If the right atrium (RA) is overfilled with blood or pressure overload, myocardial hypertrophy subsequently occurs. Signs of this condition are shortness of breath, dizziness, fainting, and irregular contractions. Treatment requires an impact on the disease that caused overstrain of the heart muscle (lung disease, valvular heart disease).
Structure
The atrium cavity is not designed for a large one-time volume of blood, so the thickness of the walls is 2-3 mm (five times less than that of the ventricle). A sufficient number of muscle fibers and the functionality of the valves avoid overload.
Anatomy
The anatomical structure of the right atrium is represented by a hexagonal cubic chamber. Characteristics of the main landmarks and elements of each of the walls are in the table:
| Wall | Structural basis | What does it border on? | Education |
| Inner (left) | Interatrial septum | Left atrium | Fossa ovale (during the prenatal period and in premature babies, a hole is located in its place, which closes in the first weeks of the newborn’s life) |
| Upper | Local expansion of the cavity of the RA (sinus cava - SV) | PVs that terminate the systemic circulation |
|
| External (right) | Three-layer heart wall | Lung tissue (under the pleura) | The lower bundle of pectineus muscles runs along the edge - roller-shaped protrusions hidden under the endocardium |
| Rear | Diaphragm | The inner surface of the PP part is smooth, without additional formations | |
| Front | Right ear (narrowed part of the RA cavity, directed forward and to the left) | Sternum and ribs, mediastinal pleura | The decussate pectineus muscles that line the cavity |
| Lower | Right atrioventricular orifice | Right ventricle | Tricuspid (tricuspid) valve |
Vessels of the right atrium
Cardiomyocytes of the RA are supplied with blood by the right coronary artery, which starts from the aortic sinus and lies in the designated coronal sulcus. Along the way, the vessel gives off branches:
- to the sinoatrial node (the main pacemaker of the heart);
- atrial (2-6), which supply the ear and nearby tissues;
- intermediate branch (nourishes the bulk of the myocardium).
The outflow of venous blood from the myocardium of the right atrium occurs in two ways:
- Through the coronary veins, the fluid enters the coronary sinus of the left part of the diaphragmatic surface of the heart. The length of the sinus is 2-3 cm and opens into the cavity of the RA at the confluence of the inferior vena cava.
- Direct outflow from small-caliber vessels (the group of “right atrial veins” of Viessen-Tibizia) into the chamber cavity.
The lymphatic system of the right heart is represented by three networks:
- deep (subendothelial);
- intermediate (myocardial);
- superficial (subepicardial).
The spent lymph from the local system enters large vessels, on the way of which there are regional nodes.
Histology
The collection of venous blood from the entire body and its direction into the pulmonary circulation requires a specific structure of the walls of the right atrium. The histological structure of the PP is presented in the table:
| Shell | Layers | Structural features | Functions |
| Endocardium | Endothelium | Epithelial tissue on a thick basement membrane |
|
| Subendothelial | Contains progenitor cells for endothelial repair | ||
| Muscular-elastic | Consists of smooth myocytes and elastic fibers | ||
| Connective tissue | Presented by:
| ||
| Myocardium | Cardiomyocytes are muscle cells that form fibers | Contractile cardiomyocytes with intertwined fibers |
|
| Conducting cells | Pacemakers (“pace-setters”). In the area of the sinoatrial node, impulses are generated that are responsible for the contraction of the heart | ||
| Transitional - an integral part of the conduction system of the heart. Form “channels” for the passage of excitation waves | |||
| Purkinje fibers transmit impulses from the conduction system to working cardiomyocytes | |||
| Loose connective tissue | Loose fiber bundles | Separates separate groups of randomly located cardiomyocytes | |
| Epicard | Surface layer of collagen fibers | A thin layer of connective tissue covered with mesothelium (a type of epithelium that can produce fluid) that adheres to the myocardium |
|
| Elastic bundles | |||
| Deep collagen fibers | |||
| Collagen-elastic layer |
All chambers of the heart are enclosed in an external cavity formation of connective tissue - the pericardium (pericardial sac).
Anatomical features
Structure of the heart
The right atrium is located anterior and to the right relative to the left. On the outside it is covered with the epicardium, under which there is a thin layer of myocardium and an inner layer - the endocardium. From the inside of the atrium, the surface is smooth, except for the inner surface of the appendage and part of the anterior wall, where ribbing is noticeable. This ribbing is due to the presence of the pectineus muscles, which are delimited by the border ridge from the rest of the inner surface. The right ear is an additional cavity in the shape of a pyramid.
The appendage functions as a blood reservoir and decompression chamber during ventricular systole. The ear also has a receptor zone, which allows it to take part in the regulation of heart contractions. Not far from the ear, on the anterior wall, there is an atrioventricular opening, through which communication occurs with the ventricle. The medial wall of the atrium plays the role of the interatrial septum. It has an oval fossa, which is closed by a thin connective tissue membrane.
Oval hole
Before birth and during the neonatal period, in its place is the foramen ovale, which takes part in the fetal circulation. After birth, the function of the foramen ovale is lost and it closes, leaving a hole. In a quarter of the population, the opening does not close and an atrial septal defect called the foramen ovale is formed.
In most cases, the defect does not cause any problems, but over time, with large sizes of the oval window, there is a risk of paradoxical embolism and heart attacks. The foramen ovale also ensures the discharge of blood from the left to the right atrium, which causes the mixing of arterial and venous blood and a decrease in cardiac output.
Functions and participation in blood circulation
Features of the location and structure of the walls of the PP regulate the performance of the chamber functions:
- Control of the heart rate, which is realized by a conglomerate of pacemaker cells located between the mouth of the superior PV and the right ear.
- Blood sampling from the entire body through the superior and inferior vena cava systems. There are no valves at their openings, so the RA fills even at low venous pressure.
- Regulation of blood pressure due to:
- reflexes from baroreceptors (nerve endings that respond to a decrease in blood pressure in the half of the RA): the signal transmitted to the hypothalamus stimulates the production of vasopressin, fluid retention in the body and stabilization of indicators;
- natriuretic peptide, which dilates peripheral vessels and reduces the volume of circulating fluid (through diuresis) in arterial hypertension.
- Blood deposition (reservoir function) is provided by the right ear when the RA is overloaded (excess fluid stretches the walls of the structure).
The role of the right atrium in systemic hemodynamics is determined by:
- collection of venous blood (PP - the functional end of a large circle of hemodynamics);
- filling of the right ventricle;
- formation and control of the tricuspid valve, pathologies of which cause disorders in the small and large circle of hemodynamics.
Severe dystrophic damage to the walls of the RA leads to arrhythmias, stagnation of blood in peripheral vessels (swelling of the legs, enlarged liver, fluid in the abdomen, chest cavity) and systemic failure.
Walls
The human right atrium is a cavity with four walls.
The important thing is that the inner surface of its walls is very smooth. It is as smooth as the inner surface of the other cavities of the heart, as well as the inner surface of the blood vessels.
Why is it important? Because the almost perfect smoothness of the inner layer of the walls ensures careful treatment of blood cells, ease of blood sliding through the chambers and cavities, and its calm movement without unnecessary turbulence.
So, the right atrium has four walls:
- top
- rear
- septal
- front
The structure of the wall of this heart chamber itself is the same as that of all its other cavities. It has three layers:
- inner layer - endocardium
- middle layer - myocardium
- outer layer - pericardium
You can read more about the structure of the walls of the heart in the article “Structure of the Human Heart.”
A distinctive feature of the structure of the wall of this chamber of the heart is that its thickness is insignificant, since the layer of muscle cells is much thinner than in the walls of other cavities.
Normal indicators of the right atrium
The functional state of the sinoatrial node is assessed using:
- Objective examination, measurement of pulse rate on the radial artery (normally 60-90 beats per minute of satisfactory filling). Reduced indicators are characteristic of pathologies of the conduction system (blockade) or sick sinus syndrome.
- Instrumental studies: ECG (electrocardiography) and EchoCG (echocardiography).
Information about the functioning of the heart chambers is obtained using the ultrasound method of EchoCG. The additional use of Doppler scanning on ultrasound visualizes the speed and direction of blood flow in the cavities.
Average dimensions of the right atrium on echocardiography:
- end-diastolic volume (EDV): from 20 to 100 ml;
- structural integrity of the RA cavity (in premature infants – atrial septal defect);
- reverse blood flow (regurgitation) during ventricular systole with prolapse and tricuspid valve insufficiency;
- pressure: systolic 4-7 mm Hg. Art., diastolic – 0-2 mm Hg. Art.
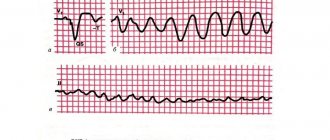
The right atrium on the ECG is represented by the initial section of the P wave. The passage of a nerve impulse causes the appearance of amplitude (a rise above the isoline). The length of the wave is determined by the speed of the signal.
During electrocardiogram analysis, the entire P wave is assessed (right atrium and left atrium simultaneously). Standard indicators:
- symmetry, presence in all leads;
- duration 0.11 s;
- amplitude 0.2 mV (2 mm on film).
The listed values change in case of intracardiac conduction disturbances or massive myocardial damage.
Left atrium value
What does a human heart look like?
How does the heart work?
Chambers of the human heart
What is myocardium: function and structure
What is an oval window
All articles about the heart
The left atrium meets and receives blood from the veins leading to the heart from the lungs, from the veins of the small circulation ring. From those veins that carry blood from the lungs to the heart, and, therefore, carry blood enriched with oxygen and purified from carbon dioxide.
In the cavity of the left ventricle, blood circulation through the small ring ends, and with each contraction of the small cavity of the atrium, a portion of blood entering the left ventricle begins a long journey through the large circulation ring.
Signs of heart chamber damage
Right atrium dysfunction most often develops against the background of combined myocardial damage (valvular defects, coronary artery disease). Clinical manifestations are nonspecific, so a complex of studies is required to make a diagnosis.
Typical malfunctions of the PP:
- hypertrophy;
- overvoltage;
- presence of a blood clot;
- dilatation;
- arrhythmias (if the sinoatrial node is involved in the process).
Symptoms of increased load
Increased stress on the chambers of the heart develops as resistance or fluid volume increases.
Characteristic deviations due to overload of the right atrium:
- increase in EDV (200-300 ml);
- thickening of the myocardial layer (more than 3-4 mm);
- increased pressure (systolic and diastolic) in the cavity.
The load on the RA increases with stenosis of the right ventricular outlet. After the completed contraction during systole, a small volume of blood remains in the chamber, which requires additional effort to push out. With each new cycle, the amount of residual fluid increases - overstrain of the right half of the heart occurs.
With uncorrectable stenosis of the aortic ostium or pathology of the mitral valve (defects of the left sections), changes in the right atrium and ventricle develop compensatoryly.
Hypertrophy
Hypertrophy is the proliferation of myocardial muscle mass, which develops to compensate for pathological changes in internal hemodynamics.
Changes in electrocardiography characteristic of hypertrophied PP:
- pronounced P wave in leads I, II;
- height exceeds 0.2 mV (more than two mm), width remains within normal limits;
- in leads V1 and V2 there is a pointed and high (more than 0.15 mV) anterior half of the P wave.
Slight myocardial thickening is not visualized on echocardiography, so ECG remains the main method for diagnosing right atrial hypertrophy.
Extension
With a significant expansion of the PP cavity, the final volume of the chamber reaches 200-300 ml or more. Such enlargement of the right atrium develops when the fibers are stretched due to:
- valve defects (impaired blood flow, so the walls first grow, and when energy reserves are depleted, they become thinner);
- post-infarction aneurysms;
- dilated cardiomyopathy is a pathology of unknown origin, which is characterized by dilation of the chambers of the heart and a decrease in contractility.
Presence of a blood clot
A thrombus (blood clot) in the RA is most often introduced with the flow of venous blood from the lower limb (through the vena cava). The risk of pathology increases with thrombophlebitis, varicose veins and other vascular diseases.
To identify disorders, transesophageal echocardiography is used - an ultrasound diagnostic method with a sensor inserted into the lumen of the esophagus. The clot is visualized as an echo-positive (relatively light-colored) formation in the RA cavity.
A “local” thrombus (formed in the chamber cavity) is located on a stalk - a thin outgrowth that is attached to the wall of the RA and moves under the influence of blood flow. The mobility of the clot is the reason for the sharp deterioration of the patient’s condition (feeling better in the supine position). Parietal thrombus has a more stable clinical picture.
Clot rupture leads to thromboembolism, the main cause of myocardial infarction and ischemic stroke.
Photo of a thrombus in the PP
Description of the disease
Atrial hypertrophy develops as a result of functional abnormalities. Let's figure out what it is. Heavy loads on the myocardium entail an increase in the number of its contractions, which, in turn, leads to disruption of metabolic processes. Metabolic deviations provoke an increase in cell mass and thickening of the walls of the atria.
At the initial stage of the disease, hypertrophy tends to adapt to the needs of the body, and the heart maintains blood circulation at the proper level. However, in the absence of effective treatment for a long time, the myocardium becomes depleted, losing its functionality.
Pathology on ECG
Pathology occurs against the background of various diseases that put stress on the heart muscle, as a result of local or general disruption of blood flow. The only exception is the compaction of the myocardium under the influence of constant physical activity. This deviation is called “athlete’s heart” and is not classified as pathological.
You can completely get rid of hypertrophy if you promptly cure the disease that provoked hardening of the heart tissue. Effective complex therapy will help reduce wall thickness and restore healthy heart function.
Methods for diagnosing disorders
Comprehensive diagnosis of right atrium dysfunction includes:
- X-ray of the chest organs (diagnosed as a shift in the boundaries or an increase in the size of the heart);
- electrocardiography (bioelectric characteristics of the myocardium, state of the cardiac conduction system);
- ultrasound examination (EchoCG);
- Doppler diagnostics to study the speed, volume and presence of obstacles to blood flow.
Functional methods that assess the body's response to stress tests have become widespread. For example, dosed walking (treadmill) or bicycle ergometry are used for ECG load.
Function
But what is the purpose of the human right atrium? What role does it play in the circulation of blood throughout the body?
The right atrium receives blood coming from all the veins of the systemic circulation.
The atrium is the vestibule of the heart. This chamber only welcomes “guests” and directs them further, into the heart itself - into the ventricle.
Its function, although important, does not require significant physical effort. This is why the layer of muscle cells in the wall of the right atrium is much thinner than the same layer in the wall of the right ventricle.
conclusions
The most common pathology is considered to be hypertrophy of the right atrium, which refers to the consequences of valve defects or diseases of the respiratory system. For example, chronic obstructive pulmonary disease. In athletes, moderate symmetrical thickening of the myocardium develops due to regular training. The prognosis for PP pathology depends on the severity and control of the underlying disease. The effectiveness of drug therapy is determined by the stage and the presence of dense connective tissue changes. If ectopic pacemakers are identified, a pacemaker is installed.