Pathogenesis
It is important to understand that a scar on the heart is a protective reaction of the body that occurs when necrotic foci form. In most cases, death of heart muscle cells occurs after a heart attack.
As soon as the process of cell death begins, connective tissue begins to form in this area. In this way, the body tries to prevent an increase in the area of necrosis. However, the scar on the heart after a heart attack cannot perform the functions of the organ. That is why the formation of connective tissue is only a temporary solution to the problem, which often leads to the development of life-threatening pathologies.
It is important to understand that a scar on the heart is a condition that prevents the development of acute myocardial failure and death. But it also delays the development of all kinds of complications. This is due to the fact that heart failure takes on a chronic form, characterized by constant alternation between periods of remission and relapse.
How to treat deviations
It is not possible to influence already formed scars in the myocardium.
For this purpose, medications from various groups are prescribed:
- for angina pectoris - beta blockers (Bisoprol), nitrates (Cardiket), ACE inhibitors (Enap), diuretics (Trifas), anticoagulants (Aspirin, Clopidogrel);
- for myocarditis - antibiotics (Augmentin), anti-inflammatory (Nimid), antiviral and immunomodulators (Cycloferon), vitamin complexes (Milgamma);
- to improve myocardial nutrition - antioxidants (Kudesan, Cytochrome C), metabolism stimulants (Mexidol, Panangin, Riboxin);
- hypolipidemic - Tulip, Roxera;
- antiarrhythmic - Ritmonorm, Cordarone;
- cardiac glycosides - Korglykon, Digoxin.
If there is no result from drug therapy, and the threat of recurrent infarction remains, in case of severe rhythm disturbance, surgical treatment is performed: installation of a stent or shunt, pacemaker, suturing of the aneurysm.
We recommend reading the article about heart valve fibrosis. From it you will learn about the causes of the development of pathology, symptoms, methods of diagnosis and treatment, and prognosis for patients.
And here is more information about posterobasal infarction.
Scar formation in the heart muscle is the final stage after myocarditis or myocardial infarction; it is also considered the outcome of atherosclerotic lesions of the coronary vessels. An ECG is used to detect focal or diffuse myocardial scarring.
To clarify the diagnosis, an in-depth clinical and instrumental examination is recommended. Symptoms and prognosis of cardiosclerosis depend on the severity of the underlying pathology. There are no specific manifestations; complications can include various heart rhythm disturbances and circulatory failure. For treatment, drug therapy is used; in case of threatening conditions, surgery is prescribed.
Recognizing myocardial infarction on an ECG can be difficult due to the fact that different stages have different signs and variations of waveforms. For example, the acute and acute stage may not be noticeable in the first hours. Localization also has its own characteristics: the infarction on the ECG is transmural, q, anterior, posterior, transferred, large-focal, lateral, different.
A repeated myocardial infarction can occur within a month (then it is called recurrent), as well as 5 years or more. To prevent the consequences as much as possible, it is important to know the symptoms and carry out prevention. The prognosis is not the most optimistic for patients.
The T wave on the ECG is determined to identify pathologies of cardiac activity. It can be negative, high, biphasic, smoothed, flat, reduced, and depression of the coronary T wave can also be detected. Changes can also be in the ST, ST-T, QT segments. What is an alternation, discordant, absent, double-humped tooth.
Myocardial dystrophy, or dystrophic changes in the myocardium, can be associated with an incorrect lifestyle and work disorders. Diffuse, metabolic, and moderate changes can be detected during an ECG. To begin with, treatment involves taking vitamins.
Myocardial ischemia on the ECG shows the degree of heart damage. Anyone can figure out the meanings, but it’s better to leave the question to the experts.
Post-infarction cardiosclerosis occurs quite often. He may have an aneurysm or ischemic heart disease. Recognizing symptoms and timely diagnosis will help save lives, and ECG signs will help establish the correct diagnosis. Treatment is lengthy, rehabilitation is required, and there may be complications, including disability.
After suffering certain diseases, myocardial cardiosclerosis may develop. This pathology is characterized by rhythm disturbances and other unpleasant manifestations. Treatment needs to start the sooner the better.
Depending on the time of onset, as well as the complexity, the following complications of myocardial infarction are distinguished: early, late, acute, frequent. Their treatment is not easy. To avoid them, preventing complications will help.
It is quite difficult to diagnose, since subendocardial myocardial infarction quite often has an abnormal course. It is usually detected using ECG and laboratory examination methods. An acute heart attack threatens the patient's death.
Etiology
A scar always forms in the area of muscle fiber rupture or in areas of necrosis. The body starts the synthesis of fibrin protein, which quickly fills the damage.
Causes of scars on the heart:
- Thrombosis and embolism of blood vessels. According to statistics, half of the world's population aged 40 years and older suffer from pathological changes. For example, a combination of increased blood clotting and even the initial stage of atherosclerosis leads to thrombosis. The resulting clot of liquid connective tissue partially narrows the lumen of the vessel. As a result, heart cells do not receive the required amount of nutrients and oxygen and begin to die. This situation is life-threatening, so fibrotic changes occur very quickly.
- Myocarditis. One of the most common causes of heart scars. Under the influence of unfavorable factors (allergy, infection, etc.), the myocardial muscle tissue becomes inflamed. As a result, dilatation develops, causing the heart to wear out and become damaged. Microtraumas are subsequently replaced by connective tissue.
- Cardiac ischemia. This term refers to a pathological condition characterized by chronic oxygen starvation of the myocardium. As a result, the process of degenerative-dystrophic changes is launched.
- Heart attack. A scar on the heart appears after it most often. The danger is that sometimes a heart attack is asymptomatic, and changes are detected only on an ECG.
Doctors identify myocardial dystrophy as a separate cause of scar formation. This is a pathological condition in which atrophic changes are noticeable in the heart, that is, the tissue is weaker and thinner than it should be.
Causes of myocardial dystrophy:
- Vitamin deficiency in the body.
- Lack of magnesium, calcium and potassium.
- Excess body weight.
- Frequent and high-intensity physical activity.
Doctors say that if at least one close relative has a heart scar after a heart attack, it is necessary to visit a cardiologist annually for prevention.
Scar on the heart: what is it, photos, causes and treatment
A scar on the heart in medical terminology is called cardiosclerosis.
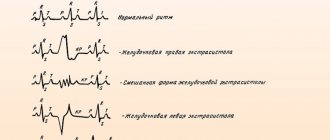
The essence of the pathological process is the death of cardiac muscle cells and their replacement with connective tissue, this can happen after a heart attack or as a result of an inflammatory process. An ECG helps identify changes in the heart muscle and specify the extent of damage. This process is dangerous for the patient’s life, since fibrous tissue is tougher in structure than muscle fibers; it is not able to contract in a rhythm synchronous with all other parts of the heart.
For patients experiencing heart scarring, it is important to know the causes of this phenomenon and to prevent further changes in the heart muscle.
Without appropriate help, the consequences of fibrosis can be very diverse, from heart failure and aneurysm of the lower wall of the heart to sudden death as a result of a second heart attack.
Where do scars come from?
Heart scars form where muscle fibers have ruptured or large numbers of cells have died. The body compensates for the damage as quickly as possible - the protein fibrin is produced, which fills the damaged area. What causes lead to heart injuries:
- Thrombosis and vascular embolism. About 45% of the population over 40 years of age already have pathological changes in the blood vessels of the heart. Even the initial stage of atherosclerosis, combined with increased blood clotting, can cause thrombosis, in which a clot of coagulated blood seals the vessel bed. Some cells that do not receive the necessary oxygen and nutrients die, and local tissue necrosis occurs. Such damage poses a threat to the body, so healing occurs very quickly and with fibrotic changes in the tissue. The extent of damage to the contractility of the organ depends on the area of scar growth. An ECG helps diagnose early irregularities in heart rhythm, in particular arrhythmia. For a more detailed study of the coronary vessels, in addition to the ECG, Doppler ultrasound is prescribed. Doppler sonography shows not only the condition of the coronary vessels, but also stenosis of the aorta or inferior vena cava.
- Myocarditis. This is a group of diseases in which inflammation of the myocardial muscle tissue occurs due to infection, allergy, or other reason. Myocarditis often provokes dilatation, in which the volume of the heart chambers increases, but the thickness of the lower or lateral wall remains the same. As a result of dilatation, the heart quickly wears out and receives microtrauma in the area of the wall aneurysm. Tears and focal necrosis of the wall are replaced by fibrous fibers. The results of an ECG can reveal disturbances in the rhythm or strength of heart contractions.
- Ischemia. This is a disease in which the coronary vessels cannot meet the heart's need for oxygen, resulting in chronic oxygen deprivation. Ischemic disease often occurs with damage to the ventricles, with atrophic changes in the posterior or lower wall of the heart, and with myocardial fibrosis (especially in the area of the coronary artery). A natural consequence of ischemic disease is a heart attack. An ECG during ischemia often reveals pathological changes in the walls of the left ventricle; for a more detailed picture, ultrasound dopplerography is used.
- Heart attack. According to cardiologists, this reason is the most popular and most often provokes cardiosclerosis. A heart attack is not always accompanied by a typical clinical picture; in some people it is asymptomatic, and only an ECG can show what happened. Fibrosis in the myocardium, ventricular walls, or interventricular septum increases the risk of recurrent infarction by 45%.
A separate item can be highlighted myocardial dystrophy, that is, a condition in which the muscles of the myocardium and pericardium have atrophic changes; they are thinner and weaker than they should be according to the anatomical norm. Leads to myocardial dystrophy:
- amitaminosis;
- lack of potassium, calcium or magnesium;
- obesity;
- excessive physical activity, irrational sports;
- diseases of the endocrine system, as well as kidneys and liver.
Patients who have at least one blood relative affected by diseases of the cardiovascular system must undergo an ECG and examination by a cardiologist once a year. An ECG can prevent dangerous fibrosis of the left ventricle, protect against heart attack and premature death.
Advice! The cardiologist should be informed about existing endocrine diseases and family history. This information is important for proper prevention or treatment.
What are the dangers of a scar on the heart, what types of scars are there?
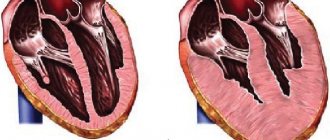
Immediately after the death of myocardial cells, focal hypertrophy occurs, that is, a separate area, for example, in the area of the left ventricle, temporarily increases in size. After healing, a dense scar forms in this place, and hypertrophy either disappears or turns into dilatation.
Cardiosclerosis never develops as a separate disease; it is always preceded by other diseases of the endocrine or cardiovascular system. According to statistics, fibrosis most often occurs in the left ventricle. This arrangement is considered the most dangerous, because the left ventricle plays an extremely important role in the proper functioning of the heart:
- The left ventricle has a larger volume compared to other chambers, which means it is subject to greater load. Fibrosis in the area of the ventricular wall will lead to heart failure in a short time.
- The left ventricle receives arterial blood from the right atrium at the moment when the walls relax, and then sends it through the systemic circulation. The force of contraction of the ventricle must be sufficient to provide the necessary pressure inside the aorta. If the left ventricle cannot cope with its task, the patient suffers from heart failure, the brain and other organs do not receive a sufficient amount of oxygen and suffer from hypoxia.
- From the left ventricle, blood splashes into the aorta. If fibrosis affects the mitral or aortic valve, aortic stenosis develops, a condition in which the lumen of this important blood vessel narrows. Cardiosclerosis of the left ventricle in combination with valvular insufficiency is a reason to undergo treatment in the cardiology department as soon as possible.
Scarring of the interventricular septum is considered a relatively safe fibrosis, provided that the ECG shows normal heart rhythm and strength of contractions. Myocardial dystrophy and other diseases of the heart and blood vessels provoke 3 types of fibrosis:
- Focal. It has clear boundaries of location, for example, it is located only on the posterior wall of the heart. Fibrin inclusions do not exceed a few cubic millimeters in size.
- Diffuse. Affects all muscle tissue of the heart completely.
- Diffuse-focal. This is a mixed form, in which small foci of pathology can be identified, distributed evenly over the entire area of the heart. The size of fibrin fibers can increase due to the fusion of several small foci.
In cardiology, scarring of the heart muscle is considered a chronic disease, occurring with temporary improvements or deterioration in well-being. Treating this condition and maintaining normal heart function is not an easy task.
Fact! It is easier to prevent fibrotic changes by training the heart and strengthening blood vessels than to eliminate them if they have already occurred. There are no medications or surgeries that completely restore the normal structure of the heart muscle.
How to remove a scar?
The symptoms of heart scars directly depend on the disease that caused them. Within 5-10 years, fibrous replacement can occur without specific symptoms, as long as the heart manages to compensate for the volume of connective tissue and maintain contractility. Then the complaints appear:
- for chest pain;
- for shortness of breath;
- for complete or partial intolerance to physical activity;
- swelling of the face and limbs;
- for rapid fatigue.
The tips of the fingers and toes acquire a characteristic bluish tint, which signals heart failure. Treatment at this stage is aimed at protecting the heart from further damage; surgery or special medications (except cardioprotectors) are not required.
If a heart attack occurs as a result of ischemia or atherosclerosis, extensive fibrosis develops after necrosis, affecting the posterior wall, coronary vessels, often even the aortic valves. In this case, urgent drug treatment is started, which includes:
- beta blockers;
- acetylsalicylic acid;
- diuretics;
- metabolites (ATP and others);
- nitrates.
It is strictly prohibited to select medications on your own after a heart attack; you should contact your cardiologist for detailed prescriptions. Treatment should be continued until the relative normalization of well-being, not forgetting that cardiosclerosis increases the likelihood of a recurrent heart attack by 50-75%.
Fact! The scar after a heart attack continues to increase in area for 2-4 months, all this time it is necessary to maintain dynamic monitoring of the patient. Surgery may be required if the condition suddenly worsens.
Other recommendations from cardiologists regarding the treatment of fibrotic changes:
- do not overload the heart, avoid active sports and physical activity;
- remain calm, avoid emotional stress;
- support the heart muscle with a special diet.
After a heart attack, it is useful to undergo treatment in specialized cardiac centers rather than at home, this helps reduce the damage resulting from impaired blood supply to the heart muscle.
Interesting! If scars on the heart affect more than a quarter of the total volume of the organ, this is an indication for surgery.
Surgical care for scars
In extremely severe cases, an operation is used in which a pacemaker or a cardioverter-defibrillator is installed to maintain the normal rhythm and conduction of the heart. Several more types of surgical intervention that are used for cardiosclerosis:
- Living heart transplantation from a donor. The operation is performed on people under 65 years of age without a history of serious diseases of the internal organs (which is rare, given coronary artery disease or atherosclerosis).
- Bypass surgery is an expansion of the lumen of narrowed coronary vessels. The operation is performed for severe atherosclerosis.
- Removal of the aneurysm. The bulge most often forms in the posterior wall or in the area of the left ventricle. The operation takes place under general anesthesia and consists of truncation of the protruding area.
Surgery is used as both conventional and palliative treatment. The scar after the intervention usually does not pose a threat compared to existing fibrosis.
Source: https://HelperSkin.ru/orubcah/rubec-na-serdce-chto-eto-takoe
Types of scars
Against the background of various pathologies, fibrosis of one of three types can form:
- Focal. It has clear boundaries and a specific location. For example, the scar may be on the back wall of the heart muscle.
- Diffuse. It differs in that it affects all tissues.
- Diffuse-focal. This form is mixed. It is characterized by the presence of small pathological foci that are evenly distributed over the entire surface of the heart. Sometimes scars grow together.
Cardiologists say that scars on the heart are a pathology, the treatment of which is not only complex, but also lengthy. In most cases, doctors create a treatment plan aimed at maintaining the functioning of the organ.
Clinical manifestations
Symptoms and their severity directly depend on what disease caused the damage to muscle tissue. Cardiologists say that scars on the heart after a heart attack (a photo of the affected organ is shown schematically below) can form over several years. In this case, the process is often asymptomatic.
The absence of clinical manifestations is due to the fact that the organ manages to maintain contractility and compensate for the volume of normal tissue. When it is no longer able to function fully, the following symptoms appear:
- Painful sensations in the chest.
- Severe shortness of breath.
- Swelling of the face and limbs.
- Severe fatigue even after minor physical exertion.
- Increased degree of fatigue.
Over time, the fingertips on both the upper and lower extremities acquire a bluish tint. This is a specific sign of severe heart failure. At this stage, doctors take measures to prevent further damage to the heart. Often the only way to save the patient's life is surgery.
Scars on the back of the heart
In many people, during the diagnostic process, scars on the heart are detected using an electrocardiogram, but not everyone understands what it is and how to deal with it.
In medical terminology, the pathology is called cardiosclerosis, which can occur at any age, but is mainly detected in people over forty years of age.
This disease signals a critical condition of the cardiovascular system and requires urgent treatment, which can be carried out using medication, folk and surgical methods.
What causes scarring on the heart muscle?
What is a heart scar? In fact, it is connective tissue that fills the space created as a result of damage to a certain area of the heart muscle. This happens with an inflammatory disease or myocardial infarction, which is caused by various factors. The appearance of numerous notches on the heart can occur due to progressive vascular atherosclerosis.
The appearance of scars is caused by the death of heart cells as a result of blocking the access of oxygen-enriched blood to them. A common cause of heart scars is thrombosis. If a person has a prolonged vascular spasm, this will lead to partial necrosis of the organ. Other diseases that cause scarring of the heart include:
- Cardiac form of rheumatism.
With this type of disease, inflammation of the myocardium and cardiac membranes occurs. As a rule, the pathology is a consequence of frequently recurring tonsillitis, chronic tonsillitis, scarlet fever and streptococcal diseases. In this case, damage to the epicardium is observed, which ultimately ends in scarring and thickening, which is necessary to restore and maintain the functionality of the heart. - Myocarditis.
If a person has previously suffered any infectious diseases that resulted in complications in the form of inflammation of the heart tissue, this can cause scarring. Intoxication as a result of poisoning and parasitic infestations also leads to this. - Cardiac ischemia.
This pathology accounts for 90% of all deaths from heart disease. It is the cause of numerous scars, and can also be a consequence of their appearance. This creates a vicious circle that quickly leads the patient to a heart attack or stroke. - Myocardial infarction.
In most cases, a heart attack ends in death, but if the patient received timely medical care and survived as a result of resuscitation measures, scarring will occur.This condition is the main cause of the proliferation of connective tissue, which fills the wound formed after cell necrosis.
The cause of scars can be not only the presence of one or more diseases of the cardiovascular system, but also an incorrect lifestyle, endocrine disorders, and severe stress.
The development of cardiosclerosis can be indirectly affected by the following pathological conditions:
- diabetes;
- anemia;
- obesity;
- amyloidosis;
- metabolic disease;
- premature wear of the heart as a result of heavy physical exertion;
- hemosiderosis.
In rare cases, cardiosclerosis can be detected in a child with congenital heart defects. Some adults experience a mild heart attack on their legs, thinking they are having an attack of tachycardia or angina.
Sometimes a person suffering from a suffocating cough turns to a therapist for help, and the therapist, having not found the reasons for its occurrence, sends the patient for a comprehensive examination. As a result of EGC or ultrasound, cardiosclerosis is detected.
In this case, the patient needs to make an appointment with a cardiologist, find out the main reason for the appearance of scars on the heart and begin treatment.
What is the danger?
If a person develops a scar on their heart after a heart attack, it can lead to coronary artery disease, heart failure, and an aneurysm. Much depends on what type of disease the patient suffers from. Cardiosclerosis is divided into:
- Diffuse. With this type of disease, a uniform thickening of the walls of the heart muscle occurs due to the appearance of pinpoint foci of connective tissue on them. In this case, large scars may not occur.
- Large-focal. The most dangerous type of cardiosclerosis, since it involves the replacement of large affected areas with fibrous tissue that is unable to contract. As a result of dysfunction of the cardiovascular system, serious diseases begin to develop, most often ending in death.
- Finely focal. This type of disease has a generally positive prognosis with proper treatment and systematic testing. This form is the result of a microinfarction, after which one small scar remains on the heart, which does not significantly limit the functionality of the organ.
Sometimes the appearance of a scar on the heart goes away almost unnoticed and the person continues to live without taking any measures. But it is possible to detect cardiosclerosis without undergoing special diagnostic procedures, based on the characteristic symptoms of the disease:
- cardiopalmus;
- dyspnea;
- fast fatiguability;
- constantly cold hands or feet, as well as their numbness;
- swelling of the face;
- exercise intolerance;
- blueness of fingertips.
A person who has scars on the heart suffers from severe chest pain, which can be paroxysmal (paroxysmal) in nature, looks pale due to insufficient blood supply to the tissues as a result of cardiac dysfunction.
The main consequences of cardiosclerosis are atrial fibrillation, extrasystole, heart block, stroke and heart attack. These are serious diseases that most often cause disability and death.
What to do if a scar is found?
If a scar is discovered during diagnosis, the person needs to make an appointment with a cardiologist and undergo additional examinations. This should be done to exclude or confirm the presence of other heart diseases. Cardiosclerosis is very rarely a separate disease; it is usually a marker of various other heart pathologies.
During the examination, the doctor will find out how many lesions there are in the heart muscle and what condition the blood vessels are in. If there are blood clots and cholesterol plaques, medications that thin the blood, improve metabolic processes in the heart, and lower blood pressure will be prescribed.
Source: https://women-land.ru/varikoz/rubcy-na-zadnej-stenke-serdca.html
Diagnostics
If the first alarming signs occur, you should contact a cardiologist as soon as possible. The specialist will collect anamnesis, conduct a physical examination and issue a referral for a comprehensive diagnosis, including the following studies:
- ECG.
- Dopplerography.
- EchoCG.
- X-ray.
- Coronary angiography.
Based on the diagnostic results, the doctor draws up the most effective treatment regimen. In severe cases, he evaluates the feasibility of surgical intervention.
Drug treatment
Conservative therapy involves taking medications whose active components help maintain heart function. In addition, patients need to follow the principles of a healthy lifestyle.
The choice of medications is made by the attending physician based on the diagnostic results. The cardiologist prescribes medications that improve heart function by accelerating metabolic processes and restoring the circulation of fluid connective tissue.
An effective method is stem cell treatment. Against the background of their use, natural processes of restoration of affected tissues are launched in the body. They are noticeable soon after the introduction of a cardiomyoblast (a specific cellular element). During treatment, the contractility of the organ is restored and blood circulation improves. In addition, atherosclerotic plaques dissolve, vessel walls are strengthened and necrosis is prevented.
If a heart attack develops as a result of ischemic disease, urgent medical treatment is indicated, which involves taking or intravenously administering the following drugs:
- Beta blockers.
- Diuretics.
- Metabolites.
- Nitrates.
- Acetylsalicylic acid.
If a scar on the heart was discovered during an ECG, you need to be prepared for the fact that it will increase in size for several more months. This information is also relevant for patients who have already undergone treatment. If your health suddenly deteriorates, you must call an ambulance. It is possible that emergency surgery will be required.
Self-medication is strictly prohibited. The wrong choice of drug can be fatal.
Scar on the heart - what is it? Causes, treatment, potential danger
Under the influence of various unfavorable factors, the process of death of heart cells can begin. As a result, they are replaced by scar tissue, characterized by a high content of protein and collagen. In medicine, the pathology is usually called cardiosclerosis.
It is important to understand that a scar on the heart is a condition that poses a danger not only to the health, but also to the life of the patient. In this regard, when the first alarming signs occur, you should contact a cardiologist.
The specialist will issue a referral for comprehensive diagnostics, based on the results of which he will create the most effective treatment regimen. Therapy may include both conservative and surgical techniques.
Pathogenesis
It is important to understand that a scar on the heart is a protective reaction of the body that occurs when necrotic foci form. In most cases, death of heart muscle cells occurs after a heart attack.
As soon as the process of cell death begins, connective tissue begins to form in this area. In this way, the body tries to prevent an increase in the area of necrosis.
However, the scar on the heart after a heart attack cannot perform the functions of the organ.
That is why the formation of connective tissue is only a temporary solution to the problem, which often leads to the development of life-threatening pathologies.
It is important to understand that a scar on the heart is a condition that prevents the development of acute myocardial failure and death. But it also delays the development of all kinds of complications. This is due to the fact that heart failure takes on a chronic form, characterized by constant alternation between periods of remission and relapse.
Etiology
A scar always forms in the area of muscle fiber rupture or in areas of necrosis. The body starts the synthesis of fibrin protein, which quickly fills the damage.
Causes of scars on the heart:
- Thrombosis and embolism of blood vessels. According to statistics, half of the world's population aged 40 years and older suffer from pathological changes. For example, a combination of increased blood clotting and even the initial stage of atherosclerosis leads to thrombosis. The resulting clot of liquid connective tissue partially narrows the lumen of the vessel. As a result, heart cells do not receive the required amount of nutrients and oxygen and begin to die. This situation is life-threatening, so fibrotic changes occur very quickly.
- Myocarditis. One of the most common causes of heart scars. Under the influence of unfavorable factors (allergy, infection, etc.), the myocardial muscle tissue becomes inflamed. As a result, dilatation develops, causing the heart to wear out and become damaged. Microtraumas are subsequently replaced by connective tissue.
- Cardiac ischemia. This term refers to a pathological condition characterized by chronic oxygen starvation of the myocardium. As a result, the process of degenerative-dystrophic changes is launched.
- Heart attack. A scar on the heart appears after it most often. The danger is that sometimes a heart attack is asymptomatic, and changes are detected only on an ECG.
Doctors identify myocardial dystrophy as a separate cause of scar formation. This is a pathological condition in which atrophic changes are noticeable in the heart, that is, the tissue is weaker and thinner than it should be.
Causes of myocardial dystrophy:
- Vitamin deficiency in the body.
- Lack of magnesium, calcium and potassium.
- Excess body weight.
- Frequent and high-intensity physical activity.
Doctors say that if at least one close relative has a heart scar after a heart attack, it is necessary to visit a cardiologist annually for prevention.
Types of scars
Against the background of various pathologies, fibrosis of one of three types can form:
- Focal. It has clear boundaries and a specific location. For example, the scar may be on the back wall of the heart muscle.
- Diffuse. It differs in that it affects all tissues.
- Diffuse-focal. This form is mixed. It is characterized by the presence of small pathological foci that are evenly distributed over the entire surface of the heart. Sometimes scars grow together.
Cardiologists say that scars on the heart are a pathology, the treatment of which is not only complex, but also lengthy. In most cases, doctors create a treatment plan aimed at maintaining the functioning of the organ.
Clinical manifestations
Symptoms and their severity directly depend on what disease caused the damage to muscle tissue. Cardiologists say that scars on the heart after a heart attack (a photo of the affected organ is shown schematically below) can form over several years. In this case, the process is often asymptomatic.
The absence of clinical manifestations is due to the fact that the organ manages to maintain contractility and compensate for the volume of normal tissue. When it is no longer able to function fully, the following symptoms appear:
- Painful sensations in the chest.
- Severe shortness of breath.
- Swelling of the face and limbs.
- Severe fatigue even after minor physical exertion.
- Increased degree of fatigue.
Over time, the fingertips on both the upper and lower extremities acquire a bluish tint. This is a specific sign of severe heart failure. At this stage, doctors take measures to prevent further damage to the heart. Often the only way to save the patient's life is surgery.
Diagnostics
If the first alarming signs occur, you should contact a cardiologist as soon as possible. The specialist will collect anamnesis, conduct a physical examination and issue a referral for a comprehensive diagnosis, including the following studies:
- ECG.
- Dopplerography.
- EchoCG.
- X-ray.
- Coronary angiography.
Based on the diagnostic results, the doctor draws up the most effective treatment regimen. In severe cases, he evaluates the feasibility of surgical intervention.
Drug treatment
Conservative therapy involves taking medications whose active components help maintain heart function. In addition, patients need to follow the principles of a healthy lifestyle.
The choice of medications is made by the attending physician based on the diagnostic results. The cardiologist prescribes medications that improve heart function by accelerating metabolic processes and restoring the circulation of fluid connective tissue.
An effective method is stem cell treatment. Against the background of their use, natural processes of restoration of affected tissues are launched in the body.
They are noticeable soon after the introduction of a cardiomyoblast (a specific cellular element). During treatment, the contractility of the organ is restored and blood circulation improves.
In addition, atherosclerotic plaques dissolve, vessel walls are strengthened and necrosis is prevented.
If a heart attack develops as a result of ischemic disease, urgent medical treatment is indicated, which involves taking or intravenously administering the following drugs:
- Beta blockers.
- Diuretics.
- Metabolites.
- Nitrates.
- Acetylsalicylic acid.
If a scar on the heart was discovered during an ECG, you need to be prepared for the fact that it will increase in size for several more months. This information is also relevant for patients who have already undergone treatment. If your health suddenly deteriorates, you must call an ambulance. It is possible that emergency surgery will be required.
Self-medication is strictly prohibited. The wrong choice of drug can be fatal.
Installation of a pacemaker
This is a type of surgical treatment during which the surgeon implants a device in the patient whose task is to maintain normal heart conduction and rhythm. Installation of a pacemaker has no contraindications. In other words, the operation can be performed even on children.
In rare cases, the device is rejected by the body. Typically, this occurs in 2-8% of elderly patients.
Donor organ transplantation
This is a radical operation, which is performed only if it is impossible to save the patient’s life using other methods. Donor organ transplantation is performed only on persons under 65 years of age.
Contraindications are serious pathologies of internal organs, which in practice is very rare, since, for example, both atherosclerosis and ischemia are on the list of restrictions.
Bypass surgery
The essence of the operation is to expand the lumen of the affected blood vessels. As a rule, this type of surgical intervention is prescribed for severe atherosclerosis.
This is a disease in which plaques consisting of “bad” cholesterol settle on the walls of blood vessels. They narrow the lumen, as a result of which the heart does not receive the required amount of oxygen and nutritional components.
The natural consequence is tissue necrosis.
If the lumen is completely blocked by plaques, the surgeon creates a new vessel to bypass the affected one. This can significantly improve tissue nutrition and, accordingly, heart function.
Aneurysm removal
This is a specific bulge that most often forms in the area of the left ventricle or the posterior wall. After the aneurysm is removed, the blood stops stagnating, and the heart muscle again receives the necessary amount of nutrients and oxygen.
Why are scars dangerous?
Many patients are interested in how long they live with a scar on the heart. It is important to understand that the prognosis depends not only on the underlying disease, but also on the timeliness of seeing a doctor. What is it, the causes of scars on the heart, how to treat the pathology - the cardiologist provides all information regarding the disease during the appointment.
The most unfavorable prognosis is considered if the scar has formed in the area of the left ventricle. This area is subject to the greatest load, which means its damage will invariably lead to the development of heart failure. In addition, other organs (including the brain) will begin to suffer from hypoxia, not receiving the required amount of oxygen.
A condition in which both the left ventricle and the mitral valve are affected is also a life-threatening condition. In this case, a life-threatening pathology develops - aortic stenosis.
If you consult a doctor in a timely manner and follow all recommendations, the patient has every chance of living a very long time.
Prevention
Cardiosclerosis is a disease of the cardiovascular system. In this regard, both primary and secondary prevention consists of observing the following rules:
- Balanced diet.
- Regular but moderate physical activity.
- Quitting smoking and drinking alcoholic beverages.
- Avoiding getting into stressful situations.
- Frequent walks.
- Spa treatment.
In addition, it is necessary to be examined annually by a cardiologist in order to prevent pathologies of the cardiovascular system.
Finally
Sometimes, based on research results, the doctor diagnoses a “scar on the heart.” What does this concept mean? A heart scar is a pathological condition that is a kind of protective reaction of the body to myocardial damage.
The formation of dense connective tissue is triggered when the integrity of the muscle is damaged or when areas of necrosis appear on it. Despite this, the pathology needs treatment. It is important to understand that scar tissue cannot perform the functions of the heart, which means that sooner or later it will cause the development of other diseases.
The doctor draws up a treatment regimen based on the results of instrumental diagnostics. The treatment plan may include both conservative and surgical methods.
Source: https://labuda.blog/230542
Bypass surgery
The essence of the operation is to expand the lumen of the affected blood vessels. As a rule, this type of surgical intervention is prescribed for severe atherosclerosis. This is a disease in which plaques consisting of “bad” cholesterol settle on the walls of blood vessels. They narrow the lumen, as a result of which the heart does not receive the required amount of oxygen and nutritional components. The natural consequence is tissue necrosis.
If the lumen is completely blocked by plaques, the surgeon creates a new vessel to bypass the affected one. This can significantly improve tissue nutrition and, accordingly, heart function.
Why are scars dangerous?
Many patients are interested in how long they live with a scar on the heart. It is important to understand that the prognosis depends not only on the underlying disease, but also on the timeliness of seeing a doctor. What is it, the causes of scars on the heart, how to treat the pathology - the cardiologist provides all information regarding the disease during the appointment.
The most unfavorable prognosis is considered if the scar has formed in the area of the left ventricle. This area is subject to the greatest load, which means its damage will invariably lead to the development of heart failure. In addition, other organs (including the brain) will begin to suffer from hypoxia, not receiving the required amount of oxygen.
A condition in which both the left ventricle and the mitral valve are affected is also a life-threatening condition. In this case, a life-threatening pathology develops - aortic stenosis.
If you consult a doctor in a timely manner and follow all recommendations, the patient has every chance of living a very long time.
What to do if a scar is found?
Most often, cardiosclerosis is detected during an ECG, as well as during an ultrasound of the heart.
Note! If you have discovered such changes, then you need to seek help from a cardiologist and undergo annual examinations with him.
It is usually not the only condition that needs treatment, but is usually associated with coronary artery disease, hypertension and heart failure.
Cardiosclerosis on ECG
After a complete examination, based on the medical history, the doctor will prescribe a comprehensive treatment for all existing cardiac diseases. Of course, areas of connective tissue will not be able to turn into muscle tissue after treatment; the main goal of treatment in this case is to prevent further spread of the process and eliminate the symptoms of heart failure.
However, no treatment can stop the progression of cardiosclerosis unless you lead a healthy lifestyle and adhere to a diet.
The diet should primarily limit animal fats and should be aimed at reducing consumed cholesterol. Moderate physical activity is very important to prevent the spread of cardiosclerosis.
A sedentary lifestyle and obesity are the main causes of all serious diseases, including cardiac diseases.
In conclusion, I would like to say that almost every person over 50 years of age learns during an ECG that there are areas of cardiosclerosis in his heart.
This condition is the beginning of coronary heart disease and requires serious attention to your lifestyle and often even taking medications.
The main goal of treatment is to stop the further spread of scar tissue throughout the heart muscle, ensure the survival of all remaining muscle tissue, and control and treat all cardiac diseases. To prevent the spread of atherosclerosis through the vessels of the heart, strict control over the level of cholesterol and lipids in the blood, a diet limiting animal fats, and taking cholesterol-lowering drugs are necessary.
The ECG showed large focal cicatricial changes in the anterior wall of the left ventricle. Sent for consultation to a cardiologist. The presence of scars in the heart was confirmed by cardiac ultrasound. Vladimir suffered a myocardial infarction and did not pay attention to it; he also never measured his blood pressure, which turned out to be elevated.
The patient was prescribed cholesterol-lowering drugs, aspirin for blood thinning, drugs for the treatment of arterial hypertension, and dietary recommendations were given. A follow-up appointment is recommended in two weeks to determine further treatment tactics and examination.
Brief background: Scars in the heart are areas of connective tissue that most often appear after a myocardial infarction.
At the site of scarring, the heart muscle gradually loses its ability to contract, and heart failure develops and progresses. In order not to miss the appearance of such changes in the heart muscle, it is necessary for all people after 50 years to undergo an ECG annually.
Prevention
Cardiosclerosis is a disease of the cardiovascular system. In this regard, both primary and secondary prevention consists of observing the following rules:
- Balanced diet.
- Regular but moderate physical activity.
- Quitting smoking and drinking alcoholic beverages.
- Avoiding getting into stressful situations.
- Frequent walks.
- Spa treatment.
In addition, it is necessary to be examined annually by a cardiologist in order to prevent pathologies of the cardiovascular system.