Main vessels of the neck: location and functions
In humans, there are two main types of main arteries of the neck - carotid and vertebral (vertebral).
Both are paired. The right one arises from the brachiocephalic trunk, the left one from the aortic arch. Further, at the level of the upper edge of the thyroid cartilage, they are divided into the external and internal carotid arteries (ECA and ICA, respectively). The common carotid artery supplies blood to the scalp, tongue, pharyngeal muscles, the internal artery supplies the organ of vision, the cerebral hemispheres and the diencephalon (thalamus and hypothalamus).
The vertebral arteries depart from the subclavian and through the openings in the vertebrae of the cervical spine are directed to the brain, where they form the so-called vertebrobasilar basin, which supplies blood to the spinal and medulla oblongata, as well as the cerebellum. The ICA and vertebral arteries, as the main sources of nutrition to the brain, are combined under the name “brachiocephalic” or “extracranial”.
The main problem is atherosclerosis of the internal carotid arteries.
Diagnosis of the disease
Diagnostic measures begin with examining the patient, identifying complaints, measuring blood pressure, pulse and auscultatory examinations. Laboratory tests include mandatory tests for the level of:
- glucose;
- total bilirubin;
- alanine-AT;
- aspartate-AT;
- LDL and VLDL;
- cholesterol;
- albumin;
- creatinine;
- C-reactive protein;
- uric acid.
Instrumental diagnostic methods are selected based on test results. Typically, instrumental diagnostics are carried out using:
- Ultrasound;
- radiography;
- aortography;
- electrocardiography;
- magnetic resonance imaging;
- MR perfusion;
- rheoencelography;
- rheovasography;
- bicycle ergometry;
- cerebral angiography.
The methods are aimed at assessing the condition of blood vessels, determining the speed of blood movement and the degree of damage to the main arteries, etc.
Atherosclerosis of the carotid arteries
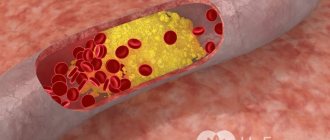
The pathology is a chronic vascular disease in which cholesterol is deposited in the wall of the carotid arteries. Over time, plaques form, narrowing their lumen and disrupting the hemodynamics of the brain. In the international classification of diseases, this pathology is coded I65.2 . The risk of ischemic stroke (death of a part of the brain due to cessation or obstruction of blood flow) when the lumen of the ICA is narrowed by more than 50% increases 3 times.
Atherosclerosis of the ICA is responsible for approximately 20% of ischemic strokes.
Atherosclerosis of the carotid arteries is part of the structure of the so-called cerebrovascular disease, which, along with myocardial infarction and stroke, occupies a leading position among the causes of death. Its prevalence is approximately 6,000 cases per 100,000 population. It is especially common in older people.
How does atherosclerosis develop?
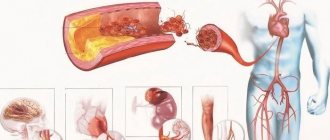
In a healthy body, blood circulates freely through the arteries, delivering oxygen and nutrients to all parts of the body. When the amount of cholesterol exceeds the norm, it begins to deposit on the inside of blood vessels, thereby forming an atherosclerotic plaque.
It is a mixture of fats and calcium. Gradually, the plaque loses its strength and defects form on it. Over time, platelets and blood proteins accumulate at the site of injury, a mixture of which is commonly called a blood clot. It complicates the course of the disease and poses a serious threat to life because:
- further narrows the lumen of the artery;
- a thrombus or part of it can break away from the plaque and, with the flow of blood, clog the vessel at the point of its greatest narrowing.
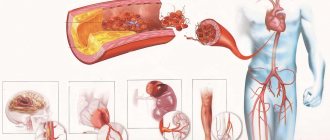
As a result of this pathological process, a stroke can develop, because blockage of blood vessels leads to a cessation of blood supply.
The formation of atherosclerotic plaque in blood vessels and arteries goes through 3 main stages:
- Lipoidosis. Formation of lipid stripes and spots on the vascular wall. They are small in size, no more than 1.5 mm, and outwardly look like yellowish spots. Over time, their size increases due to the fact that the spots merge. Following this, lipid strips are formed, which rise slightly above the surface of the cells.
- Liposclerosis. The appearance of a fibrous plaque. At the sites of lipid deposits, connective tissue with a lipid core in the center is formed.
- Formation of a full-fledged atherosclerotic plaque. As the disease progresses, the lipid core increases by more than 30% of the total plaque volume.
By nature, stable and unstable atherosclerotic plaques are distinguished. This condition depends on the size, configuration and structure of such a lipid formation. Stable plaques are static or characterized by slow growth. They are mainly composed of collagen, while unstable ones are rich in lipids. Cholesterol plaques, forming in various parts of the vessels, cause circulatory disorders of two types: acute and chronic.
Acute circulatory disorders develop as a result of a sudden cessation of blood flow in an artery. This happens when the contents of the plaque breaks into the lumen of the vessel, and then thrombosis occurs. The detached blood clot eventually reaches narrower vessels, through which it can no longer pass and gets stuck there. This condition is fraught with ischemic stroke.
Chronic circulatory disorders are recurrent in nature and manifest themselves in the fact that the vessels affected by sclerotic and degenerative processes narrow significantly, but do not completely overlap. As a result, cerebral circulation is disrupted. It should be noted that the blood vessels of the brain are very vulnerable to blockage. This is due to the peculiarity of their anatomical structure.
Causes and mechanism of disease development
Atherosclerosis of the carotid arteries develops due to many reasons. We list them in order of importance:
- Dyslipidemia. It is a disorder of lipid metabolism, namely the appearance of high levels of total cholesterol, low-density lipoproteins (“bad cholesterol”), as well as low levels of high-density lipoproteins (“good cholesterol”). Hereditary hypercholesterolemia sometimes occurs.
- High blood pressure. Constantly elevated blood pressure increases the risk of complications of any heart and vascular diseases.
- Diabetes. It has long been known that prolonged high concentrations of glucose in the blood accelerate the development of atherosclerosis several times.
- Obesity. Overweight people have much higher levels of cholesterol and triglycerides in their blood than those who are of normal weight. You can determine your body mass index here.
- Sedentary lifestyle – insufficient physical activity naturally leads to obesity.
- Smoking – components of tobacco smoke, including nicotine, contribute to the formation of free radicals (reactive oxygen species) in the body, which trigger lipid peroxidation. This cholesterol is deposited in the walls of blood vessels.
- Poor nutrition. Too much meat and not enough vegetables, fruits and fish lead to metabolic syndrome, which increases the risk of fatal heart conditions.
- Stress leads to increased blood pressure and the release of hormones that increase blood glucose.
- Genetic predisposition.
- Male gender. In men, atherosclerosis develops earlier and faster, because female sex hormones (estrogens) can slow down the process of plaque formation.
The mechanism of atherosclerotic plaque formation itself is quite complex and not fully understood.
It is worth noting that any person has cholesterol deposits on large vessels; even in stillborn children, at autopsy, minimal atherosclerotic changes in the walls of the aorta are found.
At this point in time, scientists distinguish three main stages of atherosclerosis:
- Formation of lipid spots and streaks. The first link is damage to the endothelium (inner lining) of the artery, which creates favorable conditions for the penetration of cholesterol particles. High blood pressure contributes most strongly to this. Macrophages absorb lipoprotein molecules, turning into foam cells.
- The appearance of a fibrous plaque. Further, due to damage to the endothelium and the accumulation of foam cells, growth factors are released, which leads to increased division of smooth muscle cells and the production of connective tissue fibers (collagen and elastin). A stable plaque is formed with a thick and dense fibrous cap and a soft lipid core, narrowing the lumen of the vessel.
- Formation of a complicated plaque. Progression of the process leads to an increase in the lipid core, gradual thinning of the fibrous capsule, rupture and parietal thrombus formation, almost or completely blocking the lumen of the artery.
In the case of the internal carotid artery, the parietal thrombus breaks off and occludes smaller vessels (middle, anterior cerebral arteries), causing an ischemic stroke.
Prevention
Prevention methods are aimed at preventing the influence of risk factors on increasing cholesterol accumulation in the body, which leads to excessive deposits on the lining of blood vessels.
The most susceptible to the accumulation of plaques are the cervical spine.
Methods of preventive action on atherosclerosis:
- Proper nutrition, which contains a minimum of cholesterol-containing foods;
- Get rid of excess weight, which will help restore lipid metabolism;
- The constant fight against physical inactivity is to include sports loads on the body at least several times a week;
- Get rid of alcohol addiction;
- Quit smoking;
- Avoid stressful situations.
Favorite spots for plaques
Most often, atherosclerotic plaques are located in the following places:
- in the area of the bifurcation of the carotid artery, i.e., where the common carotid is divided into external and internal;
- at the mouth of the ICA – the initial segment of its branch from the ECA;
- at the mouth of the vertebral arteries;
- in the ICA siphon (the place of bend at its entry into the skull).
This is explained by the fact that in these places, due to the unevenness of the vessel, a turbulent (vortex) blood flow is created, which increases the likelihood of endothelial damage.
Symptoms
They may not appear for a very long time, and this is a huge danger. Tangible signs can be different and they depend on many factors - the size of the deposit, location, and so on. Most often, a decrease in blood flow in a certain area is characterized by the appearance of fatigue after physical activity or with any acceleration of blood circulation. Many patients note mild pain, but do not pay due attention to it. And of course, a symptom of the decomposition of an unstable cholesterol plaque is a heart attack or stroke.
Most often, the symptoms go in parallel with those signs that are observed in obese patients. Thus, ischemic attacks may also occur, during which the following may be observed:
- Confusion of speech. Disruption of the blood supply to the brain leads to multiple changes, symptoms of which can include confusion of speech. Such oxygen starvation of the brain prevents a person from composing even a simple sentence.
- Numbness. It appears suddenly and is localized only on one side of the body.
- Deterioration of vision in one eye. A very formidable symptom, indicating a pre-stroke state of the body.
- Weakness. Perhaps the most insignificant symptom, according to patients. The fact is that an atherosclerotic plaque blocks the blood flow, which leads to a lack of oxygen. In turn, the body turns on the “energy saving” mode. The patient feels tired constantly, chronically, and even feels a loss of strength without physical work.
In each individual person, symptoms may be more pronounced or weaker. Some patients have only one sign from the list, while others describe the complete clinical picture. At first, ischemic attacks can be very short-lived, up to an hour, and subsequently can last almost a day. Over time, the periods between attacks may become shorter, and now the person becomes a patient of a cardiologist who requires immediate treatment.
Symptoms and complaints of the patient
Clinical symptoms of cervical atherosclerosis occur when the lumen of the artery is narrowed by more than 50%, and the brain begins to experience oxygen starvation. As practice shows, there are patients with a greater degree of stenosis who do not show any complaints and feel completely healthy. Long-term insufficiency of blood supply to the brain is called chronic ischemia or discirculatory encephalopathy . Its symptoms:
- rapid onset of fatigue, decreased physical and intellectual performance;
- memory impairment and mental degradation;
- loss of critical thinking;
- frequent mood swings;
- sleep disturbance – drowsiness during the day, insomnia at night;
- dizziness, headache, tinnitus.
The insidiousness of atherosclerosis is that for a long time it can be completely asymptomatic until the development of acute conditions. These include:
- transient ischemic attack;
- ischemic stroke (ICH).
A transient ischemic attack (TIA) is a sudden deterioration in blood circulation in a certain area of the brain. It is a pre-stroke condition. Symptoms:
- dizziness;
- imbalance, unsteadiness of gait;
- transient blindness in 1 eye;
- speech disorder;
- numbness, feeling of weakness in one half of the face, arm, leg, etc.
With an ischemic stroke, almost the same picture is observed, but more severe, with a risk of death; complete paralysis of one half of the body or an epileptic seizure may also occur. The main difference between TIA and stroke is that its symptoms completely disappear after 24 hours, and in the case of stroke they remain for a long time and also require specialized measures. If a TIA is not diagnosed in time and not provided with qualified treatment, it can turn into a stroke.
Features of treatment
Treatment tactics depend on the stage of the disease. If cholesterol plaques in the vessels of the neck are discovered by chance, when there are no symptoms, the person is advised to reconsider his lifestyle and eating style. This is usually enough to slow down the progression of the disease as much as possible. Larger deposits, in addition to lifestyle correction, require the use of medications. Atherosclerotic plaques that significantly narrow the lumen of the artery require removal.
Conservative therapy
Most of the reasons that provoke the appearance of atherosclerotic formations are associated with lifestyle errors or poor diet. All of them disrupt fat metabolism, increasing bad cholesterol (hypercholesterolemia) and decreasing good cholesterol. Such disease triggers are called risk factors. These include:
- excess weight;
- a diet rich in saturated heat, cholesterol, poor in fiber sources;
- smoking;
- alcoholism;
- inactivity.
Eliminating them helps stop the growth of plaques and prevent the formation of new ones. For a positive effect you need:
- Watch your scales. The presence of extra pounds is accompanied by a violation of fat metabolism. In obese people, the level of bad cholesterol and triglycerides is usually elevated, and mobility is limited. This creates ideal conditions for the formation of deposits on the walls of blood vessels.
- Move more. Doctors recommend that all people devote at least 30 minutes/day to physical activity. These include sports, outdoor games, walks, and cycling. Make sure you do some of these types of physical activity every day.
- Quit smoking. Tobacco smoke increases the concentration of bad cholesterol, lowers the content of good cholesterol, and disrupts the functioning of the heart. The sooner you give up a bad habit, the better the prognosis will be. According to doctors, the risk of developing a plaque in the vessels of the neck in a person who has not smoked for 10 years is the same as in someone who has never smoked.
- Monitor the amount of alcohol you consume. Doctors do not have a unanimous opinion about the benefits of small doses of alcohol. On the one hand, ethanol can partially eliminate hypercholesterolemia and normalize blood pressure, on the other hand, daily alcohol consumption easily becomes a bad habit. Over time, a person ceases to control the amount he drinks and achieves the opposite effect: cholesterol concentration increases, blood pressure rises. This leads to a manifold increase in the risk of developing cardiovascular diseases. The norm is to consume up to 2 servings of alcohol per day for men, and no more than 1 for women. One serving is the equivalent of 14 g of pure alcohol or 350 ml of beer, 150 ml of wine, 45 ml of cognac or vodka.
Particular attention must be paid to diet. A balanced diet helps normalize fat metabolism and achieve a healthy weight. Basic nutritional rules for high cholesterol and atherosclerosis:
- Don't overeat. Monitor your daily calorie intake and eat small meals often. For snacks, use fruits, vegetables, nuts, and seeds.
- Drink 1.5-2 liters of water daily. Its deficiency leads to increased cholesterol levels.
- Give preference to fats rich in unsaturated fatty acids. There are many of them in vegetable oils, nuts, and seeds. An exception to this rule is palm and coconut oil. The first of them is often used for the production of various finished products: pay attention to their composition.
- Eliminate trans fats. They are formed during the industrial processing of vegetable oils, which increases the shelf life of the product. Therefore, when purchasing any prepared food that may contain margarine or other plant-derived lipids, be sure to review the nutritional information. A responsible manufacturer will always indicate the content of trans fats.
- Eat a lot of vegetables, fruits, greens, cereals, legumes. These products are rich in minerals, vitamins, and fiber, which prevents the formation of atherosclerotic plaques. From the point of view of the presence of dietary fiber, bran is a very valuable product. They can be added to almost any dish: omelettes, salads, baked goods, stews, soups. The taste of the food will not suffer from this, but the satiety and nutritional value will increase.
- Watch for foods containing omega-3 fatty acids. They help the body normalize fat metabolism and improve heart function. The leaders in the content of omega-3 fatty acids are fatty fish and flax seeds. Seaweed, spinach, mustard oil, and seafood are considered good sources.
Medications
Medicines are prescribed to people who have not responded to non-drug treatments or who are at high risk of developing complications from the disease. Taking medications does not replace the need to follow a diet or give up bad habits. The best medicines are effective only with an integrated approach.
Goals of drug therapy.
| Target | Group of drugs |
| Reduce the content of bad cholesterol, increase the concentration of good cholesterol. Stop the growth of existing atherosclerotic plaques and prevent new ones from forming |
|
| Prevent blood clots | antiplatelet agents (disaggregants): clopidogrel, aspirin |
| Normalize blood pressure |
|
Usually the patient is prescribed at least one medicine from each group. To achieve a lasting effect, most of them must be taken for life.
Surgical intervention
Surgical treatment of plaques in the vessels of the neck is required when there is significant narrowing of the lumen of the carotid artery. This is the only method that eliminates the cause of the blockage - cholesterol plaque.
The gold standard for surgery for cervical artery atherosclerosis is carotid endarterectomy (CE). During the operation, the surgeon excises the atherosclerotic plaque along with a piece of the inner layer of the artery (intima). Most often, CE is performed under general anesthesia, but with the appropriate equipment and highly qualified surgeon, only local anesthesia is possible.
Absolute indications for surgery:
- narrowing of the lumen of the vessel by 70-99%;
- presence of symptoms of cerebrovascular insufficiency;
- tortuous shape of the carotid arteries, aggravating the course of the disease.
CE cannot be performed in patients with:
- serious disorders of the central nervous system that occur after cerebral infarction or aging;
- brain tumors;
- incurable diseases that limit the patient’s life expectancy;
- myocardial infarction in the last 6 months;
- hypertension.
If there are contraindications or the need for emergency surgery, another type of operation is preferred - carotid angioplasty with stenting. It is effective in the symptomatic course of the disease with a narrowing of more than 50%, and in the asymptomatic form with a narrowing of more than 80%.
Carotid artery stenting.
During the procedure, the surgeon expands the narrowed area using a special miniature balloon located at the end of the catheter. It is injected into the vessel under the control of a special device that visualizes the artery. After expanding the lumen, a frame is installed inside the affected vessel - a stent, which prevents the development of re-stenosis.
Folk remedies
Alternative medicine manuals contain many recommendations on how to get rid of plaques on the neck. The essence of most methods comes down to the use of herbal preparations that normalize cholesterol metabolism. The effectiveness of certain folk remedies has been confirmed by serious research. These include (4.5)):
- Garlic. It has a pronounced hypolipidemic property; it is eaten raw and added to various dishes. If you pour a head of peeled garlic into 500 ml of vegetable oil and let it sit for 2-3 days, you get a fragrant salad dressing. The spice helps fight arterial hypertension, one of the risk factors for stroke and heart attack.
- Flax seeds. Rich in alpha-linolenic acid, which is an omega-3 fatty acid. Eating 50 grams of seeds or flaxseed oil daily helps lower cholesterol levels. For better absorption, the grains need to be crushed before adding to salads and vegetable stews.
- Ginger root. Able to lower bad cholesterol and increase good cholesterol. This spice is very versatile: it can be added to drinks, meat dishes, vegetables, and baked goods. Fresh and dried root, as well as dietary supplements based on it, have the same effect.
- Soy, soy products. Reduces the concentration of bad cholesterol. In addition, tofu, soy milk, and beans are excellent sources of complete protein that can replace red meat, which is rich in saturated fat.
- Blueberry. Blueberries have the ability to lower plasma cholesterol and blood sugar. You can eat it fresh, add it to savory desserts, or take medications made from its extract.
- Turmeric. The use of this spice gives the dish a beautiful appearance and normalizes fat metabolism. The latter property helps prevent clogging of arteries with cholesterol plaques.
Official medicine recommends using traditional methods of treatment only in the early stages of the disease. More serious forms of atherosclerosis require medication, and the most advanced cases require surgery.
Signs of atherosclerosis on ultrasound, Doppler and duplex
Ultrasound is a quick and easy way to assess the condition of the vessels. This is one of the first instrumental diagnostic methods that is prescribed to a patient if a diagnosis such as atherosclerosis of the carotid arteries is suspected.
There are 2 methods of ultrasound examination of blood vessels:
- dopplerography;
- duplex scanning.
With Doppler ultrasound, you can only see the speed of blood flow and determine whether it is disturbed. Duplex scanning allows you to evaluate the anatomy of the vessel, its tortuosity, wall thickness and plaques. To diagnose atherosclerosis of the carotid arteries, this type of study is prescribed, since it is more informative.
Diagnostics
To make a correct diagnosis, it is necessary to undergo examination using the following methods:
- The patient's pulse is measured by palpation;
- An examination of the arteries is carried out using the auscultation method.
After this, the doctor refers the patient for instrumental diagnostics:
- Rheovasography method;
- To study the vessels of the head - Rheoencephalography;
- Methodology for diagnosing blood vessels - sphygmography;
- Vascular ultrasound;
- To detect sclerosis in the aorta, an x-ray with contrast is performed;
- Echo signs of stenosing sclerosis of arteries and non-stenosing atherosclerosis are detected by isotope aerography.
Diagnostic methods
Treatment methods
Treatment of atherosclerosis of the carotid arteries is a complex task. The method of therapy directly depends on the degree of vascular stenosis and the clinical picture, namely the presence of dyscirculatory encephalopathy and previous transient ischemic attacks and strokes. With a slight narrowing of the ICA and minor symptoms, the absence of acute conditions, you can manage only with drug therapy:
- Statins (Atorvastatin, Rosuvastatin) are the main type of drugs that slow down the progression of atherosclerosis. They reduce the concentration of cholesterol in the blood. The target low-density lipoprotein level is less than 1.8 mmol/L.
- Acetylsalicylic acid prevents the formation of a blood clot on an atherosclerotic plaque. If the patient has a peptic ulcer of the stomach or duodenum, he is preferably prescribed Clopidogrel.
- Means for lowering blood pressure. The patient needs to maintain blood pressure numbers at a certain level (<140/90 mm Hg, and for diabetes <130/80 mm Hg). For patients with atherosclerosis, ACE inhibitors (Perindopril, Lisinopril), sartans (Losartan, Valsartan) or calcium antagonists (Amlodipine) are preferred from all pharmacological groups.
- Medicines for diabetes. To stabilize blood glucose levels, hypoglycemic agents (Metformin, Glibenclamide) or insulin injections are prescribed.
What surgical treatment methods are applicable for cervical atherosclerosis? There are 3 main indications for their use:
- stenosis more than 70% with absolutely asymptomatic course;
- stenosis more than 60% with dyscirculatory encephalopathy;
- stenosis more than 50% if there were acute conditions (TIA or ischemic stroke).
Even if a person decides to undergo surgical treatment of an atherosclerotic plaque in the carotid artery, he must still take the medications listed above.
There are the following methods of surgical intervention for atherosclerosis of the ICA, each of which has its own subtleties and nuances:
- carotid endarterectomy – classic and eversion;
- stenting.
With classic endarterectomy, the operation is performed under general anesthesia. After dissection of the skin and subcutaneous fatty tissue, the carotid artery is isolated in the bifurcation area. Then, to avoid massive bleeding, the CCA is clamped. A longitudinal incision is made into the ICA, and the atherosclerotic plaque is carefully separated from the intima with a spatula.
The hole is closed with a patch made from the large saphenous vein or synthetic material. Its installation is preferable to simple suturing, as it has a lower rate of restenosis. This method is used when the plaque length is more than 2 cm.
Eversion endraterectomy differs in that it does not involve a longitudinal incision of the ICA, but its complete separation from the CCA, gradual eversion and cleansing of the cholesterol plaque. The advantage of this method is less deformation and a reduced risk of arterial restenosis. However, it can only be used for small lesions (up to 1.5-2 cm).
The third method is endovascular stenting. This operation is performed under local anesthesia. A catheter with a balloon is inserted through a puncture in the femoral artery. Under fluoroscopic control, he reaches the site of narrowing in the carotid artery. The balloon is inflated, then a metal stent (wire cylinder) is installed using another catheter to hold the vessel in an expanded state. This operation is less traumatic, safer, and does not require general anesthesia. However, it is less effective compared to endarterectomy, especially with a severe degree of stenosis (more than 85%).
Symptoms of cholesterol deposits in the vessels of the neck
At the initial stage of their formation, plaques located in the cervical arteries do not manifest themselves in any way. The fact that there are lipid deposits in the brachiocephalic arteries (BCA), in the carotid arteries or at the mouth of the right subclavian artery becomes clear only when the first symptoms appear. From the onset of pathological changes in the vascular wall to the appearance of the clinical picture, more than one year passes.
The fact that the vessels of the neck are clogged with fat can be suspected when the following symptoms appear: cephalgia, a feeling of numbness in the upper extremities, flashing black spots before the eyes, sleep disturbance, blurred vision, vestibular disorders, decreased overall tone of the body.
The picture shows the result of angiography. Arrows indicate areas of blockage of the internal and external carotid arteries.
To detect cholesterol plaques in the vessels of the neck, the patient must undergo an examination. Modern diagnosis of the disease includes ultrasound of the vessels of the head and neck, angiography of this anatomical area. In order for a doctor to assess the state of lipid metabolism, the patient must donate blood for a lipid profile. This analysis allows you to determine the level of serum cholesterol, as well as the ratio of all its fractions.
Expert advice: lifestyle changes
In addition to drug and surgical treatment, lifestyle correction plays an important role. I always recommend that my patients stop smoking, exercise regularly, and make changes to their diet (eat more vegetables, fruits and fish). Patients with diabetes need to periodically donate blood for glycated hemoglobin, follow a low-carbohydrate diet, visit an endocrinologist and take prescribed medications to lower blood sugar.
Treatment and prevention
The level of development of modern medicine makes it possible to almost completely stop the progression of atherosclerosis. This means that if you identify the disease in the early stages, when irreversible processes have not yet occurred, you can protect yourself from serious consequences. It is necessary to fight the root of the problem - you need to normalize the level of cholesterol in the blood.
Treatment of atherosclerosis, first of all, begins with lifestyle modification - increasing physical activity and normalizing nutrition. Harmful foods that contain a large amount of animal fats, fast food, and fried foods are excluded from the diet. You should limit baked goods, salted and smoked foods. You need to eat more vegetables and fruits, give up negative habits. In addition to the therapeutic effect, this lifestyle is an excellent prevention of atherosclerosis and other pathologies of the cardiovascular system.
Atherosclerotic lesions of other vessels of the neck: signs, diagnosis and treatment
Atherosclerosis of the vertebral arteries is less common and develops at a later age than the carotid arteries. However, it is responsible for 20% of ischemic strokes in the occipital region of the brain.
Clinical symptoms are as follows:
- vision problems - double vision, flashes, lightning, blurred or loss of visual fields;
- hearing loss, tinnitus;
- imbalance, body instability when walking or standing;
- dizziness, sometimes so severe that it causes nausea and vomiting.
A very characteristic sign of damage to the vertebral arteries are drop attacks. These are sudden falls without loss of consciousness that occur during sudden turns or throwing back the head. With severe stenosis, the acute conditions described above (TIA and stroke) may develop. Diagnosis is carried out using the same methods as for atherosclerosis of the carotid arteries - Doppler ultrasound and duplex scanning. CT angiography is sometimes used.
Drug therapy remains unchanged, but the indications for surgery are somewhat different.
If the patient does not have any symptoms of cerebrovascular accident, then surgery is not performed, even despite the severe degree of stenosis.
If clinical signs are present and stenosis is more than 50%, surgical intervention is performed. Preference is given to open endarterectomy, since endovascular stenting in such patients has shown very low effectiveness.
Treatment
A number of techniques are used to treat non-stenotic atherosclerosis. The patient must always adhere to all doctor's recommendations. Only in this case will he be able to prolong the period of active life and avoid negative consequences (complete blockage of blood vessels, strokes and death).
To prescribe optimal therapy for non-stenotic atherosclerosis, the doctor:
- Determines the stage of the disease.
- Records general symptoms.
All medications are prescribed individually and take into account the patient’s condition.
As a rule, patients take:
- Anticoagulants. This reduces the risk of blood clots and strokes.
- Medicines to lower blood pressure (if it increases). Such remedies can reduce the load on the arteries, dilate blood vessels, improve blood flow and relieve spasms.
- Medicines to lower cholesterol levels. Typically, such drugs are taken throughout life after atherosclerosis of the brachiocephalic arteries is detected.
It is also very important to constantly monitor the patient's lipid balance. If necessary, sedatives are prescribed. They allow you to normalize the emotional background, avoid depression, improve the quality of sleep, and get rid of headaches. Patients are often prescribed physiotherapy.
The decision to undergo surgical intervention is usually made if the passages are significantly narrowed and the disease has reached a high stage of development.
The following types of operations are carried out today:
- Removing part of the artery and replacing it with a prosthesis.
- Stitching a vessel to reduce its size.
Endovascular operations are increasingly being performed. They are as safe as possible, and recovery from them takes a short period of time.
Are you interested in all the features of therapy? Contact our specialists. You will not have to overpay for a consultation. Prices are indicated on the website. Note! The cost is approximate. The exact price of therapy will be announced by your attending physician. In any case, you will not overpay. Our private clinic in Moscow adheres to a loyal pricing policy.
Case study: atherosclerosis of the vertebral arteries
A 57-year-old man began to complain of slight dizziness and hearing loss.
Those close to him told him that his gait had become uneven. A week ago, when he suddenly turned his head, he lost his sense of balance and fell, after which the patient came to the doctor. Upon questioning, it turned out that he suffers from hypertension and type 2 diabetes. Takes prescribed medications irregularly. When measuring blood pressure, the tonometer showed a value of 165/95 mm Hg. Art. Suspecting atherosclerotic lesions of the vertebral arteries, I ordered a duplex scan, during which stenosis of the right VA up to 65% and narrowing of the left VA up to 40% were detected. I referred the patient for surgical treatment.
Endarterectomy of the right VA was performed. The patient was also prescribed drug therapy - Rosuvastatin, Acetylsalicylic acid, Perindopril, Metformin. The patient noted a significant improvement - the dizziness stopped and a sense of balance returned.
Drug treatment
It is usually called conservative, because it allows patients to be treated without surgery and modern medical equipment. The medications prescribed by the cardiologist (statins) help reduce lipids in the blood vessels. Normalizing cholesterol levels is an important step in maintaining the patient’s life. This will also help fix the size of the atherosclerotic plaque and prevent its further growth.
If blood pressure is excessive, part of the medication will be aimed at reducing this indicator. This will help the patient improve their well-being and quality of life.
It is mandatory to take medications that thin the blood. This is necessary in order to prevent the appearance of new plaques. By the way, even therapists today prescribe such drugs to people over 50 years of age. With age, blood becomes more viscous. Against the background of weakened and damaged blood vessels, this becomes dangerous, because the body will perceive any damage as a call to action and will actively begin to thicken this area of blood, as well as increase the number of platelets.
All these medications can be called not even a treatment, but a way of life for a person who is a patient of a cardiologist. It is important to take all medications regularly and not occasionally.
While taking medications, it is important to exclude risk factors. It is worth reviewing your diet and introducing fiber-rich foods into it. As for physical education, it is better to contact a specialist. The fact is that it is impossible for an unprepared person to start doing physical exercise intensively. Most likely, the patient is overweight, and not all types of activities will be suitable for him. Over time, the amount of physical activity can be increased, but this must be done gradually and only under the supervision of an experienced trainer.
It is important to monitor your body throughout the treatment period. As the situation improves, the content of individual blood components will also change. The risks of progression and severe consequences will also tend to zero.
Non-stenotic atherosclerosis of the arteries of the lower extremities
In the absence of blockage of blood vessels, symptoms are usually absent or mild. However, when the arteries in the leg become narrow enough to prevent the flow of nourishing, oxygen-rich blood to the affected limb, lactic acid begins to accumulate in the muscles, leading to pain during exercise.
Pain associated with exercise in atherosclerosis of the arteries of the lower extremities is called “intermittent claudication . It may be described as leg fatigue, muscle cramps, or severe muscle pain.
Similar symptoms may also be found in venous disease, arthritis, neuropathies, or spinal diseases, but patients with claudication due to arterial atherosclerosis experience symptoms only with exercise. During rest, the pain goes away within a few minutes. Patients with multiple severely blocked arteries may experience severe restriction of blood flow. In such cases, pain occurs in the limbs at rest, and in severe conditions, non-healing ulcers or gangrene appear.
Symptoms that may appear with atherosclerosis of the leg arteries include the following:
- Exercise-related leg pain.
- Numbness of the legs or feet at rest.
- Cold extremities.
- Muscle pain in the thighs, calves or feet.
- Hair loss on legs.
- Change in skin color (pale or bluish).
- Weakened or absent pulse in a limb.
- Walking/gait disturbance.
The diagnosis of non-stenotic atherosclerosis of the arteries of the lower extremities is usually made on the basis of a thorough history and physical examination. Arterial Doppler studies are often performed to provide a baseline study and help determine the extent of vessel blockage.
When surgery or endovascular therapy is considered, more detailed imaging will be required to plan appropriate treatment. Although the gold standard for preoperative planning is arteriography, other less invasive alternative studies, including CT angiography and MR angiography, are also used.
Diagnosis of non-stenotic atherosclerosis of arteries
After collecting complaints and an objective examination, the doctor, as a rule, prescribes laboratory tests such as a general and biochemical blood test, lipid profile. Afterwards, instrumental diagnostics are necessarily carried out, with the help of which the exact condition of the blood vessels is determined.
- Ultrasound examination of the carotid artery
This diagnostic method includes Doppler ultrasound. This test uses sound waves to create real-time images of the arteries and detect narrowing or stenosis. Doppler is a special ultrasound technique that is non-invasive and safe and can help detect areas of abnormal blood flow in the arteries.
- Computed tomographic angiography (CT angiography, CTA)
A CTA is performed using a CT scanner to produce detailed images of arteries from anywhere in the body, including the neck. The study is especially useful for those patients who have pacemakers or stents implanted.
- Magnetic resonance angiography (MRA)
This non-invasive test provides information similar to CTA, while the patient is exposed to minimal ionizing radiation.
- Cerebral angiography
Also known as intra-arterial digital angiography (IADSA). Cerebral angiography is a minimally invasive test in which a catheter is guided through an artery to the area of interest. Contrast material is injected through a tube and images are captured using X-rays.