Causes
This disease is called phlebectasia, which can appear on a person’s neck on both the right and left. The reasons for the expansion of the right or left jugular vein are the following factors:
- serious disruption of the venous valves;
- valves are not able to carry out processes of control and regulation of blood flow;
- the walls of blood vessels are stretched, which interferes with the functioning of the valves;
- the release of blood from the veins that are located under the muscles.
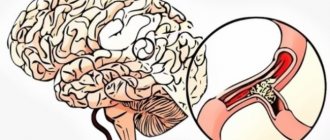
As a result, there is serious dysfunction of the venous system, which becomes the cause of pathology. The jugular vein is anterior, internal, external. Its purpose is to ensure constant transfer of blood between the brain and neck. Therefore, pathologies in this area of the body are extremely dangerous for humans.
The reason for the expansion of the jugular vein is often various injuries of the back, neck, cervical spine, and head. The disease can also be triggered by a blow to the back, causing injuries to the back and spine, fractures of ribs and bones, which can result in venous stagnation.
Separately, it is necessary to note other factors that negatively affect the jugular veins:
- constant and prolonged sitting in a rather uncomfortable position, which may be related to work or lifestyle;
- genetic predisposition of blood vessels to diseases;
- heart disease, including ischemic and hypertensive, defects and insufficiency;
- the presence of tumors of varying severity;
- osteochondrosis;
- diseases of the endocrine system.
Usually, dilatation of the jugular vein is caused by several reasons at once, so seeing a doctor is a mandatory measure.
Symptoms of the disease do not appear immediately, sometimes even within several years. Signs that the neck is not in order are that there is a significant increase in the veins in the neck - the upper vessels become blue, and the lower ones clearly appear under the skin.
At this stage, the sick child does not yet feel obvious discomfort, pain or anxiety in the neck area. If the disease progresses, then pressure begins on the left or right, especially if you move your head, talk or bend over.
The neglect of the pathology causes severe pain in the throat and neck, the voice begins to hoarse, and breathing becomes difficult. This is evidence that the disease has entered the active phase; it is necessary to undergo urgent diagnosis. The doctor makes a final diagnosis only after receiving the results of clinical tests and examination. In order to establish the degree of development of the disease and the causes of its occurrence, a set of special instrumental studies is carried out.
This may be a scan of the neck vessels or multislice tomography.
Phlebectasia has no time limits and occurs in both adults and children.
Causes of dilatation of the jugular vein in the neck:
- Injured ribs, cervical spine, spine, which provoke stagnation of venous blood.
- Concussion, osteochondrosis.
- Dysfunction of the cardiovascular system - heart failure, hypertension, ischemia.
- Endocrine disorders.
- Sedentary work for long periods of time.
- Tumors of different ethnogenesis (benign and malignant).
It takes time and accompanying factors for pathology to occur. Therefore, it is very important to identify it early, since the disease leads to disruption of the valves.
Cervical varicose veins occur in every third inhabitant of the planet. But for the development of pathology, predisposing factors are needed:
- natural lack of connective tissue development;
- restructuring of the hormonal system;
- spinal and back injuries;
- passive lifestyle;
- poor nutrition.
The hormonal factor concerns women more. During puberty and pregnancy, there is a risk of vein swelling.
Also important factors in the occurrence of phlebectasis are stress and nervous breakdowns. The neck veins have nerve endings. In normal condition, they form elastic venous vessels. But as soon as a person gets nervous, the pressure in the veins increases and elasticity is lost.
Alcohol, smoking, toxins, and excessive physical and mental stress negatively affect the normal circulation of venous blood.
Prevention of jugular vein phlebectasis
Preventive measures should be aimed at combating physical inactivity. For example, when working sedentarily, you need to do periodic warm-ups. A contrast shower is recommended to strengthen blood vessels and increase their elasticity.
It is also necessary to pay attention to the daily diet, which should include foods that help prevent the formation of blood clots and strengthen blood vessels: beets, tomatoes, ginger, lemons, apple cider vinegar, cocoa, fatty fish, garlic, onions, cherries, raspberries, strawberries and etc. Traditional methods offer treatment with decoctions of medicinal herbs. The most popular in this case is sage decoction, which is used for a month once a year.
Thus, we received an answer about what phlebectasia is and developed a general treatment and prevention scheme. The disease does not depend on age and can occur in both adults and children.
Types of jugular vessels
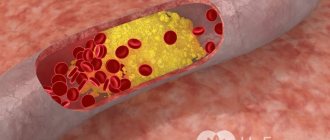
Thrombosis, or the appearance of a blood clot inside a vessel, forms mainly in the presence of chronic diseases in the body. If a blood clot appears in a vessel, there is a danger of it breaking off and blocking vital arteries.
In this case, the doctor suggests taking anticoagulants - heparin and fibrinolysin. To relieve inflammation, relax muscles and thin the blood, and, consequently, to resolve a blood clot, the administration of nicotinic acid, antispasmodics, and venotonics is prescribed. The operation is rarely used.
The jugular veins are a set of vessels that take blood flow from the head, brain, and neck and carry it further to the area under the collarbone. Their main functional load is to prevent blood stagnation in the head, brain and neck. For a person to feel well, it is necessary that these veins function correctly. The presence of diseases leads to serious consequences. The jugular canals contain three main vessels:
- Anterior (the main functional load is the timely outflow of blood from the chin. Located in the middle part of the cervical region, it also passes through the tongue and jaw muscles. Connects on both sides to form an arch);
- External (located in the tissues of the neck. Blood departs from the facial part, the external part. It is easy to detect during coughing, difficult physical work, when turning the head to the side);
- The internal jugular vein (is a fairly large canal in relation to the other two. It narrows and expands very easily when blood is pushed out. This process is carried out due to thin walls and a diameter of no more than 20 mm. Equipped with a valve system).
Diagnosis of phlebectasia
Laboratory tests include several general and detailed tests and taking a puncture from a vessel in the neck. A doctor can prescribe one or several types of instrumental diagnostics in order to have sufficient information about the disease. It is possible that more specialized specialists will be invited to clarify the causes of inflammation of the jugular vein: oncologist, endocrinologist and neurologist.
Drug treatment is carried out strictly under the supervision of doctors. If the vein causes a negative reaction in the body, then surgery is performed. The affected part of the vein is removed, and healthy ones are connected to form a healthy vessel.
Prevention of the disease is a set of mandatory measures that help avoid inflammation from developing into a serious pathology:
- No stress on the body and neck if there is the slightest predisposition to the expansion of this vein.
- Elimination of vein diseases that cause their expansion.
- Regular examinations.
- Healthy lifestyle and proper nutrition.
Prevention is especially important for those who have a hereditary predisposition to the disease.
The jugular vein is a blood vein that is responsible for the process of blood circulation from the brain to the cervical region. In certain areas of the brain, the blood absorbs carbon dioxide and various toxic substances. The jugular vein delivers unpurified blood to the heart for filtering. It is the proximity of the vein to such an important human organ that prompts us to take seriously any changes in its functioning.
Therefore, if the jugular vein in the neck is dilated, examination and therapy are required after the exact causes of the pathology are established.
If the dilatation of the jugular vein is in the first stage, then a visual examination by a doctor is quite sufficient. In the second and third stages of the disease, more serious studies are used.
To make a diagnosis when pain and blood circulation problems occur, laboratory tests are used - a general blood test and instrumental tests. Instrumental ones include:
- Ultrasound or computed tomography of the cervical, thoracic and skull.
- Diagnostic puncture.
- MRI with contrast agent.
- Doppler ultrasound of neck vessels.
These are the main diagnostic methods that are used to make a final medical opinion.
In certain situations, it is better to diagnose phlebitis with the help of a tandem of doctors of various specializations (therapist, neurologist, vascular surgeon, cardiologist, endocrinologist, oncologist). This allows you to prescribe more precise conservative treatment.
Treatment depends on the expansion of the internal jugular vein on the right or internal on the left, the results of the tests performed, and the degree of influence of the disorders on the entire body. Often, during one therapeutic complex, not only varicose veins are cured, but also other physiological disorders.
The occurrence of expansion on the right does not pose a particular threat to the patient. The pathology on the left side is much more dangerous. This is due to the impossibility of a thorough diagnosis due to the risk of damage to the lymphatic system.
A therapeutic course of medications relieves inflammation, removes swelling, and strengthens blood vessels. With long-term administration of the drug, the installation of a venous catheter is practiced.
At the third stage of the disease, surgical intervention is indispensable. The affected parts of the vein are surgically removed, and healthy ones are connected into one vessel.
If symptoms of the disease occur, you should consult a physician. After consultation, he can refer you to see a phlebologist.
Based on the patient’s complaints, the phlebologist conducts an initial visual examination, the result of which should be the identification of pronounced symptoms of venous disease.
In addition, all patients suffering from vascular diseases must be registered with a cardiologist. Jugular vein diseases must be identified in the early stages. Be aware of possible serious consequences.
Diagnosis of jugular vein phlebectasis
When diagnosing and carrying out therapeutic measures, a specialist should focus on phlebitis as the main disease, considering ectasia as the most obvious symptom of the disease. The doctor receives the initial information that allows him to make a decision about sending the patient for a specialized examination from the initial survey and examination of the prospective patient. To make a final diagnosis, one of the following methods can be used: duplex scanning, ultrasound, MRI (the use of contrast agents is recommended), venography. If the diagnosis is confirmed and/or the presence of cancer is suspected, a puncture is required.
Functional load
The entire jugular circulatory system, including the external jugular vessel, is necessary to maintain the life of the human body. It performs the following functions:
- Remove blood poor in oxygen, saturated with carbon dioxide, toxic substances, and decay products from vital organs, such as the brain, neck, eye area and head as a whole;
- Ensures normal blood circulation in the cerebral area.
The external jugular vein is formed by the fusion of two venous trunks, among which there is a large anastomosis between the external jugular vein and the mandibular vein. Various factors can cause improper blood circulation in this area. It is necessary to seek help from a doctor as soon as possible. With minor violations, patients report symptoms such as headaches and general malaise. In severe cases, doctors diagnose various diseases. In this situation, a qualified approach and the prescription of adequate treatment are already required.
The internal jugular vein collects blood from the head. Its main task is to promptly drain venous fluid from the brain, cervical spine, eyeballs, tongue, and chin. Due to the fairly large diameter, up to 2 cm, as well as the thin walls of the canal, the vessel narrows and stretches if necessary to allow a large volume of blood to pass through.
The internal canal originates in the region of the jugular foramen in the bone structure of the skull and is a continuation of the sigmoid sinus. After exiting and opening the bone, the vein immediately expands, forming a bulb, then continues its path to the junction of the clavicle and sternum. Passes behind the muscle fibers. Reaching the surface, the canal passes next to the carotid artery (back and outside).
The internal jugular vein flows into the subclavian vein. Until the moment of union, the internal channel increases in diameter, creating the lower bulb. Then there is a connection with the subclavian, where the brachiocephalic vein begins. In the area where the internal jugular vein meets the subclavian vein there are valves.
The main functional load of this type of channel is the timely outflow of blood from the head, neck, brain, eyes and ears. Intracranial vessels collect venous fluid from the following parts:
- orbital and auditory region;
- meningeal vessels;
- cerebral canals;
- sinuses of the dura mater;
- diploic veins of the cranium.
The main functions are to remove toxins and waste products from the head and neck, and to ensure proper blood circulation in the system. Tributaries located outside the skull take blood flow from the soft tissues of the head, skin, outer surface of the skull, and also the facial part. Both internal and external flows of the jugular canals are interconnected with emissary ones, which enter through openings in the bone structure of the skull.
Features of the pathology
Phlebectasia, or dilatation of the jugular vein, is a disruption of the functioning of blood vessels and valves. Vascular valves cease to regulate the flow of venous blood. The blood, in turn, begins to accumulate, forming clots. A large number of them causes a process of dysfunction in the functioning of almost the entire venous network of the body. Normal blood circulation stops and the person becomes ill.
This condition largely depends on the anatomical structure of the veins.
Each of the jugular veins is divided into anterior, external and internal and has its own location:
- The internal jugular vein stretches from the base of the skull and ends near the subclavian fossa. There she pours venous blood, which comes from the skull, into the large brachiocephalic vessel.
- The beginning of the external jugular vein is located under the auricle. From this point it descends down the upper part of the sternoclavicular muscle. Having reached its posterior edge, it penetrates the vessels of the internal jugular and subclavian veins. The external vessel has many branches and valves.
- The anterior jugular vein is initially located on the outer surface of the mylohyoid muscle, moves along the sternothyroid muscle and passes near the midline of the neck. It enters the external and subclavian jugular veins, forming an anastomosis.
The anterior jugular vein is very small and forms a pair of vessels, that is, it is paired.
About the cost of the operation
The cost of phlebectomy in Moscow averages about 30 thousand rubles, which ranges from 20 to 40 thousand, depending on the scope of the preoperative examination, the qualifications of the surgeon and the conditions of the postoperative period.
Problems with blood vessels arise quite often, so phlebectomy of the veins of the lower extremities is included in compulsory medical insurance. However, the policy provides only the classic version of the procedure. If it is necessary to use other methods, the patient pays for them independently.
Symptoms
If the jugular veins are even slightly dilated, then specific signs appear indicating pathology. They depend on the stage of the disease:
- Stage 1. A slight swelling (enlargement) in the neck that does not cause discomfort or pain. Determined during a visual inspection.
- Stage 2. Pulling pain and the appearance of increased intravenous pressure with rapid movement and sudden turns of the head.
- Stage 3. The pain is sharp, intense, there is hoarseness and difficulty breathing.
If the internal jugular vein expands, serious disruptions occur in the functioning of the circulatory system. This situation requires a thorough diagnosis of the causes of the pathology and comprehensive treatment.
Diseases and changes
The reasons for the expansion make it known about the dysfunction of the circulatory system. This situation requires an immediate solution. You should know that there are no age restrictions for YV pathologies. They affect both adults and children.
Phlebectasia
A thorough, accurate diagnosis is necessary, the result of which should be the identification of the causes of the pathology, as well as the prescription of comprehensive effective treatment.
Extensions occur:
- in case of stagnation, due to injury to the neck, spine or ribs;
- for osteochondrosis, concussion;
- for ischemia, hypertension, heart failure;
- for endocrine disorders;
- with prolonged sitting at work;
- for malignant and benign tumors.
Phlebectasis can also be caused by stress and nervous tension. With nervous excitement, pressure can increase, resulting in a loss of elasticity of the walls of blood vessels. This can lead to valve dysfunction. Therefore, phlebectasia needs to be detected early.
Thrombosis
It may occur due to the presence of a chronic disease in the body. If they are present, as a rule, blood clots form in the vessels. Once a blood clot has formed, there is a possibility of it breaking off at any time, which entails blocking vital arteries.
Signs of thrombosis:
- sometimes pain occurs in the hand;
- swelling of the face;
- appearance of venous networks on the skin;
- When turning the head, pain occurs in the cervical region and neck.
The result of thrombosis can be rupture of the jugular venous channels, which leads to death.
Inflammatory changes occurring in the mastoid process or middle ear are called phlebitis. The cause of phlebitis and thrombophlebitis can be:
- bruises, wounds;
- placement of injections and catheters in violation of sterility;
- penetration of medications into the tissues around the vessel. This can often be triggered by calcium chloride when it is injected past an artery;
- infection from the skin.
Aneurysm
A rare pathology is an aneurysm. It can even occur in children at an early age from 2 to 7 years. The pathology has not been fully studied. It is believed that its occurrence occurs from improper development of the base of the venous bed, or rather its connective tissue. It is formed during intrauterine development of the fetus. The anomaly does not manifest itself clinically. It can only be noticed when a child cries or screams.
Symptoms of an aneurysm:
- headache;
- anxiety;
- sleep disturbance;
- fast fatiguability.
Treatment consists of draining venous blood and vascular prosthetics.
The complex of jugular vessels drains vital organs, so it is very important to monitor the proper functioning of the circulatory system. Among the most common diseases diagnosed by doctors are thrombosis, dilation or ectasia (widening of the lumen), inflammatory processes (phlebitis), and congenital malformations.
If you discover any problem with the venous channels, you must visit a phlebologist as soon as possible and undergo an examination. Only a correct diagnosis will allow you to avoid advanced processes, severe complications and even death. It is necessary to take care of your health from a young age. The earlier the pathology is detected, the easier it is to cure. It is recommended to regularly visit specialists and undergo preventive examinations in the clinic.
It should be clearly understood that any pathological process in the venous system can cause death, so you should not delay the treatment of problems. Among the most common diseases are:
- phlebitis (the disease is characterized by an inflammatory process of the venous walls. The degree of the disease is expressed by various symptoms. Patients note swelling in the neck, pain. In severe situations, acute inflammation is diagnosed, often purulent; with such a disease, the correct outflow of venous blood is disrupted);
- thrombosis (the formation of blood clots causes a narrowing of the lumen or its complete closure. Blood clots can also break off and move towards vital organs. In this case, instant death occurs. Among the accompanying symptoms of thrombosis, there is a sharp pain in the clavicle area, neck radiating to the arm, pain in the cervical area, general malaise, tissue swelling, itching, chills, blue discoloration of the skin);
- ectasia (expansion of the lumen of the vessel. In this case, swelling of the blood vessels becomes clearly noticeable. There is a feeling of compression in the neck area, loss of voice is observed, respiratory function is impaired. Symptoms intensify when turning the head).
The danger of the above diseases lies in their proximity to the brain. What causes the malfunction of many organs and systems. It is necessary to treat diseases in a timely manner and regularly visit a specialist.
Treatment
There are no specific treatment methods for hypoplasia of the vertebral arteries today. If the disease does not produce clinical symptoms and is detected by chance during a routine examination, specialists usually choose observation tactics .
The patient is advised to give up bad habits, normalize his daily routine and limit his time working at the computer. Patients are also advised to undergo physical therapy, moderate physical activity and proper sleep on anatomically correct pillows.
Hypoplasia tends to worsen in spring and autumn, so at this time you should be especially careful about your health.
At the stage of pronounced clinical symptoms of hypoplasia of the right or left vertebral artery, conservative treatment with vasodilators - they eliminate unpleasant phenomena and improve the patient’s quality of life. In cases where there is a risk of blood clots, taking anticoagulants (blood thinning medications) is indicated.
Phlebectasia in children
Vein enlargement occurs at any age. But it is more dangerous for children. Most often, phlebectasia in a child is detected at birth, but cases of pathology appearing at the age of 3–5 years are not uncommon.
The main symptomatic indicators: tumor formation, dilated blood vessels, increased temperature.
The treatment uses approaches used for the recovery of adults. The only difference is that phlebectasia in children is most often treated through surgery.
Contraindications and prevention
People suffering from pathology and having a hereditary predisposition to it are contraindicated:
- sedentary work and vice versa - excessive physical activity;
- frequent stressful situations;
- bad habits;
- ignoring chronic diseases;
- consumption of fatty, spicy, smoked foods, canned food, sweet carbonated drinks.
To prevent jugular vein phlebectasis from occurring, it is advisable to take preventive measures. The main preventive measures are:
- regular medical examination;
- avoiding stressful situations and physical activity;
- timely removal of small enlargements using special ointments;
- treatment of chronic diseases;
- healthy lifestyle.
By following these recommendations, the disease will not cause significant harm to the patient’s health.
Together, the vessels that make up the jugular veins perform the most important functions in the body. Violations in their work lead to serious consequences. To exclude the occurrence of venous pathologies, you need to know more about the jugular vein and possible problems associated with it.
Treatment of jugular vein phlebectasia
In the absence of rapid development of pathology and the presence of complications in the form of ectasia against the background of standard phlebitis, aseptic phlebitis, periphlebitis, symptomatic conservative therapy is used. The drugs of choice are the following:
- Anti-inflammatory drugs for topical use: diclofenac, ibuprofen, indomethacin.
- General antihistamines: diphenhydramine, suprastin.
- Antibiotic drugs (except aseptic phlebitis): amoxicillin, tetracycline.
Attention is paid to the root cause of the pathology in order to direct therapeutic measures to treat the underlying disease. In most cases, surgical intervention is not required, but the patient should be under periodic monitoring (visiting a doctor at least once every three days until the pathology regresses).
In the absence of rapid development of the pathological condition with thrombophlebitis, the following medications are prescribed in addition to the above-described treatment:
- Local alcohol compresses.
- Local anticoagulant drugs: heparin ointment and so on.
- Drugs that reduce blood clotting: aspirin, aescusan, phenylin, and so on.
If there is a pronounced decrease in the lumen of the jugular vein due to blood clots, which significantly impairs blood circulation, and the lack of proper results from the use of conservative therapy, surgical intervention is necessary to restore adequate blood flow and prevent complications.
Location
The venous vein consists of 3 independent venous channels. Accordingly, their anatomy is separate.
Internal
It has a relatively wide trunk, compared to the other 2. In the process of pushing out blood, it easily expands and contracts, thanks to its thin walls and diameter of 20 mm. The outflow of blood in a certain amount occurs with the help of valves.
As the lumen expands, the superior bulb of the jugular vein is formed. This occurs at the moment when the IJV enters from the hole.
Typical anatomy diagram:
- start – area of the jugular foramen;
- localization - the skull, or rather its base;
- further - its path goes down, the place of localization is in the posterior muscle, the place of attachment is the collarbone and sternum;
- the place of intersection with the posterior muscle is the area of its lower and posterior parts;
- after that the path is laid along the trajectory of the carotid artery;
- a little lower it comes forward and is located in front of the carotid artery;
- then, together with the carotid artery and the vagus nerve, they are directed through the site of expansion;
- as a result, a powerful bundle of arteries is created, which includes the carotid artery and all jugular veins.
Blood enters the IJV from the tributaries of the skull, the location of which is the cranium and outside it. Comes from vessels: brain, eye, auditory.
Also suppliers are the dura mater of the brain, or rather its sinuses.
Outdoor
Location: neck tissue. Blood is directed from the face, head and outer part of the cervical region. Perfectly visible visually when coughing, screaming or stress.
- origin - lower angle of the jaw;
- further down the muscle that attaches the sternum and clavicle;
- crosses the outer part of the muscle. The place of intersection is the area of the rear and lower part.
It has only 2 valves located in the initial and middle parts of the neck.
Front
The main task is to carry out drainage from the chin area. Location: neck, middle line.
- passes along the muscle of the tongue and jaw (along the front), downwards;
- Then, on both sides, the veins connect with each other, and a venous arch is formed.
Sometimes an arc of channels collected together forms a middle one.
The external jugular vein is located very close to the skin. In diameter, it occupies a middle position among all venous pathways. Not the biggest. It consists of two large vessels, among which are:
- Auricular (located behind the auricle, hence the name);
- The vessel that connects the external vein with the mandibular venous trunk.
The external jugular tract has its own branches and a system of valves that prevent reverse blood flow. Connected to this venous route are:
- transverse jugular veins;
- anterior jugular;
- suprascapular;
- posterior ear;
- occipital branch.
In the absence of medical education, immediately accurately determining the location of the jugular vein will be quite problematic. In simple words, its beginning is located behind the auricle, approximately in the area of the angle of the lower jaw. Then it passes down from the outer part of the clavicular-sternal muscle up to its posterior edge. Then the vessel enters through the fascia of the neck and connects with the internal jugular vein, subclavian vein, or enters the venous angle.
The external jugular vein collects blood from the head, neck, eye area and brain. Its close location to the skin allows you to easily see it when turning your head to the sides, or coughing or strong tension during physical activity. It is secreted through the skin and can be easily felt with your fingers.