Structure of the heart
The heart is one of the organs responsible for human life support. It pumps blood through the vascular bed, so tissues and internal organs receive a sufficient amount of oxygen and nutritional components. The heart is a kind of pump.
The organ has a muscular-fibrous structure. Its cavity is divided into four chambers:
- right atrium (RA);
- right ventricle (RV);
- left atrium (LA);
- left ventricle
During normal operation of the organ, the blood that enters the right and left sections does not mix. To ensure the necessary direction of blood flow, there are connective tissue elements. They are called valves, and are located on the border between the atria and ventricles, heart chambers and great vessels. Valves include:
- mitral, or tricuspid (in the left half of the organ);
- tricuspid, or bicuspid (localized on the right side of the heart);
- aortic;
- pulmonary.
When the myocardium relaxes (diastole), blood is pumped from the atria into the ventricles. When the heart muscle contracts (systole), blood flow is directed into the vascular bed. From the LV cavity it enters the aorta, from where well-oxygenated blood flows to the somatic organs, providing them with nutrition. From the pancreatic chamber, blood is directed to the pulmonary vascular basin. In this case, it is saturated with carbon dioxide.
To maintain the tone of the valve apparatus and create a strong frame, connective tissue threads stretch from the muscular trabeculae in the ventricular cavity to the valve leaflets. They are called cords. Their task is to prevent the valve leaflets from opening during systole.
Attention! There are clinical situations when an extra notochord is formed during intrauterine development. It's called additional. According to statistics, in 90-95% of cases the developmental anomaly concerns the LV cavity.
Symptoms and manifestations
An abnormal chord in the heart does not show any characteristic external signs; its existence may not be known for years. Most often, it is detected only during an ultrasound examination, and the basis for referral for an ultrasound is when the doctor listens to a noise in the area during normal heart function, which should not exist.
For information! Murmurs are acoustic phenomena (whistle, creaking) that appear during contraction of the heart muscle, between beats, and are audible when listening with a stethoscope.
The intensity of the noise depends on the location of the abnormal chord of the left ventricle and on their number (if there is a multiple phenomenon). Also, with multiple anomalies, you can notice some features of the general condition:
- increased fatigue;
- mood swings and instability of psycho-emotional state;
- arrhythmia;
- increased heart rate;
- pain in the chest area.
Get a treatment program
Varieties of cardiac chords
There is a generally accepted classification of LVDC. Additional chords differ in cellular structure:
- connective tissue;
- tendon;
- muscular;
- mixed.
By localization they distinguish:
- apical (in the area of the apex of the ventricle);
- mid-located;
- in the area of the basal part of the ventricle.
According to the number of cords formed, chords can be single or multiple. Based on the plane in which the cord is located, there are:
- longitudinal;
- diagonal;
- transverse.
The chords of the left ventricle, which extend in longitudinal or diagonal directions, do not create obstacles to normal blood flow. If the cord is located in the transverse plane, it becomes a barrier to blood flow. Transverse chord of the left ventricle often leads to various types of arrhythmias in adult patients.
What are false chords of the left ventricle?
False chords are small, thread-like tendon structures. They contain elements of the conduction system of the heart. This causes the risk of blood flowing not only through physiological pathways, but also through these tendon structures. In this case, a disturbance in the rhythm of the heart may occur. In medicine, chords are usually classified depending on their location (diagonally, longitudinally or transversely), as well as their number (one chord occurs in approximately 60% of cases, in other cases there are several formations).
Causes of pathology
The disease is characterized by a hereditary predisposition. Route of transmission: from mother to child. An infant can inherit the pathology from its father in no more than 7-8% of cases. The formation of an accessory chord in the cavity of the left ventricle occurs in the prenatal period, that is, a person is already born with it.
The formation of an anomaly in later periods of life (childhood, adolescence, adulthood) is excluded.
The formation and development of structures of the cardiovascular system begins at the 5-6th week of embryogenesis. The influence of unfavorable external factors leads to the formation of congenital malformations, or MARS. Negative reasons include:
- unfavorable environmental situation;
- work associated with hazardous production, contact with volatile chemical compounds, adverse effects of physical factors;
- harmful addictions of a pregnant woman (drinking alcohol, drugs, chronic nicotine intoxication).
Description of the pathology
The reason for the development of anomalies is associated with deviations in genes located on the X chromosomes.
The more there are, the greater the likelihood of developing an accessory chord in a child. Important! The trait is transmitted through the maternal line in 90%, and through the paternal line in 10%.
It is not the chord itself that is inherited, but the factors that cause it. Even in the first months of the baby’s intrauterine development, additional tissue is laid down.
During the formation of the interventricular septum, “extra” tissue often becomes part of it. A child with a hereditary history of heart abnormalities is born without LVDC.
But the action of a number of factors during pregnancy contributes to the fact that the “excess” tissue degenerates into an additional chord. This:
- bad habits (smoking, alcohol);
- use of certain medications (ACE inhibitors);
- stress;
- viral diseases.
In the presence of such chronic diseases as diabetes mellitus, systemic lupus erythematosus and rheumatoid arthritis, there is a risk of developing an accessory chord even without heredity.
The notochord in the heart is a fibrous tissue (very similar to muscle) that connects the walls of the left ventricle. It may be abnormal, that is, it may have a connection in the heart muscle that is atypical for the human body.
In addition, there may be an extra chord in the heart, that is, an additional one. Such defects are transmitted hereditarily.
It should be noted that the carrier of the pathology is exclusively the mother. There are several types of cardiac chords, they are divided by type of direction, location, connection of the walls of the ventricle.
By type of direction, diagonal, transverse and longitudinal chords are distinguished; by location, they are located in the left or right ventricle. Depending on the method of connecting the walls of the ventricle, there are basal, middle and apical chords. They can also be single or multiple.
An abnormal chord is a feature of the anatomical structure of the heart, which is a fibrous muscle or fibrous cords located in the left ventricle of the heart. These cords connect the walls of the left ventricle to each other.
Characteristic symptoms
In children, the disease is characterized by an asymptomatic course. Over time, when an intense growth spurt occurs, nonspecific signs may appear. They are due to the fact that the child’s body does not have time to adapt to the changed conditions.
Clinical symptoms of the accessory chord of the left ventricle of the heart:
- chest pain;
- dizziness, syncope;
- asthenic syndrome;
- impaired ability to concentrate;
- arrhythmias;
- surges in blood pressure.
Attention! Similar manifestations of the disease will occur in the presence of several false cords in the LV cavity and impaired myocardial functioning.
The clinical picture may be supplemented by symptoms that are caused by inadequate development of connective tissue. These include:
- pathological mobility of articular surfaces;
- nephroptosis (pathological change in the position of the kidneys);
- megaureter (enlargement of the ureter due to a stricture above the entrance to the bladder);
- hiatal hernia;
- gastroesophageal reflux disease;
- scoliosis.
In adult patients, the following signs of cardiac development abnormalities are recorded:
- increased heart rate;
- rhythm disturbances;
- pathological change in the structure of the endocardium;
- dilated ventricular dysfunction.
Clinical picture
False chord of the left ventricle of the heart in most cases does not manifest its presence and does not affect a person’s quality of life. Many patients with this diagnosis do not even suspect an anomaly in the main organ for years.
Read it! Bacterial endocarditis
It should be noted that there are not only single anomalies, but also multiple ones. In this case, there is a connection between the false chord and heart block in the form of cardiac arrhythmias, early repolarization of the ventricles or their overexcitation.
The anomaly cannot be determined by listening, but in some cases the presence of a pathology can be suspected, as with many other heart pathologies. For example, a false chord and blockade of the legs of His may be accompanied by systolic murmurs in the upper part of the organ (the latter causing brighter sounds).
Deterioration in general health is often observed, such as:
- increased fatigue;
- weakness, lethargy;
- the appearance of pain in the chest;
- constant emotional stress.
Attention! With this anomaly, patients complain of the sensation of distinct sounds during heart contractions.
Diagnostic methods
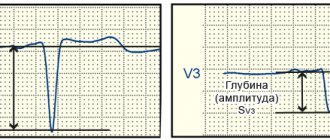
A specialist can detect a false chord only based on the results of an instrumental examination. In some clinical situations, the physician or pediatrician will listen for a systolic murmur when performing a physical examination of the patient. The electrocardiogram is uninformative. Deviations in the tape are recorded only when a heart rhythm disturbance occurs.
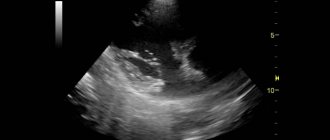
The main diagnostic method is echocardiography - ultrasound examination of organ chambers, their structure and functions. If the specialist additionally performs Doppler sonography, he will get an idea of the location, thickness, length and place of attachment of the connective tissue cord, and the speed of blood flow in this area. This is the most accurate method to diagnose LVDC.
For some patients, the doctor recommends daily monitoring of cardiogram parameters. The patient walks with a portable ECG machine for 24 hours, following instructions regarding physical activity. Based on the results of the study, the doctor can judge the presence or absence of hemodynamic disorders. This result determines the need for drug support.
Features of the disease in children
If the ectopic chord of the left ventricle in a newborn does not cause negative symptoms, special therapy is not required. It is necessary to perform an echocardiogram annually and show the child to a cardiologist. Additional activities recommended:
- compliance with the rest and work regime;
- proper nutrition;
- physical therapy classes;
- hardening;
- frequent walks in the fresh air;
- 8-10 hour sleep.
Important! It is prohibited to subject a child to psycho-emotional overload and send him to sports clubs without the permission of a cardiologist.
Diagnostics
The main method for diagnosing an abnormal chord of the left ventricle is ultrasound examination. For children in the first year of life, it is prescribed only for indications, for example, after a sore throat or in the presence of risk factors for the development of heart disease. An unscheduled ultrasound of the heart may be prescribed if, during listening, systolic murmurs were detected - murmurs heard during the contraction period between the first and subsequent sounds of the heart muscle. In some cases, for example, with multiple chordae, ultrasound alone is not enough to make an accurate diagnosis and objectively assess the child’s health, so the doctor may prescribe additional examinations.
Ultrasound of a child's heart
Methods of auxiliary diagnostics for suspected LVDC include:
- electrocardiography;
- daily monitoring using Holter;
- bicycle ergometry (electrocardiographic research method to determine individual tolerance to physical activity).
Bicycle ergometry is used mainly in older children and adolescents. To compile a complete clinical picture, the child is also prescribed a laboratory test of biochemical parameters of blood and urine.
Bicycle ergometry
Treatment
The disease cannot be corrected with medication. The doctor recommends taking medications to patients who have detected pathological changes in hemodynamics, diagnosed rhythm disturbances or other complications.
Pharmacological agents:
- vitamins (group PP, B) – improve trophism of the heart muscle;
- medications based on magnesium and potassium - they normalize the conduction of nerve impulses;
- L-carnitine – enhances metabolic processes in the myocardium (the medicine is prescribed in courses);
- nootropics – for the correction of unstable blood pressure, vegetative-vascular dystonia;
- antiarrhythmic drugs.
Attention! If endocarditis and paroxysmal tachycardia occur against the background of pathology, surgical intervention is recommended.
Cardiac surgery includes:
- cryodestruction of the additional chord;
- Let's cut off the cord.
Rarely, but the following complications may occur:
- paroxysmal tachycardia;
- ischemic stroke;
- arrhythmias;
- chronic cardiovascular failure;
- ventricular fibrillation;
- endocarditis;
- formation of connective tissue compactions in the thickness of the heart walls;
- pulmonary embolism.
Lifestyle with pathology
A child diagnosed with LVDC is not sick. He can lead a normal life according to his age. The disease prohibits professional participation in sports that involve heavy physical activity. To avoid complications, you must adhere to the following rules:
- A clear daily routine that balances work and rest time.
- Sleep at least eight hours a day.
- Adhere to the principles of proper nutrition.
- Eliminate fatty, fried foods, spices, spices, and fast food from your diet.
- Regularly perform therapeutic exercises and harden.
- Avoid psycho-emotional overload.
- Do not do heavy physical work.
- Take a course of restorative massage annually.
- Do not self-medicate.
- Visit a cardiologist regularly.
For sports activities, a child who has an additional chord in the left ventricle of the heart is allowed to:
- athletics (amateur sports);
- exercises using the Swedish wall;
- ballroom dancing;
- medium-long distance hiking trips.
Children with LVDC are prohibited from:
- skydive;
- go diving;
- visit the panic room;
- any extreme entertainment.
Attention! The presence of an additional chord in the left ventricle cannot be a medical disqualification from military service. Young people who have been diagnosed with serious complications of the disease will not be subject to conscription. During the physiological course of pregnancy, a woman can give birth on her own.
What diagnostics and therapy are prescribed?
If the doctor detects murmurs during auscultation (listening), or the patient’s visit contains the above signs indicating problems with the heart, you must undergo:
- electrocardiogram (ECG);
- ultrasonography.
Read it! Myocardial dystrophy of mixed origin - what is it?
With a false chord in the left ventricle in a child or adult, an accurate diagnosis, as well as the location of the cord and possible danger, can only be determined by ultrasound.
In most cases, no special treatment is required, you just need to take control of your heart function and lead a healthy lifestyle. If the false chord causes discomfort or is accompanied by some characteristic signs, then drug therapy may be prescribed. It can be:
- vitamins (to improve nutrition of organ cells);
- antioxidants (for metabolism in cells);
- nootropic drugs (if a functional disease is detected).
Important! Surgical interventions are an extremely rare occurrence; they can only be indicated for a “hemodynamically significant” type of anomaly, and only if it interferes with the functioning of the organ.
Prevention and prognosis
There are no effective preventive measures. This is due to a genetic factor in the transmission of the disease. It would be useful to give up bad habits during gestation, provide proper nutrition to the pregnant woman, and transfer her to light work in safe conditions.
According to statistics, patients diagnosed with LVDC have a favorable prognosis. Over time, the body adapts to the existing anomaly of heart development. It does not manifest itself clinically and does not bother the patient. The situation is worse in those patients who have several additional chords or they are located transversely.
The additional chord in the cavity of the left ventricle does not threaten life. A child with such a diagnosis is able to grow and develop without strict restrictions. Treatment is required only if complications are detected. In other cases, it is enough to visit a cardiologist annually and perform echocardiography.
Prevalence and causes
Abnormal chord
The accessory chord, like the patent foramen ovale (POA), is a common minor anomaly of cardiac development in newborns. This is not a heart disease, but only a deviation in its development. This term means that this anomaly should not lead to heart failure. Since LVDC is most easily detected by ultrasound, appropriate conclusions can be drawn.
Scientists studying this issue have concluded that with cardiac ultrasound, the incidence can reach 22 percent. Although this indicator can vary significantly.
Most often, an additional chord is detected in childhood. What causes an anomalous left ventricular chord (LVAC)? Heredity plays the lion's share in this situation. If parents have this kind of heart anomaly, then there is a high probability that their child may also have LVDC. In addition to heredity, a number of factors also play a role in the development of this cardiac anomaly. The intrauterine period consists of certain time periods during which a particular system is especially vulnerable.
Causes of cardiovascular diseases
For the cardiovascular system, such a dangerous period is the 5-6th week of intrauterine development. Therefore, the expectant mother’s consumption of alcoholic beverages, smoking, drugs, excessive physical activity, stressful situations, weakened immunity, and exposure to radiation can play a negative role on the development of the cardiovascular system. On the part of the child, intrauterine infections can be a causative factor in the development of LVDC.