CORONARY HEART DISEASE (I20-I25)
Note.
For morbidity statistics, the definition of “duration” used in rubrics I21, I22, I24 and I25 includes the length of time from the onset of an ischemic attack to the patient’s admission to a medical facility. For mortality statistics, it covers the period of time from the onset of an ischemic attack to the onset of death. Included: with mention of hypertension (I10-I15)
If necessary, indicate the presence of hypertension, use an additional code.
Included: myocardial infarction, specified as acute or specified duration of 4 weeks (28 days) or less from onset
Excluded:
- some current complications after acute myocardial infarction (I23.-)
- myocardial infarction: previous (I25.2)
- specified as chronic or lasting more than 4 weeks (more than 28 days) from onset (I25.8)
- subsequent (I22.-)
This category is used to code infarction of any myocardial site occurring within 4 weeks (28 days) of the onset of the previous infarction
Included:
- growing (extension)
- recurrent myocardial infarction (recurrent)
- repeated myocardial infarction (reinfarction)
Excluded: myocardial infarction, specified as chronic or with an established duration of more than 4 weeks (more than 28 days) from onset (I25.8)
Excluded: listed conditions:
- accompanying acute myocardial infarction (I21-I22)
- not specified as current complications of acute myocardial infarction (I31.-, I51.-)
Excluded:
- angina (I20.-)
- transient neonatal myocardial ischemia (P29.4)
ICD-10 alphabetical indexes
External Causes of Injury - The terms in this section are not medical diagnoses, but rather a description of the circumstances under which the event occurred (Class XX. External Causes of Morbidity and Mortality. Heading Codes V01-Y98).
Medicines and chemicals - table of medicines and chemicals that have caused poisoning or other adverse reactions.
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997 No. 170
The release of the new revision (ICD-11) is planned by WHO in 2022.
Abbreviations and symbols in the International Classification of Diseases, 10th Revision
NOS
- without other instructions.
NEC
— not classified in other categories.
†
— code of the main disease. The main code in the dual coding system contains information about the underlying generalized disease.
*
- optional code. An additional code in the double coding system contains information about the manifestation of the main generalized disease in a separate organ or area of the body.
general information
Short description
Angina pectoris (HF) is a pathophysiological syndrome in which, as a result of one or another disease of the cardiovascular system (CVS), a decrease in the pumping function of the heart occurs, which leads to an imbalance between the hemodynamic need of the body and the capabilities of the heart.
Protocol code: H-T-007 “IHD, exertional angina FC3.
Post-infarction cardiosclerosis" For therapeutic hospitals
Diagnostics
The clinical picture of angina pectoris is similar to many other diseases, and not only of the heart. Symptoms can be caused by myalgia, neuralgia, stomach diseases, inflammation of the costal cartilages, and diaphragmatic hernia. Compiling an anamnesis based on the patient’s complaints is an essential part of the diagnosis. But a doctor cannot diagnose the disease only by describing the pain, even if it has features characteristic of angina pectoris.
The full diagnostic looks like this:
- Taking an anamnesis, examining the patient, measuring blood pressure, listening with a phonendoscope.
- Taking clinical and biochemical blood tests, analysis of glycemia, and thyroid hormones.
- Electrocardiogram (ECG) at rest and during exercise.
- Daily monitoring of heart function using Holter.
- Ultrasound of the heart (echocardiography) at rest.
- Stress echocardiography.
- Scintigraphy with drug or physical activity.
- Coronary angiography (X-ray with contrast, which is injected directly into the coronary arteries using an angiocatheter).
Based on the data obtained, the cardiologist diagnoses the disease. All studies conducted provide information, including information about concomitant pathologies. Coronary angiography is used in severe cases when heart surgery is necessary or if it was not possible to make an accurate diagnosis using other methods.
Classification
Classification of coronary heart disease (CHD) VKSC AMS USSR 1989
1. Sudden coronary death
2. Angina: - exertional angina; - first-time exertional angina (up to 1 month); - stable angina pectoris (indicating functional class from I to IV); - progressive angina pectoris; - rapidly progressing angina pectoris; - spontaneous (vasospastic) angina.
3. Myocardial infarction: - large-focal (transmural); - small-focal; - primary recurrent, repeated (3.1-3.2)
4. Focal myocardial dystrophy
5. Cardiosclerosis: - post-infarction; - finely focal, diffuse.
6. Arrhythmic form (indicating the type of heart rhythm disorder)
7. Heart failure
8. Painless form
Angina pectoris
FC I (functional class) - latent angina . Angina attacks occur only during high-intensity physical activity; the power of the mastered load according to the bicycle ergometer test (VET) is 125 W, the double product is not less than 278 conventional. units; the number of metabolic units is more than 7.
FC II (mild angina) : angina attacks occur when walking on level ground over a distance of more than 500 m, especially in cold weather, against the wind; climbing stairs more than 1 floor; emotional excitement. The power of the mastered load according to the VEM sample is 75-100 W, the double product is 218-277 conventional units, the number of metabolic units is 4.9-6.9. Normal physical activity requires little restriction.
FC III (moderate angina) : angina attacks occur when walking at a normal pace on level ground for a distance of 100-500 m, or when climbing stairs to the 1st floor. There may be rare attacks of angina at rest. The power of the mastered load according to the VEM sample is 25-50 W, double product 151-217 conventional units; number of metabolic units 2.0-3.9. There is a pronounced limitation of usual physical activity.
IV FC (severe form) : angina attacks occur with minor physical exertion, walking on level ground for a distance of less than 100 m, at rest, when the patient moves to a horizontal position.
The power of the mastered load according to the VEM sample is less than 25 W, the double product is less than 150 conventional units; the number of metabolic units is less than 2. Load functional tests, as a rule, are not performed; patients experience a pronounced limitation of usual physical activity.
Progressive angina pectoris: what is it, treatment
Unstable angina is a period of exacerbation of coronary heart disease, accompanied by a high risk of developing necrotic changes in the myocardium and sudden cardiac death. Patients report severe chest pain, rhythm disturbances, shortness of breath and generalized swelling.
The diagnostic plan includes cardiography, echocardiography, laboratory methods and angiography. Treatment is based on complex drug therapy. If conservative measures are ineffective or the damage to the cardiac muscle is extensive, invasive methods (revascularization) are used.
Next, let's look at what this condition is, classification, causes, symptoms and treatment.
Unstable angina of the heart: what kind of disease is it?
Unstable angina is a pathological condition of the body in which severe pain occurs in the heart, radiating to the upper limbs, neck, and shoulders.
Since angina is considered unstable, this suggests that such attacks are difficult to predict, determine their cyclicity, and etiology.
In the patient’s body, they appear unexpectedly and also disappear imperceptibly until the next relapse.
This pathology is especially dangerous for human life, since exacerbation occurs without the presence of pathogenic factors and occurs at the most unexpected moment. It is not possible to control the characteristic illness, so it is necessary to consult a specialist in a timely manner, go to the hospital for examination, and then prescribe an intensive care regimen.
One of the types is unstable angina, which is a period of ischemic heart disease (coronary heart disease), occupying an intermediate place between angina with a stable course (angina pectoris) and acute myocardial infarction. Most often, the painful condition is diagnosed in men of retirement age, but this does not exclude the fact that it develops in young patients.
Currently, active advisory work is being carried out among the population aimed at disseminating information about what unstable angina is, how to identify it and where to go at the first manifestations of this disease.
Expert advice
- Stop smoking, as it significantly worsens the course of angina.
- Monitor your body weight, calculate the index and adjust it to your personal norm (you can do this here).
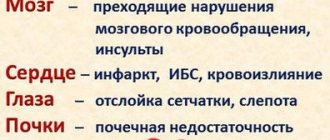
- Monitor your blood pressure - the higher it is, the greater the chance of developing a cardiovascular accident.
- Take medications designed to stabilize angina - statins, antiplatelet agents and beta blockers.
Why is it developing?
To date, it has been established that the main etiological factor in the progressive course of coronary artery disease in general and unstable angina in particular is the gradual narrowing of the lumen of the coronary arteries.
This creates the preconditions for cardiomyocyte necrosis and worsens the prognosis for the patient. The main cause of the pathological process is considered to be atherosclerosis.
The deposition of lipids on the endothelium of the coronary vessels leads to the formation of plaque, which can significantly reduce the volume of blood flow through the artery.
The size of the formation is of secondary importance; the presence of a large lipid core and a thin cap, when ruptured, blood clots begin to form, comes to the fore. At the same time, damaged vessels become overly susceptible to vasoconstrictor substances secreted by platelets, which entails additional narrowing of the lumen of the arteries.
Causes
Unstable angina develops against the background of rupture of a fibrous plaque in the coronary artery and the formation of a blood clot in it, which interferes with the normal blood supply to the myocardium and causes its hypoxia.
Damage to the integrity of the fibrous plaque can be caused by the accumulation of fatty deposits in it, inflammatory processes, lack of collagen and various hemodynamic disorders.
Also, the development of unstable angina can be provoked by:
- increasing the ability of platelets to stick together;
- hemorrhage into the plaque caused by rupture of a network of small blood vessels;
- local narrowing of the blood vessels of the heart, provoked by the release of vasoactive agents (serotonin or thromboxane A2);
- decreased antithrombotic properties of the endothelium.
Signs
What are the characteristic signs of unstable angina? Here's what a typical attack looks like:
- The pain occurs sharply, suddenly. It is felt behind the sternum and can radiate to the shoulder and other areas.
- Taking nitroglycerin and rest help relieve pain.
- The usual duration of an attack is less than 10 minutes. You can clearly name the time of its beginning and end.
- There is also usually a clear cause (physical stress, emotional stress).
Often, angina pectoris occurs in those who indulge in alcohol or spicy foods, since they also require more active work of the heart.
The insidiousness of the syndrome is that sometimes these symptoms are delayed by a day or even two. A person believes that there is no reason to worry, while he is already developing a myocardial infarction.
Kinds
Unstable angina is essentially an exacerbation of chronic ischemic heart disease (coronary heart disease). Under the influence of certain factors, the frequency of attacks, the duration of pain and their intensity increase. Physical exercise tolerance decreases.
There are 4 types of unstable angina:
- New-onset angina.
- Progressive
- Post-infarction.
- Princemetal.
Typically, any of the variants of unstable angina after treatment turns into stable angina, but with a decrease in exercise tolerance. This disease is popularly called a “pre-infarction condition” due to the fact that a complication often occurs in the form of myocardial infarction.
The second classification of unstable angina is based on the severity of the pathological process:
- 1st degree. The attack develops spontaneously, prevails for less than 2 months, and is characterized by the severe condition of the clinical patient.
- 2nd degree. Characterizes the subacute form of the disease, which is difficult to identify if symptoms are not expressed for less than 2 weeks.
- 3rd degree. The pain has been bothering me for the last 2 days, lasting up to 15 minutes, characterizing the acute period, the risk of developing myocardial infarction.
Clinical case
A 53-year-old woman, whom I had previously observed, came to see me. Her diagnosis was: “Ischemic heart disease, exertional angina pectoris II FC NK I stage CH 1 FC (NYHA). Arterial hypertension stage II, risk 4. Diabetes mellitus type 2, moderate severity, regulated .
Her main complaints were: increased frequency of attacks of anginal pain with the appearance of pain in the left half of the body (scapula, shoulder), increased shortness of breath during normal physical activity, lack of effect from 1 tablet of Sidnopharm. Objectively: auscultation heard an accent of the second tone over the aorta, 3 extrasystoles per minute. There was an increase in blood pressure to 150/95 mm Hg. Art.
Clinical tests are unchanged, blood sugar is 5.9 mmol/l. In the lipidogram, cholesterol increased to 6.1 mmol/l, VLDL to 1.9 mmol/l, LDL - 3.94 mmol/l. Troponin test is negative. During 3 days of Holter ECG monitoring, the following were revealed: single extrasystoles, ST segment elevation in the lateral leads after ascending to the second floor.
The results of coronary angiography showed the presence of atherosclerotic plaques in the anterior descending and circumflex branches of the left coronary artery.
The pain syndrome was successfully relieved with Nitroglycerin, and treatment was also carried out, including anticoagulants (Cibor) and metabolic therapy (potassium-magnesium mixture).
Statins (Mertenil), beta-blockers (Carvedilol), antiplatelet agents (Lopigrol), nitrates to resolve the attack (Nitrosprey) were prescribed, and stenting of the affected vessels was recommended.
The patient refused surgical treatment, but noted a decrease in the number of anginal attacks.
Progressive angina is a common pathology that requires immediate hospitalization when detected.
Based on my personal experience, I would like to note that surgical techniques show the best results in the treatment of this disease.
In most cases, my patients who underwent stenting and coronary artery bypass grafting of coronary vessels damaged by atherosclerosis noted a complete regression of clinical manifestations.
Do you have any friends or relatives who have undergone surgery for progressive exertional angina?
Symptoms of unstable angina
Manifestations occur when the lumen of the artery is blocked by 70% or more. Blood supply drops significantly, hemodynamics are disrupted. An attack is difficult to confuse with other processes.
Symptoms of unstable angina are determined from the nervous and cardiovascular systems:
- Intense pain in the chest on the left side. It radiates to the arm, shoulder blade, back or lower back.
- The duration corresponds to the length of the episode. Relief is carried out with analgesic drugs.
- Dyspnea. Against the background of physical activity. And if the pathological process has been going on for a long time, then even in a state of complete rest. Dyspeptic phenomena. Heartburn, nausea, vomiting, abdominal pain. They arise as a consequence.
Unstable angina in rare cases can be mistaken for an ulcer or other gastroenterological processes.
The duration of the episode is about 10-30 minutes or a little more. It goes away on its own if there is no heart attack.
Consequences
Due to its progressive course, unstable angina often causes complications. The main adverse effects are myocardial infarction and increased likelihood of sudden cardiac death. Possible cardiac arrhythmias:
- pathological tachycardia,
- bradycardia of the heart,
- extrasystoles,
- blockade of impulse conduction.
The constant nature of the process affects directly the myocardium, which leads to the development of chronic heart failure in both circulations. In severe cases, the outcome of CHF is pulmonary edema and death of the patient.
Diagnostic methods
To make a diagnosis, the following types of diagnostic procedures are used:
- general examination of the patient, listening to heart sounds, studying symptoms and medical history;
- a blood test to detect inflammatory processes;
- urinalysis – necessary to exclude other pathologies;
- ECG – to identify complications of coronary artery disease;
- Holter ECG - used to determine the conditions, frequency and duration of attacks;
- Echo-ECG - required to study the structure and size of the heart, as well as the condition of the valves and blood circulation;
- coronary angiography, which allows you to study blood flow in the heart vessels;
- Stress echo-ECG – carried out to identify areas of myocardial hypoxia under conditions of physical activity; scintigraphy, which allows you to study the condition of the walls and cavities of the heart.
Only after collecting complete data from all examinations can an appropriate diagnosis be made.
Advantages of the clinic
We employ highly qualified cardiologists and other doctors. They conduct successful examinations and treatment of various pathologies. The multidisciplinary nature of the clinic allows doctors of various specializations to work in a single team. Combining knowledge and skills makes it possible to eliminate even serious pathologies.
Our specialists comply with medical ethics, have extensive diagnostic capabilities and provide a safe and comfortable environment for all patients. In addition, our clinic adheres to a loyal pricing policy. Anyone can benefit from the help of professionals.
Unique comprehensive therapeutic programs are used in priority medical areas. Each patient is valuable to us primarily as an individual, and not as a patient with an interesting medical history or a client who creates the financial well-being of a specialist.
Source: https://gp195.ru/bolezni/nestabilnaya-stenokardiya-simptomy-i-lechenie.html
I23 Some current complications of acute myocardial infarction
Excluded: Conditions listed:
- not specified as current complications of acute myocardial infarction (I31.-, I51.-)
— accompanying acute myocardial infarction (I21-I22)
I23.0 Hemopericardium as an immediate complication of acute myocardial infarction
I23.1 Atrial septal defect as a current complication of acute myocardial infarction
I23.2 Ventricular septal defect as a current complication of acute myocardial infarction
I23.3 Cardiac wall rupture without hemopericardium as a current complication of acute myocardial infarction
Excluded: with hemopericardium (I23.0)
I23.4 Chordae tendinus rupture as a current complication of acute myocardial infarction
I23.5 Papillary muscle rupture as a current complication of acute myocardial infarction
I23.6 Thrombosis of the atrium, atrial appendage and ventricle of the heart as a current complication of acute myocardial infarction
I23.8 Other current complications of acute myocardial infarction
ICD-10: I20-I25 - Coronary heart disease
Diagnosis with code I20-I25 includes 6 clarifying diagnoses (ICD-10 headings):
- I20 - Angina pectoris [angina pectoris] Contains 4 blocks of diagnoses.
- I21 - Acute myocardial infarction Contains 6 blocks of diagnoses. Included: myocardial infarction, specified as acute or specified duration of 4 weeks (28 days) or less from onset. Excluded: some ongoing complications after acute myocardial infarction (I23.-) myocardial infarction: . transferred in the past (I25.2). specified as chronic or lasting more than 4 weeks (more than 28 days) from onset (I25.8). subsequent (I22.-) post-infarction myocardial syndrome (I24.1).
- I22 - Repeated myocardial infarction Contains 4 blocks of diagnoses. Included: recurrent myocardial infarction. Excluded: myocardial infarction, specified as chronic or with an established duration of more than 4 weeks (more than 28 days) from onset (I25.8).
- I23 - Some current complications of acute myocardial infarction Contains 8 blocks of diagnoses. Excluded: listed conditions: . accompanying acute myocardial infarction (I21-I22). not specified as current complications of acute myocardial infarction (I31.-, I51.-).
- I24 - Other forms of acute coronary heart disease Contains 4 blocks of diagnoses. Excluded: angina pectoris (I20.-) transient myocardial ischemia of the newborn (P29.4).
- I25 - Chronic ischemic heart disease Contains 9 blocks of diagnoses. Excludes: cardiovascular disease NOS (I51.6).
Chain in classification:
mkb10.su - International classification of diseases, 10th revision. Online version of 2020 with search for diseases by code and decoding.
Preventive actions
To prevent the development of the disease or recurrent heart attack, you must adhere to the following rules:
- Avoid intense physical activity.
- Don't be nervous and don't expose yourself to stress.
- Take prescribed medications regularly and on time.
- Stick to a diet (proper nutrition).
- Exercise therapy classes.
- Rejection of bad habits.
- Walk outdoors.
- Ensure adequate and healthy sleep.
- Regularly undergo medical examination.