Today, the question of methods and treatment regimens for patients with an established diagnosis of deep vein thrombosis of the lower extremities is raised with particular urgency. This is due to the frequent development of the disease during active working age.
Of particular concern to doctors is the disability of a large part of patients after suffering from the disease and the subsequent development of post-thrombotic syndrome, progression of chronic venous insufficiency, and most importantly, the high threat of death of patients if acute pulmonary embolism occurs.
Causes of thrombosis and its signs
- If the integrity of the vascular wall is compromised, the development of thrombosis begins. This usually happens as a result of injuries, during pregnancy, when the vessels narrow and become deformed, or if the doctor’s recommendations are not followed after operations.
- When blood stagnation occurs - due to insufficient physical activity or prolonged bed rest. Venous congestion often leads to deep vein thrombosis and varicose veins. To reduce the risk of developing blood clots, it is recommended to use venotonic agents for varicose veins: for example, Normaven® Leg Cream. This product was developed by specialists from the pharmaceutical company VERTEX, has undergone clinical studies and has all the necessary documents and quality certificates confirming its effectiveness and safety. As a result of the testing, it was found that a three-month course of using Normaven® Leg Cream helps to improve the condition of the blood vessels of the lower extremities, due to which cramps disappear, the severity of the venous pattern decreases, swelling and a feeling of heaviness in the legs disappear.
- When the number of platelets and red blood cells in the blood increases, blood clotting parameters change. The cause may be hormonal imbalances, metabolic disorders and oral contraceptives.
- Thrombosis can develop in patients with cancer, as well as with kidney dysfunction.
Factors that increase the risk of thrombosis:
- injuries;
- obesity and excess weight;
Obesity and excess weight are factors in the development of thrombosis
- pregnancy and childbirth;
- smoking;
- infections;
- long-term and frequent trips and air flights;
- age from 40 years;
- taking medications that increase blood clotting;
- surgical intervention on joints and abdominal operations under anesthesia;
- bone fracture;
- sedentary lifestyle.
Therapy methods
To treat thrombosis of large arteries, the following are used:
- Medicines that help dilate blood vessels and relieve reflex spasms.
- Anticoagulants that reduce blood clotting.
- Novocaine blockades, and after them painkillers.
To get rid of oxygen deficiency, the patient is placed in special pressure chambers with pure oxygen under high pressure.
If during diagnosis a blockage of half the lumen of the vessel is detected, lytic medications are administered through a catheter connected to the site of thrombus formation. Surgery is resorted to when an acute course is detected or with the rapid development of gangrene. During this procedure, the clot is surgically removed.
The acute form of the pathology has three stages of development: ischemia, infarction, peritonitis. If the disease can be diagnosed in the first two stages, the patient can be helped to fully recover. If the diagnostic search is delayed, the stage of peritonitis becomes irreversible and the patient dies.
Signs of vein thrombosis in the legs: what precedes it
In healthy people, blood flows freely through arteries and veins.
Signs of thrombosis:
- The speed of blood flow in certain areas decreases. This may be due to heart failure, heart defects, varicose veins or atherosclerosis.
- Blood density increases
- The blood vessels narrow. The causes of this may be the following diseases: endocarditis, arteritis.
- Blood clotting factors are deficient, and blood clots worse.
The disease occurs in the veins; inflammation of the walls usually occurs, followed by venous thrombosis. Shock and severe bleeding provoke thrombus formation.
Thrombosis is a reaction to acute diseases. It is important that the nervous and endocrine systems have sufficient response to protect against the onset of any disease. Thrombosis poses a great threat to life in diseases of the brain and changes in hormonal levels.
Expert opinion
With arterial thrombosis, a fibrin film forms at the injured site, to which platelets with a negative electrical charge begin to flock. Blood clots become fixed to the walls. Then they begin to increase in size, collecting leukocytes, red blood cells and fibrin films.
Vascular surgeon, phlebologist
Osipova Ekaterina Yakovlevna
Blood clots can be:
- red (blood flows slowly, but clots well),
- white (blood flows quickly, clots slowly).
Layered blood clots that form over a long period of time are capable of splitting on their own. This phenomenon is referred to as revascularization (the throughput of the vessel is restored). It is possible to trace the signs and symptoms of thrombosis only if at least 10-50% of the vessel is affected.
First signs of thrombosis
The formation of blood clots is painful, with a feeling of heaviness and swelling.
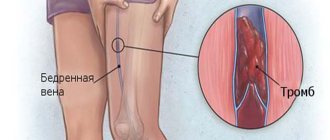
If the blood clot is located in the femoral or iliac vein, the entire leg swells and the skin takes on a blue tint. Due to altered blood flow, clots are redistributed into the veins under the skin. A vascular network appears, which is noticeable on the abdomen along the protruding veins. The patient indicates weakness, chills, and body temperature above normal.
When blood clots form in small veins, signs of thrombosis for various reasons may not be expressed for a long time. And only unpleasant sensations when walking will signal a problem.
Signs and features of thrombosis
Signs of thrombosis depending on the location of the thrombus
- The portal vein facilitates the flow of blood from unpaired organs in the abdominal cavity (from the stomach, intestines, spleen, pancreas). From them the blood is sent to the liver (where it is cleansed). If thrombosis occurs in the portal vein, the risk of liver disease increases.
Symptoms of portal vein thrombosis include abdominal pain and bloating, intestinal distress, vomiting, rarely black stools, and an enlarged spleen.
- The pulmonary artery becomes blocked after blood flows from the veins of the legs and pelvis. The number of clots, the reaction of the lungs to them and the action of the homeostasis system are important. The smaller the clot, the less severe the symptoms. Large blood clots interfere with gas exchange in the lungs, and hypoxia develops.
Symptoms: chest pain; the skin turns pale and blue; veins swell in the neck; a cough with bloody discharge and wheezing appears; loss of consciousness.
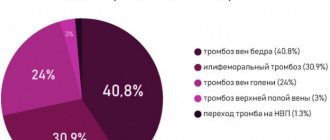
- Thrombosis of the lower extremities accounts for up to 70% of the total number of thromboses. It is especially dangerous when the deep veins in the thighs and below the knees are thrombosed (it is necessary to monitor for signs of lower leg thrombosis). The first symptoms are invisible.
Swelling, pain when walking or bending the lower leg, pain in the inner thigh and foot, reddened skin and cramps are all signs of the development of the disease. If the acute form occurs, the person begins to suffer from shortness of breath, his temperature rises, he becomes dizzy and loses consciousness. You can compare the signs of thrombosis of the lower extremities from the photo, but the diagnosis must be made by the attending physician.
- In the upper extremities, thrombosis is less common (subclavian vein thrombosis), and it is difficult to distinguish its initial symptoms from arm injury. They manifest themselves in swelling, pain and blueness. The patient feels a burning sensation, his hands go numb, and his skin becomes insensitive.
- The vessels of the brain connect with veins and arteries, where blood clots can also appear, and this leads to a stroke. Symptoms of cerebral thrombosis are more pronounced than with thrombosis of other vessels. The disease is accompanied by headaches, dizziness, decreased hearing and visual acuity, loss of consciousness, and periodic convulsions. The person is feeling sick.
- Blood clots also settle in the veins of hemorrhoids, this is considered a complication of hemorrhoids. Signs of thrombosis of hemorrhoids (Haemorrhoids): pain, the affected area itches, fever, swelling.
- The central retinal vein is also affected by thrombosis. Signs of the disease may not be expressed, and the person loses vision as a result.
- Thrombosis of the mesenteric veins of the intestine is manifested by prolonged abdominal pain. Other signs: bloating, high fever, vomiting and nausea. In the early stages, it is difficult to determine the disease by symptoms. Usually they talk about a complication of the pathology.
- If the femoral and iliac veins are affected, then we are talking about ileofemoral thrombosis. It is accompanied by swelling of the legs (the skin changes color from reddish to blue), when pressure is applied, brown marks appear, the legs and groin hurt, and the body temperature rises.
Treatment and diagnosis of venous thrombosis
Symptoms of chronic course
The clinical picture that develops when the lumen of the abdominal aorta is blocked depends on the degree of occlusion, the presence of collateral circulation, and the level of damage.
When a blood clot forms, a spasm of the artery walls occurs in parallel, which aggravates the situation. When the lumen of the vessel narrows by more than 10%, additional collateral blood flow begins to connect, which further complicates the diagnosis. It is also worth considering that if thrombosis of the inferior mesenteric artery occurs, then the upper one takes the entire load upon itself; in the opposite situation, this does not happen.
When there is difficulty in the blood supply to the kidneys, one of the most striking clinical symptoms is arterial hypertension, which is malignant.
When the abdominal aorta is damaged in the bifurcation area with transition to the iliac arteries, intermittent claudication syndrome occurs. It is expressed in the appearance of burning intense pain in the calves, back, buttocks (high intermittent claudication), and a feeling of fatigue. This symptom complex occurs after walking on a flat surface. Pain in the foot, numbness, coldness of the limb, and trophic disorders are noted.
Signs of thrombosis and treatment
The severity of the disease is indicated by signs of thrombosis; treatment is prescribed depending on the stage of the disease.
What to do? First of all, an accurate diagnosis is necessary. The doctor must determine where the blood clot is located, clarify its size and mobility. It is necessary to understand how firmly the blood clot is fixed and what is the likelihood that it will come off.
!
There are several main methods of therapy: surgery, thrombolysis, medication and implantation of a vena cava filter.
Heparin injections and anticoagulant drugs are also prescribed. Additionally, they can also prescribe a complex of venotonic vitamins and plant extracts, as well as prescribe a therapeutic diet.
Thrombolysis involves surgically dissolving blood clots using a catheter through which a substance is injected to dissolve the blood clot.
Surgical treatment of thrombosis
Doctors resort to surgical intervention only in case of complications, and here the location of the blood clot is important. It is possible to eliminate the entire thrombotic mass.
A vena cava filter is a metal device similar to an umbrella. It is implanted into the lumen of the inferior vena cava endovascularly.
Prevention
Most often, blood clots form in the summer. This is due to the fact that the body is dehydrated. Dehydration develops even more severely in women who want to lose weight (many diets are based on removing fluid from the body). Therefore, it is important to drink enough fluid. Your lifestyle should be active. Moderate physical activity improves blood circulation, metabolism, and prevents blood stagnation. It's important to eat right. The diet should be based on plant foods. It is advisable to consume a minimum of foods containing cholesterol. Blood clots tend to appear in connection with infectious diseases, operations, and injuries. Try to avoid these moments. The connection between smoking, atherosclerosis and thrombosis has been proven. If you smoke, then give up cigarettes. Visit your doctor regularly for routine examinations.
Originally posted 2014-01-09 00:56:29.
Recovery after thrombosis
Recanalization is the restoration of the capacity of an artery or vein after thrombosis. It can occur through medical intervention or naturally. Recanalization occurs no earlier than after 6 months with long-term treatment. It requires constant prevention.
After thrombosis, the clot in the vein goes away over time and normal blood flow is restored. Sometimes recanalization does not occur. Even after complete cleansing, the vein cannot function normally.
Thrombosis destroys its internal valves, and they are responsible for the outflow of blood in one direction. As a result, the outflow of blood from the limb is disrupted, the pressure in its venous system increases, and the disease develops again. Therefore, signs of recanalization of thrombosis may be short-lived.
Expert opinion
Unfortunately, thrombosis of the veins of the lower extremities has a tendency to recur even after the clot has resolved. Therefore, it is extremely important to make lifestyle changes and follow the preventive measures recommended by your doctor to reduce the risk of recurrent blood clots.
Vascular surgeon, phlebologist
Osipova Ekaterina Yakovlevna
Suspicion of thrombosis
To properly treat thrombosis, you need to make an accurate diagnosis. Different methods are used for this:
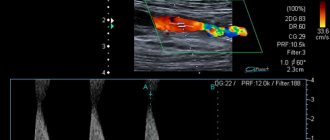
- Duplex scanning. With its help, visualization of blood vessels is created and blood flow is examined.
- X-ray contrast venography. In this case, a contrast agent is injected into the vessel.
- In case of doubt, MR-CT angiography is performed when making a diagnosis.
- If there is a risk of pulmonary thromboembolism, the patient undergoes a chest x-ray and scintigraphy.
- Impedance plethysmography is performed if there are signs of leg thrombosis. This method uses a cuff that compresses the lower leg for subsequent short-term occlusion of the veins. The new vessel volume after blood flow is then measured. This analysis provides an accurate diagnosis (up to 90%) and allows one to recognize the presence of deep venous thrombosis in the area above the knee.
At the first suspicion of thrombosis, you should immediately consult a doctor. Self-medication at home is very dangerous.
Symptoms of chronic course
The development of the clinical picture depends on the extent of the aortic lesion.
When its lumen is closed by only ten percent, the general blood supply system begins to support additional collateral blood flow. Therefore, there are no visible manifestations, which makes diagnosis difficult. The first symptoms appear when there is a long-term lack of blood supply. In this case, the intestines, kidneys and lower limbs suffer. Each form of pathology has its own symptoms. Intestinal ischemia manifests itself as follows:
- After a heavy meal, a sharp pain occurs in the stomach, which simultaneously radiates to the lower back, back of the head and left side of the chest. It goes away on its own two to three hours after eating.
- The patient suffers from tract dysfunction syndrome. Periodically, a feeling of heaviness and fullness occurs, mild nausea develops, diarrhea alternates with constipation, vomiting brings obvious relief. In this state, the patient consciously begins to refuse food, and therefore quickly loses weight.
- In the area of the duodenum, the formation of a secondary ulcer is possible.
- Against the background of these dysfunctions, asthenia develops. It is expressed in the form of weakness, decreased performance.
- Depression gradually sets in.
Renal ischemia is characterized by a persistent increase in blood pressure. The tonometer shows more than 140/90 mmHg. This condition is dangerous because it can cause a heart attack or stroke.
If the patient complains of burning pain in the calves, buttocks, lower back, numbness in the foot, coldness of the legs, and at the same time intermittent claudication occurs, partial closure of the lumen of the abdominal aorta in the area of transition to the iliac arteries can be suspected.
Video: how to recognize thrombosis?
is not responsible for the accuracy of the information presented in this video clip. Source - Phlebologist Ignatov V.N.
Sources:
- NEW APPROACHES TO ANTICOAGULANT THERAPY OF ACUTE DEEP VEIN THROMBOSIS OF THE LOWER LIMB. Sukovatykh B.S., Belikov L.N., Savchuk O.F., Chernyatina M.A. // Kursk scientific and practical bulletin “Man and his health”. – 2008. – No. 3. – pp. 74-78.
- STRUCTURE OF RISK FACTORS FOR ACUTE DEEP VEIN THROMBOSIS OF THE LOWER LIMB. Usov S.A., Rovenskikh D.N., Sartakov G.G. // Acta Biomedica Scientifica. – 2012. – No. 4 (86). – pp. 106-107.
- https://www.researchgate.net/publication/261258086_Scientific_Publications_on_Portal_Vein_Thrombosis…
- https://www.researchgate.net/publication/7711586_Ultrasound_criteria_for_embologenicity_of_venous_th…
- https://thrombosisjournal.biomedcentral.com/
- https://www.isth.org/page/JTH
For an accurate diagnosis, contact a specialist.