appear. Sometimes there may be a sensation of tremors in the chest, a feeling of turning over or a sinking heart, and interruptions in the functioning of the organ. During the compensatory pause, dizziness, lack of air, weakness, aching pain and a feeling of compression behind the chest may occur.
How to treat heart failure
Therapy is aimed at eliminating the root cause of the disorder and stopping it itself. It is possible to restore the normal functioning of the organ with the help of antiarrhythmic drugs, but they are effective only for the duration of their use. If the cause of freezing is hidden in organic lesions of the myocardium or disorders of the coronary circulation, then appropriate therapy is needed, aimed at dilating blood vessels.
If the reasons are hidden in emotional or physical stress, then rest and taking medications that reduce cardiac excitability are recommended. In any case, smoking and drinking alcohol are contraindicated for patients.
When heart disease is present, treatment is usually aimed at preventing life-threatening conditions. For this reason, people with hypertension, coronary artery disease, myocarditis, defects, etc. should be regularly examined by a cardiologist.
Such patients require constant monitoring of the function of the cardiovascular system.
What is the risk of heart stopping?
Given the functional nature of this phenomenon, serious complications do not arise. If extrasystole occurs against the background of myocardial infarction, cardiomyopathy, or myocarditis, then the person is at risk. The atrial form can lead to atrial fibrillation and tachycardia. The supraventricular form, if left untreated, ends in fatal arrhythmia and, as a consequence, arrhythmic death.
Heart failure with vegetative-vascular dystonia (VSD)
VSD is a complex of pathologies that arise as a result of disturbances in vascular tone of the autonomic nervous system. Dystonia is a rather dangerous condition, as it can provoke the development of arterial hypertension, neurosis, and significantly worsen the quality of life.
VSD is accompanied by rapid heartbeat (constant or attacks), hyperhidrosis, headaches, tingling in the heart area, pallor or, conversely, redness of the skin, chilliness of the limbs, and a tendency to faint.
Treatment is prescribed depending on the manifestations of vegetative-vascular dystonia.
Typically it includes:
- Normalization of the daily routine;
- Balanced diet;
- Sufficient time outdoors;
- Elimination of stress;
- Increased physical activity;
- Working with a psychologist;
- Massotherapy;
- Acupuncture;
- Water and physiotherapeutic procedures.
Therapy can be aimed at eliminating foci of infection and concomitant diseases. Patients are advised to undergo clinical observation and preventive measures. As for medications, sedatives (sedatives), tranquilizers, antidepressants, nootropics, vitamins and minerals, beta-blockers, and herbal psychostimulants are prescribed.
Acupressure for work interruptions and heart failure
First of all, you need to consult a doctor, who, in turn, must make a diagnosis and establish the cause of the rhythm disturbances. After this, you must strictly adhere to the specialist’s instructions, observe the dosage and regularity of taking the medications he prescribes, avoid stressful situations, and adjust your diet and daily routine.
As first aid, you can use some tricks, for example, “straining,” pressing on the eyeballs, or performing a massage of the sinocarotid zone.
Acupressure will help with functional disorders of the cardiovascular system. This procedure will improve your well-being and normalize the rhythm during arrhythmia. As a rule, massage involves treating biologically active points on the upper and lower extremities, as well as the ears.
Acupressure is carried out twice a day, affecting each point for 2-3 minutes. Only 3-4 points are processed at a time. During an attack, the points of the heart channel and a number of others are affected.
In medical institutions, massage can be performed using electropuncture.
In case of functional disorders, you can get rid of the feeling of a sinking heart without radical methods and medications, for example, by changing your diet, adding foods rich in potassium and magnesium to the menu, and doing physical therapy. Organic disorders cannot be avoided without the help of a cardiologist.
mjusli.ru
Possible complications
Among the likely consequences of untreated or insufficiently compensated interruptions are:
- Ventricular fibrillation. In 100% of cases it ends in cardiac arrest. As soon as the process has begun, you need to prepare for resuscitation measures.
- Cardiac asthma as a result of insufficient trophism of the pulmonary structures.
- Cardiogenic shock. Mortality is close to 100%.
- Brain stroke or chronic ischemia of the central nervous system.
- Thromboembolism.
- Impaired tissue nutrition, hypoxia with gradual muscle atrophy, organ dysfunction.
- Collapse as a result of a critical decrease in blood pressure.
All conditions require urgent hospitalization and treatment in a cardiology hospital.
Forecast
Forecasts are determined by the type of violation and the state of the process.
- Non-hazardous forms of treatment do not require. It is necessary to eliminate the root cause of the phenomenon and everything will return to normal.
- Other types involve etiotropic treatment (elimination of the root cause) and symptomatic correction.
- Severe organic pathologies require lifelong exposure.
The probability of developing the described complications over a 3-5 year period without treatment is 35-40%. With proper and comprehensive treatment - 10-15%.
If the heart beats intermittently, the causes are pathological in 60% of cases, less often natural, not requiring medication or surgical correction. It is important to contact a cardiologist in time. It is impossible to say in advance what form of the process we are talking about. Everything is revealed during diagnostics.