Heart defects are represented by a heterogeneous, heterogeneous group of pathological processes. By their nature, they are always associated with defects of certain structures. Recovery is possible, but with great difficulty, is carried out surgically, and sometimes has no prospects at all.
Cardiomyopathy is a change in the size of a muscular organ, as a result of which the functionally active layer of myocytes is unable to adequately contract and pump blood. This is a simplified definition, but it gets the point across.
The pathological process is represented by intensive growth of the muscle layer, that is, the myocardium. Evenly or not does not play a big role. There are active discussions regarding what is classified as a myopathy and what processes should be classified differently.
The true variety of the disease described is a completely incurable cellular transformation of the heart. The only option for radical therapy is transplantation.
In other cases, a conservative technique is indicated, aimed at slowing the progression of the pathological process.
Forecasts are variable; a lot of factors are taken into account (see below).
Myodystrophies
Strictly speaking, this type is not considered cardiomyopathy. The essence is the development of muscle weakness, a gradual weakening of contractility, and a decrease in the total mass of active tissues in general. The heart also suffers. Objectively, the pathological process manifests itself as the proliferation of cardiac structures.
What are the reasons for the formation?
The disease is purely genetic in origin. Represented by a group of syndromes: Noonan, Friedreich, Duchenne. Inherited from parents. It shows itself actively from the very first months of life.
The clinical picture worsens gradually as the condition progresses:
- Chest pain, muscle discomfort. Accompanies a person from the very beginning.
- Muscular weakness. It manifests itself in the insufficient development of facial structures, the patient cannot express emotions normally, he has a motionless face, and his speech is slurred for the same reasons. Children with genetic syndromes get back on their feet later. Movements are uncertain, frequent falls are possible.
- Decrease in intelligence. It shows up from the very beginning.
- Dyspnea. At rest due to impaired gas exchange.
- Dangerous arrhythmias. Atrial fibrillation or extrasystole, when there are too many abnormal contractions during the day.
At approximately 10-12 years of age, patients completely lose the ability to walk. The size of the myocardium reaches significant values, changes are diagnosed by echocardiography.
The contractility of the muscle layer decreases, hence hypoxia and tissue ischemia. Possible heart attack. Death occurs as a result of heart failure at a maximum age of 25-30 years. There are exceptions to the rule, but they are few in number and have no clinical significance.
Treatment is not possible because these are genetic pathologies. They are embedded in a person at a fundamental level.
There is a chance of slowing progression with steroid medications. Additionally, physical education is prescribed according to the approved plan. The effect is partial.
Dangers of Cardiomyopathy
There are 6 main, life-threatening complications:
- heart failure
- myocardial infarction
- thromboembolic complications
- arrhythmias
- pulmonary edema
- sudden cardiac death
Heart failure
As we see, all types of this pathology lead to the development of heart failure. Most often, it has a chronic stagnant nature, associated with a decrease in the volume of blood released into the vessels, as well as oxygen starvation of the internal organs.
In some cases, acute heart failure may develop:
- systolic - when the heart cannot contract normally and push out a sufficient volume of blood. This is typical for the dilated form of pathology;
- diastolic: the ventricle does not fill with enough blood. This is typical for a restrictive type of cardiomyopathy.
Myocardial infarction
This is the name of the condition when a larger or smaller section of the myocardium dies due to insufficient blood supply.
This complication in its “pure form” is characteristic of hypertrophic cardiomyopathy, because such a thickened myocardium is difficult to provide with a sufficient amount of oxygen. But a similar pathology can develop in any other form of the disease if it is combined with an abnormal structure of the coronary arteries supplying the heart, their atherosclerosis or the development of hypertension.
A heart attack should be suspected if:
- there was a sharp and severe pain behind the sternum;
- it radiates to the left hand (the little finger of this hand), the left shoulder, the shoulder blade or the left half of the jaw;
- pain does not respond to nitroglycerin;
- there may be one-time vomiting that does not alleviate the condition;
- the person turns pale;
- covered in cold sweat;
- breathing quickens.
In this case, you need to chew 1-2 Aspekarda tablets (Aspirin, Cardio-Magnyl), lay him down, open the window and call an ambulance.
Thromboembolism
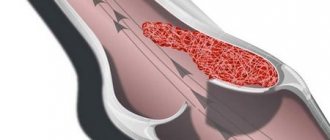
Blood stagnation, characteristic of a heart with damaged myocardium, causes activation of the blood coagulation system. This is how blood clots appear. Arrhythmias, that is, uneven muscle contractions, in turn, increase the likelihood of such a blood clot “traveling” from the heart cavity (in this case, the blood clot is called a thromboembolus) with its subsequent fixation in a vessel “suitable” in diameter. The organ or part of it fed by this vessel dies.
The most dangerous thromboembolisms are:
- ischemic stroke - due to blockage of one of the arteries of the brain by a blood clot;
- thromboembolism of one or more branches of the pulmonary artery, leading to deterioration of blood supply to various parts of the lung;
- mesenteric thrombosis - when a thromboembolus clogs a more or less large arterial branch feeding the intestine, which leads to the death of its various areas;
- thrombosis of the arteries of the extremities, resulting in the development of gangrene.
Arrhythmias
Violation of the normal sequential contraction of myocardial cells leads to oxygen starvation of tissues. If the cells of the ventricle begin to contract “randomly,” and this condition is not immediately corrected, the person may die.
Pulmonary edema
When congestion develops in the left half of the heart, excess blood volume remains in the vessels leading to the lungs. Over time, these vessels expand and begin to pass the liquid part of the blood through their wall - into the lung tissue.
The condition requires emergency medical attention and is manifested by shortness of breath, pink foam from the mouth, blue lips and fingertips, a feeling of shortness of breath and panic.
Autoimmune form
It develops as a result of a long-term or acute, aggressive course of systemic pathologies in which the reaction of the body’s defenses is involved. Lupus erythematosus, psoriasis, rheumatoid arthritis, leukemia as the main diagnoses. Cardiomyopathy is a complication.
The exact reasons for the occurrence of such consequences are not known. It is assumed that there is a connection between the underlying disease and the anatomical defect.
Symptoms of the CMP itself are represented by cardiac manifestations, less often by nervous moments:
- Severe arrhythmia. By type of increase in heart rate at an early stage. The level reaches 130-150 beats, this situation lasts for a relatively short time.
As it progresses, things get worse. The process enters a constant phase. Over time, the person ceases to notice the deviation and lives relatively normally.
- Ascites. Accumulation of fluid inside the abdominal cavity. It appears as a late symptom. Talks about liver dysfunction.
- Edema of the lower extremities. For reasons of the heart. On the other hand, it is possible that the kidneys may be involved in destructive changes.
- Dyspnea. In a state of physical activity in the early stages. As it progresses, the threshold of activity required for symptom development drops until it reaches a minimum. The person is unable to even walk or get out of bed. Profound disability ensues.
- Blueness of the skin. The patient becomes like a wax figure.
- Pale or cyanotic nasolabial triangle.
- Episodic short-term chest pain. There may be a feeling of heaviness without visible
- reasons. Weakness, fatigue.
- Dizziness and headache.
- Fainting. Neurogenic manifestations occur relatively late. A threatening sign. There is a possibility of a stroke.
Treatment involves eliminating the underlying condition. This is very problematic, since autoimmune processes are not completely eradicated. There are good chances only in the early stages of transferring the disease into stable remission.
This is a long process, not always one hundred percent effective. Immunosuppressants and glucocorticoids are used. A change in lifestyle is indicated.
Symptomatic measures include the use of cardioprotectors, diuretics in minimal dosages, and blood pressure lowering agents. Every step is controlled by a group of specialists.
Causes
So far, scientists suggest that broken heart syndrome develops under the influence of the following factors:
- severe stress and intense psycho-emotional experiences: news of a serious illness, death of a relative, accidents, etc.;
- physical activity exceeding the body's capabilities: sudden serious illness, asthmatic attack, etc.
The mechanisms of development of such cardiomyopathy are still unclear. There are several theories of pathogenesis: transient vagospasm, microvascular dysfunction, twisted left anterior descending artery. However, none of them have yet been fully proven. Observations of large groups of people with Takotsubo cardiomyopathy showed that in many of them the disease developed precisely against the background of intense stress (emotional or physical). However, in approximately a third of patients such factors were absent.
Observations by European specialists have shown that takotsubo cardiomyopathy develops somewhat more often in winter. This fact can be explained by two probable reasons:
- in the cold season, spasm of small branches of the coronary vessels occurs more often;
- During the autumn and winter months, people are more likely to suffer from viral diseases.
It is believed that bulging of the left ventricular apex occurs due to increased levels of catecholamines in the blood. The mechanism of development of this disease has not yet been fully elucidated. Scientists believe that the most likely role is played by the release of adrenaline that appears at the moment of stress, which provokes vasospasm and sharply worsens the quality of microcirculation in the vessels of the heart. As a result, the patient experiences transient dysfunction of the left ventricle, manifested by changes in the ECG and blood tests characteristic of myocardial infarction.
Expert observations show that in addition to psycho-emotional and physical stress, the following predisposing factors can contribute to the development of broken heart syndrome:
- a constant source of traumatic situations in the family or at work;
- intense pain syndrome;
- addiction to alcohol or nicotine addiction;
- hyperlipidemia;
- a sharp decrease in blood pressure;
- performing procedures or surgery (eg, cardiac stress test).
Toxic form
Represented by a number of pathological processes. The origin is always the same in essence - the effect on the body of toxic substances.
These are drugs, for example, cardiac glycosides, beta blockers, antipsychotics in large dosages. Also salts of heavy metals, mercury vapor, ethyl alcohol (alcohol). In relatively rare cases, smokers suffer.
Patients working in hazardous industrial enterprises are at increased risk. The probability of such an unfavorable scenario is 25%.
The reasons lie in the disruption of myocardial nutrition at the cellular level. The heart does not receive enough oxygen as a result of two factors: narrowing of the coronary arteries, as well as metabolic abnormalities, a decrease in the rate of metabolic processes.
The symptoms are approximately the same. Chest pain, rhythm disturbances such as tachycardia and other subjective issues. However, the pathological process is many times more aggressive, and the likelihood of death is also higher.
Cardiomyopathy is aggravated by the influence of the main etiological factor. An alcoholic will not stop drinking because of a diagnosis, a smoker will find it difficult to give up cigarettes, and so on. However, lifestyle changes along with taking medications are the main condition for effective treatment.
Factors contributing to the development of broken heart syndrome
Based on clinical observations, the main triggers (“triggers”) for the occurrence of Takotsubo cardiomyopathy have been identified:
- strong emotional experiences - loss of loved ones, natural disaster, armed conflicts, news of an incurable illness, financial collapse, illegal actions;
- hypothermia;
- intense physical stress;
- brain damage - concussion, meningitis, abscess (ulcer), encephalitis, heart attack (ischemic stroke), hemorrhage, vascular thrombosis, epilepsy, tumors;
- mental illnesses – panic disorders, psychosis, suicide attempts, withdrawal symptoms when withdrawing from drugs or alcohol;
- autoimmune pathology;
- exacerbation of bronchial asthma, especially against the backdrop of massive use of adrenergic stimulants to relieve an attack;
- acute emergency conditions for chest injuries - pneumothorax, pneumopericardium (air in the chest cavity or pericardial sac);
- consequences of operations on the brain, heart, and extensive surgical interventions;
- endocrine diseases - a sharp decrease or increase in sugar levels in diabetes, a crisis release of thyroid or adrenal hormones.
In cardiological practice, the occurrence of broken heart syndrome was preceded by pericarditis, Dressler's syndrome after a heart attack, vasospastic angina, rhythm disturbances (QT prolongation, atrioventricular block), myocardial hypertrophy, implantation of a pacemaker, cauterization with radio waves (ablation), resuscitation measures, defibrillation, administration of Dobutamine during stress. tests
Interestingly, when examining patients, traditional risk factors for heart disease (smoking, high cholesterol, hypertension) were not found. Although most cases are found in elderly women, there are also descriptions of this disease in pregnant women, immediately after childbirth, and in childhood and adolescence.
There is a hypothesis about hereditary predisposition and the anatomical variant of the structure of the left coronary artery (elongation) as the probable causes of cardiomyopathy.
Metabolic form
Cardiomyopathy developing as a result of metabolic disorders. In particular, weakening of the nutrition of cardiac structures.
The main factors in the development of the problem are diseases of the adrenal glands, thyroid gland, and pituitary system.
Excess hormones are considered the main development factors. T3, T4, TSH, cortisol, adrenaline, dopamine and other neurotransmitters in excessive quantities lead to an acceleration of the heart.
Hence the increase in blood pressure and the increase in the volume of pumped blood. This means expansion of the chambers of the organ, thickening of the walls.
Symptoms include cardiac and neurological components. In addition, respiratory function is impaired. Progresses slowly over years. Until a certain point, there are no manifestations at all. Metabolic cardiomyopathy is an incidental finding.
Treatment is carried out as planned, immediately after identifying the pathological process. The bottom line is to eliminate the underlying endocrine diagnosis.
Replacement therapy and surgical intervention are carried out. Often diseases are caused by tumor changes. Neoplasia is excised, malignant tumors are irradiated.
Symptomatic measures involve relief of pain, arrhythmia, hepatic and renal manifestations in combination. The main goal is to slow down the progression and prevent the development of complications.
Infectious-toxic cardiopathy: what is it and how to deal with it Poisoning.ru
Toxic cardiomyopathy is a myocardial pathology in which anatomical and functional changes in the heart muscle occur . In this case, the coronary vessels (arteries and veins that supply the heart) are not affected. The valves of the ventricles and atria remain without structural changes, and blood pressure does not increase.
The disease is inflammatory in nature. It develops in patients regardless of their gender and age. An ECG examination reveals changes in heart rhythms, which indicate the rapid development of circulatory failure. As a result of the decompensatory mechanism, the heart increases in size.
What kind of disease is this?
Toxic cardiomyopathy is a disease that is manifested by an inflammatory process of the muscle tissue of the heart, without the influence of the pathology of the coronary blood supply or the functioning of the valve apparatus.
Judging by the name, it is easy to guess that the main pathogenetic factor in the development of the disease is exposure to toxic substances.
But in fact, the classification of the causes of the disease is more extensive.
Primary causes include:
- congenital, when the normal formation of heart tissue in the womb is disrupted;
- acquired factors when another heart disease progresses to cause toxic cardiomyopathy.
Among the secondary causes, it is worth highlighting the following:
- Infectious damage to the heart muscle.
- Exposure to toxic substances – alcohol abuse, smoking, drug use. You can also be poisoned by heavy metals such as mercury, zinc, cadmium, lead, nickel and many others.
- Lack of vitamins, especially group B.
- Diseases of the endocrine glands (pituitary gland, adrenal glands, thyroid gland).
- Drug poisoning.
It should be borne in mind that the main pathological causes are not only alcohol and drugs, but also medicines, poisons, very poor ecology, or, what happens most often, a combination of factors.
That is why toxic cardiomyopathy in ICD 10 is divided into several classes, according to its genesis.
Refinement and weakening of the walls of blood vessels is one of the manifestations of cardiomyopathy
Causes of toxic damage to the heart muscle
Toxic cardiomyopathy develops due to exposure to toxic substances . Chemical elements that can lead to disease:
- mercury;
- lead;
- arsenic;
- cadmium;
- zinc;
- nickel.
In chronic alcoholism, prolonged exposure to ethanol on the heart muscle also contributes to the development of pathology.
There are a number of infectious diseases that damage the myocardium. As a rule, signs of cardiomyopathy appear several months or years after the illness :
- tuberculosis;
- syphilis;
- diphtheria;
- typhoid and typhus;
- scarlet fever;
- parasitic infestations.
The disease also develops in people with drug addiction, with long-term treatment with pharmacological drugs. There is evidence that cardiomyopathy may occur due to chronic deficiency of B vitamins.
In some cases, the cause of the disease may be an increase in the body's production of catecholamines - mediators, biologically active substances (serotonin, adrenaline, norepinephrine, dopamine).
The causes of the disease include inflammatory processes in the body of a pregnant woman. As a result of the influence of an infectious agent at birth, the child is diagnosed with congenital cardiomyopathy.
Inflammatory type
Relatively rare. It occurs as a consequence of myocarditis, damage to the muscular layer of the heart.
As the process continues, the probability increases. Cardiomyopathy is asymmetrical in nature and develops at the level of individual chambers.
The deviation progresses at different rates, depending on the degree of damage.
Treatment is urgent, in a hospital setting. At an early stage of the process, when there is an acute infectious period, antibiotics are indicated, plus cardioprotectors to protect cells from destruction.
Autoimmune varieties are eliminated by glucocorticoids in a system with immunosuppressants. In case of total destruction of the atria, prosthetics are indicated.
Clinic
Clinical symptoms are caused by the disease that provoked the appearance of secondary cardiomyopathy.
Symptoms characteristic of the patient’s pathology include:
- pain in the apex of the heart - downward from the middle of the left clavicle, at the intersection with the fifth intercostal space (in 92% of cases);
- pain behind the sternum (15%);
- expansion of the borders of the heart during percussion examination (the damaged myocardium is stretched);
- muffled first and second sounds over all points of auscultation (the heart muscle is softened);
- arrhythmias (violation of intracardiac control over the activity of the conduction system).
Hypertensive form
Presented in two varieties.
- Peripartum cardiomyopathy is a result of pregnancy. The exact origin of the deviation is unknown; it is assumed that we are talking about changes in hormonal levels and changes in the body.
There is a correlation between the number of children and the likelihood of deviation. It is rare; a predisposing factor is a history of cardiovascular disease.
- The second type is associated with insufficient nutrition of the heart. Ischemic cardiomyopathy is a decrease in the quality of tissue trophism, as a result of which a compensatory reaction begins with the growth of the muscle layer. It turns out to be the result of a stable increase in blood pressure.
Symptoms of cardiomyopathy are vague. They overlap with signs of hypertension and are therefore not noticeable without a special examination. The prognosis is unfavorable for advanced hypertension, since a prerequisite for cure is correction of tonometer readings.
Therapy is carried out using beta blockers, ACE inhibitors, centrally acting drugs, calcium antagonists. The doctor selects specific names; incorrect combinations are critically dangerous for the heart and kidneys.
Symptoms of the disease
Answering the question - toxic cardiomyopathy, what is it - you need to know the main symptoms of the disease. Among them it is worth highlighting:
- Substernal pain, which can be localized both in the projection of the heart and throughout the chest.
- Dyspnea. A very common and important sign of cardiac pathology is inspiratory dyspnea. That is, when it is difficult for a person to inhale, but it is easy to exhale.
- Arrhythmia or other heart rhythm disturbances.
- Dizziness that is not associated with other causes.
- Frequent increase in blood pressure, as a result of improper functioning of the heart and poor condition of blood vessels.
- Swelling. Most often, it is the extremities that swell.
- An increase in body temperature against the background of other symptoms may indicate an infectious accompaniment of toxic cardiomyopathy.
Be careful: if the pain behind the sternum continues for several days in a row and is aching in nature, this is a direct reason to consult a doctor.
Valve shape
It occurs as a result of an uneven load on the cardiac structures: mitral, aortic, tricuspid stenosis and other defects. Causes may be congenital or acquired.
Symptoms are caused by regurgitation. Improper hemodynamics in the heart itself.
The basis is made up of cardiac manifestations, such as shortness of breath, arrhythmia, pain, and general discomfort. Recovery is strictly surgical. The operation involves valve replacement.
All described diseases have a single ICD code - I42, followed by a postfix through a dot, it indicates the etiology of the process.
Regardless of the type and origin, there is always a group of objective features that are visible on echocardiography, ECG and MRI:
- Enlargement of the heart.
- Increased pressure in the aorta and pulmonary artery.
- Decrease in the ability of the myocardium to contract.
- Dilatation, that is, expansion of the chambers of a muscular organ.
- Hypertrophy of the walls.
In approximately 70% of cases there are no symptoms at all, but anatomical changes are already present. Therefore, it is necessary to contact a cardiologist in a timely manner. At least for the sake of undergoing a preventive assessment of the patient’s condition.
Other classifications are used much less frequently. It is possible to distinguish hypertrophic, dilated and restrictive forms.
The first is characterized by thickening of the ventricular myocardium, the septum and the release of blood into the aorta are also affected. The second is the expansion of the chambers, the third is the growth of the walls themselves along the entire length of the heart.
Toxic cardiomyopathy: causes, symptoms, treatment methods
The toxic form of cardiomyopathy is characterized by the presence of an inflammatory process in the muscle tissue of the myocardium, while the patient does not have any pathologies of the coronary valves and arteries. This disease can be life-threatening, as it causes an increase in the size of the heart and circulatory failure.
Causes
Toxic cardiomyopathy can be found in any person, regardless of gender and age. The causes that cause this disease are divided into primary and secondary by doctors.
Among the primary ones, it is worth noting the following types of cardiomyopathy:
- congenital;
- acquired;
- mixed.
The first type is often a consequence of an unhealthy lifestyle or frequent stressful situations during a woman’s pregnancy. In such cases, the child is born with disturbances in the formation of myocardial muscle tissue.
Also, the occurrence of congenital cardiomyopathy can be the result of diseases suffered by a pregnant woman, which are characterized by inflammatory processes in the body.
This leads to the child’s heart becoming vulnerable to all kinds of infections and toxins.
Secondary causes of the development of toxic cardiomyopathy are:
- disturbances in the functioning of the thyroid gland, adrenal glands, pituitary gland;
- irregular heartbeat, palpitations;
- diseases caused by infections;
- insufficient intake of B vitamins;
- scleroderma;
- systemic lupus erythematosus;
- polyarteritis nodosa;
- heavy metal poisoning;
- intoxication with medications used in the treatment of cancer;
- toxic effects of drugs and alcoholic beverages.
Clinical picture
The first symptom to look out for is shortness of breath, which occurs after physical activity and moderate exercise.
With toxic cardiomyopathy, the pumping functions of the heart deteriorate, resulting in increased fatigue and general weakness of the body.
But if the illness was caused by an infection, the first symptoms are very similar to those of the flu (general malaise, fever).
In addition to the above symptoms, the toxic form of cardiomyopathy is characterized by:
- dizziness;
- feeling of lack of air;
- pain in the chest and heart;
- general weakness;
- tremor;
- swelling;
- disturbances in heart rhythm;
- increased blood pressure.
These symptoms may occur due to age-related or physiological changes in the body. In such cases, there is no need to worry. You should seek the help of doctors when the pain is aching in nature, combined with constant shortness of breath, and the patient feels it for a long time.
You should be very attentive to such manifestations, because these symptoms can occur periodically, and not be present constantly, and people mistake them for the consequences of lack of sleep, chronic fatigue, etc., which is why they do not turn to specialists in a timely manner.
But the symptoms do not cause discomfort to the patient only up to a certain point. If treatment is left untreated and toxic cardiomyopathy develops, the following will be added to the main symptoms:
- a painful cough that occurs even at rest;
- the skin becomes pale and acquires a bluish tint;
- the pain in the heart intensifies, sometimes making it difficult for a person to lie down.
With proper and timely treatment, the prognosis is usually favorable, and a person can live a long, fulfilling life. But if the patient leaves the disease in question unattended, it can lead to the following complications:
- arrhythmias;
- thromboembolism, and later – to stroke;
- accumulation of fluid in the lungs, legs, and abdominal area due to severe swelling;
- heart failure;
- malfunctions of myocardial valves;
- death due to cardiac arrest.
Diagnostics
It is almost impossible to determine the disease at home on your own, so the first thing you need to do is visit a doctor. He will analyze the clinical picture, find out whether the patient has a hereditary tendency to heart disease, etc. The doctor will also listen to the heart rhythm and myocardial sounds, which can help identify any heart pathologies.
Next, the patient will have to undergo a comprehensive examination so that specialists can establish an accurate diagnosis. It includes the following activities:
- Blood chemistry. It will help rule out the presence of other myocardial diseases.
- Research of kidneys and liver.
- Electrocardiography.
- Chest X-ray, the results of which indicate an increase in the left myocardium and overload of the entire system.
- Sometimes the patient is referred for magnetic resonance imaging and ultrasound examination.
- Also, a cardiologist can give a referral to geneticists to confirm or rule out genetic causes of cardiomyopathy.
At any stage of the examination, the patient may be additionally referred for urine and blood tests.
Treatment of this disease is a long and complex process. Depending on the stage of the disease, the cardiologist selects treatment regimens and methods. It can be medical or surgical.
Drug therapy
Conservative treatment includes taking medications:
- Heart rhythm disturbances can lead to blood clots. In such cases, anticoagulants are prescribed.
- When the symptoms of toxic cardiomyopathy are quite pronounced, the patient should take beta-blockers, for example, Bisoprolol or Atenolol.
- If the previous group of medications does not give the desired result, the cardiologist may prescribe Verapamil, which reduces the severity of disturbances in the functioning of the heart muscle.
Radical treatment methods are resorted to when the use of medications is powerless. For toxic cardiomyopathy, the following types of operations are performed:
- Defibrillator installation. Such surgical intervention is indicated in the case where genetic tests have confirmed a person’s hereditary tendency to heart disease, and he is at risk of cardiac arrest. Using a defibrillator, the rhythm and heart rate are adjusted.
- Introduction of a pacemaker. This method is used for serious irregularities in the heart rhythm. This device helps normalize it.
- Heart transplantation. It is carried out only in the most severe cases, when neither medication nor surgery gives a positive result.
General recommendations
Of course, it is important to take the prescribed medications, but recommendations regarding lifestyle are no less important:
- Get rid of bad habits completely or at least minimize them.
- Follow a healthy diet and, if necessary, lose extra pounds.
- Strong physical activity is strictly prohibited.
- Avoid stressful situations, depression, normalize the psycho-emotional background.
- Reduce the presence of toxins in the patient’s life, which became the factor that caused the form of cardiomyopathy in question.
Folk remedies
When diagnosing toxic cardiomyopathy, as with any other form of this disease, you can resort to traditional medicine recipes. They are based on natural ingredients, so they will not harm your body. But still, before using them, you should consult with your doctor to rule out the presence of contraindications to the use of certain drugs.
The most popular are the following recipes :
- Flax seeds. To prepare, you will need 1 spoon of seeds and 1 liter of boiling water. The product should be simmered for three quarters of an hour over low heat. Then strain and drink 100 ml at a time throughout the day.
- Kefir. This product is easily absorbed by the body, so it does not put a lot of stress on the heart (unlike hard-to-digest foods, which are unacceptable for any form of cardiomyopathy). The greatest benefits will come from kefir prepared at home yourself.
To prepare the product you will need:
- 0.5 cups of kefir;
- 100 g honey;
- 1 tbsp. l. lemon juice;
- 1 glass of carrot juice.
All ingredients must be stirred until smooth, divided into three equal portions and consumed before meals. The product should be stored in the refrigerator.
- Jaundice. 40 g of the plant should be poured into 1 liter of boiling water and left for 2 hours. Then strain and take 100 ml 2 times a day. This drug has anti-inflammatory, diuretic, expectorant, hypotensive, and antiseptic effects.
- Motherwort five-lobed. 2 tbsp. l. plants are poured with 1.5 glasses of 70 percent alcohol and infused for a week at room temperature. Use strained tincture 25 drops 3 times a day.
You can also pour 30 g of motherwort with two cups of boiling water, leave until it cools and drink 1/3 cup 3 times a day.
- Kalina. To normalize heart function and fight cardiomyopathy, you need to eat about 100 g of berries daily. It is not recommended to overuse viburnum for this disease, as this can lead to the formation of blood clots.
- Hare cabbage. For 1 glass of boiling water you will need 20 g of herb. The product must be left for a couple of hours, strained and taken 4 times a day, several tablespoons.
- Oats. 50 g of oats are poured into 2 glasses of water and brought to a boil. Leave for 4 hours, then warm up a little and add 100 g of kefir and red juice. Then knead until smooth, leave for 2 hours and add 0.5 cups of honey. Take this remedy before meals, 100 mg 3 times a day.
- Chicory. 1 cup of boiling water pour 1 tsp. powder from ground chicory roots. The product is kept on the fire for a quarter of an hour, then filtered. Drink a healing drink 4 times a day, 2 tbsp. l.
- Calendula. A few tablespoons should be infused in 100 ml of boiling water for an hour. Then strain and take 100 ml at intervals of 6 hours.
- Herbal collection. For preparation you will need chicory root, adonis, mint, rose hips, calendula, and sweet clover in equal proportions. 2 tbsp. l. collection, pour 1 liter of water and boil for a quarter of an hour. Then leave in a thermos until the morning. Drink 2/3 cup before meals. The course of treatment lasts 2 years, but every 3-4 months you should take a break.
Prevention measures
To prevent the development of the disease, you must adhere to these simple rules:
- a healthy lifestyle is the key to good health and prevention of many diseases;
- doing physical exercise helps improve blood circulation and heart muscle function;
- proper nutrition will prevent the deposition of harmful substances, the appearance of excess weight and minimize the risk of heart and vascular diseases;
- It is necessary to undergo regular medical examinations, promptly treat diseases and not take any medications without consulting a specialist.
Toxic cardiomyopathy is a serious disease, but it is not a death sentence. Modern treatment methods will help normalize the functioning of the heart and allow the patient to live a full life. But to do this, you need to not let the disease progress and consult a doctor at the first symptoms of toxic cardiomyopathy.
Source: //serdce.biz/zabolevaniya/kardity/miokardit/toksicheskaya-kardiomiopatiya.html
Diagnostics
It is carried out under the supervision of a cardiologist, and third-party specialists are involved as necessary. It is difficult to define the disease. List of events:
- Oral survey. It is impossible to identify the process based on the nature of the complaints.
- Anamnesis collection. Age is taken into account. Thus, the dilated form is more common in young men under 35 years old, hypertrophic in people around 40, restrictive after 45, and is also observed in women.
Also, lifestyle, diet, past illnesses, addictions, family history and other factors.
- Measurement of blood pressure and heart rate. Both indicators are deviated from the norm. The first is in the direction of increase at first, then in a falling manner, which indicates insufficiency. Heart rate increases, tachycardia occurs.
- Auscultation. Listening to heart sounds. Sinus murmur occurs against the background of valve defects. Muted tones.
- Daily monitoring. In controversial cases. Records heart rate and blood pressure for 24 hours. Gives a dynamic picture.
- Electrocardiography. Specific manifestations are represented by arrhythmias such as tachycardia, fibrillation, extrasystole
- Echocardiography. Profile technique. Aimed at assessing the anatomical state of a muscular organ, measuring pressure in the aorta and pulmonary artery.
- MRI if necessary to clarify the extent of disorders.
- General blood test, biochemical, hormones. Including liver tests.
- Urine examination. Necessary for assessing the functioning of the excretory system.
Identifying the cause of cardiomyopathy is difficult. In 15-20% of cases, an idiopathic, that is, clinically unexplained form is diagnosed.
This complicates therapy; it is necessary to limit oneself to symptomatic measures. The examination is repeated every 6-12 months. In threatening forms, more often, since there is a risk of death.
Features of the flow
The problem with timely diagnosis of this form of cardiomyopathy is that the results of blood tests and ECG are almost identical to the manifestations of myocardial infarction. Broken heart syndrome can be distinguished from this common disease only by the results of coronary angiography, which shows that the arteries of the heart remain healthy and there is no hemodynamically significant narrowing of these vessels.
Published in the European Heart Journal, the most significant studies of this form of cardiomyopathy showed that approximately 1.7-2.2% of myocardial infarctions are actually Takotsubo cardiomyopathy. In more than half of patients with this disease, the attack is preceded by intense stress and in 74% of patients the level of catecholamines increases. It is noted that compared with normal values in Takotsubo cardiomyopathy, the level of these hormones can increase tens of times.
Treatment
Requires elimination of the etiological factor: endocrine disease, defect or other. Manifestations are stopped in the second place. The list of methods is huge, since there are a lot of options for the formation of a pathological process.
Surgical intervention is prescribed when anatomical defects are detected. The essence is the expansion of coronary vessels, prosthetic valves, sections of arteries. Strictly according to indications.
The drugs are used to treat the underlying condition.
Symptomatic remedies:
- Nitroglycerin for pain relief.
- Cardioprotectors. Protect myocytes from oxidation and destruction. They also improve metabolism at the local level. Mildronate.
- Antiarrhythmic. Small doses when detecting abnormalities in the heart. Amiodarone as the main one.
- Glycosides. Improves myocardial contractility. Digoxin. Prescribed with great caution. In the later stages of cardiomyopathies, they are not used, the risks are too great.
- Beta blockers. To relieve tachycardia, lower blood pressure and normalize vascular tone. Carvedilol or Anaprilin.
- Antiplatelet agents. Normalize blood fluidity. Prevents the formation of blood clots. Aspiran-Cardio, Heparin.
- Means for lowering blood pressure. Calcium antagonists, ACE inhibitors and centrally acting medications.
As needed, diuretics. They remove excess fluid and reduce the load on the heart. Quitting smoking and drinking alcohol is mandatory.
The diet is moderate, low in fat. Treatment table No. 10 is shown.
Physical activity in the form of walking, swimming or exercise therapy, no gyms or overload. Cardiac arrest and sudden death are possible.
Treatment of cardiomyopathy is medicinal, using a group of drugs. Surgery is a last resort. Advanced cases require transplantation. This is the only chance.
What is toxic cardiomyopathy?
Toxic cardiomyopathy is a disease characterized by inflammation of the muscle tissue of the heart in the absence of painful abnormalities of the coronary arteries and valves.
Why does toxic cardiomyopathy occur?
Toxic cardiomyopathy has no age limit and can occur in both men and women. Changes can be observed on the electrocardiogram: impaired blood circulation and an increase in the volume of the heart, subsequently a negative outcome for the entire body and human life.
Cardiomyopathy comes in two types: primary and secondary. Primary - these are congenital, acquired and mixed disorders:
- Congenital toxic cardiomyopathy develops in the fetus as a result of an unhealthy lifestyle or severe stress in a pregnant woman. Inflammatory diseases in the body of a pregnant woman are also the cause of the disease, as the heart becomes susceptible to infections and toxic substances.
- Secondary cardiomyopathies are toxic and infectious diseases. Alcoholic cardiomyopathy is caused by alcohol abuse, it is also provoked by drugs for cancer, lack of vitamin B, thyroid diseases - diffuse toxic goiter, hyperthyroidism; pathologies of the adrenal glands, polyarthritis; IBS.
Alcoholic cardiomyopathy
Ischemic cardiomyopathy is provoked by ischemic heart disease, that is, a condition caused by impaired blood supply and oxygen supply to the myocardium.
Symptoms of the disease
Symptoms of toxic cardiomyopathy:
- pain in the heart and chest;
- dyspnea;
- change in heart rate;
- dizziness;
- bad feeling;
- increased blood pressure;
- swelling.
The patient experiences shortness of breath with moderate exertion. The pumping function of the heart worsens. If the cause is an infection, then people may not pay attention to the development of the disease, since the symptoms of the disease are not pronounced and are not regular. Symptoms are similar to the flu: fever, malaise.
If you experience aching chest pain with shortness of breath, consult a doctor immediately. Symptoms of IHD:
- pain behind the sternum during exercise;
- back and arm pain;
- heartbeat;
- dyspnea;
- dizziness;
- confusion;
- increased sweating.
How is cardiopathy treated?
Diagnosis begins with a trip to a specialist. The doctor will ask questions about what illnesses the relatives had, whether there were heart-related diseases, and whether there were people in the family who died at a young age. The doctor will do an examination: listen to heart sounds, frequency and amount of noise to rule out a particular disease.
Blood is examined. Additionally, they donate blood and urine, and examine the liver and kidneys. A chest x-ray is taken - this is necessary to see an enlargement of the left side of the heart, which will indicate one or another pathology.
A chest x-ray will help determine the enlargement of the left side of the heart and prove the presence of a pathology such as cardiopathy.
Taking an ECG
An ECG is taken. Hypertrophic cardiomyopathy is an enlargement of the wall of the heart ventricle. MRI and ultrasound are less commonly prescribed. People cannot determine the disease on their own, so in order to accurately establish the diagnosis, you need to go to a cardiologist. He makes a diagnosis and refers to a specialist to exclude the elimination of genetic diseases.
Treatment of ICMP is to eliminate the cause. IHD is the cause of ICMP. IHD is treated non-pharmacologically. You need to maintain a healthy lifestyle, adjust your diet, limit exercise and physical activity in order to reduce the heart’s consumption of oxygen.
The diet limits fluid and salt intake. Products excluded:
- butter;
- fatty meats;
- spicy, peppered, fried, fast foods;
- cakes, coffee, chocolate.
When dieting, you need to maintain a balance of energy intake and energy expenditure. Every day you should consume 3000 kcal with an expenditure of 2000 to 2500 kcal.
Patients are prescribed medication:
- antiplatelet agents;
- beta blockers;
- hypocholesterolemic drugs.
If there are no contraindications, use:
- nitrates;
- diuretics;
- antiarrhythmics.
If there is no effect, surgical treatment - CABG - is recommended. Coronary artery bypass grafting is the restoration of an ischemic area that is resistant to drug therapy. The essence is the imposition of an autovenous anastomosis between the aorta and the affected cardiac artery below the area of narrowing.
A bypass channel of the vessel is created, which delivers blood to myocardial ischemia. The operation is performed using artificial circulation or on a functioning heart.
Treatment of coronary artery disease includes percutaneous transluminal corneal angioplasty - expansion of the affected vessel with prosthetic frame - a stand to maintain the lumen for blood movement.
Coronary artery bypass grafting
Treatment of ACM. If a person has alcoholic cardiomyopathy, treatment includes avoiding alcoholic beverages. Stopping alcohol intake stops the destruction of the liver, heart, and pancreas. If the functions of organs are severely impaired, their work must be supported with medications.
At the initial stage, vitamins, microelements, and radioprotectors are needed to improve processes in the heart. As a result, the heart rhythm normalizes. The following drugs are used to improve blood pressure and heart rate:
- Enalapril;
- Pristarium;
- Cordarone;
- Anaprilin and others.
Subsequently, diuretics (Lasix) and cardiac glycosides (Digoxin) are taken. They are used constantly for tachyarrhythmias and to eliminate paroxysms and heart rhythm disturbances. For ischemic heart disease, obesity, and pathology of cholesterol metabolism: Rosuvastatin is prescribed to normalize blood cholesterol. Also prescribed:
- Nitroglycerine;
- Pectrol;
- Aspirin;
- ThromboAss.
If a patient is diagnosed with ischemic cardiomyopathy, the consequences can be severe. Complications of ICMP:
- changes in the left ventricle of the heart in favor of its reduction;
- stagnation in the pulmonary circulation;
- ischemia;
- heart attacks;
- arrhythmia;
- death.
Therefore, ischemic cardiomyopathy requires immediate treatment in a hospital.
With a disease such as alcoholic cardiomyopathy, death can occur from cardiac arrest. Symptoms: poor health, rapid pulse, followed by respiratory and cardiac arrest.
Thromboembolism develops when a blood clot forms and impedes the movement of blood to the heart. If, as a result, a blood clot breaks off, it will cause an ischemic stroke, myocardial infarction, and thrombosis of the arteries of the lower extremities.
In secondary cardiomyopathy, the cause of death is extensive myocardial infarction or stroke.
Source: //zdorovnet.ru/alkogol/chto-predstavlyaet-soboj-toksicheskaya-kardiomiopatiya.html
Forecast
Depends on the underlying diagnosis, rate of progression, risk factors. On average, 5-10% of patients die within 5 years. As the defect develops, the percentage increases.
Age over 50+, smoking, bad habits in general, taking heavy medications, such as cytostatics, antipsychotics, tranquilizers, unfavorable family history, and the presence of concomitant diseases significantly worsens the prognosis.
Treatment, especially if carried out in the early stages, contributes to a good outcome, although no one can give guarantees.
You need to take a closer look and assess the patient’s health status. Each case is individual, but the chances for a long and high-quality life are more than real.
Toxic cardiomyopathy: causes of development, treatment and prevention
Additional education:
"Emergency Cardiology"
1990 – Ryazan Medical Institute named after Academician I.P. Pavlova
Contacts
Diseases of the cardiovascular system are the most widespread. Cardiomyopathies occupy one of the leading positions among them. These pathologies are divided into primary - without an established cause, and secondary, the etiology of which is established.
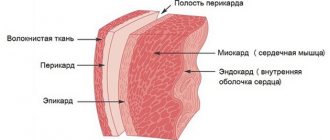
Thyrotoxic cardiomyopathy is a secondary type of disease, which is characterized by damage to the cardiac myocardium (the middle layer of muscle tissue) as a result of exposure to toxic and potent substances on the body.
The pathology is also called toxic; it is directly related to the process of thyrotoxicosis, a syndrome that develops with an excess of certain enzymes and hormones produced by the thyroid gland. There are medicinal and radiation forms of the disease.
Like most specific pathologies, toxic cardiomyopathy predominantly develops gradually.
The appearance of the disease is justified by the fact that taking certain drugs, medications and substances causes a direct cardiotoxic effect, leading to myocardial damage and the development of severe bradycardia (heart rhythm disturbance), slowing of intracardiac conduction and a drop in blood pressure to life-threatening values - collapse. Toxic substances affect the myocardium and cause its structural and functional changes, which affect health in the most negative way.
Some features of the appearance and development of pathology
The disease affects all age groups, regardless of gender or race. With the development of the dosage form, chronic intoxication occurs as a result of exposure to the body of inorganic salts, opiates, alkaloids and lactones. The development of the radiation form is associated with the negative influence of radiation from certain metals and substances.
Most often, the pathology manifests itself in patients suffering from cancer, undergoing radiation therapy and traditional chemotherapy treatment. A distinct toxic cardiomyopathy is observed when the body is poisoned with barium chloride, opiates in combination with ethanol (or ethyl alcohols), as well as such alkaloids and lactones as:
- quinine;
- aconitine;
- veratrine;
- coumarin;
- pachycarpin.
The severity of poisoning depends on the duration and severity of intoxication. One of the late manifestations of pathology is an acute disruption of the normal process of nutrition of heart tissue and dystrophic damage to the heart muscle, which inevitably leads to premature death.
Toxic cardiomyopathy is characterized by an increase in the size and weight of the heart due to hypertrophy of the walls of the right and left ventricles, a decrease in the amount of cardiac fiber and expansion of the cardiac cavities.
In this case, a decrease in the values of the cardiac, atrial and ventricular indices is observed, since functional and, in particular, structural changes interfere with the normal functioning of the organ.
Risk factors for developing toxic cardiomyopathy
Along with the main cause - intoxication of the body, risk factors play an important role in the development of pathology. First of all, these include smoking, which has the most negative effect on the human body. Other risk factors include:
- alcohol abuse;
- drug use;
- the occurrence of infectious diseases in the body;
- lack of vitamin B;
- inflammatory damage to the glands and pituitary gland;
- transfer of endocrine diseases;
- damage by scleroderma;
- heavy metal intoxication;
- inadequate filling of the heart cavities with blood mass due to vascular damage;
- persistent disruption of the normal heart rhythm;
- drug intoxication.
Alcoholism significantly increases the risk of developing toxic cardiomyopathy
In most cases, intoxication with medical drugs occurs during self-medication, since without professional help it is not always possible to determine a safe dose of the drug.
Before using potent substances, you should consult a specialist! Incorrect introduction of certain medications into the body can cause a sharp deterioration in overall health.
Main symptoms of the disease
Most pathologies of the cardiovascular system manifest themselves with similar symptoms.
Identifying characteristic signs and correctly diagnosing the disease is possible only through a specialized examination using hardware and instrumental methods.
Toxic cardiomyopathy is no exception; outwardly it manifests itself with common symptoms characteristic of most heart diseases, namely:
- the appearance of pain in the heart area;
- heart rhythm disturbances;
- feeling of hand weakness;
- the appearance of tremor of the upper and lower extremities;
- increased fatigue;
- shortness of breath and feeling of lack of air;
- dizziness test;
- sudden changes in blood pressure values.
All types and methods of examining the organs of the cardiovascular system are used for diagnosis. Symptoms, depending on the individual characteristics of the organism, may not manifest themselves until a certain stage of development of the disease.
Sometimes patients live to a ripe old age, unaware of the pathological process occurring in their body. The main sign of a disorder in the normal functioning of the heart is pain and discomfort in the chest area.
The painful sensations experienced by the patient due to dysfunction of the heart muscle tissue are not sharp, they are aching and pressing in nature, and can be observed over a long period of time. The appearance of shortness of breath in combination with pain is more than enough reason to contact a specialized medical institution for professional help.
Complications that can cause the development of pathology
Uncontrolled development of the disease can cause a number of complications that are difficult to cure and significantly worsen the patient’s health, in particular the following are possible:
- the appearance of heart failure;
- development of heart valve dysfunction;
- abnormal heart rate;
- development of embolism - blockage of blood vessels;
- sudden cardiac arrest.
A healthy lifestyle helps to avoid the development of the disease. There is no effective system of preventive measures aimed at preventing this particular pathology. Success in treatment can be achieved by strictly following the doctor’s instructions and timely medical assistance.
Drug treatment of toxic cardiomyopathy
The therapeutic effect provided depends on the characteristics of functional and structural changes in the myocardium.
A comprehensive examination of the state of the cardiovascular system allows you to choose the right treatment tactics.
Electrocardiographic diagnostic methods are of greatest importance; they make it possible to study changes in the repolarization phases of sinus rhythm and to study other features of heart contractions.
To reduce bradycardia, solutions of atropine sulfate and potassium chloride are used. In case of conduction disturbances, carbon monoxide, isopropyl alcohol, some opiate-based drugs, meprobomate are used to accelerate intraventricular conduction, and to slow down transmitted impulses it is recommended:
- antiarrhythmic drugs;
- antidepressants;
- chloroquine;
- some b-blockers;
- some phenotheazines.
Treatment is always accompanied by systematic monitoring of heart rate, changes in hemodynamics, and electrolyte levels in the blood. The features and duration of observation of the condition are determined by the specialist individually.
Surgery for the treatment of toxic cardiomyopathy
Surgical intervention is recommended only in cases where possible and acceptable other methods of therapeutic influence have not been successful.
To correct the disturbed heart rhythm, patients are implanted with a pacemaker - a special device that generates the correct frequency of contractile impulses.
A defibrillator is used to coordinate the work of the elements of the heart; it allows one to influence the processes of contraction of individual muscle fibers, performing ventricular fibrillation and maintaining a normal heart rhythm.
If the drug therapy used is not successful, and the use of a pacemaker or defibrillator is contraindicated, a heart transplant is recommended - a complex and lengthy operation, the success and feasibility of which depends on many factors.
Source: //CardioPlanet.ru/zabolevaniya/vospaleniya/toksicheskaya-kardiomiopatiya
Complications
The following consequences are observed:
- Cardiogenic shock. Almost 100% lethal.
- Heart failure. No possibility of resuscitation. Because the organ has been changed.
- Fainting and injuries incompatible with life.
- Stroke. Critical malnutrition of the nerve cells of the brain.
- Heart attack. Necrosis of active muscle tissue with subsequent scarring. Even if life is preserved, coronary disease and CLS occur.
Death is a logical continuation of these complications.
Cardiomyopathy of the heart is the growth of the myocardium, thickening of its walls, expansion of the chambers. Requires urgent treatment immediately after detection of a deviation. The prognosis depends on the start of therapy.