HYPEREMIA
HYPEREMIA
(
hyperaemia
; Greek, hyper- + haima blood) - an increase in blood supply in any part of the peripheral vascular system (small arteries, capillaries and veins), caused by an increase in blood flow into the microcirculatory system (arterial G.) or a weakening of blood outflow (venous G. .).
The biophysical mechanisms of hyperemia are determined by the basic laws of hemodynamics (see).
In the G. area, intravascular pressure is increased. Its level is determined according to the Bernoulli equation by the amount of energy consumption in the vessels, which depends on changes in the vascular lumen, blood flow speed, etc. In arterial hypertension, the increase in blood pressure in the microvessels is due to a decrease in resistance in the dilated arteries, and in venous hypertension, a slowdown in blood flow in peripheral vascular system.
The diameter of the vessels is determined by the ratio of two oppositely directed forces - intravascular pressure (P), which tends to expand them, and the tension (tone) of the vessel wall (F), which narrows them. Under conditions of constant radius (r), this relationship is as follows: F - Рr (Laplace equation).
In G., vasodilation depends on an increase in P and a decrease in F (in arterial G., on neurohumoral effects on the arteries and capillaries, and in venous G., on an increase in the extensibility of the connective tissue surrounding the capillaries and veins). The dilation of blood vessels that has begun continues until the above equality is established again, otherwise a rupture of the vascular wall will inevitably occur.
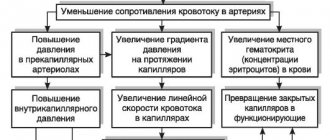
The linear speed of blood flow in the microcirculatory system depends on the arteriovenous pressure difference. It increases with arterial G. due to increased pressure in the arterial part of the capillaries and decreases with venous G. as a result of a significant increase in pressure in the veins. In each vascular region, according to the law of continuity, the cross-sectional area of the vascular bed (S), volumetric (Q) and linear (v) velocities are related by the expression: Q = Sv. In arterial hypertension, the Q value increases, which is due to an increase in v and S (due to an increase in the number and partly the diameter of functioning capillaries). With venous G., the Q value falls due to a sharp decrease in v, overriding the increase in S.
Arterial hyperemia (syn. active G.) can occur in normal and patol conditions. In a healthy body, it can be a manifestation of the regulation of adequate, i.e., corresponding to metabolic needs, blood supply to the tissue, when, due to increased functioning of the organ and metabolism, the intensity of microcirculation (see) increases (functional, or working, hyperemia).
Under pathological conditions, arterial G. can be a manifestation of compensatory regulation of blood circulation in certain disorders: a) following temporary ischemia (see), when the tissue experiences a significant deficiency of blood supply (post-ischemic, or reactive, G.); a special case of it is the so-called. post-compression G., which occurs after temporary compression of the vessels of an organ or tissue; b) around the ischemic focus, arterial G. promotes collateral blood flow (collateral G.); c) in the focus of inflammation (see), arterial blood compensates for changes in microcirculation that occur as a result of a sharp expansion and increase in the number of functioning capillaries, as well as an increase in blood viscosity due to increased intravascular aggregation of erythrocytes.
Arterial G.
may be a purely patol phenomenon and arise as a result of disorders of vasomotor regulation of local blood circulation: a) with erythromelalgia (see), the skin of the extremities turns sharply red, its temperature rises, severe pain appears caused by stretching of blood vessels; b) with angioedema of Quincke, when, along with arterial G., the permeability of the vascular walls sharply increases and edema appears (see Quincke's edema); c) with migraine (see) - headache is accompanied by increased pulsation of blood vessels and an increase in blood supply to the vessels of the face, etc.
Local dilation of the arteries is caused by vasomotor nerve impulses or humoral factors. The latter can be specific physiologically active substances circulating in the blood or formed in the vascular wall or surrounding tissues (eg, acetylcholine, histamine, bradykinin), or metabolic products that accumulate in arterial walls or diffuse from surrounding tissues. The dilation of arteries (especially skin ones) may also depend on the direct action of heat.
With arterial hypertension in the microcirculatory system, the speed of blood flow increases, the lumen of the arterial sections of the capillaries and the number of functioning capillaries increase; this helps to increase the volumetric velocity of blood flow. An increase in intracapillary blood pressure causes increased filtration of fluid through the walls of blood vessels, its accumulation in tissues and increased lymph flow.
Due to the expansion of microvessels and their overflow with blood, as well as an increase in the amount of tissue fluid, the volume of tissue and organ increases, which can be clinically recorded by plethysmography (see). Increased blood flow in organs involved in heat transfer leads to an increase in their temperature. The color of the organ in arterial G. is scarlet-red due to the expansion of superficially located vessels (in the skin and mucous membranes - the main form of the superficial venous plexuses) containing arterial blood (oxyhemoglobin), since due to excess blood flow, oxygen is only partially used by tissues .
Since arterial G. is a compensatory phenomenon during inflammation, to lay down. methods that enhance it (eg, thermal procedures) are widely used.
Venous hyperemia
(syn.: congestive G., venous stagnation of blood) - patol, a change in blood circulation, which occurs when the outflow of venous blood is disrupted. With cardiac insufficiency, general venous stagnation of blood occurs in the systemic or pulmonary circulation. Obstacles to the outflow of blood from the venous system of a particular organ occur when the lumen of the veins is blocked by a blood clot or they are compressed from the outside by a tumor, scar or nearby organ (for example, the uterus during pregnancy), etc.
With venous G., the linear and volumetric velocities of blood flow decrease in the veins and capillaries, and intravascular pressure in them increases significantly, which contributes to the expansion of the lumen of all functioning veins and the opening of those venous vessels that were not functioning before. Due to the greater extensibility of the walls and the relatively greater increase in pressure in the venous section of the capillaries, their dilatation is noted, which is also facilitated by the increased extensibility of the supporting connective tissue during venous G. An increase in intravascular pressure, an increase in the permeability of vascular walls (a consequence of hypoxia) and the extensibility of the supporting connective tissue, in turn, contributes to a decrease in the hydrostatic pressure of tissue fluid and the accumulation of transudate.
The general symptoms of venous G. are associated with a decrease in the volumetric velocity of blood flow and overflow of blood vessels, the hemoglobin cut is predominantly reduced; as a result of this, the tissues experience insufficient blood supply and hypoxia (see).
Typical wedge, symptoms for venous G. are swelling (see) and cyanosis of the skin and mucous membranes (see Cyanosis). The bluish tint depends on the filling of the superficial venous plexuses with blood containing reduced hemoglobin, and on the optical phenomenon (florocontrast), when the dark red color of venous blood changes when translucent through the translucent layer of the epidermis. Due to the fact that the expansion of the veins may be uneven along their length, nodular protrusions appear in places (see Varicose veins).
The general principle of therapy for venous stagnation of blood is to eliminate patol, processes that impede blood flow in the veins (thrombosis, tumors, scars, etc.), and with general venous stagnation of blood - treatment of heart failure.
G. I. Mchedlishvili.
PATHOLOGI.COM
Blood circulation disorders include plethora (hyperemia) and anemia. Both conditions can be either venous or arterial, and each of them can be general or local (regional).
ARTERIAL HYPEREMIA
Arterial hyperemia is an increase in blood supply to organs and tissues as a result of an increase in the influx of arterial blood with its outflow unchanged. It is also possible to develop hyperemia with normal blood flow, but obstructed outflow. Arterial hyperemia can be physiological and pathological.
● Physiological arterial hyperemia develops locally, it can be working and reflex.
◊ Working (functional) hyperemia occurs with increased functional activity of an organ, tissue or system.
◊ Reflex hyperemia is manifested by redness of the facial skin when feeling anger or shame, or when exposed to physical and chemical factors (heat, cold, radiation).
● Pathological general arterial hyperemia develops with an increase in the volume of circulating blood (hypervolemia, plethora) or the number of red blood cells (erythrocytosis).
● Pathological local arterial hyperemia is more common; its pathogenesis can be inflammatory, post-ischemic, discompression, angioneurotic, collateral, or shunting.
◊ Inflammatory hyperemia is one of the signs of inflammation.
◊ Post-ischemic hyperemia forms after elimination of the factor that caused compression of the artery (removal of a tourniquet, etc.), which leads to anemia (ischemia) of neighboring organs.
◊ Discompression or vacate hyperemia (from the Latin vacuus - empty) is caused by a drop in barometric pressure (when placing medical cups, rapid removal of fluid during ascites or hydrothorax). This hyperemia can be general - during decompression sickness, a rapid rise from the depth of a diver, after depressurization of airplanes, pressure chambers.
◊ Angioedema develops in the presence of myoparalytic, neuroparalytic or neurotonic factors in the main vessel.
◊ Collateral hyperemia occurs in anastomoses when blood outflow is obstructed.
◊ In the presence of an arteriovenous shunt, as a result of which arterial blood flows into the veins, for example, in case of wounds, patent ductus arteriosus, oval window in the heart.
Interesting medical articles:
1) Forms of rickets
2) Massive aspiration syndrome
3) Morphogenesis of polyarteritis nodosa
| < Previous | Next > |
Pathological physiology
This type of arterial hyperemia occurs when the tone of the vasoconstrictor nerves decreases. In this case, the tone of vasodilators becomes higher than the tone of vasoconstrictors and the vessels dilate. One of the forms of neuroparalytic arterial hyperemia is hyperemia after previous ischemia, that is, after a state of local anemia. Under conditions of ischemia, tissue oxygenation is disrupted, and blood vessels, due to paralysis of the neuromuscular apparatus of their walls, lose their tone. If after this the ischemia stops and blood begins to flow to this area, then, due to the reduced tone of the vasoconstrictors, the arteries sharply dilate. This must be taken into account when carrying out certain medical procedures, in particular when releasing ascitic fluid, which in a number of diseases (heart failure, cirrhosis of the liver, etc.) can accumulate in the abdominal cavity in large quantities. This fluid compresses the mesenteric vessels and causes ischemia. If ascitic fluid is quickly released, a state of neuroparalytic arterial hyperemia will develop in the mesentery and its arteries will sharply dilate. As is known, the vessels of the mesentery can accommodate up to two-thirds of the blood circulating in the body. With such rapid redistribution, fainting may develop due to insufficient blood supply to the brain.
However, the phenomenon of post-ischemic arterial hyperemia can be successfully used in the practice of certain medical procedures, for example, in the case when it is necessary to perform venipuncture, and the patient’s arm veins are of small caliber, which makes it difficult to insert a needle. In this case, a tourniquet is applied to the patient’s shoulder so that the pulse on the radial artery disappears. After 1.5-2 minutes, the tourniquet is loosened until a pulse appears. During the period of ischemia, the tone of the arteries will decrease somewhat, and after the tourniquet is loosened, they begin to intensively fill with blood. Since the tourniquet compresses the veins, and the blood flow through the arteries is increased, the veins swell more and it becomes possible to perform venipuncture.
Assessing the role of arterial hyperemia in physiological and pathological conditions, it should be said that in general this change in local blood circulation has a positive meaning in pathological conditions, since with arterial hyperemia blood circulation in the hyperemic area increases, this area is more intensively washed with blood, and various harmful substances are quickly removed from it. substances, tissues are more oxygenated. Therefore, arterial hyperemia is often caused for therapeutic purposes using various physiotherapeutic procedures. However, sometimes arterial hyperemia can cause harm to the body, as, for example, when the head overheats. In this case, arterial hyperemia of the brain occurs, and the hyperemic tissue, due to increased blood and lymph filling, slightly increases in volume. Since the brain is located in a tight and hard cranium, even a slight increase in its volume leads to compression of the walls of the veins, which in turn causes a state of venous hyperemia and cerebral edema. This can lead to loss of consciousness, profound disorders of the vital functions of the body, and even death. Therefore, when exposed to intense sunlight for a long time, in order to prevent sunstroke, you should cover your head from direct sunlight, and when swimming for a long time in sunny weather, periodically cool your head in water.
Concluding the section on arterial hyperemia, it should be noted that its development is based on neurogenic mechanisms for regulating vascular tone. Therefore, arterial hyperemia is also called active hyperemia, since active changes in the tone of the vascular wall play a decisive role in its occurrence.