Pathologies of the cardiovascular system are diverse in nature, the number of independent units in the classifier reaches hundreds. They vary both in course and in origin, but many sooner or later lead to fatal consequences. Without treatment - these are the absolute majority.
A number of processes are not subject to any correction at all; only prolongation of life is possible. According to statistics, mortality from cardiac problems in the world is in first or second place in terms of the number of situations.
Hypertrophic cardiomyopathy is a congenital or acquired malformation of the heart, when the volume of the muscle layer of the left, less often the right, ventricle increases spontaneously.
The disease is controversial. Scientists still cannot come to a consensus regarding the genesis of the condition.
Some point to a purely genetic nature (that is, the phenomenon is associated only with a family factor), while others speak of a high probability of sporadic moments (possibly spontaneous, secondary development).
The truth is somewhere in the middle. In any case, the disease without proper treatment in the early stages carries enormous danger.
The mechanism of pathology development
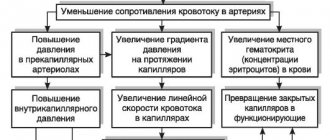
The genesis of the condition is based on two opposing processes.
The first is the so-called myocardial weakness. It causes insufficient contractility of cardiac structures during systole, as well as a small volume of incoming blood at the moment of complete relaxation of the organ.
Hence the disruption of the normal supply of oxygen and essential substances to tissues. In the early stages, this is a subtle process; as ischemia intensifies, organic abnormalities increase.
The body, trying to compensate for functional failure, increases the volume of muscle tissue. But this is useless, since significant heart volumes do not equal adequate activity.
On the contrary, even greater relaxation of the myocardium occurs, since the conduction of the His bundles is disrupted. As a result, the patient has a significant proliferation of organ tissue, its pathological increase with a drop in hemodynamic potential.
Over the course of several years, the neglected variant leads to death from cardiac arrest. Resuscitation measures do not make sense, since the anatomical defect is too pronounced.
The second clinical variant of cardiomyopathy is hypertrophy of the interventricular septum. It occurs against the background of mitral valve stenosis, prolapse or fusion as a result of primary pathological processes.
As a result, the amount of blood that is transported through the chambers of the organ again decreases. The further development scheme is identical.
In rare cases, for example, against the background of congenital genetic syndromes or phenotypic abnormalities during the prenatal period, a combined process occurs. When both mechanisms work at once. This is potentially more dangerous and more difficult to eliminate.
The prospects for the development of lethal complications with isolated defects of the first or second type range from 5 to 20 years, and even longer with treatment.
If two defects are present at once (relatively speaking), the terms are reduced to 2-5 years, even medical care does not guarantee stabilization of the condition.
Therefore, it is necessary to undergo preventive examinations every six months to a year; if there is a history of pathologies of cardiac structures, even more often.
Symptoms and treatment of hypertensive cardiomyopathy
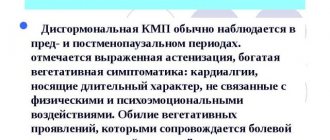
A rare heart disease is hypertensive cardiomyopathy. The disease is caused by pathological changes in the heart muscle and myocardial walls with increased pressure in the blood vessels.
The disease is congenital or acquired. The occurrence of hypertensive cardiomyopathy threatens a person with the development of heart failure, cardiac arrhythmia and sudden death.
Mechanism and causes of occurrence
The main cause of hypertensive cardiomyopathy is hypertension. Regular increase in blood pressure to 140/90 mmHg. Art.
and more leads to structural changes in the myocardium and promotes thickening of the heart walls. With increased pressure in the blood vessels, the thickened walls of the ventricles of the heart lose their elasticity and do not allow enough blood to pass through.
This process promotes oxygen starvation of myocardial cells and tissues.
The disease affects 0.2% of the population and is observed predominantly in men.
When the heart muscle thickens and the cavity of the chambers of the left (rarely right) ventricle does not expand, blood circulation is disrupted and hypertrophic cardiomyopathy develops. A characteristic sign of hypertrophic cardiomyopathy is hypertrophy of the interventricular septum, which leads to various myocardial diseases and poses a direct threat to human life.
Types of hypertensive cardiomyopathy are caused by:
- segment of heart enlargement;
- symmetry of lesions;
- the level of narrowing of the area between the interventricular septum and the anterior leaflet of the mitral valve.
The occurrence of the disease is provoked by the following factors:
- heredity;
- psychological stress;
- chronic kidney disease;
- smoking;
- age over 55-60 years;
- hormonal imbalance of the body.
Main symptoms
Tachycardia may be a symptom of pathology.
The disease is characterized by a slow increase in symptoms and characteristic signs. Relapses of the disease predominate in older people or develop as complications of other chronic diseases. The main symptoms of hypertensive cardiomyopathy are:
- loss of performance;
- severe pain in the chest area;
- tachycardia;
- dyspnea;
- dizziness, disorientation;
- fainting;
- sudden cardiovascular failure with threat of death.
Diagnostic methods for hypertensive cardiomyopathy
The main methods for diagnosing hypertensive cardiomyopathy are presented in the table:
MethodWhat shows
| Visual inspection and listening | The presence of a systolic murmur during auscultation confirms the presence of cardiovascular disease |
| Ultrasound of the heart | Thickening of the walls, valves and shape of the left ventricle is examined, pathologies in the cardiovascular system and features of the functioning of the heart muscle are determined. |
| ECG | Carry out a graphic recording of the work of the heart and the pulsation of the heart muscle |
| Chest X-ray | A detailed description of anomalies in the myocardium is given. |
| Holter monitoring | Using a special device - a Holter, the dynamics of the myocardium are continuously recorded on the ECG |
| Polycardiography | The contractile function of the heart is assessed |
| Rhythmocardiography | Graphically displays 200 or more cardiac cycles following each other |
Medical therapy
For hypertensive cardiomyopathy, drug therapy is used. The main drugs and their effect on the body are presented in the table:
NameTherapeutic effect
| Normalizes heart rate, reduces blood pressure |
| Affects the blood clotting process |
| Have an arthrythmic effect |
| Reduce blood pressure |
| Rids the body of excess salt and water |
For the treatment of hypertensive cardiomyopathy, medications and their dosage are taken strictly as prescribed by the doctor.
Schematic representation of mitral replacement.
For irreversible pathological changes in the myocardium, surgical intervention is used. Cardiac surgery treatment includes:
- septal myectomy - removal of part of the interventricular septum;
- mitral valve replacement;
- implantation of a pacemaker or cardioverter-defibrillator.
Preventive measures and prognosis
The main goal of preventive measures is to reduce the physical and emotional stress on the human body. Recommended:
- give up alcohol and cigarettes;
- balance nutrition;
- take daily walks;
- monitor blood glucose levels;
- avoid excess weight;
- forget about nervous worries and stress;
- visit a cardiologist once a year;
- check blood pressure.
The favorable prognosis depends on the stage of hypertensive cardiomyopathy and the main manifestations of the disease. With timely and effective treatment, complete recovery is possible. The postoperative prognosis depends on rehabilitation measures and compliance with all recommended preventive measures.
Source: https://EtoDavlenie.ru/serdce/gipertonicheskaya-kardiomiopatiya.html
Classification
The distinction between hypertrophic cardiomyopathy (HCM for short) is made on several grounds. The disease has its own ICD-10 code: I42.2, but the code does not reflect the entirety of the process.
Based on the prevalence of the phenomenon, there are:
- Left ventricular damage. Potentially fatal condition. Because the normal movement of blood in a large circle is disrupted. This means that over time the phenomena of hypoxia of all tissues increase. Signs from the brain, liver, and kidneys are especially pronounced.
- Enlargement of the right ventricle. Considered relatively less dangerous. As it develops, the clinical picture manifests itself as respiratory failure and general lung problems. The small circle suffers.
- Bilateral deviation. It incorporates typical signs of one and the other, significantly worsening the prognosis.
Depending on the volume of circulating blood they are called:
- A type with outflow tract obstruction.
- The type without one.
This classification has clinical significance only for doctors. In the first situation, the amount of liquid connective tissue released during systole decreases due to the narrowing of cardiac structures.
Left ventricular hypertrophic cardiomyopathy itself has two main forms:
- Symmetrical. When the lesion affects all departments equally. It occurs in approximately 25% of cases and is considered a less common variety. It makes itself felt by severe deviations in the functioning of cardiac structures. The likelihood of successful treatment decreases.
- Asymmetrical. When the myocardium is affected in separate areas or in several, but unevenly.
Finally, depending on the nature of the pathological process, the degree of deviation from the norm can be called:
- Mild hypertrophic cardiomyopathy. When the muscle is thickened to a size of 15-20 mm.
- Average. It is characterized by the growth of an anatomical formation up to 25 mm.
- Heavy. More than the specified value.
Accordingly, similar types proceed differently. The larger the heart, the worse it contracts, pumps blood, and supplies itself. In addition, the likelihood of a sudden stop increases.
These classifications play a large role in determining diagnostic and therapeutic tactics at any stage. The prognosis is favorable only in the early stages and not in all cases.
Who is guilty
"Family hypertrophic cardiomyopathy"
For what reason does a disease such as HCM develop? Who is to blame - the patient leading an unhealthy lifestyle, or the doctor who incorrectly prescribed treatment for arterial hypertension? Scientific research confirms the hereditary nature of hypertrophic cardiomyopathy. Moreover, the term “familial hypertrophic cardiomyopathy” is firmly rooted in the scientific literature. Scientists have proven that more than half of the detected cases of hypertrophic cardiomyopathy are hereditary diseases.
That is, the patient’s relatives suffered from this disease. The rest of the cases are sporadic (without a hereditary factor). The incidence of the disease depending on the age of patients differs significantly in different regions. Men get sick more often than women. A disease such as HCM can occur in childhood, youth, and old age. However, it is most often detected in young patients.
Causes
Development factors can be divided into two groups. The first concerns innate aspects.
A large category of scientists and cardiologist practitioners point to a predominantly genetic etiology of the process. Whether this is true or not is difficult to say. But the hereditary factor is of great clinical importance.
It has been proven that if there was a person in the family who suffered from the condition in question, the risk of manifestation in the descendant increases by 25-30%.
Disturbance of the normal genotype also plays a role. The pattern of inheritance is autosomal dominant. That is, it is enough that the damaged area is present in at least one parent, which causes a significant prevalence of the process.
Another group of scientists and practitioners speaks of predominantly acquired causes of the pathological phenomenon, and the fact of the presence of a similar condition in newborns is explained by a violation of the intrauterine development of the fetus.
Apparently, both occur in different clinical cases. It is also known that hypertrophic cardiomyopathy is not a purely genetic disease. It may be caused by third-party deviations.
Among which:
- Inflammatory processes in the heart. Myocarditis, damage to the muscle layer, is especially common. Occurs against the background of infections and autoimmune phenomena. Accompanied by prolonged chest pain, shortness of breath and increased rhythm. She is being treated in a hospital with the use of antibiotics. The risk of developing a defect against the background of inflammation is high. This is largely due to scarring of the cardiac structures. Mass gain is a compensatory mechanism that is initially flawed.
- Congenital and acquired heart defects. It is not known exactly whether they can directly determine hypertrophic type cardiomyopathy. But often this condition occurs in patients with other abnormalities of anatomical development. Research in this area is ongoing, but specific conclusions are not yet sufficient for a general understanding of the problem.
- Rheumatism. Systemic autoimmune disease with a relapsing course. It has a destructive-inflammatory nature. Treatment is long-term, sometimes lifelong. The quality of recovery depends on the moment of initiation of therapy and the characteristics of the patient’s body. It will take more than one year for cardiomyopathy to form.
- Mitral valve stenosis. Also prolapse and other options. The only defects that have been proven to influence the possibility of developing hypertrophic type cardiomyopathy. It is characterized by regurgitation (backflow of blood into the atria), hemodynamic disturbances, sometimes fatal. Against the background of a long sluggish course of the defect, parallel formation of other defects occurs.
- History of heart attack. Acute violation of the trophism of the muscle layer. The result is a sharp drop in contractility and hemodynamics. Without timely assistance, the death of the patient is inevitable. Even with successful treatment, areas of functional tissue replacement with scar tissue are formed. They are not able to contract and act as fillers of disturbed space. Hence the need to increase the volume of the myocardium; this is also a compensatory mechanism.
- Inflammation of the pericardial sac. A relatively rare condition (3-5% of cases of all primary pathologies of this kind). It has an infectious, less often immune origin. It is characterized by a rapid aggressive course, expressed by the clinic. It is often complicated by inflammation of the myocardium (it is difficult to say exactly whether the first causes the second or vice versa). Treatment in a hospital under the supervision of a doctor. Chest injuries with damage to cardiac structures.
Causes of the disease
Heredity
Thanks to the fact that science does not stand still, data on such a disease as hypertrophic cardiomyopathy has expanded significantly. HCM is a hereditary disease that has an autosomal dominant pattern of inheritance. This means that if at least one of the parents is a carrier of the “defective” gene, then the child can develop the disease with a probability of 50 percent. At the moment, it is generally accepted that the development of hypertrophic cardiomyopathy is based on mutations in 10 specific genes.
Each of these genes determines the development of hypertrophic cardiomyopathy. For the disease to occur, a mutation in one of 10 genes is sufficient. Many mutations can occur in one gene responsible for the development of HCM. The most significant and common mutations are mutations of the β-myosin heavy chain, protein C, and troponin T. With HCM, uneven hypertrophy of the interventricular septum occurs, and the ability to contract and relax the left ventricle is impaired. The hypertrophied interventricular septum has a worse blood supply.
Risk factors
The so-called risk factors are also of great importance. They predispose to the formation of dangerous conditions. Among them:
- Physical inactivity. Or insufficient physical activity of the patient. Due to everyday life, professional activities, prolonged stay in bed.
- Smoking. Long lasting. Patients with a significant history of consuming tobacco products are especially at risk.
- Obesity. It is not dangerous in itself. All overweight patients have problems with metabolism and lipid metabolism.
- Excessive physical activity. Myocardial hypertrophy of the so-called natural type is formed. It can be called such with a great degree of convention. The patient does not really experience discomfort, but at a certain point the anatomical changes necessary to ensure the level of mechanical activity will turn against the person.
- Alcoholism.
- Consumption of narcotic substances.
- Long-term use of drugs that affect the heart and blood vessels.
- History of arterial hypertension.
- Ischemic disease.
Typical symptoms
Signs of the pathological process in the early stages are completely absent. As it progresses, the following manifestations occur:
- Dyspnea. First, during intense physical activity. Since few people provide themselves with this level of activity, there is no manifestation. Later at rest. The patient cannot climb the stairs, then walk down the street, and then even get out of bed. Detection of deviations is possible using special tests (bicycle ergometry as a gentle option).
- Chest pain. Unreliable diagnostic sign. May be of extracardiac origin. They flow in paroxysms and develop spontaneously. Especially against the background of stress, activity, consumption of alcohol, tobacco, and drugs.
- Drowsiness, weakness, feeling of body weakness, decreased performance.
- Increased sweating at night.
- Cyanosis of the nasolabial triangle.
- Headache.
- Vertigo. Both signs are noted in the later stages, when hemodynamics decline.
- Nausea, vomiting (rare).
- Paleness of the skin.
- Severe arrhythmias such as tachycardia, bradycardia, extrasystole or fibrillation. They occur in attacks or on an ongoing basis.
Symptoms are nonspecific. It is impossible to determine pathology from them. If you detect at least one of the described phenomena, you should contact a doctor.
Indications for hospitalization
The list of these is relatively wide. No special clinical recommendations have been developed. Based on the experience of the attending physicians, we can talk about the following points:
- Decrease in heart rate to 60 beats per minute or less. Critical conditions require calling an ambulance to resolve the issue of transportation to a specialized hospital.
- Tachycardia at a level of over 120 beats, provided that it lasts more than 2 hours in a row.
- Severe degree of hypertrophic cardiomyopathy (average according to the above classification and below).
- Arrhythmia of another type (extrasystole, fibrillation). Subjectively, it is felt as a sharp jolt in the chest, heart inversions, irregular, uneven beating.
- Intense pain syndrome. Until the reason is found out.
- Severe shortness of breath, up to the inability to perform simple household duties.
- Neurological deficit disorders (speech, visual, auditory, other dysfunctions).
In any controversial case, if you have any suspicions, you should contact a doctor. Also call an ambulance. Resolving the issue of hospitalization is the prerogative of qualified personnel.
What needs to be examined?
Diagnosis is carried out by cardiology specialists. Primary measures are aimed at determining the probable disease. Only then is verification and clarification of the version shown.
The full list of events is as follows:
- Oral questioning of the patient about his complaints.
- Collection of anamnestic data.
- Measurement of blood pressure and heart rate.
- Daily monitoring using an automatic programmable tonometer.
- Electrocardiography to assess the functional activity of the heart muscle and detect arrhythmia.
- Echocardiography. The main method in diagnosis. It is most often used at the first moment. Allows visualization of tissue, although significant qualifications are required from medical personnel.
- General and biochemical blood test.
- Scintigraphy according to indications.
- MRI. Used in extreme cases as a way to display cardiac structures in detail. It is considered a relatively expensive and inaccessible method, at least in reality in the CIS countries.
The main activities are aimed at establishing a diagnosis, its verification and determining the cause of the problem.
Diagnosis of the disease
Auscultation of the heart
For a long time, patients may have no complaints, look physically strong, and have an athletic build. When collecting complaints, it is important to collect anamnesis. A major role in the diagnosis is played by the fact of sudden cardiac death in relatives, especially at a young age, who had hypertrophy or a specific diagnosis of HCM.
- Examination and physical examination. When examining patients with a non-obstructive form of HCM, changes in the cardiovascular system may be absent. The most obvious signs are obstructive hypertrophic cardiomyopathy. When examining the cardiovascular system, it is possible to detect a displacement of the apical impulse to the left, while it is high and diffuse. The pulse is increased. Auscultation of the heart may reveal a systolic murmur.
- Laboratory tests only allow us to exclude other possible diseases of the cardiovascular system that lead to hypertrophy.
Electrocardiographic study - Electrocardiographic study (ECG). ECG signs of HCM are changes in the T wave and Q wave. When assessing the ECG, signs of overload or hypertrophy of the left ventricle can be identified. The T waves are negative in the chest leads, and atypical Q waves are found in II, III, AVF. In addition to changes in the waves, various disturbances of the rhythm and conduction of the heart occur.
- Holter ECG monitoring is carried out to identify disturbances in heart rhythm and conduction, as well as to assess the prognosis of the disease.
- A chest x-ray (CHX) shows enlargement of the ventricle and atrium, but in some cases the heart shadow may be normal.
- Echocardiographic examination (ultrasound of the heart) is the most informative method for diagnosing a disease such as HCM. By carrying out this study, it is possible to identify asymmetric or symmetric (less commonly) hypertrophy, obstruction of the outflow tract of the ventricle, changes in the functioning of the valve apparatus in systole and diastole, and evaluate the contractile and diastolic function of the ventricles of the heart.
Magnetic resonance imaging - Magnetic resonance imaging is a method that allows us to assess the condition of the myocardium and identify pathological flows in the heart with greater accuracy than echocardiography. However, due to its less availability, this method is used before surgery.
- Corona angiography is also used in the diagnosis of HCM. The main indication for its use is the presence of constant chest pain.
- Genetic research. The genetic screening method is indicated for patients with a questionable diagnosis in the presence of a hereditary predisposition. Identification of gene mutations makes it possible to verify the diagnosis in favor of hypertrophic cardiomyopathy.
Treatment
Treatment for hypertrophic cardiomyopathy involves addressing the symptoms and the underlying cause of the condition. Therapy is systematic, prescribed at the moment of detection of the pathological process. Has two planes.
The first is etiotropic influence. Possibly due to the acquired nature of cardiomyopathy. In the case of genetic defects, it makes no sense.
The second is symptomatic. Relieving symptoms and improving quality of life. Conservative and surgical techniques are used.
Among the first, the following drugs are used:
- Antihypertensive. The classic regimen is Diltiazem or Verapamil, Perindopril and Moxonidine in combination.
- Antiarrhythmic. Hindin, Amiodarone.
- Cardioprotectors.
- Products based on potassium and magnesium (Asparkam and others).
Glycosides are contraindicated. Other types are possible at the discretion of the physician.
Surgical treatment is indicated in extreme cases. Basically, this is a measure to combat the acquired process.
The methods are different. Thus, hypertrophic obstructive cardiomyopathy is eliminated by aortic valve replacement or stenting. It is possible to install a pacemaker, restore the anatomical integrity of an organ, etc. There are a lot of options.
The use of folk recipes does not make sense. Lifestyle changes are required (see prevention).
Treatment methods for hypertrophic cardiomyopathy
Therapeutic measures can only achieve temporary stabilization of the patient’s condition and are symptomatic in nature.
The main goals of treatment in this case are:
- improvement of left ventricular diastolic function;
- relief of rhythm disturbances;
- decrease in pressure gradient;
- relief of angiotic attacks.
Conservative therapy
Drug treatment of pathology involves the use of the following medications:
- Beta blockers. Drugs of this pharmacological group stabilize the heart rhythm, reduce myocardial contractility, and normalize vascular tone. Beta blockers relax the heart muscle while the left ventricle fills with blood. Modern drugs of this group, which are usually prescribed for the pathology in question, are Celipres, Obzidan, Carvedilol, Enalapril-Farmak, Amiodarone.
- Antiarrhythmic drugs. Disopyramide is usually used. The drug reduces the pressure gradient and eliminates the symptoms of the pathology: shortness of breath, chest pain. This medication also increases tolerance to physical activity.
- Calcium antagonists. Drugs in this group reduce the concentration of calcium in the systemic coronary arteries. With their help, it is possible to achieve improved diastolic relaxation of the left ventricle and a decrease in myocardial contractility. Calcium antagonists also have a pronounced antiarrhythmic and antianginal effect. For the treatment of pathology, Finoptin, Cardil, Amiodarone are recommended.
- Diuretics (Lasix, Furosemide). They are prescribed for the development of congestive heart failure.
In case of hypertrophic cardiomyopathy, taking medications belonging to the groups of cardiac glycosides, nitrites, and nifedipine is contraindicated. This limitation is due to the fact that these medications increase obstruction.
Surgery
In addition to taking medications, surgical methods may be used to treat patients with hypertrophic cardiomyopathy. This is the only way to save the life of a patient with a severe form of pathology.
Surgery involves removing hypertrophied muscle tissue in the interatrial septum.
The main methods of surgical treatment in this case include:
- Myotomy is the removal of the inner region of the interventricular septum.
- Ethanol ablation. The method involves making a puncture in the septum, into which a concentrated solution of medical alcohol is then injected. The amount of substance administered is from 1 to 4 mg. Such manipulation causes a heart attack in the patient. Thus, the septum becomes thinner. The event is carried out under ultrasound control.
- Implantation of a three-chamber electrical stimulator. The device stimulates intracardiac circulation and prevents the development of complications.
- Implantation of a cardioverter-defibrillator. The essence of the procedure is that a device connected to the heart using electrodes is implanted into the abdominal or chest muscle. This allows you to record the heart rhythm and restore it in case of failure.
The choice of methodology is carried out on an individual basis.
Lifestyle correction
Patients with hypertrophic cardiomyopathy are advised to limit physical activity and follow a low-salt diet.
Prognosis and possible complications
Determining outcome early in patient management is difficult. One thing is worth saying. The initial stages of the pathological process are relatively favorable, since the survival rate is 85-90%.
As it progresses, the numbers become more and more pessimistic. In any case, a complete cure is impossible. The defect will still remain to some extent.
But, with minimal deviations, stabilization of the condition and an increase in life expectancy are likely. To what extent is difficult to say. Usually no less than the average person.
Complications develop at any stage, but the risks are higher when the process is advanced.
Among the consequences:
- Heart failure.
- Cardiogenic shock.
- Hypertensive crisis.
- Stroke.
- Heart attack.
- Multiple organ failure.
- Vascular dementia.
The quality of life also decreases significantly. All of these complications sooner or later lead to the death of the patient.
Prevention is possible, but it takes effort. Both for the patient himself and for his doctor.
Prevention
Both during the treatment of hypertrophic cardiomyopathy and as part of its prevention, special actions are indicated.
Preventive measures present certain difficulties. First of all, in field terms. It is difficult to change your way of thinking and habits. But health requires it.
Among the recommendations:
- Complete cessation of smoking, alcohol, and drugs.
- Normalization of physical activity. No overload, but physical inactivity is also unacceptable. About an hour or two of walking a day, exercise therapy, swimming, that’s enough.
- Drinking regime. 1.5-2 liters per day. If there is arterial hypertension, use the lower limit.
- Salt is within reason (7 grams is enough). There should be no radical exclusion from the diet.
- Reconsidering your approach to nutrition. More vitamins, protein, less carbohydrates, fats, no fried, smoked foods, fast food, semi-finished products, canned food. Recommended treatment table is No. 10.
- Adequate sleep of at least 8 hours.
- Avoid stress whenever possible.
- Constant monitoring of blood pressure and heart rate.
It is also worthwhile to promptly treat all identified diseases, regardless of type. At a certain moment, they may manifest themselves in unexpected ways. Visiting a cardiologist every six months to a year is a good practice.
Causes of hypertrophic cardiomyopathy
Signs of hypertrophic cardiomyopathy are considered a hereditary disease. Hypertrophic cardiomyopathy occurs as a result of mutations in one of the four genes encoding cardiac proteins (/3-myosin heavy chains, the gene is localized on chromosome 14; cardiac troponin T, the gene is localized on chromosome 1; a-tropomyosin, the gene is located on chromosome 15; myosin-binding protein C, the gene is located on chromosome 11).
Hypertrophic cardiomyopathy often runs in families. At least 6 genetic loci have been identified that are responsible for the occurrence of the disease and the need for treatment of hypertrophic cardiomyopathy. The causes of hypertrophic cardiomyopathy can be various mutations in one of the five genes encoding the synthesis of cardiac sarcomere proteins (troponin T, troponin I, α-tropomyosin, /3-myosin and myosin-binding protein C). About 70 mutations have been found in these genes that cause hypertrophic cardiomyopathy. The survival rate of patients with hypertrophic cardiomyopathy, resulting from a particularly clinically malignant mutation of the /3-myosin heavy chain gene, is significantly lower than with a mutation of the cardiac troponin T gene, and in the latter case, clinical manifestations occur at a later age.
Classification of hypertrophic cardiomyopathy
There are obstructive (narrowing the outflow tract of the left ventricle) and non-obstructive hypertrophic cardiomyopathies. Hypertrophy can be symmetrical (enlargement involving all walls of the left ventricle) and asymmetrical (enlargement involving one of the walls). Hypertrophy can cover only the apex of the heart in isolation (symptoms - apical hypertrophic cardiomyopathy). When there is hypertrophy of the upper part of the interventricular septum directly under the fibrous ring of the aortic valve, they speak of subaortic stenosis.
Important general signs of hypertrophic cardiomyopathy (both with and without obstruction) are a high frequency of cardiac arrhythmias, primarily ventricular extrasystole and paroxysmal tachycardia, and impaired diastolic filling of the left ventricle, which can lead to signs of heart failure. Arrhythmias are associated with sudden death, which occurs in 50% of patients with untreated hypertrophic cardiomyopathy.