In the early and late neonatal period of a child’s life, many decompensated pathologies of its development may appear, including congenital malformations of various organs and systems.
Such pathological conditions also include congenital heart disease such as patent ductus arteriosus (PDA), which occurs in 10-18% of newborns, more often in girls.
general information
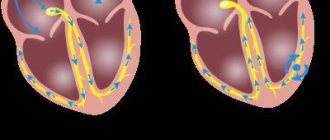
This congenital defect, related to the pathology of the cardiovascular system, is the absence of closure of the arterial (botallian) duct , which connects the pulmonary artery and the baby’s aorta in the prenatal period.
What happens if a child has patent ductus arteriosus? The baby begins to form a functioning “vessel” between these anatomical formations, which is unnecessary for the body existing outside the mother’s womb, which leads to obvious disruptions in the functioning of not only the heart, but also the respiratory system .
Diagnosis of pathology and listening noises
According to the examination, there may be a deformed chest in the cardiac region and at the site of the projection of the apex - strong pulsation.
The noise on auscultation has a rough timbre, with a hard, metallic (machine) tint, and is heard constantly. The best place to listen to it is the left second intercostal space or subclavian fossa.
Instrumental examination data can help in making a diagnosis:
- On the radiograph, the size of the heart is increased and the pulmonary pattern is enhanced.
- ECG - there is an overload of the heart. Tachycardia, arrhythmia.
- EchoCG - the length and width of the duct is determined.
X-ray with patent ductus arteriosus
If necessary, to distinguish this defect from another pathology, the following may be prescribed: aortographic examination, cardiac catheterization, MRI.
Causes and risk factors
Knowledge of the etiological factors that contribute to the failure of this fetal communication is especially important not only for doctors, but also for expectant mothers, so that they can promptly sound the alarm and seek medical help in case of any suspicion. This knowledge is also no less important for preventing the occurrence of PDA.
Normally, the ductus botallus should be replaced by the ligament arteriosus in newborns 2-10 weeks after birth; if the baby is premature, it can become obliterated within a few months or even within the first 1-2 years.
However, some factors can affect its healing. Among the main causes of patent ductus arteriosus and congenital heart defects of the newborn in general are :
- Infectious factor (herpes viruses, CMV, mumps, influenza, herpes, rubella, enteroviruses or Coxsackie virus in the first third of gestation).
- Chronic extragenital maternal pathology (diabetes mellitus, hypothyroidism and other diseases).
- An abnormal pregnancy with the development of early toxicosis or a threat leading to its premature termination.
- Heredity (if there is a congenital unclosed ductus arteriosus in the mother or in the child’s closest relatives).
- The influence of toxic compounds during pregnancy (chronic alcoholism, occupational hazards in the mother, nicotine intoxication, drugs, some medications).
- PDA in the structure of chromosomal diseases (Shereshevsky-Turner, Patau, Down, Edwards syndrome).
- Mixed influence of the above factors.
Types and phases of flow
There are isolated PDA, which occurs in approximately 10% of all cases of this defect, and combined with other heart defects (atrial septal defect in children, coarctation of the aorta in newborns, forms of pulmonary artery stenosis).
It is also customary to classify open botalls according to the phases of its development :
- Stage 1 is called “primary adaptation” and lasts during the first 3 years of the baby’s life. This is the most intense stage in terms of severity of clinical symptoms, which can even lead to death if suitable surgical treatment is not provided.
- Stage 2 is characterized by relative compensation of the clinical picture of the disease and lasts 3 to 20 years. A decrease in pressure in the vessels of the pulmonary (pulmonary) circulation and an increase in pressure in the cavity of the right ventricle develops, which leads to its functional overload during the work of the heart.
- At stage 3, irreversible sclerosis of blood vessels in the lungs steadily progresses, which causes pulmonary hypertension.
Considering the level of pressure in the lumen of the pulmonary artery and pulmonary trunk, the following degrees of PDA are distinguished :
- When the systolic pressure of the pulmonary artery is no more than 40% of the body's blood pressure.
- The presence of symptoms of moderate hypertension in the pulmonary artery (40-75%).
- When there are symptoms of severe hypertension in the pulmonary artery (over 75%) and there is blood flow from left to right.
- When severe hypertension develops in the pulmonary vessels and the pressure equals the systemic arterial pressure, the blood flows from right to left.
Pathogenesis
Hemodynamic disturbances in congenital heart defects such as patent duct of Batalov are caused primarily by the discharge of blood from the aorta into the pulmonary trunk due to a pronounced pressure gradient. As a result, the pulmonary circulation becomes overloaded, and stagnation gradually develops in it, followed by the exudation of the liquid part of the plasma into the surrounding tissues. The lungs become easily susceptible to infections and become unable to properly oxygenate the blood. At the same time, due to a decrease in the volume of circulating blood in the systemic circle, it becomes depleted, all organs suffer from severe hypoxia, and since the baby’s body grows at maximum intensity during the first year, they require an extremely large amount of nutrients and energy. And due to a deficiency of this, their dystrophy increases, as a result of which their functioning suffers. The child slowly gains weight, often gets sick, becomes restless, and constantly screams.
Why it’s dangerous: possible complications
- The development of endocarditis of a bacterial nature, leading to damage to the inner layer of the wall of the heart chambers, primarily in the area of the valve apparatus.
- Bacterial endarteritis.
- Myocardial infarction with risk of rhythm disturbance or death.
- Heart failure of varying severity.
- Swelling of the lung tissue due to increased pressure in the pulmonary vessels, requiring extremely rapid action by medical personnel.
- Rupture of the main vessel of the human body – the aorta.
Symptoms
The symptoms that appear with this type of congenital heart defect depend entirely on the degree of hemodynamic changes in the body . In certain cases, the clinical picture will not be traced.
In others, it progresses to extreme degrees of severity and manifests itself in the development of a cardiac hump (a convex deformation of the anterior chest wall in the area of the projection of the heart), downward movement of the apical impulse of the heart along with the expansion of its zone, tremors of the heart in its lower and left parts, persistent shortness of breath with the position of orthopnea and severe cyanosis.
The main symptoms of PDA in less severe clinical cases are:
- increased heart rate;
- increased breathing;
- enlarged liver (hepatomegaly) and spleen;
- electrocardiographic signs of left side enlargement;
- specific murmur during auscultation of the heart in the second left intercostal space near the sternum (systole-diastolic);
- rapid high pulse on the radial arteries;
- an increase in the level of systolic systemic pressure and a decrease in diastolic pressure (sometimes to zero).
When to see a doctor
Not in every case, parents can notice changes in the health of their child and suspect this congenital pathology, which, of course, worsens the prognosis for the baby.
The earlier the developmental defect was found, the greater the chance of providing adequate therapy and compensating for the pathological symptoms of the disease that have developed.
Parents should remember that a trip to the doctor is necessary if they identify the following symptoms in their baby:
- sleep rhythm disturbance;
- drowsiness;
- slow weight gain;
- shortness of breath at rest or after light exertion;
- bluish discoloration of the skin after exercise;
- lethargy, refusal of games and entertainment;
- frequent acute respiratory infections and acute respiratory viral infections.
You should contact your local pediatrician , who, if there are pathological symptoms, can refer you for consultation to other specialists: a pediatric cardiologist, a pediatric cardiac surgeon.
Complications
Severe complications and dangerous consequences of PDA:
- Bacterial endocarditis is an infectious inflammation of the inner lining of the heart, leading to dysfunction of the valve apparatus. Patients develop fever, chills and sweating. Signs of intoxication are combined with headache and lethargy. Hepatosplenomegaly develops, hemorrhages appear in the fundus and small painful nodules on the palms. Treatment of pathology is antibacterial. Patients are prescribed antibiotics from the group of cephalosporins, macrolides, fluoroquinolones, and aminoglycosides.
- Heart failure develops in the absence of timely cardiac surgery and consists of insufficient blood supply to internal organs. The heart stops pumping blood in full, which leads to chronic hypoxia and deterioration in the functioning of the entire body. Patients experience shortness of breath, tachycardia, swelling of the lower extremities, fatigue, sleep disturbance, and persistent dry cough. Treatment of pathology includes diet therapy, drug therapy aimed at normalizing blood pressure, stabilizing heart function and improving blood supply.
- Myocardial infarction is an acute disease caused by the appearance of foci of ischemic necrosis in the heart muscle. The pathology manifests itself as characteristic pain, which is not relieved by taking nitrates, agitation and anxiety of the patient, pale skin, and sweating. Treatment is carried out in a hospital setting. Patients are prescribed thrombolytics, narcotic analgesics, and nitrates.
- Reverse blood flow through the wide ductus arteriosus can lead to cerebral ischemia and intracerebral hemorrhage.
- Pulmonary edema develops when fluid moves from the pulmonary capillaries into the interstitial space.
Rarer complications of PDA include: aortic rupture, incompatible with life; aneurysm and rupture of the ductus arteriosus; pulmonary hypertension of sclerotic nature; cardiac arrest in the absence of corrective therapy; frequent acute respiratory infections and acute respiratory viral infections.
Diagnostics
Diagnosis of patent ductus botallus includes several groups of research methods. With an objective examination of the child, the doctor can determine:
- rapid pulse;
- an increase in systolic pressure with a simultaneous decrease in diastolic pressure;
- changes from the apical impulse;
- expansion of the boundaries of cardiac dullness (borders of the heart);
- Gibson's murmur described above (systole-diastolic);
- anamnestic symptoms associated with possible exposure to risk factors for this defect.
Among the instrumental diagnostic techniques, the following are actively used:
- ECG (electrocardiography) . There is a tendency towards hypertrophy of the left parts of the heart, and in more severe stages, the right parts with deviation of the cardiac axis to the right. As the disease progresses, signs of heart rhythm disturbances appear.
- Echocardiography . It also gives information about the expansion of the left heart cavities. If you add a Doppler study, a mosaic pattern of blood flow through the pulmonary artery is determined.
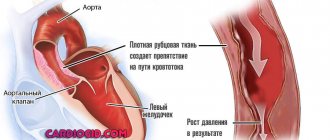
- X-ray of the chest organs. Characteristic is the strengthening of the contours of the lung pattern, an increase in the transverse size of the heart due to the left ventricle in the initial stages of the manifestations of PDA symptoms. If hypertension of the pulmonary vessels develops, the pattern of the lungs, on the contrary, becomes poorer, the trunk of the pulmonary artery bulges, and the heart is enlarged.
Differentiation of the diagnosis is necessarily carried out with other congenital heart defects, such as:
- combined aortic disease;
- incomplete atrioventricular canal;
- defective septum between the ventricles;
- defective septum of the aorta and pulmonary artery.
Treatment of patent ductus arteriosus
When should treatment be given?
Treatment should be carried out when the first signs of the disease (symptoms) are detected,
Principle and methods of treatment:
The choice of treatment method in children with patent ductus arteriosus depends on many factors - the degree of patent closure, concomitant diseases, other congenital anomalies and malformations of the heart, increasing symptoms, complications and disturbances in hemodynamic parameters.
There are two types of treatment: medication and surgery.
Drug or conservative treatment:
- This method is indicated for mild pathology without significant changes in hemodynamic parameters, concomitant pathology, including additional defects and anomalies of heart development, complications.
- The doctor prescribes non-steroidal anti-inflammatory drugs (ibuprofen, indomethacin), the essence of which is that they block the excretion of prostaglandins, which contribute to patent ductus arteriosus, antibiotic therapy, and drugs that stimulate diuresis.
Of the surgical methods, the most commonly used are ligation of the duct, application of clips at its ends with intersection and ligation on the wall of the aorta and pulmonary artery; they also use the embolization method with a spiral wire; this type of surgical treatment is indicated for large duct diameters of about 5 millimeters.
Surgery is best performed when the child reaches two to five years of age.
Treatment
A conservative treatment method is used only in premature babies and consists of administering prostaglandin formation inhibitors to medically stimulate the spontaneous closure of the duct.
The main drug in this group is Indomethacin . If there is no effect after repeated administration of the drug three times in children over three weeks of age, then surgical obliteration is performed.
Children are surgically treated at the age of 2-4 years , this is the best period for this method of therapy. In extended use is the method of ligating the ductus botallus or transversely crossing it, followed by suturing the remaining ends.
These operations are quite simple in nature, however, pediatric cardiac surgeons must have high professional skills for the best outcome of the operation.
Prognosis and prevention
If the duct is not operated on, death occurs in people aged about 40 years due to the development of severe hypertension in the pulmonary arteries and severe degrees of heart failure. Surgical treatment provides favorable outcomes in 98% of young patients.
Preventive actions:
- Avoiding smoking, alcohol abuse, and drugs.
- Avoiding stress.
- Mandatory medical and genetic counseling both before and during pregnancy;
- Sanitation of foci of chronic infection.
Patent ductus arteriosus is a serious congenital pathology that carries high mortality rates if untimely or inadequate treatment occurs.
The debut of its clinical picture is the development of signs of pulmonary hypertension and cardiac failure. However, if this disease is diagnosed in time, its outcome is very favorable , which is confirmed by modern statistical data.
Symptoms of PDA
Patent ductus botallus accounts for 9.8% of all congenital heart defects. Its severity and prognosis strongly depend on the width of the shunt - the larger it is, the more difficult it is for the body to compensate for the pathology. As a result, arterial and venous blood flows mix, the heart and lungs experience severe overload, and pulmonary hypertension can develop, followed by heart failure.
Hemorrhoids kill the patient in 79% of cases
Children with PDA are characterized by slow growth and development, they are weak, often get sick, they have poor appetite and fatigue. If the duct is wide enough, symptoms will appear in the first months; parents may notice the following features:
- Pallor (PDA refers to the so-called “white” heart defects), which is gradually replaced by cyanosis of the skin.
- Frequent breathing, shortness of breath after eating or crying.
- Poor weight gain.
- Developmental delay.
If the duct is small, it may not appear during the first years. You can suspect the presence of pathology based on the following general signs:
- Fast fatiguability.
- Soreness, frequent acute respiratory infections, bronchitis, pneumonia.
- Tachycardia.
- Increased sweating.
Patent ductus arteriosus leads to progressive heart failure and symptoms develop and progress in all children over time. In some cases, patients develop underlying heart disease. Thus, patients with PDA are characterized by the presence of bacterial endocarditis - inflammation of the inner lining of the heart. Aneurysms can also form in the ductus botallus, and their rupture causes death.