Main causes of cerebral ischemia in newborns
Intrauterine hypoxia or asphyxia during childbirth (complete stop of oxygen supply)
- acute placental insufficiency (see fetal hypoxia), placental abruption
- long labor
- umbilical cord compression during contractions and pushing
Respiratory failure after birth
- congenital heart defects
- disturbance of the blood supply to the heart
- patent ductus arteriosus
- respiratory failure in premature infants
Decreased blood pressure after birth
- sepsis
- excessive bleeding (blood clotting disorders, liver injuries and other causes)
Degrees of development and their signs
The classification of ischemia is based on the severity of the syndrome of depression of cerebral functions. Infants have slightly different criteria than older children and adults.
This is due to the immaturity of the nervous system itself and the peculiarities of the neurological examination of newborns.
Newborns:
| Symptom | 1st degree | 2nd degree | 3rd degree |
| Onset of symptoms | First 7 days | First day | Immediately after birth |
| General state | Excitement, frequent crying, sometimes on the contrary drowsiness | Slow, frequent fainting | Profound cerebral depression |
| Muscle tone | Promoted | Weakened | Reduced or absent |
| Tendon reflexes | Promoted | Reduced | Reduced or absent |
| Newborn reflexes | Normal or slightly weakened | Reduced | Significantly reduced or absent |
| Breathing problems | Absent | Frequent episodes of sleep apnea | Frequent apneas, need for mechanical ventilation |
| Pathology of the cardiovascular system | Absent | Rhythm disturbance | Various rhythm disturbances, hypotension |
| Pathology of vision | Absent | Strabismus | Strabismus, nystagmus, uncoordinated eye movements |
| Convulsions | Absent | Possible clonic | Frequent, up to epistatus |
| Hydrocephalus | Absent | Possible transient | Progressive |
In adults and older children, total ischemia develops gradually, against the background of other diseases.
1st degree:
- Frequent headaches. In children, it may manifest itself as mood swings, constant crying;
- Insomnia;
- Fast fatiguability;
- Deterioration of memory, concentration, thinking;
- Initial coordination problems;
- Change in gait - becomes shuffling, mincing;
- Older people become intolerant of criticism;
- Character change;
- The appearance of pathological reflexes in the neonatal period is not in infancy.
2nd degree:
- Unsteadiness of gait, poor coordination of movements;
- Weakness in the limbs;
- Headaches and dizziness;
- Episodes of seizures are possible;
- Severe impairments of memory and attention;
- Emotional instability, apathy;
- Changes in personal qualities;
- Tearfulness is common;
- Patients gradually lose everyday and professional skills.
3rd degree:
- Profound loss of coordination of movements;
- Spastic paresis and paralysis;
- Various disturbances of consciousness, up to coma;
- Significant difficulty, up to complete inability to navigate in space;
- Profound impairment of memory, thinking, even dementia;
- Difficulty speaking;
- Uncontrolled urination;
- Parkinson's syndrome.
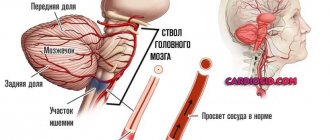
How does cerebral ischemia develop in newborns?
Oxygen carried by the blood to every cell of the body is essential for life. When its content is low, blood redistribution in organs begins. The brain and heart begin to receive the maximum possible amount of oxygen and nutrients, while other tissues and organs experience their deficiency.
If asphyxia continues, then these compensatory abilities are not enough for the life of nerve cells. They begin to die one after another. Hypoxic-ischemic encephalopathy of newborns occurs. The more brain tissue is damaged, the worse the prognosis for the baby will be. In some cases, due to hypoxia, cerebral hemorrhages may occur, which increases the risk of an unfavorable outcome.
Causes of the disease
Cerebral ischemia in a small child develops under the influence of internal and external factors. Several points can be distinguished from the first group:
- Bad habits, such as smoking and excessive drinking by the expectant mother.
- Infectious and viral diseases. They are especially dangerous in the first months of pregnancy, when the formation of the child’s internal organs and systems occurs.
- Hormonal imbalances.
- Age. Most often, hypoxia during pregnancy occurs in women giving birth under 18 and after 35 years.
- Toxicosis in the last months of pregnancy.
- Impaired blood flow in the placenta.
- Lack of amniotic fluid (oligohydramnios).
- Pregnancy with twins, triplets and more children.
- Post-term pregnancy or, conversely, premature birth.
- Umbilical cord entanglement in a baby.
- The fruit is too big.
Risk factors for hypoxic-ischemic encephalopathy
Mother's side
- Neurological diseases in the family and epilepsy in the mother
- Infertility treatment
- Endocrine diseases (for example, thyroid pathology)
Features of pregnancy
- Preeclampsia and eclampsia
- Pathology of the placenta
Features of childbirth
- Heavy bleeding during pregnancy and at the time of birth
- Gestational age at the time of delivery is less than 37 or more than 42 weeks
- Low birth weight
- Lack of qualified medical care
- Rapid labor (less than 2 hours)
- Fever at the time of delivery (more than 38 degrees)
- Emergency caesarean section
All of the above factors do not guarantee the occurrence of hypoxia in the newborn. They only reflect the degree of fetal health and danger at the time of birth. For example, bleeding, pathology of the placenta and low birth weight of the child are interrelated factors. They often lead to premature birth and emergency caesarean section (indications). The combination of such moments slightly increases the risk of brain damage in a baby, but only in a small percentage of cases.
- Approximately 70% of children with encephalopathy had developmental disorders and risk factors already during pregnancy.
- 25% of babies also had problems during childbirth.
- And only a small number of children with cerebral ischemia suffered after birth.
Treatment
Therapy for children with HIE is aimed at:
- providing optimal conditions for their further nursing;
- correction of disorders of the respiratory and cardiovascular systems; elimination of hemodynamic disorders;
- normalization of blood gas composition, elimination of electrolyte disturbances;
- preventing the development and eliminating existing seizures.
Further treatment is aimed at correcting developed complications and consequences. Can be assigned:
- exercise therapy courses, massage,
- drugs that normalize cerebral circulation (piracetam),
- vitamin therapy (group B),
- use of levocarnitine (Elcar).
Degrees of cerebral ischemia
Lightweight | Average | Heavy |
In premature infants, mild ischemia may be manifested not by increased, but by decreased reflexes and muscle tone. |
Recovery within the first two weeks indicates a favorable prognosis. |
|
Manifestations of ischemia in infants
Ischemia of brain structures is a disease that is accompanied in newborns by hypoxia (low oxygen content in tissues) or anoxia (lack of oxygen in tissues), which leads to acute oxygen starvation. In 40% of cases, central nervous system lesions in childhood are associated with perinatal pathology.
Prematurity is the leading factor associated with morphofunctional immaturity of brain structures, which increases the risk of cerebral ischemia in premature infants during premature birth. Due to oxygen starvation, necrosis (tissue death) develops, which leads to focal and diffuse structural changes in the brain matter. Depending on the location and nature of the damage, the following are distinguished:
- Multicystic leukomalacia (diffuse damage to the white matter of hypoxic, ischemic etiology).
- Subcortical (subcortical) leukomalacia.
- Ischemic necrosis (focal or diffuse).
Atrophic changes in brain structures are detected during instrumental diagnostics. When conducting an Echo-EG (echoencephalography) study, in 80% of cases, compactions are observed in the periventricular (near the ventricles) region, in 20% of cases the picture is complemented by the expansion of the ventricles and spaces in which the cerebrospinal fluid is located (ducts, subarachnoid space).
Often (about 18% of cases) ischemia that affects the brain in a child occurs without obvious abnormalities in the structure of the brain matter. An EEG study (electroencephalography) in premature infants in 73% of cases shows the inconsistent nature of the bioelectrical activity of the brain with a predominance of slow, low-amplitude waves, periodically alternating with short-term regular waves.
In 23% of children, various pathological patterns (sample patterns) of the EEG and waves of an epileptic nature in a general oscillatory rhythm are detected. Rarely (3% of cases) the EEG does not show significant deviations from the norm in children with ischemia occurring in the brain.
Signs of prolonged asphyxia and severe ischemia in newborns
- Low Apgar scores (0-3) after the first 5 minutes of life
- Coma, absence of tendon reflexes and muscle tone
- Disorders of internal organs (kidneys, lungs, liver, heart)
The degree of cerebral ischemia is determined by the doctor after examining the child; this figure should appear in the discharge diagnosis. Initial data on the baby’s condition are obtained immediately after birth using the Apgar scale:
| Sign | 0 points | 1 point | 2 points |
| Heart rate | Absent | Slow (less than 100 beats per minute) | More than 100 beats per minute |
| Attempts to breathe | Absence | Weak squeaking, insufficient ventilation of the lungs | Strong scream |
| Muscle tone | Muscles are relaxed | Limbs are slightly bent | Limbs bend well, movements are active |
| Vivacity of reflexes (to irritation of the foot) | None | Grimaces on the face | Scream |
| Color of the skin | Blue, pale | Pink body, bluish limbs | The whole baby is pink |
The baby's condition is recorded 1 and 5 minutes after birth. After 1 minute, the need for resuscitation is determined by the number of points. Scores at 5 minutes reflect to some extent hypoxic brain damage (if any).
Main signs of the disease
Signs of stage 1 ischemia:
- Restless behavior of the newborn.
- Lethargy.
- Restless sleep.
- Strong excitement.
- Weakening of reflexes.
Signs of grade 2 ischemia:
- Cramps.
- Fainting conditions.
- Frequent regurgitation of food.
- Paleness of the skin.
- Constant restless behavior of the baby.
Signs of grade 3 ischemia:
- Recurrent fainting.
- Severe cramps.
- Almost complete loss of hearing and vision.
- Vomit.
Cerebral ischemia in full-term and premature infants
The nature of brain damage due to asphyxia differs between children born at term and premature babies. The earlier a child is born, the greater the risk of periventricular leukomalacia (PVL). This term means necrosis of the white matter of the brain located near special cavities (ventricles). Cysts form in place of dead cells. It is PVL that is responsible for most cases of cerebral palsy and dementia in children born before 31 weeks of pregnancy.
In full-term infants, the cerebral cortex - the gray matter - is more often damaged. The health consequences will depend on the volume and location of damaged neurons. If the asphyxia was severe and acute, the brain stem, which is responsible for breathing and heartbeat, may be damaged. This poses a direct threat to the baby's life.
Symptoms of cerebral ischemia
Among the symptoms of childhood cerebral ischemia, the most striking and common are:
- increased excitability: the baby will constantly shudder, tremors of individual parts of the body will be observed, restless sleep, crying for no apparent reason;
- depression of the central nervous system: decreased muscle tone, low motor activity, weakened sucking and swallowing reflexes, facial asymmetry, strabismus;
- hydrocephalus: increased head size, increased intracranial pressure;
- coma: unconscious state, brain function to coordinate movements is absent;
- convulsions.
Thus, brain ischemia in a child manifests itself already in the first hours of his life. In the maternity hospital, they most often already assume that the baby has such a diagnosis, especially if pregnancy and childbirth were accompanied by pathologies and fetal hypoxia. However, all these signs can appear in newborns to varying degrees.
Consequences of oxygen deprivation of the brain
- Severe cerebral ischemia in 25-50% of cases ends in the death of the child in the first days of life, or a little later from pneumonia and other infections. Among surviving children, 80% have severe long-term consequences (dementia, cerebral palsy, autism), 10% suffer from moderate complications and 10% do not have significant consequences of asphyxia.
- Cerebral ischemia of grade 2 (moderate) causes severe long-term consequences in 30-50% of surviving children, and moderate complications in 10-20% (see increased intracranial pressure, frequent regurgitation in a newborn).
- Mild cerebral ischemia in newborns almost always ends safely, without significant consequences for the child (see hyperactivity in a child, malnutrition in a child).
Degrees of the disease
With ischemia in newborns, there are three degrees.
Mild ischemia - with this diagnosis the maximum percentage of survival (100%). In this case, hyperreactivity may be observed during the first week of life. If the disease was detected in a timely manner, then further threats to neurological diseases are excluded.
Symptoms:
- Tearfulness, sleep disturbance.
- Decreased appetite.
- Increased muscle tone.
Ischemia in newborns, grade 2 - according to statistics, 50% of children will experience depression of the central nervous system (CNS). In 10% of cases, complications such as increased intracranial pressure and convulsions are observed. Inpatient treatment is being carried out.
Symptoms:
- Sluggish infant reflexes.
- There are pauses in the respiratory process.
- Decreased muscle tone.
If there is an improvement in the condition in the first 2 weeks, then the prognosis is good. There is every reason to believe that the child will be able to cope with the disease with the right approach to treatment.
Severe degree - in 35-50% of cases, death occurs in the first week of life. If the child survives, then death from infectious diseases may occur in the future. In addition, he has cerebral palsy, autism, dementia, impaired development of hearing and vision. Treatment is carried out in intensive care conditions, and after that there is still a long rehabilitation. Most often, this degree of cerebral ischemia can occur in a prematurely born child.
Symptoms:
- Coma state
- The need for artificial ventilation due to the inability to breathe independently.
- Decline of muscle and tendon tone.
- Unstable blood pressure.
- Moro reflexes, sucking and grasping are not observed.
- Strabismus or unconscious movement of the eyeballs.
- Cramps.
Diagnostics
Typically, cerebral ischemia manifests itself in the first days after birth. Mild encephalopathy resolves fairly quickly, but severe encephalopathy may have a false “bright spot,” a few hours or days of improvement followed by a sharp deterioration. Therefore, a complete examination is necessary to make a diagnosis.
Examination of the baby
The examination includes an assessment on the Apgar scale, testing of all important reflexes (sucking, swallowing, grasping), measurement of body weight and height.
Analyzes
- general blood analysis
- blood electrolyte level
- blood clotting assessment
- amount of blood gases (oxygen, carbon dioxide)
MRI of the brain
For moderate and severe cerebral ischemia, magnetic resonance imaging of its structures is often used. With mild ischemia that resolves within 24 hours, there is rarely a need for MRI.
Ultrasound of the brain
Despite popular belief, ultrasound is not an accurate way to detect hypoxic encephalopathy. With its help, you can sometimes notice signs of cerebral edema and hemorrhage. But more often this research method gives a false positive result. Therefore, ultrasound is used for the initial diagnosis, with the need for additional examination.
EEG (electroencephalography)
This study is indispensable in children with severe cerebral ischemia. With its help, you can identify hidden seizures, assess the degree of brain damage and the integrity of its activity, and select the correct anticonvulsant therapy.
Preventive measures
Preventing the development of cerebral ischemia in a child is quite problematic. However, you can take a number of measures that will significantly reduce the chance of its occurrence:
Plan your pregnancy carefully. It is necessary to undergo an examination in advance and eliminate possible risks.
Even during the planning period and already during pregnancy, give up bad habits, such as smoking and excessive drinking.
Set aside time every day to do simple exercises.
Walk outdoors regularly.
Adjust your diet by adding more fresh fruits and vegetables to your menu.
Take care of your diet. If possible, eat at the same time every day.
If possible, protect yourself from stress and nervous overexcitation.
During the period of bearing a child, follow all doctor's orders. This is especially true for regular tests (blood, urine) and ultrasound.
If tests show a decrease in hemoglobin, take iron supplements.
And the most important preventive measure is to consult a doctor at the slightest discomfort.
Treatment of cerebral ischemia
There is no specific treatment that can restore brain cells damaged by ischemia. There are no pills, no IVs, no physical procedures that can replace dead areas with viable ones. But there are methods to prevent further hypoxia and help the child to rehabilitate.
Methods in the acute period of ischemia
Since moderate and severe ischemia usually manifests itself immediately and clearly, the Apgar scale can give a preliminary assessment of the condition. If within the first two minutes of life the baby does not begin to breathe on his own or with the help of an oxygen mask, then resuscitation measures begin:
- Intubation and artificial ventilation
With minor injuries, most children can be transferred to spontaneous breathing within 2-3 minutes after intubation. Such babies are handed over to the mother and are under close medical supervision. If longer resuscitation measures are required, the child is transferred to the intensive care unit, where respiratory parameters, blood circulation, blood gas levels, hemoglobin and glucose are actively monitored.
- Treatment of seizures
Anticonvulsant drugs (phenobarbital, phenytoin and others) in the correct dosage stop seizures and save the child from additional brain damage.
- Maintaining cardiac activity
Since the heart suffers along with the brain during hypoxia, it is sometimes necessary to maintain its function. Drugs such as dopamine and dobutamine keep the heart rate adequate.
- Hypothermia
In recent years, studies have been carried out related to a decrease in temperature by 3-4 degrees below normal. There is evidence that such hypothermia can preserve brain cells, preventing the spread of necrosis. It has been introduced into the standard treatment of encephalopathy since 2010. The main rule of hypothermia: specialist supervision and gradual warming.
Thus, there are no drugs yet that can cure hypoxic brain damage. You can only stop them and provide the child with support for all important functions until recovery.
Treatment of the consequences of cerebral ischemia in newborns
Moderate and severe encephalopathy often results in permanent brain changes. They can manifest themselves insignificantly (attention deficit disorder, for example) or lead to disability (cerebral palsy, mental retardation).
For any outcome of encephalopathy, the range of medications for treatment is very limited:
- If seizures persist, anticonvulsant therapy is administered
- In severe cerebral palsy with spasticity of the arms or legs, muscle relaxants are used
This is where the list of tablets ends. The only way to influence the development of a child with the consequences of severe ischemia is regular exercise.
- Cerebral palsy requires a special massage, which is best left to specialists. At least in the early stages.
- Physical therapy is necessary for older children
- Special devices for correcting incorrect postures. With spasticity, the baby's limbs often take an inadequate position, which worsens the prognosis in the future. Splints, bolsters, strollers, and special chairs provide a physiological position of the body in space.
- Classes with a speech therapist and home exercises for the development of speech, attention, perseverance
- Communication with children, adults and surrounding wildlife is an important stage in the rehabilitation of children after cerebral ischemia.
Treatment methods
Timely diagnosis of disorders and treatment will help to avoid serious consequences of cerebral ischemia in newborns. Complex neurorehabilitation includes:
- Drug therapy using drugs with neuroprotective effects.
- Massotherapy.
- Passive therapeutic exercises.
- Applications of ozokerite in the extremities.
- Dry immersion. Without the use of an aquatic environment, conditions of partial weightlessness are created, similar to those in which the fetus lives during intrauterine development. An effective rehabilitation measure that allows you to reduce neurological symptoms and stabilize some hemodynamic parameters.
- Physiotherapy (laser therapy, magnetic therapy).
- Music therapy.
Therapy with pharmaceutical agents is aimed at eliminating convulsive syndrome, eliminating the consequences of hypoxia and cerebral edema. Correction of psychomotor functions will be performed using drugs:
- Vitamins of group B1, B6.
- Medicines based on L-carnitine (Elkar, Levocarnitine). They normalize metabolic processes at the cellular level and have an antihypoxic effect.
- Neuroprotectors based on amino acids and neuropeptides (Actovegin). They improve the relationship between neurons, stimulate reparative (restorative) processes in the central nervous system.
- Angioprotectors. They improve the condition of vascular walls, increase the tone of smooth muscles, and prevent the penetration of calcium ions through cell membranes.
- Nootropic (Glycine, Phenotropil, Gliatilin). Increases the resistance of brain structures to hypoxia. Accelerate the utilization of glucose, stimulate the exchange of nucleic acids, accelerate the synthesis of proteins, ATP, RNA.
- Anticonvulsants.
- Muscle relaxants. Restores normal muscle tone.
For mild forms of pathology, it is recommended to do professional massage, therapeutic exercises, physiotherapeutic and water procedures, and rehabilitation treatment can be carried out without the use of any pharmaceuticals.
Overdiagnosis and ineffective therapy of ischemic encephalopathy
Pediatric neurology is one of the few areas of Russian medicine in which most doctors do not follow the latest recommendations for the diagnosis and treatment of PEDs. And if newborn babies with brain damage in our country are looked after very well, then the “consequences of PEP” are treated incorrectly and unreasonably.
- Newborn babies and children in the first 3-6 months of life have features that are mistaken for encephalopathy. For example, trembling, increased muscle tone, Graefe's symptom - all this is the norm for babies up to six months. Most pediatricians and neurologists, unfortunately, do not know about this.
- Examination of a frightened or sleepy baby is another reason for overdiagnosis of cerebral ischemia. In such cases, he may be overly excited or lethargic.
- Overdiagnosis usually results in the prescription of unnecessary medications. Such drugs do not help children with the real consequences of hypoxia, and they are not needed at all for healthy children.
A short list of unnecessary medications:
- Vascular drugs (Cavinton, cinnarizine, etc.) see drugs to improve cerebral circulation
- Actovegin, Cerebrolysin, Cortexin
- Nootropics: phenibut, piracetam, pantogam, picamilon
- All homeopathic medicines (see placebo effect)
- Herbal remedies (motherwort, valerian) see sedatives for children.
All of the above products do not have proven effectiveness and safety. At best, they will not help, at worst, they will cause various side effects.
Symptoms
The disease has characteristic symptoms.
The most common signs of the disease:
- weakened or increased muscle tone;
- impaired functioning of the nervous system - shuddering occurs at night, there are involuntary movements of the jaw and limbs;
- weakening of the sucking reflex;
- lethargy;
- decreased activity;
- inhibited state;
- asymmetry (the size on one side is not the same as the other) of facial muscles;
- curvature of the neck;
- convulsions;
- enlargement of the head due to cerebral edema.
The exact symptoms of cerebral ischemia in children depend on the severity of the disease.
Detailed information is shown in the table:
| Name of degree of cerebral ischemia | Characteristic symptoms |
| Light | With 1 degree of cerebral ischemia, the following symptoms are identified in children:
If the baby is premature, disorders in the nervous system may develop that last up to 7 days. Signs include lethargy, decreased muscle tone, and weakened reflexes. |
| Average | Stage 2 is characterized by the following symptoms:
|
| Heavy | With stage 3 disease, the following symptoms occur:
|
FAQ
At the age of 1 month, my son underwent a routine ultrasound of the brain. In conclusion it was written: “Consequences of perinatal encephalopathy, recovery period. Signs of increased intracranial pressure." The neurologist diagnosed the threat of cerebral palsy (as there is a slight tremor of the chin) and prescribed Pantogam. How serious is this diagnosis?
With a single complaint of chin tremor, your son's development is likely not of concern. Severe encephalopathy is usually visible already in the maternity hospital. An ultrasound of the brain without supporting symptoms cannot be the basis for a diagnosis. Pantogam is an ineffective and unsafe drug. Massage with mother's hands and encouragement of any physical activity is all that a healthy child needs.
Is the diagnosis of “Residual phenomena of perinatal encephalopathy” a reason to refuse vaccinations?
This diagnosis is incorrect, as it does not reflect the child’s condition. But even if cerebral ischemia was actually observed after birth, this is not a contraindication to vaccinations. Moreover, children with such a severe consequence of ischemia as cerebral palsy must be vaccinated.
Prognosis, complications
As stated above, timely treatment will prevent the development of serious complications. But in some cases, unpleasant consequences are possible:
- sleep problems;
- frequent headaches;
- irritability;
- isolation, reluctance to communicate with others;
- disturbances in the functioning of the musculoskeletal system or physical inactivity; slow mental development;
- high blood pressure;
- autism;
- cerebral paralysis;
- attention deficit disorder;
- slow mental development;
- Graefe's syndrome (bilateral paralysis of the extraocular muscles); death.
Despite the long list of consequences of ischemic brain damage, the prognosis for the disease is favorable. Thanks to properly selected treatment, symptoms disappear within a period of six months to a year.
Ischemia in newborns is quite common. Symptoms that are uncharacteristic of a healthy child, such as seizures, pale skin or hydrocephalus, are a cause for concern. If they appear, you should immediately consult a doctor.
Provoking factors
Concomitant factors that can lead to the development of ischemia can be grouped into three groups:
- The course of labor. The risk of pathology increases if:
- bleeding occurred during pregnancy or during labor;
- emergency caesarean section;
- high temperature in a woman in labor;
- premature birth;
- low baby weight;
- turbidity of amniotic fluid;
- premature placental abruption;
- rapid labor activity.
2. The mother's condition can cause the development of ischemia in the child, especially when:
- the expectant mother suffers from neurological problems;
- there are pathologies in the functioning of the endocrine system;
- pregnancy at a later age;
- the presence of chronic pathologies in the mother.
3. The course of pregnancy is also very important: if preeclampsia or eclampsia was observed, then there is every chance of developing a pathology such as grade 2 cerebral ischemia in the newborn. The consequences may vary.
These factors are not a 100% guarantee of the development of pathology. Even intrauterine disorders do not always end with cerebral ischemia developing after birth; the consequences can be eliminated if the pathology is detected in time and all measures are taken.