When making an appointment with a doctor, we expect qualified assistance - a correct diagnosis and prescription of effective treatment. Often, an inspection and survey alone is not enough. For better treatment, the doctor prescribes tests and the necessary types of instrumental diagnostics.
A relatively inexpensive but valuable method in cardiology is ECG (electrocardiography). A referral for examination can be issued by a local internist and a specialist - a cardiologist, rheumatologist, or endocrinologist. Using the information obtained from an ECG, all deficiencies in the functioning of the heart are assessed and areas of impaired blood supply are identified. They also undergo electrocardiography for the purpose of early diagnosis of vascular and heart diseases.
If you feel pain in the chest, increased heart rate after a slight exercise, arrhythmia (irregular rhythm), increased blood pressure or shortness of breath, increased sweating and a feeling of weakness, you should consult a doctor and ask to be examined and have an ECG.
Who performs the ECG procedure
When making an appointment for diagnostics, the question arises: “ Which doctor does the ECG? » The procedure is usually performed by a nurse with special training. The result of the study is deciphered only by a functional diagnostics doctor who has the first specialization - a cardiologist. An ECG examination can be performed by a cardiologist if equipment is available in the office or when called at home.
It is recommended to conduct the examination two hours after eating, and you should not smoke 2 hours before the procedure. The procedure begins after the patient has calmed down or rested for at least 15 minutes. In emergency situations, no preparation is carried out, and the examination is done immediately.
Electrodes are placed on the skin in certain places - in the chest, forearms and lower legs. The skin is lubricated with gel to improve electrical conductivity. Therefore, take a shower before the procedure and do not use body cosmetics.
Source: artixstudio.ru
Electrocardiography at home
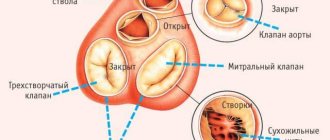
Electrical cardiography of the heart is a method that allows you to record impulses of the heart muscle that occur during the period of contraction and relaxation of the organ over a certain period of time.
Pulses are recorded using a device – an electrocardiograph. It helps convert electrical impulses into graphic patterns. The data is recorded on special paper in the form of a complex curve, called an electrocardiogram. Cardiac pathologies are quite common, especially in elderly patients. Sometimes it is difficult for a person to visit the hospital on his own, so in some cases an ECG is performed at home to obtain a cardiogram.
The peculiarity of the procedure is that diagnostics are performed using special portable equipment. Modern portable devices provide accurate data and are not much inferior to stationary devices.
ECG at home is performed using special portable devices
What is an ECG?
Electrocardiography is a non-invasive technology for graphically recording the potential difference in the electric field generated during the work of the heart. It is carried out using an electrocardiograph.
The device has electrodes that are attached to certain points on the patient's body. They capture the electrical impulses of the heart, which, after amplification, are recorded by a galvanometer and recorded on paper using curved lines. The result is a cardiogram, which is subject to further interpretation by a cardiologist or therapist.
Goal and tasks
Taking an electrocardiogram is necessary for diagnosing disorders of the heart, and is also a mandatory element of the annual medical examination of the population. Cardiologists recommend an ECG every year for all people over 40 years of age.
Looking at the cardiogram, the doctor will evaluate:
- Frequency (pulse), rhythm and regularity of heart contractions.
- Physical condition of the heart.
- The presence of disturbances in electrolyte metabolism (potassium, calcium, magnesium and others).
- Conducting system of the heart (various blockades and arrhythmias).
- The effectiveness of treatment in acute and chronic diseases.
- Localization, size and degree of damage during ischemia and myocardial infarction.
- The presence of cardiac complications in diseases of other organs and systems (pulmonary embolism).
Reasons to get tested
A cardiogram is done at the slightest complaint:
- for interruptions in heart function;
- shortness of breath;
- heaviness and pain in the chest;
- weakness, dizziness;
- high blood pressure;
- pain in the back, chest and neck.
And:
- before operations;
- at medical examinations;
- during pregnancy;
- if there is a risk of developing heart disease;
- to obtain a medical record when applying for a job.
What kind of doctor does it?
At the clinic, a referral for cardiography is given by a therapist. And the doctor who deciphers it is called a cardiologist.
The following can also be concluded:
- functional diagnostics doctor;
- emergency doctor;
- Family doctor;
- pediatrician.
The procedure itself is carried out by nurses in a specially equipped room.
Duration of the procedure
How long the study will last depends on the type of ECG.
| Type of study | Time |
| Standard ECG | 5–10 minutes |
| ECG with stress | 10–15 minutes |
Additional types of research
In addition to the standard method, Holter monitoring and stress ECG are widely used in medical practice. These types of diagnostics make it possible to record cardiac impulses over a longer period of time or during physical activity.
Holter monitoring
Holter monitoring is used to assess cardiac activity over a 24-hour period or a longer period. The method involves attaching electrodes and a special battery-powered device to the human body. After this, the patient is asked to lead a normal lifestyle for 24 hours. Sometimes the specialist may ask the patient to do physical exercises.
During the study, a person needs to record data in a special diary. Here he must indicate what exactly he did, whether there were any worries or physical activity. After the procedure is completed, the electrodes are removed from the body, and the data from the device is printed in the form of a cardiogram.
Normally, the cardiogram will show the following values:
- heart beats during wakefulness - from 60 to 100 per minute;
- heart beats during sleep – from 40 to 80 per minute;
- changes in heart rate when changing activities;
- ventricular extrasystoles are not observed normally. Up to 200 pieces are allowed;
- QT interval – women – 340 – 430 ms, men – 340 – 450 ms.
Cardiogram indicators with ECG with stress
During a stress ECG, the patient must perform various physical exercises. This helps evaluate the functioning of the heart muscle at rest and during exercise.
This type of research, unlike previous methods, has a number of contraindications. These include:
- serious heart defects;
- myocardial infarction;
- cardiac congestive failure;
- severe forms of unstable angina;
- inflammatory diseases of the heart muscle;
- stage 3 hypertension;
- the presence of blood clots in the vessels;
- patient's pacemaker.
During the study, the doctor asks the patient to perform physical activity for 60 seconds. At rest, a person's heart rate ranges from 60 to 90 beats per minute. After squats, this amount should increase by no more than 20%.
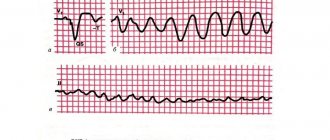
An increase in heart rate to 30–50% indicates the presence of any cardiac pathologies. Coronary heart disease may be indicated by changes in leads V 4, 5, 6 in the form of horizontal depression of the ST segment. The same changes can be observed in coronary insufficiency. With unstable angina, the cardiogram shows a distortion of T waves and a displacement of the T wave.
A specialist should decrypt the data. Based on the data obtained, the doctor selects the necessary treatment.
Preparing for the examination
Rules for preparing for an ECG:
- On the day of the procedure, you should refrain from drinking coffee, tea and energy drinks.
- Do not eat heavy food 2 hours before the test.
- Do not take sedative medications. If you regularly take cardiac medications (antiarrhythmics, beta blockers, cardiac glycosides), be sure to inform your doctor about this.
- Smokers should stop smoking an hour before the ECG.
- Do not expose yourself to physical stress. It is advisable to arrive 10–15 minutes before the examination and relax on the couch.
- Do not use greasy cream or lotion in the chest area.
- Clothing should be comfortable so that you can quickly expose your wrists, legs and chest. You will also have to remove all metal jewelry and watches.
- Be sure to take your previous cardiograms and test results with you.
How is the examination carried out?
- chest pain;
- feeling of palpitations after minor exertion;
- rapid, arrhythmic pulse;
- dyspnea;
- increased blood pressure;
- weakness, sweating;
- medical examination
Having understood what an ECG is, let’s find out how the examination is carried out. The advantages of this diagnostic method include painlessness, information content, and the possibility of examination in an outpatient clinic and at home.
To carry out the procedure, the patient must appear at the appointed time. In the office you will need to undress to the waist and lie down on the couch. After this, the medical worker lubricates the body with a special agent and attaches the electrodes. Sometimes the specialist may ask you to hold your breath, after which you can breathe at your usual rhythm.
ECG lasts no more than 7–10 minutes
The duration of the procedure is from 10 to 15 minutes. At this time, the patient does not experience any pain. To obtain reliable data, it is recommended to breathe calmly and try not to worry.
General algorithm of actions when taking an ECG
How to do an ECG:
- The health worker writes down all the patient's data in a journal.
- The wrists, legs and chest are exposed.
- Electrodes are attached while lying down. Before this, the skin is degreased with alcohol, and for better contact with the sensors, a special gel is applied, or wet gauze wipes are used.
- The indicators are recorded on paper, after which the terminals are removed and the skin is wiped dry.
Breathing should be smooth and calm. It may be necessary to record inspiratory readings. In this case, the nurse will instruct you to take a deep breath and hold your breath.
ECG manipulation is carried out in the functional diagnostics room. The room should be warm and isolated from possible sources of electrical interference. It is also recommended to turn off your mobile phone.
How to take an ECG correctly
The technique for performing electrocardiography has a simple procedure and is carried out in stages:
- patient preparation;
- application of electrodes;
- recording bioelectrical activity on paper;
- deciphering the results.
It is important not to confuse the electrodes, but to check the device for serviceability before use.
A video about the ECG recording technique was filmed by the channel - OFFICIAL TNU.
Application of electrodes
To record standard and enhanced leads, three electrodes (red, yellow and green) are used, which are placed on the arms and left leg and form an Einthoven triangle. The black electrode, which is placed on the right leg, grounds the system.
You need to set them like this:
- red - right hand;
- yellow - left hand;
- green - left leg;
- black - right leg.
To record the chest leads, one or six pear-shaped electrodes are used (depending on the type of cardiograph).
How to place chest electrodes:
- lead V1 - in the IV intercostal space along the right edge of the sternum;
- lead V2 - in the IV intercostal space along the left edge of the sternum;
- lead V3 - between the second and fourth positions;
- lead V4 - in the 5th intercostal space along the left midclavicular line;
- lead V5 - at the same horizontal level as V4, along the left anterior axillary line;
- lead V6 - along the left midaxillary line at the level of V4.5.
Marking of tips and electrodes
For convenience, all electrodes have their own color.
The location of the four main ones is easy to remember from a traffic light or from a funny reminder “Every Woman Is Meaner Than the Devil.”
In a single-channel cardiograph, one white bulb is used to take chest leads on an ECG.
In six-channel:
- V1 - red;
- V2 - yellow;
- V3 - green;
- V4 - brown;
- V5 - black;
- V6 - blue.
Lead diagram
When recording an ECG, 12 standard leads are currently used: 6 from the limbs and 6 from the chest.
Each of the 6 leads shows one or another part of the heart.
On standard leads:
- I - anterior cardiac wall;
- II - posterior cardiac wall;
- III - their totality.
On reinforced leads:
- aVR - lateral cardiac wall on the right;
- aVL - lateral cardiac wall anterior to the left;
- aVF - posterior inferior wall of the heart.
On the chest leads:
- V1 and V2 - right ventricle;
- VZ - septum between the two ventricles;
- V4 - upper cardiac section;
- V5 - anterior lateral wall of the left ventricle;
- V6 - left ventricle.
This simplifies the task of diagnosing diseases. Changes in each lead characterize the pathology in a certain area of the myocardium.
Recording a cardiogram
The procedure may differ on different cardiographs. Let's consider the ECG recording algorithm using the EK1T-03M2 device as an example.
If the device is powered from a 220V network, it must be grounded. To do this, one end of the ground wire is connected to the ground socket, and the other is connected to a water tap or an unpainted area of the central heating radiator. Devices with a battery do not require grounding.
After applying the electrodes and turning on the device, the control millivolt is recorded. This is the recording scale, it is important for further measurements and for comparing electrocardiograms recorded on different devices with each other.
Using the EK1T-03M2 device as an example, this is done like this:
- The switch should set the mV height to 10 mm, check that the lead switch is set to 1 mV.
- Turn on the belt movement at a speed of 50 mm/sec. And immediately quickly press the millivolt recording button 3-4 times, then stop the tape movement.
- Several rectangular teeth 10 mm high will be recorded on the tape; when deciphering an ECG, they are called millivolts.
Next, the standard leads are recorded sequentially:
- To do this, switch the device to lead I recording mode.
- Then turn on the tape, record 4-5 complexes and stop the tape.
- Switch the device to lead II recording mode and repeat the entire procedure.
- After recording lead III, the patient should be asked to take a deep breath, hold his breath, and in this position record lead III again.
- Then record the enhanced leads aVR, aVL and aVF.
Recording chest leads:
- To do this, set the lead switch to position V.
- The chest electrode is placed on the patient's chest at the recording point of lead V1 and the pen stabilizer is turned on.
- The sedative is turned off. Record at a speed of 50 mm/sec. 4–5 complexes.
- The pacifier is turned on and the electrode is moved to point V2.
- The entire procedure is repeated until lead V6 is recorded.
The control millivolt is recorded again, the tape is passed forward and torn off. The device is turned off.
The cardiogram indicates:
- Patient's full name;
- age;
- date and time of recording.
Indications for use
Although cardiography is a routine research method, it also has indications. To determine the cause of pain or discomfort in the chest area, the patient consults a therapist or cardiologist. The doctor initially collects anamnesis, examines, measures blood pressure and pulse, auscultates the heart, and then sends it for examination to find out what the cardiogram shows.
Indications for ECG:
- chest pain (suspicion of angina or myocardial infarction);
- dyspnea;
- discomfort in the heart after viral or bacterial infections;
- pathological heartbeat, interruptions in the functioning of the heart muscle.
An ECG is mandatory in the following cases:
- when hospitalized in an inpatient department of any profile;
- before surgical interventions;
- during preventive examinations of adults;
- for schoolchildren when choosing a group of physical education classes.
An electrocardiogram of the heart is used both for the primary diagnosis of pathological conditions and for monitoring the dynamics of the disease. When prescribing drugs, the doctor relies on both the patient’s subjective sensations and ECG data, which reflect actual changes in the cardiovascular system.
A cardiac cardiogram can detect many diseases. This type of study is prescribed to patients with the following conditions:
- suspicion of myocardial infarction and detection of other diseases of the cardiovascular system;
- assessment of the effectiveness of therapy for heart attack, coronary heart disease, arrhythmias, heart defects and other pathologies;
- patient complaints of pain and burning in the chest, shortness of breath, rapid heartbeat;
- to assess the activity of the heart muscle before upcoming surgery;
- in order to identify abnormalities in the functioning of the cardiovascular system in patients with a long history of smoking, after infectious diseases, and with elevated levels of cholesterol in the blood;
- men after reaching 40 years of age, women after 50 years of age;
- carrying out preventive examinations.
Any patient complaints regarding the functioning of the heart may be a reason for conducting electrocardiography.
Features of ECG according to Slopak
In medicine, there is another way to conduct electrocardiography - ECG according to Slopak. It differs from the standard procedure. Used to diagnose posterobasal myocardial infarction.
Description of the method:
- Green - left leg.
- Black - right leg.
- The yellow electrode is placed on the fifth intercostal space on the left along the posterior axillary line (at the level of thoracic V6).
- Red is moved sequentially and used to remove the chest leads.
The marking looks like this:
- S1 - at the left edge of the sternum;
- S2 - in the middle of the distance between leads S1 and S3;
- S3 - second intercostal space on the left along the midclavicular line;
- S4 - second intercostal space on the left along the anterior axillary line.
In this case, the contact switch must remain in position I.
How to do an ECG for women
ECGs are done for women in the same way as for men. The only peculiarity is that the girls take off their bra, since the impulse does not pass through the fabric of the bra. For the same reason, it is not advisable to wear tights or stockings.
Are there any special features during pregnancy?
There are no contraindications for ECG during pregnancy. This is the same stage of monitoring the health of the expectant mother as an ultrasound. That is why women should not refuse to perform such a study.
During pregnancy, the heart experiences increased stress. During pregnancy, an ECG is prescribed 2 times. In addition, an electrocardiogram is performed not only on the woman, but also on the fetus - this study is called CTG (cardiotocography).
During pregnancy, the following changes appear on the cardiogram:
- displacement of the electrical axis of the heart to the left;
- increased heart rate, single extrasystoles;
- negative T wave in the third and fourth leads;
- shortened PR interval;
- pathological Q wave in the third lead and aVF (right arm lead).
What can be seen on a cardiogram
Electrical cardiography is a method that is quite widely used in modern medical practice. The procedure allows you to identify abnormalities in the functioning of the cardiovascular system in a short time, which allows you to select the necessary treatment for the patient and prevent the development of complications.
Using the described method, doctors can recognize the following diseases in a person:
- hypertrophy of the heart. This condition is indicated by such ECG changes as an increase in the interval of impulse conduction, a change in the cardiac electrical axis, and a violation of the amplitude of the waves. Hypertrophy occurs due to overload of the heart parts against the background of hemodynamic disturbances;
- IHD, angina pectoris. In this case, the cardiogram will show a violation of the QRS complex, depression of the S-T segment, a change in the T wave;
- arrhythmia. Arrhythmias of various origins are accompanied by disturbances in the heart rate. The cardiogram will show changes in P – Q, R – R, Q – t complexes.
In addition, electrical cardiography allows us to identify various heart defects, aneurysms of the heart muscle, inflammation of the myocardium and many other pathologies. You can read more about interpreting ECG for various diseases here.
Decoding indicators
ECG is assessed according to several criteria:
- The rhythm is correct and regular. No extraordinary contractions (extrasystoles).
- Heart rate. Normally - 60–80 beats/min.
- Electrical axis - normally R exceeds S in all leads except aVR, V1 - V2, sometimes V3.
- Width of the ventricular QRS complex. Normally no more than 120 ms.
- QRST - complex.
Brief designation of the main elements of the film:
- P wave - shows atrial contraction;
- PQ interval is the time the impulse reaches the atrioventricular node;
- QRS complex - shows ventricular excitation;
- T wave - indicates depolarization (restoration of electrical potential).
Video about ECG norms from the Mass Medika channel.
Cardiogram of the heart in children
Like adult patients, children are prescribed electrocardiography for preventive purposes or when signs indicating the development of cardiovascular pathologies appear.
If it is necessary to conduct an ECG for a child, parents must properly prepare the child for the examination. Before doing this, it is important to explain to your child that the procedure is painless and there is no need to worry. For school-age children, the essence of the method can be shown in pictures or videos.
Features of ECG indicators when interpreted in childhood include the following aspects:
- sinus respiratory arrhythmia in some cases is considered normal;
- the ventricular complex may have alternation of teeth;
- within the atria there may be a change in rhythm sources;
- intervals of electrocardiogram readings in young children are shorter than in adults;
- in newborns there is sometimes a predominance of the right ventricle of the heart.