A huge number of people often experience headache attacks, but do not consider this a serious problem and do not pay due attention. However, this issue is very important, and the cause of the pain must be established.
In old age, a common cause of headaches is temporal arteritis. The disease is also called giant cell arteritis or Horton's syndrome. The vessels affected are mainly large and medium arteries in the temporal region. The inflammation is focal in nature, as certain areas of the vessels are affected. There is a disruption in the blood supply to the soft tissues of the brain, vision deteriorates, and throbbing pain appears in the temples. The disease is often referred to as temporal arteritis due to its localization in the temporal (temporal) blood vessels. Other arteries are much less likely to be affected by the disease.
Horton's disease is not common, but it is extremely dangerous to your health. People aged 50-70 years suffer the most. If inflammatory diseases are confirmed, self-treatment without medical supervision is not recommended.
What is temporal arteritis?
Temporal arteritis , also called Horton's disease, giant cell arteritis , or cranial arteritis, is a rheumatic vascular disease. Large and medium-sized vessels are mainly affected. Most often, the disease occurs on the branches of the carotid artery. These vessels supply blood to the temporal region, the back of the head and the eyes. In approximately every fifth patient, temporal arteritis affects the aorta. In less than one percent of cases, the disease affects blood vessels, arteries of the brain, or other arteries of internal organs.
Temporal arteritis is one of the autoimmune diseases. Because in the affected vessels certain cells of the immune system (granulocytes and lymphocytes) accumulate and form chronic inflammation. Particularly large cells called giant cells . The disease, commonly called giant cell arteritis today, causes cells in the vessel wall to multiply and eventually narrow the affected vessel . As a result, especially during physical activity, the blood supply is no longer sufficient. Depending on the organ affected, corresponding symptoms occur.
Temporal arteritis is also called Horton's disease or Horton's temporal arteritis, according to its discoverer. This is one of the most common rheumatic vascular diseases. The disease mainly affects adults and elderly people aged 50-70 years. Giant cell arteritis affects women about three times more often than men.
Symptoms
At the initial stage, the manifestation of signs of temporal arteritis is almost invisible. The clinical picture includes symptoms of an inflammatory process and disruption of the functioning of organs suffering from hypoxia.
The first signs are pain in the head, feeling unwell, and fever. The disease may be accompanied by polymyalgia rheumatica, then additional characteristic symptoms arise: pain in the muscles of the shoulders and pelvic region.
The symptoms of temporal arteritis are very similar to the symptoms of ARVI, so people often do not consult a doctor.
With the further development of the disease, the following signs appear:
- Severe pain in the temporal region, radiating to the neck and shoulders.
- Soreness of the temporal arteries, an increase in their density, which is easily felt upon palpation.
- Increased pain in the tongue area during chewing.
- Swelling and redness of the temporal area.
- Drooping eyelids.
- The scalp becomes covered with nodules.
- Problems with vision appear, up to its complete loss due to disruption of the blood flow supplying the optic nerve.
- Double vision, blurred vision, pain.
In addition, rapid weight loss occurs, appetite disappears and lethargy appears. Patients complain of pain when palpating and scratching the scalp. If treatment is not timely, in half of patients the symptoms of temporal arteritis rapidly develop, resulting in complete loss of vision.
Symptoms and signs
Almost all patients with temporal arteritis have particularly severe headaches. However, most of them have common symptoms of the disease that affect the eyes, heart, circulation or nervous system long before the first headache.
Headache due to temporal arteritis
About 70 percent of people with temporal arteritis have severe headaches. The pain is mostly boring and usually occurs on one side of the temple. The pain increases when a person chews, coughs or turns his head . This occurs due to damage to the artery that supplies the chewing muscles with oxygen and nutrients.
Horton's migraine treatment
Unfortunately, this section of medicine today remains almost a blank slate. There are no medications—at least not registered medications—that can be 100% effective in relieving Horton's migraine sufferers of their suffering.
Several medications are used to provide relief for Horton's migraine patients. The leading place in therapy is occupied by the use of lithium carbonate and steroidal anti-inflammatory drugs (methylprednisolone, prednisolone). Dehydrants (mannitol, Lasix) are also recommended for use.
Good results were obtained using an inhalation mask with 100% oxygen. However, this method often alleviates the attack rather than relieves it completely.
Triptans are also considered a good option (imigran, zomig). This is the most promising medicine at the moment.
Fun fact: Psilocybin and lysergic acid diethylamide have been shown to help relieve Horton's migraines. Statistics show the highest percentage of patients cured - more than fifty!
However, these substances are prohibited almost everywhere, which hinders the development of medicine in this direction. Therefore, patients are left to choose from what official medicine offers.
However, Swedish scientists are already developing a product based on lysergic acid diethylamine, which can be sold in pharmacies. It's a good news! The day will soon come when humanity will be able to overcome this terrible disease - we just have to wait a little longer.
ONLINE REGISTRATION at the DIANA clinic
You can make an appointment by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
Causes and risk factors
Temporal arteritis is a rheumatic disease that affects the functioning of the immune system. Certain immune cells called T cells cause an autoimmune reaction. Why this happens is not well understood. Perhaps the disease occurs as a result of infections caused by viruses (chicken pox, rubella) or bacteria (Mycoplasma pneumoniae, chlamydia).
Because not all people with such infectious diseases develop temporal arteritis, there is likely a genetic predisposition . People with certain proteins in their white blood cells (HLA-DR4) are more prone to this condition. Additionally, temporal arteritis is more common in people with polymyalgia , another rheumatic pain syndrome.
Causes
Inflammation of the temporal artery occurs as a result of an autoimmune process. In many patients, during examination, antibodies to immunoglobulins M and A are detected. Viral hepatitis, influenza, and herpes can provoke the development of pathology.
The body can produce antibodies after contact with viruses and bacteria. In some cases, viruses can change the antigenic composition of cells and provoke the immune system to perceive them as foreign.
This leads to the fact that antibodies begin to attach to the walls of blood vessels and destroy them. Foci of inflammation appear at the site of destruction.
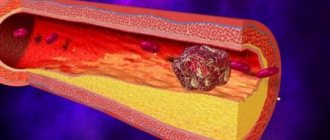
The walls first become denser, and then granulomas form in them. Due to the fact that the walls become thick with an uneven surface, blood clots can form in them. The lesion may not extend to the entire artery, but only cover a separate segment.
This process is asymmetrical and is localized in the temporal artery. Sometimes it involves the vertebral, posterior colossal, ophthalmic and central retinal arteries. There are frequent cases of detection of changes in the carotid, subclavian, mesenteric and iliac arteries.
Examinations and diagnostics
The necessary specialists if temporal arteritis is suspected are doctors of rheumatic diseases (rheumatologists) or nerve diseases (neurologists).
The American Rheumatoid Diseases Task Force (ACR) has put together a set of criteria that your doctor can use to diagnose Horton's disease.
First, the doctor takes a medical history ( anamnesis ), and then, if a disease is suspected, he orders tests, imaging studies, and a biopsy.
A blood test may show increased levels of inflammation. If a person meets at least three of the following five criteria, there is a greater than 90% chance of Horton's disease:
- age over 50 years;
- severe headaches;
- altered temporal arteries (painful, weaker pulse);
- increased erythrocyte sedimentation rate (in blood tests);
- tissue changes of the temporal artery.
Further research
In most cases, a specific ultrasound examination of the temporal arteries is performed. The temporal artery can also be examined using magnetic resonance imaging (MRI). For this purpose, the patient is first injected into a vein with a certain contrast medium, and then placed on a movable couch in an MRI chamber. This examination requires certain technical requirements, which can often only be carried out in specialized centers.
Classic manifestations of the disease
Temporal arteritis, the symptoms of which most often result from inflammation of the cranial and temporal (temporal) blood vessels, look like this:
- throbbing headache
- discomfort in the maxillofacial area while eating,
- sometimes fever
- visual impairment (“blurred vision”, double vision).
But other arteries may also be affected. Therefore, the following symptoms may appear:
- muscle pain in the shoulders or hips (called polymyalgia rheumatica);
- sore throat;
- cough;
- depression;
- fever;
- loss of appetite.
You should immediately consult a doctor if clinical manifestations of giant cell arteritis appear. Patients with this vasculitis require immediate treatment with glucocorticosteroids. If therapy is not started in time, this can lead to the development of serious complications, such as partial loss of vision.
Treatment
Once Horton's temporal arteritis has been diagnosed, the person should be immediately treated with the drug cortisone . For the first four weeks, a dosage of one milligram of prednisolone per kilogram of body weight is recommended. If symptoms have resolved due to therapy and blood levels of inflammation have returned to normal, the dose should be continuously reduced. If symptoms recur, more prednisolone should be taken again. The attending physician will work with the patient on a precise treatment schedule. If blindness is inevitable, prednisolone therapy should be given in large doses through a vein over three to five days.
Because cortisone therapy can cause many unwanted side effects, it is necessary to take additional medications. Calcium and vitamin D reduce the risk of osteoporosis (brittle bones). In case of possible vascular occlusions, aminosalicylate (for example, aspirin) should be taken. Proton pump inhibitors protect the gastric mucosa. In addition, your blood sugar levels should be checked regularly and adjusted if necessary.
Treatment method
Treatment of temporal arteritis takes a long time, but always achieves a positive result. If intervention is not timely, there is a risk of blindness and stroke. Possible treatments:
- Therapeutic;
- Surgical;
- Folk remedies.
Therapeutic method
The therapeutic method of treatment is the use of prednisolone or methylprednisolone. It is used in the absence of complications.
Initially, prednisolone is prescribed at 60 milligrams per day. The duration varies from 2 to 4 days. The amount of the drug is reduced by 5 mg weekly so that the daily dose is up to 40 mg. And they continue to reduce it, first by 2 mg every week, then by 1 mg. Active treatment usually lasts about a year. But depending on the severity of the disease, it can last up to two years.
During the treatment period, it is important to take blood tests, the composition of which affects the course of treatment of the disease. To improve the condition of the blood, the drugs chimes and aspirin are used. Medicines that have vasodilating and vasodilating effects are also prescribed.
Methylprednisolone is taken 1 g intravenously for three days. Then they continue to take it in tablet form.
If the patient suffers from diabetes or infectious diseases, additional treatment with antibacterial drugs is carried out.
If it is impossible to use prednisolone and methylprednisolone or if they are ineffective, the doctor will prescribe cytostatics: azathioprine, methotrexate.
Surgical intervention
In severe cases and complications of arteritis, surgery is prescribed. For example, in the case of blood clots in blood vessels or in the presence of oncology.
Folk remedies
Treatment with traditional methods can negatively affect the health of a sick person. With possible ineffectiveness, the disease will continue to develop, and serious complications may occur. Folk remedies help to get rid of pain and inflammation for a short time, but do not fight the source of the problem itself. In any case, therapy is necessarily accompanied by medication. Traditional methods will help strengthen the patient’s immunity and relieve negative symptoms.
To reduce headaches, use the following recipes:
- Pour boiling water over the crushed St. John's wort herb, boil for 15 minutes, strain and take throughout the day.
- Squeeze the juice out of garlic, soak a cotton pad or swab with it and apply to your head.
- Tea made from chamomile or lemon balm has a good calming effect.
- An aloe leaf will come to the rescue in the fight against pain, which is cut and applied with an incision to the temporal or frontal lobe of the head.
- It is recommended to eat several currants, lingonberries, strawberries a day or drink berry juice, which helps reduce the intensity of pain.
Etiology
To date, Horton's disease does not have an exact etiological picture. The disease belongs to the group of systemic vasculitis, as it affects only large vessels.
Most often, provoking factors for the progression of temporal arteritis are:
- severe infectious diseases;
- too weakened immune system;
- autoimmune processes.
Studies have shown that the patient’s body begins to produce antibodies. As a result of this, an autoimmune process begins to develop that affects large vessels. This is precisely what serves as the main reason for the development of the pathological process.
Causes
What causes this vasculitis and what mechanisms are involved in its development are not known for certain. There is a clear connection between the disease and the aging process. It is clear to doctors that disorders of the immune system are the basis for the development of giant cell arteritis. But why this happens and how is still unknown.
We recommend reading the article about allergic skin vasculitis. From it you will learn about the causes of the pathology, its prevalence, symptoms, diagnosis and treatment.
Diagnostics
The examination plan for a patient with temporal arteritis includes the following procedures:
- Inspection and survey. The doctor analyzes the existing symptoms, collects anamnesis, and identifies external signs of the disease.
- General blood analysis. In case of inflammatory processes in the arteries, the result of the study reflects a decrease in hemoglobin levels, an increase in the number of leukocytes and a pronounced increase in ESR (up to 70 mm/h).
- Blood chemistry. With autoimmune damage to the arteries, a decrease in albumin content is detected.
- Enzyme immunoassay blood test. Helps detect antibodies that destroy healthy cells.
- Ophthalmoscopy. Aimed at identifying signs of damage to the vessels of the fundus and optic nerve.
- Ultrasound Dopplerography of the vessels of the head. During the procedure, the patency of the arteries and the speed of blood flow are determined.
- CT and MRI of the brain. Used to identify neurological disorders associated with arteritis.
- Angiography. Helps detect signs of vessel narrowing and the presence of wall thrombi.
- Biopsy followed by histological examination. It is considered the most informative method for diagnosing the temporal artery. Horton's disease reveals thickening of the inner and middle layers of the vessel wall, infiltrative formations containing giant cells and lymphocytes. The absence of characteristic histological signs in the presence of typical symptoms is not a reason to cancel the diagnosis.
Establishing diagnosis
The final diagnosis is made only after a biopsy (usually the temporal artery is examined). To do this, a small amount of anesthetic (usually novocaine or lidocaine) is injected under the skin in the area of the temporal artery projection, after which an incision is made and the vessel is removed. This manipulation is practically safe for the patient (sometimes there are reactions to the anesthetic), and it leaves a small scar.
General blood analysis
There are blood tests that help the doctor "move in the right direction" when making a diagnosis. Almost every patient with giant cell arteritis has an increased ESR (erythrocyte sedimentation rate), in addition, anemia (few red blood cells in the blood) is quite common. In many pathological conditions, elevated ESR and anemia occur, so the final diagnosis always depends on a biopsy of the temporal artery.
There are situations when even this analysis does not bring a positive result, that is, “giant” cells are not found in the wall of the removed artery. It has been proven that Horton's disease can affect the temporal vessels individually. Therefore, when a biopsy on one side is negative, taking an artery from the other for analysis helps make a final diagnosis.
Causes of giant cell arteritis
Scientists don't yet fully know why people get giant cell arteritis.
This is an autoimmune disease. Those. a condition where the immune system, which is the body's defense system that fights infections, becomes confused and attacks healthy tissue in the body.
In people with this disease, the immune system mistakenly attacks healthy arteries.
It is possible that the genes that a child inherits from his parents increase the likelihood of developing the disease. However, just because someone has a disease does not mean that their children will necessarily get it.
Disease prevention
Primary prevention of temporal arteritis is very difficult, since to date the exact cause of the development of the disease has not been established. Secondary prevention (prevention of exacerbation) consists of lifelong prescription of steroid hormones and immunosuppressants.
How to determine whether a child has viral or bacterial conjunctivitis, you will learn in the article.
How to restore vision with farsightedness is described in detail here.
Treatment of macular degeneration of the retina: https://eyesdocs.ru/zabolevaniya/makulodistrophiya/makulyarnaya-dystrophiya-setchatki-glaza.html