What is left ventricular overload?
Overload of the left ventricle usually develops after an acute situation: for example, running, especially over long distances, overtraining in athletes, physical overexertion, hypertensive crisis, a significant increase in blood pressure without clinical signs of hypertensive crisis, an attack of cardiac asthma, etc.
In these cases, the ECG in the left chest leads V5, V6 may show a decrease in the ST segment and flattening or negativity of the T waves (in the presence or absence of enlarged RV5, V6 waves). Then, as the patient’s condition normalizes, the ECG gradually returns to the original one. When these ECG changes appear, we can talk about left ventricular overload.
Right ventricular overload
ECG changes characteristic of right ventricular overload also usually appear after acute clinical situations, for example, during pneumonia, an attack of bronchial asthma, or more often during an asthmatic condition, acute pulmonary failure, pulmonary edema, acute pulmonary hypertension, etc.
In this case, the ECG may show a decrease in the ST segment and smoothness or negativity of T waves in the right chest leads V1, V2 (in the presence or absence of enlarged RVl, V2 waves). Sometimes these ECG changes are determined in leads III, aVF and II. Then, as the patient’s condition improves and the acute situation is eliminated, the ECG gradually normalizes. Repeated dynamic monitoring of the patient helps diagnose right ventricular overload.
“Guide to electrocardiography”, V.N. Orlov
This information is for your information only; please consult your doctor for treatment.
The term “overload” implies dynamic ECG changes that appear in acute clinical situations and disappear after the patient’s condition normalizes. ECG changes are usually in the ST segments and T waves.
Systolic overload (resistance overload) of the ventricles occurs when there is an obstacle in the way of expulsion of blood from the ventricles that impedes blood flow (narrowing of the outlet from the ventricle; increased pressure in the pulmonary or systemic circulation). In such cases, the ventricle contracts, overcoming external resistance in systole, and its hypertrophy develops (ventricular dilatation is mild).
Diastolic overload (volume overload) of the ventricle occurs as a result of its overflow with blood, and the ventricle is overfilled with blood in diastole with an increase in the amount of residual blood in it. The cause of diastolic overload is valve insufficiency or increased blood flow, resulting in an increase in diastolic filling and muscle fiber length, leading to increased contractions of the ventricle. With diastolic overload, dilatation of the ventricle mainly occurs (hypertrophy is mild).
Common causes of left ventricular systolic overload:
- aortic stenosis;
- hypertonic disease;
- symptomatic and arterial hypertension;
- coarctation of the aorta.
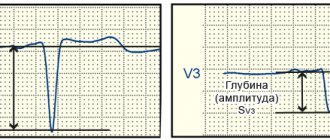
ECG signs of left ventricular systolic overload:
- qV5,V6 {amp}lt; 2 mm;
- high RV5,V6 {amp}gt; RV4 with deep SV1,V2;
- the STV5,V6 segment is located below the isoline, the TV5,V6 wave is negative (similar changes in the ST segment and T wave are usually observed in leads I, aVL);
- the activation time of the left ventricle in leads V5, V6 is increased and exceeds 0.04 s.
ECG signs of systolic overload of the right ventricle:
- high RV1,V2 (RV1 ≥ SV1), a high late R wave in lead aVR is often observed;
- the STV1,V2 segment is located below the isoline, the T wave is negative (similar changes in the ST segment and T wave are often observed in leads II, III, aVF);
- deviation of the electrical axis of the heart to the right;
- the activation time of the left ventricle in leads V1, V2 is increased and exceeds 0.03 s.
ECG signs of left ventricular diastolic overload:
- qV5,V6 {amp}gt; 2 mm, but less than a quarter of a tooth RV5,V6 and less than 0.03 s;
- high RV5,V6 {amp}gt; RV4 with deep SV1,V2;
- the STV5,V6 segment is located on the isoline or slightly higher, the TV5,V6 tooth is positive (often high and pointed).
A sign of diastolic overload of the right ventricle on the ECG is the appearance in leads V1, V2 of complete or incomplete blockade of the right bundle branch:
- The ECG looks like rsR' or rSR';
- The electrical axis of the heart is usually deviated to the right.
Left ventricular hypertrophy, or cardiomyopathy, is a very common heart disorder in patients diagnosed with hypertension. This is a rather dangerous disease, since its final stage is often death in 4% of all cases.
Heart overload
- Google+
Heart overload can occur when:
- increasing the amount of blood flowing to it, i.e. with increasing preload
(
volume overload
). Causes: physical work, heart defects accompanied by insufficiency of the heart valve apparatus, congenital defects of the heart septum;
- or when resistance to blood outflow increases, i.e. when afterload
(
pressure overload
). Causes: heart defects accompanied by narrowing of the atrioventricular orifice, pulmonary trunk or aorta, as well as hypertension, generalized atherosclerosis, pneumosclerosis.
Mechanisms of immediate (emergency) adaptation
heart overload (compensatory hyperfunction):
1) heterometric mechanism
(with volume overload - i.e. with increasing preload);
2) homeometric mechanism
(with pressure overload - i.e. with increasing afterload);
4) activation of sympathetic influences.
The efficiency of the contractile function of the heart is measured by the magnitude of cardiac output (CO
or the so-called
minute blood volume (MBV
), which is equal to stroke volume (
SV
) multiplied by heart rate.
SV=3.5-8.0 l/min
Under load, the tissue need for blood supply increases and the heart of a healthy body can increase CO by 3-4 times. Compensatory mechanisms when the heart is overloaded are aimed at ensuring cardiac output (CO) adequate to the body’s needs: hetero- and homeometric mechanisms provide optimal stroke volume, and tachycardia – heart rate.
Preload
determined by venous return to the heart and the length of myocardiocytes, which constitutes ventricular end-diastolic filling.
According to the Frank-Starling law: the greater the myocardial stretch, the greater the force of cardiac contraction ( heterometric
compensation mechanism).
Myocardial stretching - an increase in the length of myocardiocyte fibers - is a consequence of their stretching by the excess volume of blood in the cavities of the heart as a result of a decrease in its contractility. The resulting expansion of the cavities of the heart is accompanied by an increase in stroke volume and is called tonogenic dilatation
.
However, if the heart is overstretched so that actin and myosin cannot contract effectively, myogenic dilatation
, in which the increased blood supply to the heart is not accompanied by an increase in stroke volume and the Frank-Starling law does not apply here.
Afterload
- resistance to the expulsion of blood from the heart into the aorta and pulmonary artery.
Systemic blood pressure is the main source of afterload on the left heart, and pressure in the pulmonary circulation is on the right heart. Anything that prevents blood from being pumped out of the heart increases afterload. In this case, the homeometric
adaptation mechanism is activated - an increase in the force of heart contractions in response to increased load with a constant length of myocardial fibers (as opposed to heterometric) by increasing the magnitude and rate of development of muscle fiber tension. This compensation mechanism is more energy-intensive than the heterometric one and requires 10 times more oxygen.
Tachycardia-
an increase in heart rate of more than 80 per minute. A number of factors play a role in the development of tachycardia:
1 Bainbridge reflex with congested vena cava;
2. Reflex from the aortic arch and carotid sinus when blood pressure drops;
3. Increased levels of catecholamines in the blood.
There is a dependence of the IOC on the heart rate (see figure). An increase in heart rate to 100 - 120 per minute is accompanied by an increase in IOC, and above 120 beats per minute - IOC decreases. For children, these indicators are different. IOC begins to decline in infants when the contraction is above 180 beats per minute and 150 beats per minute in young children.
The main supply of energy and plastic material and oxygen to the heart muscle occurs in diastole. With tachycardia, systole time increases and diastole decreases, which leads to ATP deficiency in the heart muscle, poor energy recovery and dystrophy.
Let's take an example to see why tachycardia, being a compensatory, adaptive sign, is included in the pathogenesis of heart failure. At rest, the cardiac cycle lasts -0.85 seconds, systole - 0.35 seconds, diastole - 0.5 seconds. Under these conditions, the diastole period of 1 minute lasts 35 seconds, and the systole period lasts only 24 seconds. At 180 beats per minute, the cardiac cycle lasts 0.35 seconds, systole - 0.2 seconds, diastole -0.13 seconds, that is, the diastole period per minute is 24 seconds, the systole period per minute is 36 seconds. As a result of a decrease in diastole, the time of blood flow to the heart muscle decreases, its nutrition is disrupted, and the efficiency of the heterometric compensation mechanism decreases. Relative malnutrition leads to myocardial dystrophy as a result of ATP deficiency and poor energy recovery.
Bradycardia-
decrease in heart rate less than 60 per minute.
During hypertensive crises, baroreceptors located in the aortic arch cause a reflex slowdown of the heart rate in response to high pressure. With bradycardia, diastole time lengthens and, in accordance with the Frank-Starling mechanism, greater blood flow to the ventricle and increased stretching of myofibrils should lead to cardiac output. Studies have shown (Mukharlyamov N.M. et al., 1982) that increased cardiac output in healthy people is observed when myocardial fibers are stretched only to 146% of the original value. A volume study showed that when the left ventricle is filled by more than 20%, it is also not accompanied by an increase in cardiac output, and not all the blood enters the aorta during systole; a significant residual volume of blood remains in the ventricle.
Activation of sympathetic influences
on the heart provides a positive inotropic effect. The frequency of spontaneous depolarization of pacemaker membranes increases, impulse conduction in Purkinje fibers is facilitated, and the frequency and force of contraction of typical cardiomyocytes increases.
Mechanisms
of long-term adaptation of the heart to overload (compensatory hypertrophy).
With prolonged stress on the heart, for example, with prolonged physical activity, with heart defects, hypertension, etc. long-term adaptation mechanisms are activated
hearts to overload. They are represented by myocardial hypertrophy. To increase the load on an organ, the organ tissue responds with either hyperplasia or hypertrophy. Muscle tissue does not divide, so cardiac tissue can only hypertrophy.
There is a physiological
and
pathological
myocardial hypertrophy. Physiological hypertrophy plays an adaptive role.
Physiological hypertrophy should be considered an increase in the heart muscle, which is accompanied by an increase in mitochondria (qualitatively and quantitatively), the vital activity apparatus of the myocardiocyte, an increase in the circulatory apparatus and innervation of the heart.
Under experimental conditions, increased physical activity for 2-4 days leads to an increase in proteins in the heart muscle by 20-70%, that is, the volume of myofibrils increases, but there is no increase in blood vessels and nerves. As a result of a lack of trophism, myofibrils degenerate, dystrophic processes develop in them, and absolute and relative insufficiency of blood supply to the heart muscle. myogenic dilatation develops
. Myogenic dilatation occurs as a result of pathological hypertrophy of the heart muscle.
Consequently, the development of physiological and pathological hypertrophy lies in the development of the cell’s life support apparatus, the ratio of the area of myofibrils and the number of vessels and nerves per unit volume of myofibrils.
If a person leads a sedentary lifestyle, detraining of the heart muscle occurs. The myocardium is not prepared for physical activity. Under conditions of increased physical activity, in conditions of a previously detrained heart, pathological hypertrophy quickly develops.
Detraining of the heart muscle begins to form from birth and is associated with limited mobility of the child (prams, limited outdoor play, limited living space, etc.). Later, already as an adult, in the conditions of city life a person becomes a slave to inactivity: at home in front of the TV, in a chair at work, moving with the help of vehicles. This explains the need for active, daily physical activity in the prevention of heart failure.
Back in the 30s A.B. Vogt showed how greatly the capabilities of a trained and detrained heart differ when a provoked increase in its work occurs.
Experience of Vogt A.B.
One group of puppies was given dosed physical activity, the other led a free lifestyle without dosed physical activity. Aortic stenosis was created in both groups of puppies. In trained puppies, heart function increased 10 times or more, and under experimental pathology conditions, decompensation did not occur. In untrained puppies, the work of the heart increased 5-6 times and they quickly decompensated. Experiments by A.B. Vogt illustrate that physiological hypertrophy largely determines the outcome of cardiac pathology.
Creating physiological hypertrophy is also possible in a diseased heart with a clearly planned therapeutic load. In this case, one must adhere to the rule: a person with a heart disease should rest so as not to get tired, while a healthy person should rest when he gets tired.
When assessing the biological significance of myocardial hypertrophy, attention should be paid to the internal inconsistency of this phenomenon. On the one hand, this is a very perfect adaptive mechanism that ensures the heart performs increased work for a long time under normal and pathological conditions, and on the other, the structural and functional features of the hypertrophied heart serve as a prerequisite for the development of pathology. The predominance of one of the parties in each specific case determines the characteristics of the pathological process.
Circulatory failure due to heart defects.
Let us consider hemodynamic disturbances in heart failure arising from acquired defects
hearts, which are most often the result of rheumatism or endocarditis.
In addition to acquired ones, there are congenital
heart defects that arise during intrauterine development.
Left ventricular failure
.
Let us examine the pathogenesis of circulatory failure using the example of stenosis of the left atrioventricular orifice, mitral valve insufficiency and aortic valve insufficiency.
With these defects, so-called left ventricular failure occurs,
when the left parts of the heart cannot fulfill the load required of them.
Stenosis of the left atrioventricular orifice
The flow of blood into the left ventricle is disrupted. The left atrium is filled with blood. The left ventricle pumps little blood into the aorta. Small output syndrome develops
. The pressure in the systemic circulation drops, which is accompanied by the release of blood from the depot. Hypervolemia (plus decompensation) is created, venous return increases without adequate cardiac output.
Blood retention due to stenosis of the atrioventricular orifice is accompanied by an increase in pressure in the left atrium, which leads to increased work. The atrial muscle is very weak and the primary tonogenic dilatation is replaced by myogenic dilatation. There is stagnation and increased pressure in the pulmonary veins. The latter extends all the way to the capillaries, since the pulmonary veins do not have valves. Under these conditions, significant amounts of blood can accumulate in the lungs.
As soon as the pressure in the capillary network of the lungs reaches 25-30 mm Hg. Art. (normally 6-12 mm Hg), vascular permeability increases sharply and pulmonary edema
. At the same time, a small amount of physical or emotional stress is enough to increase blood pressure.
However, there are a number of compensatory mechanisms that prevent the development of pulmonary edema. With increased pressure in the pulmonary veins and left atrium: 1)
the anastomoses between the veins of the pulmonary and systemic circulation (between the pulmonary and bronchial veins) expand compensatoryly.
Part of the blood flows through the bronchial veins into the superior vena cava and enters the right atrium. Since a large number of anastomoses pass under the bronchial mucosa, it swells, varicose veins appear, and an increased bronchial pattern appears on the radiograph. Rupture of thinned, dilated veins often leads to hemoptysis of scarlet blood. Cells of cardiac defects
appear alveolar macrophages filled with hemosiderin;
2)
Kitaev reflex
also prevents blood stagnation in the pulmonary veins . It protects the capillary network of the lungs from overflowing with blood, although it does not completely relieve the increased pressure in the pulmonary veins and left atrium.
Prolonged spasm of the pulmonary arterioles creates resistance to blood flow in the pulmonary bed, blood pressure in the pulmonary artery increases - hypertension of the pulmonary circulation
.
Subsequently, spasm of the pulmonary arterioles turns from a functional obstacle to blood flow into an organic one, since prolonged vascular spasm disrupts the nutrition of its walls. The walls of arterial vessels become denser, sclerosed, and a persistent irreversible barrier to the movement of blood appears. He calls it the “second barrier” - morphological
, the “first barrier” -
functional
.
The function of external respiration is also impaired. Stagnation of blood in the lungs, in addition to changes in the vessels and bronchi, is accompanied by a decrease in the elasticity of the lung tissue, which in turn leads to a decrease in vital capacity. This also aggravates the appearance of shortness of breath in heart failure, since there is poor oxygenation of the blood (thickening of the walls of the alveoli, slowing of blood flow, poor ventilation of the lungs. When vital capacity decreases to 30-60%, shortness of breath occurs at the slightest exertion.
The emergence of a “second barrier” protects the lungs from edema, while the load on the right ventricle sharply increases, its work sometimes increases by 8-10 times. An increase in resistance to blood flow in the pulmonary bed and increased work of the right ventricle is accompanied by its tonogenic hypertrophy and subsequent myogenic dilation, relative insufficiency of the tricuspid valve, which leads to an increase in pressure in the right atrium (2-3 times) and the development of right ventricular failure.
Mitral valve insufficiency
The leading factor in the pathogenesis of circulatory disorders in mitral insufficiency is regurgitation
(throwing) blood from the left ventricle into the left atrium, which significantly increases the work of the heart to maintain normal blood circulation. Example: stroke volume 60 ml, return 30 ml. In the subsequent atrial systole, 90 ml of blood enters the ventricle, but 30 ml returns to the atrium. Thus, the work of the heart increases by 1.5 times.
Increased pressure in the left atrium leads to the manifestation of the Kitaev reflex
, development of hypertension of the pulmonary circulation. Further development of hemodynamic disturbances in the pulmonary and systemic circulation develops according to a mechanism similar to stenosis of the left atrioventricular orifice. Manifestations of decompensation occur as a result of right ventricular failure and are caused by blood stagnation and increased pressure in the venous system of the systemic circulation.
Treatment of left ventricular hypertrophy
Blockade on ECG
- negative tooth value;
- doublings (two parts of one tooth);
- the first half “looks” down, and the second half looks up.
A slight displacement of the S-T segment up or down relative to the horizontal line is a sign of thickening of the walls of the left ventricle. Significant displacement is an indicator of myocardial infarction or ischemic heart disease (coronary heart disease).
The S-wave in the presence of a hypertraffiated ventricle changes as follows:
- in leads: III, AVF, V1, V2 – increased depth of the tooth;
- in leads: AVL, V5, V6, I – weakly expressed;
- jaggedness is observed.
Deviations from the norm of the parameters of the Q, R, S waves are called the voltage of the cardiogram. If the teeth are located below normal by more than 0.5 mV, a low-voltage potential will be recorded on the cardiogram. Voltage changes always indicate the presence of cardiac pathology.
Electrocardiogram of the heart with LVH (signs of pathology are circled in red)
Left ventricular hypertrophy detected during an ECG means the presence of excessive load on the heart and myocardial diseases:
- narrowing of the aortic lumen in the valve area (aortic stenosis). Due to the transformation of the valve leaflets, blood flow is disrupted, and the heart is forced to work in emergency mode;
- change in the volume of the left ventricular wall towards thickening (hypertrophic cardiomyopathy). The thickness of the walls impedes blood circulation, which increases the load on the myocardium;
- persistently high blood pressure (hypertension).
Deformation can occur due to reasons that depend directly on the patient himself. First of all, these are the following factors: eating habits leading to obesity, irrational physical activity. LVH is common to many athletes, since excessive load on the heart during training provokes an increase in the volume and mass of the organ, systematic psycho-emotional overload (state of stress), and an unhealthy lifestyle (smoking, alcohol, lack of fresh air, unhealthy foods).
In addition, the culprit of ventricular pathology may be a hereditary predisposition or a congenital anatomical anomaly. In patients aged 65, the cause is often atherosclerosis.
Thickening of the heart syndrome can be caused by problems such as:
- Hypertension – in 90% of cases in people suffering from arterial hypertension.
- Heart defects – both congenital and acquired.
- Excessive physical activity.
- Diabetes.
- Excess body weight.
- Psycho-emotional unstable states – stress, anxiety, excitement, etc.
- Sedentary lifestyle.
- Heredity.
- Bad habits – alcoholism, smoking, drug addiction.
Therapy for LVH comes down to three points:
- Eliminate the symptoms of the problem.
- Improved health.
- Prevention of relapse and progression of the disease.
Since in most cases LVH is a consequence of arterial hypertension, then, under the supervision of a doctor, the patient is prescribed the following medications that can normalize his condition:
- ACE inhibitors - tablets "Lisinopril", "Quadripril" and others. These medications improve blood pressure, and if you take them for a long time (at least six months), you can achieve normalization of myocardial wall thickness.
- Beta blockers - drugs Metoprolol, Bisoprolol. These tablets reduce the load on the heart and reduce the heart rate.
- Products based on nitroglycerin. They are able to dilate myocardial vessels, thereby reducing the load on the muscle.
If the cause of wall thickening is a heart defect, then the pathology should be eliminated through surgery. In this case it can take the form:
- Aortic stenting.
- Prosthetics (heart transplant).
- Removing part of the muscle that blocks blood access to the aorta.
Home methods only deal with LVH that was caused by hypertension. You need to resort to non-traditional remedies after receiving doctor's approval.
Among the traditional methods, the following recipes can be distinguished:
- Medicine from St. John's wort - 2 liters of water per 100 g of dry herb. Boil the raw materials and simmer for 10 minutes. Infuse, add honey (200 g). Take 2 tablespoons per day for a month. St. John's wort calms, cleanses blood vessels, prevents arrhythmia.
- Cranberry slurry. Grind fresh berries with honey or sugar. Take 1 tbsp. l. after meal. Cranberry improves blood flow, restores the elasticity of blood vessels, reduces blood pressure, and has a general strengthening effect. It is advisable to make the paste daily to take the medicine fresh.
- Garlic based product. Grind the peeled cloves in a garlic press. Add honey (1:1 ratio). Leave to infuse in a dark place for 5–7 days, periodically shaking the contents of the jar. Take a tablespoon three times a day. Regular intake of garlic cleanses and strengthens blood vessels, helps eliminate arrhythmia, and is useful for hypertension and heart failure.
- Decoction of blueberry shoots. Mix 10 g of raw material with 250 ml of water. Boil for 10 minutes, cool, strain. Take a tablespoon before each meal.
The human heart muscle is a unique complex of cells that are capable of transforming energy obtained as a result of biochemical processes into mechanical energy that causes contractions of the heart.
This type of activity depends on many factors contributing to intracellular metabolism in the myocardium. Therefore, any changes in the constancy of the internal environment of the body can be reflected in disruption of the vital activity of heart cells, be it heart disease, hormonal imbalance in the body, or a condition after an infectious disease.
Diffuse changes in the myocardium are not a disease, but a syndrome, upon detection of which the doctor should determine whether the cause was a serious illness or minor metabolic disorders. The occurrence of such signs is due to the fact that some cells, due to biochemical changes, begin to work and contract not quite correctly, as a result of which the electrical activity of the areas of the heart muscle recorded on the ECG will not be uniform. In other words, diffuse changes in the myocardium are accumulations of altered cells through which the conduction of electrical impulses is impaired.
Disturbances in cell activity can be not only diffuse, that is, covering areas throughout all parts of the heart, but also focal, for example, with the formation of small or large scars in the myocardium. Scars are represented by connective tissue that cannot conduct impulses and is electrically inert, which is what the doctor sees on the cardiogram.
The reason for such deviations on the cardiogram can be both harmless and quite serious, posing a threat to human life. In order to find out more precisely what exactly causes diffuse or focal changes in the myocardium, it is necessary to carefully examine the patient. Pathological changes in the myocardium can be caused by various processes, and therefore several subgroups are distinguished among them.
The causes of inflammatory changes are myocarditis - infectious or aseptic (without the participation of microorganisms) inflammation of the heart muscle. As a rule, areas of inflammation are located diffusely, but can also occur in the form of foci.
Myocarditis of varying severity occurs in diseases such as:
- Acute rheumatic fever (rheumatism), caused by hemolytic streptococci due to tonsillitis, scarlet fever or chronic tonsillitis,
- Diphtheria, typhus,
- Influenza viruses, measles, rubella, Coxsackie, etc.
- Autoimmune diseases, for example, systemic lupus erythematosus, rheumatoid arthritis with heart damage, etc.
Dystrophic changes in the myocardium are characterized by metabolic and functional disorders in cardiac cells caused by non-inflammatory and non-coronarogenic (not caused by damage to the coronary arteries) diseases. Literally, this means that myocardial cells lack nutrients to carry out their vital functions, which leads to their heterogeneous contraction. This condition is otherwise called cardiac dystrophy. This condition may occur in the following cases:
- Severe dysfunction of the liver and kidneys with the development of failure of these organs, as a result of which toxic metabolic products accumulate in the blood,
- Diseases of the endocrine organs - diabetes mellitus, adrenal tumor, hyperfunction of the thyroid gland, as a result of which excess hormones or insufficient absorption of glucose by heart cells lead to disruption of intracellular metabolism,
- Constant stress, exhausting physical activity, malnutrition and starvation, chronic fatigue,
- In children, in addition to the previous reason, increased emotional and mental stress in the absence of sufficient mobility can lead to changes in the myocardium, as a result of which vegetative-vascular dystonia and disturbances in cardiac regulation from the nervous system develop,
- Anemia – a decrease in hemoglobin in the blood and, as a result, oxygen starvation of myocardial cells,
- Acute and chronic infectious diseases (influenza, malaria, tuberculosis),
- Fever and dehydration,
- Lack of vitamins in food,
- Acute and chronic intoxications - alcoholism, occupational poisoning with chemicals, etc.
Metabolic changes in the myocardium are caused by disruption of repolarization processes in muscle cells. Depolarization and repolarization are subtle mechanisms for the exchange of potassium and sodium ions within each cell, the energy generated during which is converted into the energy necessary for contraction and relaxation of the cell. When the electrolyte composition in the blood and heart muscle is disturbed, a change in the metabolism of muscle cells occurs. Sometimes such abnormalities in the ECG conclusion are formulated as nonspecific changes in the myocardium.
In addition to conditions that can provoke myocardial dystrophy, this can be caused by atherosclerosis of the coronary arteries and coronary heart disease, arterial hypertension, heart rhythm disturbances, and myocardial hypertrophy. That is, those conditions in which the heart does not receive enough nutrients and microelements.
Causes of heart strain in sports and methods of prevention
1. It is IMPORTANT to emphasize the main idea here: the main cause of chronic overstrain of the cardiovascular system (CVS) is physical activity of significant volume and intensity. [2] That is incorrect, “greedy” planning of training progress leads to cardiovascular pathology. In the context of bodybuilding, this takes on increased relevance! Due to the fact that one of the main goals of BB is mass gain, other systems of the body, especially the heart, simply do not keep up with the super-intensive growth of mass and in fact pathological adjustments of these organs to the inflated demands of mass appear. Numerous examples of deaths caused by the failure of the cardiovascular system, both among current bodybuilders and among former, but not yet old, bodybuilders, confirm this. Therefore, the main message of this point is that if the goal is to weigh a lot, then this must be done gradually, without extreme weight increases of tens of kilograms!
2. Illness, cold, flu, inflammation...training against the background of illness is strictly not recommended. [1,2] The adaptive forces of the body in such conditions are sharply reduced, oxidative stress is increased, and the load on the heart increases many times over. If you try to maintain training intensity against this background, it will be very easy to get cardiac overstrain. The best option is to take a break, lie down and “get sick.” As a last resort, the intensity of training should be sharply reduced - classes during this period should be considered only as physical therapy (physical therapy).
It is also necessary to strictly monitor chronic diseases. Sports medicine here pays attention to diseases of the oral cavity that can occur in an indirect form, such as tonsillitis, periodontitis, and root cysts. [2] Inflammatory factors from such foci can drain into the blood, reducing both immunity and the activity of myocardial antigens.
3. Psycho-emotional stress. The banal recommendation to be less nervous is, in fact, quite justified in its relevance. Information and communication stress, which creates the background for the development of psycho-emotional disorders, causes overstrain of the psyche and neuroendocrine system, thereby disrupting the regulation of the cardiovascular system. [2] The athlete’s exposure to any traumatic factors must be limited as much as possible.
4. Bad habits. In particular, smoking is one of the most common causes of coronary heart disease. It provokes vasospasm and thus increases blood pressure. The negative effect on the body increases many times over if it is combined with an increase in cholesterol in the blood.
5. Hypertension. This partly echoes the first point and a prerequisite for hypertrophy will be excess body weight. This pathology will be enhanced by problems of insufficient local (capillary) blood supply. Therefore, high-repetition approaches with light weights (such as the Cutting program), as well as cardio training, should be present in training programs to improve local blood supply to the muscles.
Clinical signs
Signs of left ventricular hypertrophy are absent for a long time. Symptoms appear only when a person cannot compensate for the resulting changes in blood circulation. Concentric hypertrophy of the left ventricular myocardium can be manifested by the following symptoms:
- dizziness;
- pain in the heart;
- shortness of breath;
- swelling of the lower extremities;
- sleep disturbance;
- decreased ability to work;
- weakness;
- feeling of a sinking heart;
- fainting;
- lability of blood pressure;
- heart rhythm disturbances such as atrial fibrillation or extrasystole.
Most of these patients experience pain in the heart area similar to angina pectoris. Increased blood pressure is common. A typical manifestation of myocardial hypertrophy is shortness of breath. In the early stages it bothers you when working, and then appears at rest. In severe cases, cardiac asthma develops. Many patients are bothered by periodic attacks of suffocation.
Acrocyanosis (blue discoloration of fingers, nose, lips) is possible. All these symptoms are caused by the underlying disease, which led to left ventricular hypertrophy. If the cause is hypertrophic cardiomyopathy, then the outcome of such a pathology can be non-violent death due to sudden cardiac arrest.
According to statistics, LVH is more common in elderly patients (over 60 years of age), but with some heart diseases it is observed in adulthood, childhood, and even during the neonatal period.
You can suspect the presence of left ventricular hypertrophy based on the following signs:
- pain in the heart, it can have a different nature and duration;
- dizziness and weakness;
- shortness of breath;
- a feeling of sudden sinking of the heart, followed by a strong palpitation;
- repeated fainting;
- swelling of the limbs;
- sleep disturbance;
- physical inability to do heavy work.
It is worth noting that in half of patients, hypertrophy can occur unnoticed at first, this is especially true for athletes.
The problem with hypertrophy is that it has no symptoms. Doctors may suspect the disease based on the following symptoms:
- feeling of suffocation;
- fainting;
- dizziness;
- insomnia;
- fluttering heart syndrome;
- pain in the left side of the chest - pinching, squeezing, squeezing, etc.;
- severe fatigue with previous active physical activity;
- pressure changes;
- migraine;
- accumulation of fluid in the lower extremities (edema);
- dyspnea.
Indirect signs of LVH of the heart are those indicators that are visible using instrumental research methods with an ECG. These include: disturbance of intraventricular conduction, repolarization phases, decrease in the amplitude of the T wave.
Signs of heart strain and its consequences
Dysfunctions of the heart are observed in most cases in the discrepancy between the amount of Oxygen it requires and the amount it receives. When the oxygen content decreases, it is no longer oxygen, but energy starvation. [1] The heart is not able to produce the required amount of ATP and, accordingly, is not able to carry out the required stroke volume of its work. The so-called cardiac overstrain, the symptoms of which will be:
- a sharp decrease in performance,
- weakness, increased sweating,
- shortness of breath, feeling that there is not enough oxygen, cough,
- rapid heartbeat, irregular heart rhythm (arrhythmia),
- chest pain, nausea, vomiting.
The general state of oxygen deficiency is called hypoxia. The causes of cardiac hypoxia can be various factors. In particular, in clinical practice, the most common diagnosis of cardiac hypoxia is myocardial ischemia, in which the lumen of the coronary vessels supplying the heart muscle decreases, and the cause of this condition in most cases is atherosclerosis of the arteries.
In sports practice, cardiac hypoxia occurs due to an increase in oxygen demand by all organs, primarily muscles. At the same time, the heart begins to experience oxygen deficiency, as a result of which cardiac functionality undergoes changes:
- Firstly, as mentioned above, the production of ATP molecules is reduced. In order to compensate for this dysfunction, the heart increases heart rate. Due to this, the amount of circulating blood increases and the amount of oxygen flowing through this blood also increases. However, heart rate has its own limit; for young and healthy athletes it is 200 beats/min, which is not recommended for other athletes. In addition, high heart rate is a state of cardiac overstrain, which must be clearly controlled in order to avoid irreparable pathological cardiac changes. [2] And this rule must be followed by all athletes, regardless of age and training.
“Secondly, the result of inadequate oxygen supply to tissues will be mitochondrial dysfunction, which will be manifested by phase fluctuations in the activity of mitochondrial enzymatic complexes. [2] This will lead to suppression of aerobic ATP synthesis. At the same time, the rate of formation of free radicals (FR) will increase, and the power of certain segments of the antioxidant system will decrease. A steadily increasing amount of reactive oxygen species (aka RO) and other toxic waste products will lead to the formation of oxidative stress, which is the cause of most cardiovascular diseases.
Left ventricular myocardial hypertrophy (LVH): causes, signs and diagnosis, how to treat, prognosis
Before making a diagnosis of LVH, the cardiologist at the initial appointment should:
- Interview the patient - find out what complaints he has, what he does, whether he leads an active lifestyle, whether he has any bad habits, etc.
- Perform an examination using palpation, establish the boundaries of the heart, their displacement, find out the width of the vascular bundle, etc.
- Listen to the patient, determine breathing disturbances, increased or muffled “engine” sounds.
An electrocardiogram is one of the most common diagnostic methods. The ECG determines the thickness of the myocardium, as well as pronounced signs: cardiac output, pressure gradient, etc. However, LVH of the heart on the ECG does not provide an absolute guarantee when making a diagnosis, because general signs may also be characteristic of a healthy person.
More extensive and in-depth analysis of the heart muscle. With its help, you can determine how thick the myocardium and its septa have been, which areas are observed with reduced contractility, and the general condition of the heart muscle.
This is echocardiography with the Doppler effect, thanks to which you can determine the speed and direction of blood through the vessels. With its help, a specialist can see the shape and size of the cavities of the heart, the functioning of the heart valves, and assess the contractility of the myocardium.
This is an accurate research method, thanks to which a specialist has the opportunity to obtain high-resolution images, assess myocardial contractility, and make a final diagnosis. Using MRI, the doctor can conduct dynamic observations of the patient’s health status during drug treatment or analyze the results of surgery.
To assess the work of the myocardium, a specialist can prescribe tests to the patient with changes in body position, atmospheric pressure, ambient temperature, and others.
Depending on the patient’s condition, diagnostic methods can be supplemented with coronary angiography, fluorography, etc.
Genetic testing is performed to exclude hereditary forms of HCM.
To clarify the stage of the disease, markers of chronic heart failure are examined.
Of the instrumental studies, the following are mandatory:
- LVH on ECG,
- daily ECG monitoring,
- transthoracic resting cardiography (ECHO-CG) and stress ECHO-CG,
- tissue Doppler study.
Echo-KG allows you to evaluate:
- location of the site of myocardial hypertrophy,
- wall thickness,
- LV ejection fraction,
- dynamic obstruction,
- condition of the valve apparatus,
- volume of the ventricles and atria,
- systolic pressure in the LA,
- diastolic dysfunction,
- mitral regurgitation, etc.
Chest x-ray allows you to assess the degree of left ventricular enlargement.
If necessary, MRI and CT of the heart are performed.
To identify atherosclerotic changes in the coronary vessels, coronary angiography is performed.
A consultation with a neurologist and an ophthalmologist is recommended in order to exclude the neurological nature of the complaints and consultation with an endocrinologist (excluding diabetes mellitus, thyrotoxicosis, etc.).
Chronic heart strain[edit | edit code]
In the occurrence of chronic physical overstrain, the leading role belongs to the toxic-hypoxic effects of catecholamines, electrolyte-steroid and hormonal disorders, and neurovegetative disorders. Chronic overexertion leads to the development of myocardial dystrophy (secondary cardiomyopathy, VCMP, metabolic cardiopathy).
The increase in the incidence of myocardial dystrophy, especially in child athletes, in recent years can be associated with a significant increase in both the volume and intensity of training loads without sufficient consideration of their individual tolerance. Other causes of myocardial dystrophy in children may be an incorrect combination of training and rest: highly specialized sports training, playing sports during an illness, or an insufficient break from sports activity after recovery.
Myocardial dystrophy is found in 14-35.7% of children involved in sports (Butchenko et al. 1980). Its main manifestations are weakening of the heart sounds, expansion of the boundaries, noise, additional tones, corresponding changes in the ECG (impaired conduction processes, excitability, repolarization processes, etc.).
The state of the cardiovascular system after stopping training[edit | edit code]
Changes in the activity of the heart associated with its adaptation to physical activity persist for 4-8 years after the cessation of sports activity (Myravama. Kuroda. 1980). Usually, after four years, bradycardia disappears, and the size of the heart returns to normal. In 95% of cases, atrioventricular block disappears, in 40% - incomplete blockade of the right bundle branch.
However, there is evidence that in former athletes who stopped active participation after completing their sports career, age-related degenerative changes (atherosclerosis, etc.) can develop even faster than in peers who have never played sports (Dembo, 1980).
In the work of V.M. Zatsnorsky (1988) contains generalized data from foreign studies on this problem. In particular, one of the American authors found that during the century (from 1828 to 1928) the mortality rate among rowing athletes was significantly lower than the national average. According to another study, the average life expectancy of student rowers was 67.9 years, while that of their university classmates was only 61.6 years. Particularly interesting is the work of Karvonen (cited by V.M. Zatsiorsky), which analyzed the life expectancy of 396 Finnish cross-country champions who were born between 1845 and 1910. and continued active pursuits into old age. Their average life expectancy was 73 years - 4.3 years more than the male population of Finland. A more recent study, which lasted for 20 years (a group of 600 men aged 45-64 years), showed that life expectancy in people with high physical activity was on average 2.1 years longer than in sedentary ones - due to reducing the incidence of heart attack deaths. The author concludes that a high level of physical activity can prevent premature death from heart attack, but cannot increase maximum life expectancy. As the famous American cardiologist Professor White said, “if we cannot add years to our lives, then we will add life to our years.” And this is not so little.
Stages of myocardial dystrophy in athletes according to electrocardiographic signs (L.A. Butchenko, 1984)
| Electrocardiographic signs of repolarization disorders | Reversibility of changes | |
| Spontaneous during follow-up (without treatment) | Reactions to pharmacological and stress tests | |
| Stage I | ||
| Decrease in T wave amplitude; isoelectricity of the T wave; TV1 > TV6 syndrome; flattening of the top of the T wave; central T wave inversion; terminal flattening and terminal isoelectricity of the T wave; oblique (ascending) upward displacement of the ST segment; enlargement of the U wave All changes are detected in at least two leads | Severe, often observed lability of ECG indicators with normalization and recurrence of ECG changes | a) normalization; b) lack of effect or temporary transition to stage II-III |
| Stage II | ||
| Terminal T wave inversion (in several leads); initial T wave inversion (in several leads); complete inversion of the T wave (no more than two leads); pathological downward displacement of the ST segment; T wave enlargement | Transitions to stage 1 are possible, sometimes normalization (partial) | a) transition to stage 1 or normalization; b) lack of effect or temporary transition to stage III |
| Stage III | ||
| Complete T wave inversion in many leads; pronounced ST segment displacement in many leads; syndrome simulating acute coronary insufficiency (severe ST segment elevation with terminal T wave inversion); U wave enlargement | Absent; insignificant (within the same stage) | a) temporary transition to stages II and I; b) lack of effect, deepening of violations |
Why is hypertrophy of the left ventricle of the heart dangerous?
The left ventricle is responsible for oxygen saturation and movement of arterial blood into the aorta and further through all small vessels to nourish the organs. As the volume increases, the blood presses on the walls, the connective tissue displaces the muscle tissue, and the ventricle ceases to cope with its functional duties.
Pathology can even lead to death
What such changes threaten is determined by the following diagnoses:
- coronary heart disease - a violation of the blood supply to the heart due to thickening of the walls of the gastric chamber;
- myocardial infarction – death (necrosis) of part of the heart muscle;
- ventricular extrasystole (arrhythmia) – failure of the heart rhythm;
- atrioventricular or ventricular block - cessation of the passage of electrical impulses between the atria and ventricles, leading to hemodynamics;
- heart failure is a low contractility of the heart muscle, often leading to death.
Timely detection of LVH will help prevent serious complications. The most informative in terms of diagnosing pathology is the electrocardiographic examination method.
When hypertrophy of the left ventricle of the heart develops, the nutrition of the organ is disrupted, and zones of abnormal hyperactivity and bypass conduction form. As a result, arrhythmia is observed, and due to an increase in the volume of the heart muscle and impaired blood flow in the vessels, ischemia and tissue necrosis occurs. Moreover, if for other reasons there is a deficiency of oxygen, the situation worsens.
Hypertrophy of the left ventricle of the heart can have critical consequences during sudden intense load on the myocardium, especially for inactive people and those who smoke or drink alcoholic beverages. There is a high risk of coronary artery disease, myocardial infarction, congestive heart failure, cerebral stroke, and sudden cardiac arrest.
When evaluating an electrocardiogram or performing an ultrasound of the heart, left ventricular hypertrophy is often detected. This is a condition characterized by an increase in the volume of muscle fibers. Isolated hypertrophy in the absence of heart failure is not dangerous to human health.
In cases where minor LV hypertrophy is diagnosed in the early stages, and the underlying disease is treatable, complete cure of hypertrophy has every chance of success. However, with severe heart pathology (extensive heart attacks, widespread cardiosclerosis, heart defects), complications may develop.
Such patients may experience heart attacks and strokes. Long-term hypertrophy leads to severe CHF, with swelling throughout the body up to anasarca, with complete intolerance to ordinary household stress. Patients with severe CHF cannot move around the house normally due to severe shortness of breath; they cannot tie their shoelaces or prepare food. In the later stages of CHF, the patient is unable to leave the house.
Prevention of adverse consequences is regular medical monitoring with ultrasound of the heart every six months, as well as constant use of medications.
With left ventricular hypertrophy, the structure and function of the heart changes. An enlarged left ventricle may:
- weaken the force of your contractions;
- lose elasticity, which interferes with the proper filling of the ventricle with blood and increases pressure in the heart;
- compress the coronary arteries that supply blood to the heart itself.
Acute cardiac overstrain[edit | edit code]
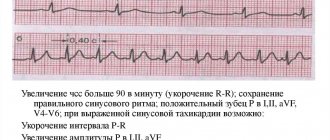
This is a pathological condition of the heart that occurs acutely when the functional capabilities of the body do not correspond to the physical activity performed. In severe cases of cardiac overstrain, acute heart failure occurs, leading to sudden death. In mild cases, the so-called heart strain syndrome is formed. This term reflects an electrocardiographic phenomenon: without a clinical picture of coronary insufficiency, a displacement of the ST segment downward with a convexity upward and inversion of T waves in the precordial leads are determined.
In severe cases, with physical overexertion, acute coronary circulatory failure may develop due to the fact that the amount of blood passing through the coronary arteries becomes insufficient to satisfy the oxygen demand of the heart muscle.
Excessive exercise may itself be a cause of sudden death in training or competition. It is usually associated with acute myogenic dilatation, depletion of the energy potential of the muscle cell. Arrhythmogenic death is possible due to ventricular fibrillation due to hypercatecholaminemia. In such cases, ruptures and contractures of muscle fibers, hemorrhages into the heart muscle are histologically determined.
Immediately after sports training, especially intense, phase syndrome of acute myocardial fatigue develops. It is characterized by prolongation of not only the isovolumic contraction phase, but also the expulsion period. The detection of this syndrome long after intense sports training indicates severe myocardial fatigue.
The main cause of sudden death during physical activity is cardiac arrhythmia, the occurrence of which may be associated with excessive stimulation of the sympathetic-adrenal system and reduced tone of the parasympathetic nervous system. Excessive release of adrenaline is accompanied by an increase in heart rate due to stimulation of beta-adrenergic receptors of the heart. The consequence of stimulation of beta-adrenergic receptors is a change in ionic homeostasis in myocardiocytes, accompanied by an increase in the entry of calcium ions into the cell and a decrease in potassium ions in it, which leads to disruption of the formation of the membrane potential and, accordingly, to the development of electrical inhomogeneity of the myocardium, which is accompanied by the development of arrhythmias. The development of sudden death may be preceded by ventricular tachycardia, turning into ventricular fibrillation. Sometimes the cause of these heart rhythm disturbances is an increase in cellular ionic imbalance associated with the loss of electrolytes (primarily potassium and magnesium ions). Sudden death was most often observed directly during marathon running or race walking competitions or immediately after the finish.
It is known that in untrained individuals, cardiac arrest as a result of ventricular fibrillation during physical or emotional stress occurs much more easily than in trained individuals. The risk of such a complication in stressful situations in people adapted to heavy physical activity is much less.
There is no doubt that the risk of sudden death increases with increasing volume and intensity of exercise. In this regard, mixed zone training and peak loads are not recommended for people over 50 years of age, since at this age it is impossible to exclude damage to the coronary arteries, which is not always detected even during a maximum stress test.
Monitoring the health of athletes has been the responsibility of FIFA doctors since 2003, when 28-year-old midfielder Marc Vivien Foe (Cameroon) died of cardiac arrest during a Confederation Cup game. Since then, the heart of athletes has become the object of close attention of sports doctors.
The essence of the problem
Hypertrophy of the left ventricle of the heart is often a consequence of overload or malfunction of the valve apparatus. This is the main diagnostic sign of hypertrophic cardiomyopathy. The left ventricle of the heart is a cavity, a muscular formation that is capable of contracting and pushing blood. This chamber begins the systemic circulation.
There are several types of hypertrophy: eccentric, concentric and with obstruction. Each form has its own characteristics. Eccentric left ventricular hypertrophy is most often formed due to insufficiency of the valve located between the left parts of the heart. Its development is based on an excess of normal blood volume in this part of the heart.
The weight of the left ventricle increases and it stretches. Such changes negatively affect heart contractions. High load leads to decreased cardiac output. The concentric form of LVH is different in that the blood is thrown back, and the myocardium requires more force to push it into the aortic lumen. This is accompanied by thickening of the walls of the heart chamber. Sometimes a decrease in the ventricular cavity is observed.
Sport for life
Continuing to exercise
An important question is whether to stop playing sports due to age or due to the end of a sports career. Research and observation to date has established the view that individuals who continue to exercise, albeit to a lesser extent, have a lower risk of developing cardiovascular disease compared to those who abruptly stop exercising. The athlete’s heart muscle (myocardium) begins to undergo reverse changes, which lead to a decrease in the functional capacity of the organ and its energy metabolism.
People who used to regularly exercise and suddenly stop doing physical activity often complain of increased blood pressure. This problem is especially acute for those people who at one time were involved in strength sports. While maintaining your level of physical activity, you need to do it at a level that makes you feel comfortable. Such training will be as safe as possible for the cardiovascular system.
Nutritional Features
To strengthen the walls of the ventricle, as well as to restore the functioning of the myocardium, it is very important to follow a diet:
- Reduce salt intake. It increases blood pressure, and this can cause strokes and ischemia.
- Eat seafood daily - squid, shrimp, mussels, oysters, fish. They improve the condition of blood vessels and reduce the likelihood of a heart attack.
- Regularly consume fresh vegetables, fruits, and dried fruits. Bananas, dried apricots, dates, figs, apples, plums, pomegranates - all these products make blood vessels elastic, relieve spasms in arterial hypertension, and remove harmful cholesterol.
- Eliminate smoked and fatty foods from your diet - they increase the risk of heart disease due to trans fats.
Patients need to eat small meals, little by little, drink carrot juice, and give preference to pureed porridge. Eliminate herbs and spices from your diet.
Main etiological factors
The rhythmic work of the heart muscle creates an electric field with electrical potentials having a negative or positive pole. The difference between these potentials is recorded in leads - electrodes attached to the patient’s limbs and chest (indicated “V” on the graph). The electrocardiograph records changes in signals that arrive over a certain time range and displays them as a graph on paper.
A fixed time period is reflected on the horizontal line of the graph. Vertical angles (teeth) indicate the depth and frequency of impulse changes. Teeth with a positive value are displayed upward from the time line, with a negative value - downward. Each tooth and lead are responsible for recording the functionality of a particular cardiac section.
Indicators of the left ventricle are: waves T, S, R, segment S-T, leads – I (first), II (second), III (third), AVL, V5, V6.
- The T-wave is an indicator of the recovery stage of the muscle tissue of the ventricles of the heart between contractions of the middle muscular layer of the heart (myocardium);
- Q, R, S - these teeth show agitation of the cardiac ventricles (excited state);
- ST,QRST, TP are segments indicating the horizontal distance between adjacent teeth. Segment prong = interval;
- Leads I and II (standard) – display the anterior and posterior walls of the heart;
- III standard lead – fixes I and II according to a set of indicators;
- V5 – lateral wall of the left ventricle in front;
- AVL – lateral cardiac wall anterior to the left;
- V6 – left ventricle.
Schematic representation of ST segment elevation in V1 and V2, indicating LVH
The electrocardiogram evaluates the frequency, height, degree of jaggedness and location of the teeth relative to the horizontal in the leads. The indicators are compared with the norms of cardiac activity, changes and deviations are analyzed.
The causes of myocardial hypertrophy are different. The development of this pathology is based on cardiac overload. It is possible under the following conditions:
- hypertension;
- stenosis of the aortic and mitral valve;
- aortic or mitral valve insufficiency;
- congenital segmental narrowing of the aorta (coarctation);
- salt deposits on valves;
- the presence of atherosclerotic lesions of the aorta;
- hyperthyroidism (thyrotoxicosis);
- pheochromocytoma (adrenal tumors);
- diabetes mellitus;
- cardiomyopathy;
- obesity;
- alcoholism.
The following risk factors for left ventricular overload are identified:
- hard physical labor;
- an increase in circulating blood volume due to obesity;
- smoking;
- stress;
- infectious diseases (endocarditis);
- dyslipidemia (blood lipid disorder);
- playing sports.
Enlarged LV is often found in professional athletes (weightlifters, runners), as well as in people engaged in heavy work (loaders).
Thickening of the walls of the heart chambers may have a hereditary predisposition. The risk group includes men over 50 years of age. The condition of the heart muscle largely depends on lifestyle. Nutrition is of great importance. Excess fat, simple carbohydrates and salt can lead to LV enlargement.
After consultation with a cardiologist, it is recommended to expand your physical activity with walks and jogging in the park, swimming, and physical therapy. In this case, all loads should be moderate. Also, for myocardial hypertrophy, drug therapy is used aimed at normalizing blood pressure, restoring rhythm and improving myocardial function. For this purpose, drugs of the following groups are used: ACE inhibitors, calcium antagonists, sartans and other drugs.
If drug therapy does not help, the pathology progresses, the normal functioning of the heart septa and valves is disrupted, and various types of surgical operations are performed.
Pathological athlete's heart
Overload during training
People who regularly exercise do not always have a healthy heart. And there are many reasons for this. In sports medicine, the concept of measure is important; a state of overtraining is dangerous for an athlete. In such cases, there is an imbalance between the needs of the heart muscle for nutrients and the possibility of their delivery to the myocardium. Processes called dystrophic begin to occur in the heart. The blood supply to the myocardium deteriorates. The elasticity of the heart muscle deteriorates and its contractility decreases. In response to overload, the heart responds by increasing atrial volume. Such changes are called maladaptive and occur in overstrain syndrome.
Overexertion can occur when athletes begin training during or immediately after an infectious disease, without maintaining the required time recommended by the doctor. Exceeding the permissible limit of physical activity, poor diet, insufficient sleep are factors that can lead to the heart being in unfavorable conditions. Taking doping drugs can also provoke a similar condition. With overexertion syndrome, patients may complain of decreased tolerance to physical activity, tingling, aching pain in the heart area, a feeling of discomfort in the heart area, and interruptions in heart function.
Signs of hypertrophy of the “athletic heart”
When conducting an electrocardiographic examination, signs may be identified that indicate deviations from the norm in people involved in sports, namely:
- decrease in heart rate (HR) less than 30 per minute,
- pathological Q wave in two or more leads,
- depression (decrease) of the ST segment in two or more leads,
- complete block of the left bundle branch,
- widening of the QRS complex more than 0.14 sec,
- deviation of the electrical axis (EOS) of the heart to the left,
- right ventricular hypertrophy,
- left atrial hypertrophy,
- shortening of the QT interval,
- rhythm disturbances - supraventricular tachycardia, atrial fibrillation and flutter,
- ventricular rhythm disturbances (tachycardia, extrasystoles).
Statistical data
- LVH of the heart is often recorded in patients aged 20-40 years.
- Women suffer from LVH less often than men.
- Thickening of the left ventricle over time and if left untreated leads to enlargement of the right atrium.
- Death from this disease occurs in 2–8% of cases.
- At the initial stage of hypertrophy, the patient has a favorable prognosis for recovery.
- It is important for patients to rest at least 7 hours a day, avoid foods that lead to intoxication and toxins, constantly monitor blood pressure, and reduce physical activity.
LVH of the heart is a dangerous pathology, because at first it may not manifest itself in any way and only on ECG, ultrasound and MRI will the cardiologist see changes in the functioning of the heart muscle. If the doctor discovers LVH, he will definitely begin to treat the patient: with medication or surgery. Depending on the cause of the pathology and its severity. If you consult a cardiologist in a timely manner, the prognosis is favorable.
Signs of an athlete's heart
Slowing your heart rate
Athletic heart has its own diagnostic signs, which indicate to the doctor that the patient regularly plays sports. To date, the Seattle criteria for athlete's heart syndrome have been proposed:
- Slow heart rate (sinus bradycardia) of 30 beats per minute or higher. This phenomenon in athletes is asymptomatic when patients feel well.
- Respiratory arrhythmia. Changes in the regularity of the heart rhythm depending on the phases of breathing. During physical activity, respiratory arrhythmia disappears. Slowing of atrioventricular conduction (atrioventricular block 1st and 2nd degree). The electrical impulse travels from the atria to the ventricles over a longer period of time. The phenomenon of slowing down atrioventricular conduction disappears during physical activity.
- Incomplete blockade of the right bundle branch. Most often, slow conduction along the right leg is associated with an increase in the size of the right ventricle.
- Escape rhythm from the atrioventricular node. Syndrome of early ventricular repolarization.
- Dome-shaped ST segment elevation in combination with a negative T wave in precordial leads (V1 to V4).
The listed electrocardiographic signs are lable and tend to disappear against the background of physical activity. If all these signs are identified, the doctor must carry out a differential diagnosis with such diseases of the cardiovascular system as hypertrophic cardiomyopathy, dilated karyomyopathy, arrhythmogenic dysplasia of the right ventricle, myocarditis. The diagnosis of sports heart is made when signs of possible organic diseases of the cardiovascular system are excluded.