Gas Bubble Promotion
Patients are most concerned about medical procedures: injections and blood sampling for analysis. A small air bubble is called an embolus in medical parlance. Let us remind people who are not familiar with anatomy: through the veins, blood always tends to the right atrium. To do this, the heart and diaphragm create a suction action, the walls of the blood vessels push the fluid, preventing it from reversing.
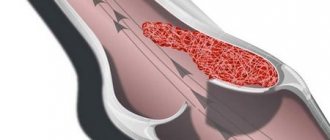
When an embolus enters the blood (regardless of the location), it necessarily moves towards the heart. If it is small, then along the way it is absorbed by the vascular walls and disappears. Only a large bubble blocking the right atrium can cause harm.
If you introduce air not into a vein, but under the skin or into a muscle, it will be absorbed by the surrounding tissues. In medicine, there is a special method for treating endarteritis of the legs - subcutaneous injection of oxygen into “starving” tissues.
Diagnosis of VE
To correctly diagnose an air embolism, it is most important to identify the possible causes of its occurrence in the patient, that is, to collect a complete medical history. The symptoms of VE themselves can be observed in many diseases. However, indication of recent diving or surgery may be a starting point in making a diagnosis.
If a patient is suspected of having an air embolism, doctors may order the following tests to identify it:
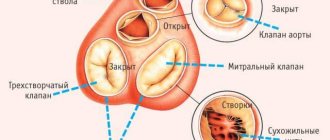
- Auscultation of the heart - if air has accumulated in the cavity of the heart, a “mill wheel” noise can be heard using a stethoscope.
- Chest X-ray - sometimes reveals gas bubbles.
- Doppler ultrasound is a non-invasive examination that evaluates blood flow in the vessels. Allows you to detect air bubbles in the heart and blood vessels of the brain.
- Transesophageal echocardiography is a method of ultrasound examination of the heart that allows you to detect air in its cavity.
- Computed tomography and magnetic resonance imaging - these methods can help detect air emboli in the central nervous system.
Causes of embolism
They are associated with pathological conditions and violations of the technique of intravenous manipulation. Some cases are caused by an attempt on human life.
The wall of the vessel is delimited from the surrounding tissues, so even if air appears in them, it will be impossible to let it into the vein. Another thing is conditions when a rupture of a large main vessel occurs (open fractures of the pelvis, femur, ribs). An entrance gate is formed through which air is sucked in. A severe infection - gas gangrene - contributes to the “corrosion” of the vascular wall, breaking its tightness.
Chest surgery
When performing operations on the thoracic and abdominal organs, the surgeon always takes into account the risk of damage to large vessels. Clamps are temporarily applied not only to prevent bleeding, but also to prevent air from entering large veins with serious consequences.
In hospitals, catheterization of the subclavian vein is used for long-term infusion therapy. The manipulation is carried out by anesthesiologists or surgeons. If the needle is directed incorrectly or the vessels are atypically positioned, they often end up in the artery. An experienced doctor will immediately notice the scarlet color of the blood and noticeable pulsation. If it is not possible to distinguish in time, a small bubble can enter the arterioles of the heart, lungs or brain.
When connecting an IV to a correctly installed catheter, the hole is open for a moment, and there is a danger of letting in a small volume of air. Doctors always cover the needle with a finger.
Criminal cases are difficult to prove. The expert is always alarmed by the presence of an injection mark, the absence of obvious signs of serious illness, and the suddenness of death.
Consequences of air ingress
Situations in which air ends up in a vein are called embolism in the medical literature. They happen extremely rarely, but if they do occur, the following can happen in the body:
- Blockage of a vessel. The likelihood of this result is highest in people who have atherosclerotic plaques and suffer from hypertension. In both cases, vessel patency is reduced, which increases the likelihood of blockage
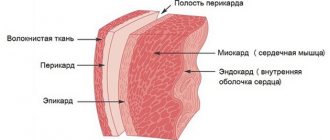
- Atrial stretch. Air that has entered the circulatory system and freely reaches the myocardium is collected in the right part of the myocardium, from where it is not able to freely exit. If its amount is quite high, muscle tissue is stretched, which has an extremely negative effect on the functioning of the heart, causing arrhythmia, paroxysms and more serious dysfunctions.
- Death. Occurs when an exorbitant volume of air (from twenty cubic meters) is introduced into a vein. The likelihood of its occurrence is greatly increased in people with cardiovascular diseases
Despite the fact that the possibility of air entering the circulatory system during an intravenous injection or placement of a drip cannot be completely excluded, doctors assure that its volume cannot cause significant harm to a healthy person. Dangerous consequences are fraught only with the deliberate introduction of an impressive amount of air or its accidental penetration during surgery, injury, childbirth, or in other emergency situations.
Is it possible to have a heart attack or stroke?
The mechanism of a heart attack or stroke is a sudden blockage of the arteries supplying the heart muscle or brain.
The heart and brain have their own blood circulation. The coronary arteries arise directly from the aorta, and the cerebral arteries arise from the internal carotid and subclavian arteries.
To form a zone of infarction or cerebrovascular insufficiency, the gas must overcome the barrier between the venous and arterial parts of the blood flow. A similar mechanism appears in patients with heart defects when communication is maintained through a “window” in the septum separating the right from the left (arterial) sections.
Air embolism - diagnosis and first aid
An air embolism is a blockage of a vessel by an air bubble. It is rare, but carries the risk of death if medical attention is not received in a timely manner.
Types of disease
Air embolism is divided into types:
- Obstetric embolism. Occurs due to incorrect management of obstetric care (uterine perforation, cervical rupture, vaginal rupture).
- Traumatic embolism. Develops in an operating or traumatic wound located above the level of the right atrium.
- Air embolism due to blood transfusions or therapeutic injections.
- Gas embolism occurring due to decompression when pressure increases.
Causes of pathology
- Air bubbles end up in the bloodstream for a variety of reasons. If the walls of blood vessels are damaged during inspiration, air is sucked through the injured vein.
- The world-famous Russian scientist N.I. Pirogov established the following: death occurs during air embolism not from air emboli entering the vein, but from how quickly they arrive.
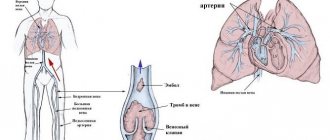
- The pathology is provoked by the entry of an air bubble into the patient’s bloodstream. Through the right side of the heart, air is directed into the pulmonary artery, embolizing it. Due to mechanical obstacles, blood circulation stops. There is a sudden deterioration in the patient's condition.
During a blood transfusion, a characteristic hissing sound is heard when air enters the vein.
Immediately the patient exhibits nervous agitation, chest pain, and severe shortness of breath. The lips and face turn blue, and there is a sharp drop in blood pressure.
Why does pathology develop?
The causes of air embolism are:
- Chest injuries. Air bubbles rush along the pressure gradient into the vessel. The blood flow is blocked. The development of an air embolism is dangerous due to bleeding from damaged veins of the chest: the pressure decreases during inspiration, which leads to air being sucked in.
- Blood transfusion. The air bubble, passing through the right side of the heart, embolizes the pulmonary artery.
- Incorrect intravenous injection technique. Air bubbles along with the drug are introduced into the blood.
- Surgical injuries to the chest and head.
- Improper obstetric care, abortion. Venous ruptures of the placenta.
- Gas embolism in divers. In the case of incomplete exhalation of air when rising from depth, the air in the lungs expands. The lungs become inflated and gas bubbles remain in the bloodstream.
- When gas emboli enter the arteries of the brain, blood circulation is blocked, which leads to unconsciousness.
Symptoms of pathology
Signs of pathology due to air embolism:
- limbs weaken;
- the skin turns pale;
- dizzy;
- a moving tingling sensation is felt;
- rashes appear on the skin;
- joint pain is observed;
- blueness of the face and limbs;
- increased heart rate;
- speech disorder;
- increased blood pressure;
- loss of coherent speech;
- the appearance of a cough with bloody discharge.
Rarely recorded symptoms:
- loss of consciousness;
- manifestation of cramps in the limbs;
- paralysis if an air embolus has blocked an artery in the brain;
- absorption of air through the lumen of a large vein. Perhaps when a person inhales. At the same time, a sound similar to squelching and gurgling is heard.
Even a single intake of air provokes a dangerous pathology - an air embolism.
Small portions of sucked air, unless they are repeated, are unable to provoke serious consequences. A large volume of air or foamed blood entering a vein causes dangerous symptoms:
- attacks of unreasonable fear;
- feeling of melancholy;
- motor overexcitation.
Fainting, convulsions, and collapse often precede death.
Diagnosis of the disease
Diagnosis of the disease is carried out by examining the patient. If the patient has not lost consciousness, signs of air embolism can be observed:
- labored breathing;
- pain in the heart;
- dry cough.
Often these symptoms are followed by loss of consciousness.
In an unconscious state, the diagnosis of air embolism is confirmed by the following symptoms:
- tachycardia;
- hypotension;
- swelling of veins.
Diagnosis uses a stethoscope, ECG, ultrasound, and magnetic resonance imaging. Central venous pressure must be measured.
To diagnose sudden death, the following is done: the heart is placed under water and the right side is punctured. If air bubbles come out of the heart cavity, then the cause of death is an air embolism.
Providing emergency assistance
An air embolism requires immediate medical attention; delay threatens the life of the victim.
The patient is urgently sent to a medical institution for assistance. With proper resuscitation measures, air bubbles dissolve and the pathology disappears.
Treatment options for air embolism
The victim is placed on his left side, his head slightly lowered. Transportation in an ambulance is carried out using a stretcher in a prone position. The legs are raised slightly to reduce the chance of air entering the heart and brain.
Air bubble extraction technique
If the integrity of the vein is compromised and air enters the resulting lumen, the doctor closes it with the tip of the left index finger. Artificial respiration is carried out using an anesthesia machine.
In this case, venous and arterial blood transfusions are performed. The area of damage to the vein is limited with ligatures. A catheter is inserted into the vein and connected to a Janet syringe. The syringe makes it possible to extract about 150 mg of blood with air bubbles in it. Further actions should be aimed at eliminating the entry of air.
The operating table tilts to the left as the end where the head is located is lowered. In this case, air becomes trapped in the right atrium.
It is necessary to begin aspiration of air from the central vein using a catheter. If the air bubble has migrated to the brain, HBOT is used.
The patient should assume the Grendelenburg position, characterized by an inclined position of the torso with the head down. In this position, it is easier to capture the air embolus in the upper part of the ventricle if it reaches the heart.
And also at the same time, the speed of the moving air bubble will slow down, which will not be able to reach the heart. If the air bubble reaches the heart, cardiopulmonary resuscitation is urgently needed.
Treatment with a hyperbaric chamber
An effective way to get rid of a dangerous pathology is a pressure chamber in which the victim is placed. In a hermetically sealed chamber, the pressure is increased, which causes air bubbles to dissolve.
The body gets rid of the disease. After this, the pressure slowly decreases, the gas mixture saturated with oxygen is calmly inhaled by the patient. Gas leaves the body slowly, and air bubbles do not re-form.
Prevention of pathology
Prevention of air embolism during surgical interventions on veins and during intravenous injections - prohibition of manipulations without the application of a provisional and closed sphincter.
To prevent pathology, you need a properly installed blood transfusion system, professional performance of the blood transfusion procedure, prohibition of manipulations without the application of a provisional and closed sphincter.
Disease prognosis
The outcome of the pathology largely depends on the timely diagnosis of the embolic process. When air enters in a small amount, air bubbles, bypassing the heart and pulmonary trunk, stop in small vessels. They will quickly dissolve, the manifestations of the disease will disappear. It will take two hours to completely eliminate them.
This condition often causes a gas embolism in the brain.
With a mild course, the pathology will manifest itself as symptoms of an unstable nature. Severe cases can lead to seizures and death.
The considered pathological processes affect not only the professional activities of doctors; sometimes injections are carried out at home. You can get dangerously injured at home.
Providing first aid to a victim, calling an emergency ambulance is a chance to save a human life.
Source:
Pathogenesis of the disease
Embolic complications can accompany a number of conditions. Therefore, it is important to know the signs of this pathology and be able to provide the necessary assistance.
Air embolism is a life-threatening condition in which the vessels of the systemic or pulmonary circulation are blocked by an air bubble. This is a frequent accompaniment of traumatic injuries and improper medical procedures.
Some authors refer to air embolism as a type of vessel blockage such as gas embolism. Both of these conditions have clinical features and different causes of occurrence. The pathophysiology of these processes also differs. All this will be discussed below.
Source: https://krovinushka.ru/zabolevaniya-krovi/vozdushnaya-emboliya.html
What is the difference between gas embolism in divers?
For divers, the main role is played by nitrogen, which is constantly present in the blood. The profession involves maintaining the relationship between ambient pressure (increases significantly at depth) and the state of the dissolved gas mixture. When lowering, the amount of nitrogen in the blood increases 4 times. If the rise is slow, microbubbles are transferred to the lungs and exhaled into the machine. With accelerated ascent, the volume of nitrogen does not have time to decrease, it “boils”.
Embolism in divers
The bubbles form emboli to which platelets attach. Gas embolism causes death from severe damage to the vascular system.
Etiology
Air cannot spontaneously enter the systemic circulation because intravascular pressure is much higher than atmospheric pressure. It prevents the absorption of gases during the destruction of blood vessels. When the body is dehydrated, the situation changes. As the volume of circulating blood decreases, the pressure in the great vessels drops. If their integrity is violated, air from the outside penetrates inside.
For an air embolism to occur, 15-25 ml of gas must immediately enter the lumen of the vessel. A smaller volume of air dissolves in the capillaries and does not cause any harm to the body.
Air embolism is a multifactorial disease. Its main reasons include:
- Various injuries - injuries to the chest with rupture of the vessels of the lungs and heart, blunt and penetrating injuries to the abdomen, neck and craniofacial region. Atmospheric gases enter the blood during continuous profuse bleeding.
- Delivery - during contractions, the uterus actively contracts, which helps to force air into the damaged veins of the placenta. Symptoms of the disease appear immediately or a couple of days after birth. Obstetrics and gynecology procedures carry a certain risk of air embolism.
- Invasive therapeutic and diagnostic procedures with violation of technique - operations on blood vessels, chest organs, brain; central vein catheterization; hemodialysis; infusion and blood transfusion therapy; X-ray contrast angiography; lung biopsy. Air remaining in the syringe can lead to irreparable consequences. Neurosurgical procedures and otolaryngological procedures performed in a sitting position are the most common iatrogenic causes of this complication.
- Pulmonary barotrauma can occur during a sharp rise from depth to the surface of a reservoir. When a person dives, he retains air. During a rapid ascent, the pulmonary system does not have time to remove its excess. Lung destruction is most often observed in divers and scuba divers when they quickly dive into water or emerge from the bottom. Sudden pressure surges lead to the formation of carbon dioxide bubbles in the vessels, their damage and rupture of the alveoli. Gas bubbles enter the blood and embolization occurs.
The causes of the pathology must be assessed comprehensively. In order to prescribe quality treatment and relieve the patient of the problem, it is necessary to understand the origin of the air embolism and know exactly the location of the lesion. Otherwise, the prognosis for recovery will be significantly worse.
During intravenous procedures
Collection for analysis from the ulnar vein is carried out after applying a tourniquet in the shoulder area. This is necessary for a short-term delay in blood flow. By pulling the syringe piston or by gravity, blood comes out of the needle, while the formation of a bubble is impossible due to the increased pressure inside the vessel. If air enters the subclavian vein during catheter installation, subcutaneous crepitus (crunching on palpation) is simultaneously observed.
When an injection is given or a system for administering a solution is installed, medical personnel are obliged to monitor the patient’s well-being, reaction to the drug, and local pain.
Symptoms
Manifestations of VE with a small volume and gradual intake of air are usually difficult to identify, since the process in this case is asymptomatic.
In cases of a sharp drop in pressure in the vessels, pathology can manifest itself in different ways.
Signs of an air or gas embolism:
- joint or muscle pain;
- drop in blood pressure, resulting in dizziness;
- due to oxygen starvation, interruptions in the heartbeat are possible, an increase in the rhythm is more often observed;
- blurred vision;
- the appearance of skin itching;
- convulsive syndrome;
- foam comes out of the mouth (sometimes with blood);
- difficulty breathing, pain in the chest;
- feeling extremely tired, anxious or panicky;
- involuntary rapid movements of the body (tremor);
- impaired coordination of movements;
- the appearance of hallucinations of various types;
- Nausea may appear, sometimes accompanied by vomiting;
- cyanosis (blueness of the skin): first in the nasolabial area, then on the nails;
- the appearance of weakness or numbness in the arms and legs, up to paralysis;
- swelling of veins;
- dry cough;
- fainting (or loss of consciousness).
If a person experiences similar symptoms, then it is necessary to urgently consult a doctor to diagnose the cause of this condition.
It is very important to quickly recognize signs of VE when a diver ascends in order to immediately call an emergency medical team.
How to do intravenous injections correctly
Intravenous injections are prescribed in the complex treatment of diseases. The doctor writes in the referral how much is recommended for a particular patient.
Intravenous injection
Manipulation requires successive steps:
- a tourniquet is applied above the intended injection site (for the elbow area it is necessary to clamp the shoulder, for injections into the hand - the forearm);
- lightly pat the hand or massage from bottom to top until a clear picture of swollen superficial vessels appears;
- insert a needle along the direction of blood flow;
- after dark blood is released, the tourniquet is removed and the solution is slowly (some medications are very slow) injected.
You should draw the medicine into the syringe and remove the bubbles by pressing the piston before applying the tourniquet.
Causes: why does pathology occur?
There should be no air bubbles in a healthy vessel. When damaged, an embolus enters the vascular bed and moves further with the blood flow. The result is a blockage of the artery or vein. An air embolism can also develop as a result of treating large wounds with hydrogen peroxide, since the drug produces oxygen during the breakdown process. If emboli reach the vessels of the heart or brain, death is possible. In general, pathology occurs under the influence of the following unfavorable causes:
- open injuries and gunshot wounds;
- damage to the vascular bed during surgery;
- being in an explosion zone;
- air entering through the oval window of the heart from a vein into an artery;
- improper installation of intravenous infusion or injection systems;
- disturbances during the blood transfusion procedure;
- failure to comply with diving rules.
Return to contents
How to remove air from the system
When attaching a syringe to a needle, the nurse must be sure that the bubbles have been removed first. To do this, tap the body with a finger in a vertical position. The bubbles connect and rise up. Then they are squeezed out by a piston with some of the liquid.
When installing the system, the medical professional monitors the fluid level and regulates the rate of administration. The bubble is either squeezed out by lifting the cannula upward, or when shaking the tube it goes into the “control”. When the injected solution has run out and the nurse has not had time to remove the needle, the gas will not be able to get inside due to insufficient pressure. Therefore, there is no need to worry if an air bubble gets into the vein through the IV, it is impossible to die from this.
Devices for plasmapheresis and hemosorption are equipped with special filters that do not allow gaseous components to pass through. Safety is guaranteed throughout the entire procedure.
Ways to prevent pathology
Prevention of air or gas embolism primarily applies to cases that are associated with deep sea diving. Since they are the ones most often accompanied by the occurrence of VE.
Preventive measures to prevent the formation of air emboli:
- Limitation of time and depth during diving.
- You need to ascend slowly, stopping periodically so that gases dissolved in the blood can evaporate freely and safely.
- Do not dive if there are signs of a cold or cough.
- When diving into low temperature water, precautions are required (properly selected scuba suit).
- Before and immediately after diving, you must refrain from drinking alcohol.
- Enough time should pass between dives for the body to rest.
Clinical recommendations for iatrogenic EV:
- Removing free air from a syringe or intravenous system before performing a procedure (injections, blood transfusions, drips).
- Sealing of catheters installed in peripheral veins.
- When performing surgical operations, take the necessary precautions to prevent VE (control, monitoring).
Life-threatening air volume
The size of the right atrium in an adult is on average 20 cm3. This is the amount of gas that can block the heart, and is therefore considered extremely dangerous. In case of heart defects with an unclosed septal window, even a smaller hit can be fatal. In one-year-old babies, the maximum diameter of the right atrium is only 11 mm (in adults up to 2.5 mm).
Ultrasound examination of a child
Physiological and anatomical abnormalities are detected during an ultrasound examination of the child.
How is the treatment carried out?
Treatment of air embolism should be carried out in a clinical setting by qualified doctors. In an emergency, you must urgently call an ambulance.
Before her arrival, it is necessary to carry out actions on which the life of the victim often depends.
First aid:
- Check for signs of VE (how air is sucked into the wound).
- Place the person on their left side with their head down.
- Apply an airtight material to the wound and then bandage it.
- Provide the victim with complete rest.
The patient is transported on a stretcher in a stomach-down position; when carrying, the legs should be higher. This is necessary to prevent air bubbles from entering the brain.
Divers
If the development of an air or gas embolism occurred against the background of a sudden ascent of a diver from great depths, then the most effective method is to place the patient in a pressure chamber.
Recompression therapy aims to immediately supply the hyperbaric oxygen chamber with 100% pure oxygen.
The patient is placed in a pressure chamber in a horizontal position and spends a couple of hours in it while the recompression process takes place.
Increased pressure is used to restore blood circulation, saturate tissues with oxygen and minimize the size of air emboli in the vessels.
Upon completion of recompression, the pressure begins to gradually decrease. This is done so that the excess volume of gases freely leaves the body without forming balloons.
As a result of therapeutic measures
If the accumulation of air occurred as a result of medical manipulations, then the patient is placed in a certain position and actions are taken to eliminate the emboli.
Table describing measures to provide care for iatrogenic (medical) embolism in a hospital setting:
| Actions and signs of VE | Description |
| Trendelenburg position | Assuming a supine position, with the part of the body below the waist raised above the level at which the heart is located. |
| On the left side | This position provides air supply to the upper right ventricle, which prevents blockage of the pulmonary artery by an embolus. |
| Changing the position of the operating table | To displace the “air lock” and localize it in the right atrium (or ventricle), the table is tilted to the left, while the head end is lowered. |
| Spontaneous breathing | It is restored by inhalation of 100% oxygen, and if necessary, mechanical ventilation is performed. |
| Occurrence of VE during general anesthesia | Stopping the supply of dinitrogen oxide, performing mechanical ventilation with FiO221.0. |
| In case of circulatory problems | Stabilization of the pressure decline is carried out using infusion therapy using a vasopressor. |
| When an air bubble migrates to the brain | The patient is placed in a hyperbaric oxygen chamber (HBO). |
| At high risk of VE | Aspiration (suction) of air is carried out from the central artery or chambers of the heart through a catheter. The installation is made 1 cm below the confluence of the inferior vena cava in the right atrium. |
| When a vessel is blocked by air bubbles (blood flow stops) | Cardiopulmonary resuscitation is performed. |
Consequences of untimely treatment and prognosis
Complications after such a pathology may be the following:
- Bleeding in the brain.
- Opening of internal bleeding.
- Brain swelling.
- Death of a person.
The prognosis for an air embolism is directly related to the cause that provoked the disease. It is equally important to consider how quickly and correctly emergency assistance was provided.
When small emboli form, the risk to health and life is minimal, since they will not be able to block the blood flow in the vessels. Usually, after no more than a couple of hours, the gas resolves on its own.
The formation of large emboli can lead to the following serious consequences:
- ischemic stroke may occur;
- swelling of the brain (or other organs) is possible;
- Infarctions of various organs are often observed;
- in severe cases (or if timely assistance is not provided), death.
As an example, consider the following cases:
- with accurate and quick diagnosis, as well as correct treatment measures, the occurrence of VE in scuba divers in most cases (up to 85%) ends in complete recovery;
- penetration of air emboli into vessels during catheterization has a disappointing prognosis - death is recorded in 30% of cases;
- severe lung injuries, as a result of which VE is formed, end tragically in 50-80% of cases.
The consequences of embolism depend on the location of the emboli. The main complication of thromboembolism is pulmonary infarction, paradoxical embolism of the vessels of the large circle, chronic increase in pressure in the vessels of the lungs. Possible consequences of fat embolism include pneumonia and acute pulmonary failure.
The consequences of gas embolism include decompression sickness and severe disturbances in the blood circulation and brain. Consequences and complications of amniotic fluid embolism can include purulent-inflammatory complications in the postpartum period, acute cerebrovascular accidents, acute renal failure, and death of the mother and fetus.