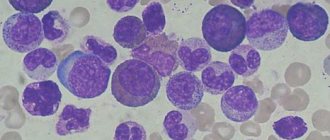
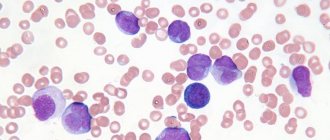
Blood picture in acute leukemia (blasts)
Acute leukemia is a group of severe blood diseases of a tumor nature, in which the pathological process begins at the level of hematopoietic precursor cells (stem cells), which lose their ability to mature to mature forms, which leads to failure of hematopoiesis and accumulation of immature blast forms in the bone marrow and blood .
The main substrate of the tumor is young, so-called blast cells.
Depending on the morphology and cytochemical parameters of cells in the group of acute leukemia, the following are distinguished: acute myeloblastic leukemia, acute monoblastic leukemia, acute myelomonoblastic leukemia, acute promyelocytic leukemia, acute erythromyelosis, acute megakaryoblastic leukemia, acute undifferentiated leukemia, acute lymphoblastic leukemia.
Etiology
The cause of acute leukemia and chronic myeloid leukemia in humans may be disturbances in the composition and structure of the chromosomal apparatus, hereditarily determined or acquired under the influence of certain mutagenic factors. One of them is ionizing radiation .
The cause of the development of leukemia is also the action of chemical mutagens . An increase in acute leukemia has been proven among individuals exposed to benzene, as well as among patients receiving cytostatic immunosuppressants (imuran, cyclophosphamide, leukaran, sarcolysin, mustargen, etc.); the frequency of acute leukemia among this group of patients increases hundreds of times. There are known facts of the occurrence of acute myeloblastic leukemia, acute erythromyelosis against the background of long-term chemotherapy for chronic lymphocytic leukemia, Waldenström's macroglobulinemia, multiple myeloma, lymphogranulomatosis and other tumors.
The role of hereditary defects in myeloid and lymphatic tissue predisposing to leukemia has been shown . Observations of dominant and recessive inheritance of chronic lymphocytic leukemia are described; a low incidence of this leukemia in some ethnic groups and an increased incidence in others is noted. More often in these cases, it is not the leukemia itself that is inherited, but increased variability—chromosomal instability, which predisposes the parent myeloid or lymphatic cells to leukemic transformation.
The use of chromosomal analysis has made it possible to establish that in any leukemia, a clone of tumor leukemia cells, the descendants of one initially mutated cell, spreads throughout the body. The instability of the genotype of malignant cells in leukemia causes the appearance of new clones in the initial tumor clone, among which the most autonomous clones are “selected” during the life of the body, as well as under the influence of therapeutic agents. This phenomenon explains the progression of leukemia and its escape from the control of cytostatics.
Content
- 1 Factors associated with increased risk of leukemia
- 2 Pathogenesis
- 3 Classification of leukemia 3.1 By type of course
- 3.2 According to the degree of differentiation of tumor cells
- 3.3 According to cytogenesis
- 3.4 Based on the immune phenotype of tumor cells
- 3.5 By the total number of leukocytes and the presence of blast cells in peripheral blood
- 6.1 Early experimental methods
Stages of leukemia
1) initial; 2) expanded; 3) remission (complete or incomplete); 4) relapse; 5) terminal.
The initial stage of acute leukemia is most often diagnosed when patients with previous anemia subsequently develop a picture of acute leukemia.
The advanced stage is characterized by the presence of the main clinical and hematological manifestations of the disease.
Remission may be complete or incomplete. Complete remission includes conditions in which there are no clinical symptoms of the disease, the number of blast cells in the bone marrow does not exceed 5% and they are absent in the blood. The composition of peripheral blood is close to normal. With incomplete remission, there is a clear clinical and hematological improvement, but the number of blast cells in the bone marrow remains elevated.
Relapse of acute leukemia can occur in the bone marrow or outside the bone marrow (skin, etc.). Each subsequent relapse is prognostically more dangerous than the previous one.
The terminal stage of acute leukemia is characterized by resistance to cytostatic therapy, pronounced inhibition of normal hematopoiesis, and the development of ulcerative necrotic processes.
In the clinical course of all forms there are significantly more common “acute leukemic” features than differences and features, but differentiation of acute leukemia is important for prognosis and selection of cytostatic therapy.
Definition of the concept and classification
The following definition of this disease is currently accepted.
Leukemia is a systemic blood disease characterized by uncontrolled proliferation and rejuvenation of hematopoietic elements with impaired maturation and metaplasia of hematopoietic tissue.
In this definition, it is necessary to highlight several important provisions:
• being systemic diseases of the blood, leukemias usually affect the entire hematopoietic system, including the erythropoietic, leukopoietic and thrombopoietic sprouts of the bone marrow;
• leukemia is based on uncontrolled growth and impaired differentiation (maturation) of hematopoietic cells, which, as is known, is observed in malignant tumors;
• with leukemia, metaplasia of hematopoietic tissue develops, in which one of the hematopoietic germs begins to develop in tissue atypical for it, for example: myeloid cells appear in lymphoid organs, lymphoid cells in the bone marrow. There are several classifications of leukemia, each of which is based on appropriate criteria that determine the characteristics of the disease.
I. Along the process:
• sharp;
• chronic.
Currently, with high-quality therapy, acute leukemia often progresses more favorably than chronic leukemia. Moreover, with aggressive chemotherapy for acute lymphocytic leukemia in children, complete recovery occurs in 70% of cases, and stable remission occurs in 90% of cases.
II. According to the source of formation of the leukemia tumor clone:
• myeloproliferative (myeloid leukemia);
• lymphoproliferative (lymphocytic leukemia).
III. Based on the number of leukocytes in the patient’s peripheral blood:
• leukemic (the number of leukocytes is more than 50 thousand/μl of blood);
• subleukemic (from 10 to 50 thousand/μl of blood);
• aleukemic (the number of leukocytes is within the normal range);
• leukopenic (less than 4 thousand/1 μl of blood).
Clinical picture
Clinical symptoms are very diverse and depend on the location and massiveness of leukemic infiltration and on signs of suppression of normal hematopoiesis (anemia, granulocytopenia, thrombocytopenia).
The first manifestations of the disease are general: weakness, loss of appetite, sweating, malaise, fever of the wrong type, pain in the joints, the appearance of small bruises after minor injuries. The disease can begin acutely - with catarrhal changes in the nasopharynx, sore throat. Sometimes acute leukemia is detected by a random blood test.
In the advanced stage of the disease, several syndromes can be distinguished in the clinical picture: anemic syndrome, hemorrhagic syndrome, infectious and ulcerative-necrotic complications.
Anemic syndrome is manifested by weakness, dizziness, pain in the heart, and shortness of breath. Objectively, pallor of the skin and mucous membranes is noted. The severity of anemia varies and is determined by the degree of inhibition of erythropoiesis, the presence of hemolysis, bleeding, etc.
Hemorrhagic syndrome occurs in almost all patients. Gingival, nasal, uterine bleeding, hemorrhage on the skin and mucous membranes are usually observed. Extensive hemorrhages occur at injection sites and intravenous injections. In the terminal stage, ulcerative necrotic changes appear at the site of hemorrhages in the mucous membrane of the stomach and intestines. The most pronounced hemorrhagic syndrome is observed in promyelocytic leukemia.
Infectious and ulcerative-necrotic complications are a consequence of granulocytopenia, a decrease in the phagocytic activity of granulocytes and occur in more than half of patients with acute leukemia. Pneumonia, sore throats, urinary tract infections, and abscesses at injection sites often occur. The temperature can vary - from low-grade to constantly high. Significant enlargement of lymph nodes is rare in adults, but quite common in children. Lymphadenopathy is especially characteristic of lymphoblastic leukemia. Lymph nodes in the supraclavicular and submandibular areas are more often enlarged. On palpation, the lymph nodes are dense, painless, and may be slightly painful if they grow rapidly. Enlargement of the liver and spleen is not always observed, mainly in lymphoblastic leukemia.
Symptoms and signs of leukemia
Leukemia is difficult to diagnose. People can have chronic leukemia for many years without any symptoms. In acute leukemia, the symptoms are similar to many other diseases. Doctors must eliminate possibilities such as rheumatic fever and anemia before diagnosing leukemia.
- Early symptoms resemble those of a cold or flu.
- A person with leukemia is likely to be pale, weak and tired, and may experience a slight fever.
- Anemia, a condition caused by a lack of red blood cells, develops in almost all leukemia patients.
- Other signs include easy bruising, frequent nosebleeds, night sweats, and scrapes and cuts that won't heal.
- Sometimes small red dots appear on the skin, similar to a rash.
- As the disease progresses, the person will feel very tired and have a high fever.
- The liver, spleen and lymph nodes swell and become very sensitive.
- Bones and joints usually become sore, and gums may swell and bleed.
All of these symptoms are caused by an increase in the number of abnormal white blood cells that fill the bone marrow and circulate in the bloodstream. Immature white blood cells do not leave enough space for normal red blood cells to supply the body with oxygen, so the patient feels tired and weak. The wounds do not heal and the nose bleeds because there are fewer platelets in the bloodstream. A person gets sick, the illness lasts a long time, because there are not enough full-fledged cells to fight infections. Some people experience joint or bone pain because abnormal cells move to the surface of the bones from the bone marrow.
But these symptoms do not necessarily mean that a person has leukemia. They can be caused by a number of other diseases. The only way a doctor can accurately diagnose leukemia during cancer treatment abroad is through a blood test. More and more patients are now choosing treatment abroad, because the prices for cancer treatment abroad correspond to and outstrip the quality and effectiveness of treatment.
Diagnostics
In the peripheral blood of most patients, anemia of the normochromic, less often hyperchromic type is detected. Anemia deepens with the progression of the disease to 20 g/l, and the number of red blood cells is noted below 1.0 g/l. Anemia is often the first manifestation of leukemia. The number of reticulocytes is also reduced. The number of leukocytes is usually increased, but does not reach such high numbers as in chronic leukemia. The number of leukocytes varies widely from 0.5 to 50-300 g/l.
Forms of acute leukemia with high leukocytosis have a less favorable prognosis. There are forms of leukemia that are characterized by leukopenia from the very beginning. Total blastic hyperplasia occurs only in the terminal stage of the disease.
All forms of acute leukemia are characterized by a decrease in platelet count to 15-30 g/l. Particularly pronounced thrombocytopenia is observed in the terminal stage.
The leukocyte formula contains blast cells up to 90% of all cells and a small amount of mature elements. The release of blast cells into the peripheral blood is the main morphological sign of acute leukemia.
To differentiate forms of leukemia, in addition to morphological characteristics, cytochemical studies (lipid content, peroxidase activity, glycogen content, acid phosphatase activity, nonspecific esterase activity, etc.), bone marrow biopsy, and blood smears are used.
Main causes of death in leukemia
1. Severe anemia. In most cases, chronic leukemia develops profound anemia, which can cause death.
2. Hemorrhagic syndrome . Many forms of leukemia cause thrombocytopenia, causing severe bleeding or hemorrhage (such as gastrointestinal bleeding or cerebral hemorrhage) even if a blood vessel is slightly damaged. Hemorrhagic complications of leukemia are also facilitated by the appearance of the above-mentioned extramedullary foci of hematopoiesis in the wall of blood vessels, as a result of which they become especially fragile and are easily subject to through rupture.
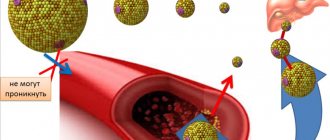
3. Secondary infections . With leukemia, the number of leukocytes in the peripheral blood can reach very high levels. However, most of these cells do not mature into their final forms. Such immature cells are unable to perform their protective function, which manifests itself in the form of a sharply increased susceptibility of the body to any infections.
4. Thromboembolic complications . In some forms of leukemia, accompanied by thrombocythemia, polycythemia, etc., the hematocrit and the number of platelets per unit volume of blood increase significantly, which, against the background of even minor changes in the wall of arterial vessels, leads to the appearance of blood clots, their separation and transfer with the blood flow to various organs.
5. Cachexia . In the later stages of leukemia development, cachexia often develops, i.e. extreme exhaustion. However, as such, it quite rarely becomes the direct cause of death, since more often patients die earlier from the causes indicated in the previous paragraphs.
Forms of leukemia
Acute promyelocytic leukemia is characterized by extreme malignancy of the process, rapid increase in severe intoxication, severe hemorrhagic syndrome, leading to hemorrhage in the brain and death of the patient.
Tumor cells with coarse granularity in the cytoplasm make it difficult to determine nuclear structures. Positive cytochemical signs: peroxidase activity, a lot of lipids and glycogen, the reaction to acid phosphatase is sharply positive, the presence of glycosaminoglycan.
Hemorrhagic syndrome depends on severe hypofibrinogenemia and excessive thromboplastin content in leukemic cells. The release of thromboplastin provokes intravascular coagulation.
Acute myeloblastic leukemia is characterized by a progressive course, severe intoxication and fever, early clinical and hematological decompensation of the process in the form of severe anemia, moderate intensity of hemorrhagic manifestations, and partial ulcerative-necrotic lesions of the mucous membranes and skin.
Myeloblasts predominate in the peripheral blood and bone marrow. A cytochemical study reveals peroxidase activity, increased lipid content, and low nonspecific esterase activity.
Acute lymphomonoblastic leukemia is a subvariant of acute myeloblastic leukemia. According to the clinical picture, they are almost identical, but the myelomonoblastic form is more malignant, with more severe intoxication, profound anemia, thrombocytopenia, more severe hemorrhagic syndrome, frequent necrosis of the mucous membranes and skin, hyperplasia of the gums and tonsils. Blast cells are detected in the blood - large, irregularly shaped, with a young nucleus resembling the shape of a monocyte nucleus. A cytochemical study reveals a positive reaction to peroxidase, glycogen and lipids in the cells. A characteristic feature is a positive reaction to nonspecific esterase in cells and lysozyme in serum and urine.
The average life expectancy of patients is half that of myeloblastic leukemia. The cause of death is usually infectious complications.
Acute monoblastic leukemia is a rare form of leukemia. The clinical picture resembles acute myeloblastic leukemia and is characterized by an anemic tendency to hemorrhages, enlarged lymph nodes, enlarged liver, and necrotizing ulcerative stomatitis. In peripheral blood - anemia, thrombocytopenia, lymphomonocytic profile, increased leukocytosis. Young blast cells appear. A cytochemical study reveals a weakly positive reaction to lipids and high activity of nonspecific esterase in the cells. Treatment rarely causes clinical and hematological remissions. The patient's life expectancy is about 8-9 months.
Acute lymphoblastic leukemia is more common in children and young people. Characterized by an enlargement of any group of lymph nodes, the spleen. The patients' health does not suffer, intoxication is moderate, anemia is insignificant. Hemorrhagic syndrome is often absent. Patients complain of bone pain. Acute lymphoblastic leukemia is distinguished by the frequency of neurological manifestations (neuroleukemia).
In the peripheral blood and in the punctate lymphoblast, there are young large cells with a rounded nucleus. Cytochemical examination: the reaction to peroxidase is always negative, there are no lipids, glycogen is in the form of large granules.
A distinctive feature of lymphoblastic acute leukemia is a positive response to the therapy used. The remission rate is from 50% to 90%. Remission is achieved by using a complex of cytostatic agents. Relapse of the disease can manifest itself as neuroleukemia, infiltration of nerve roots, bone marrow tissue. Each subsequent relapse has a worse prognosis and is more malignant than the previous one. In adults, the disease is more severe than in children.
Erythromyelosis is characterized by the fact that the pathological transformation of hematopoiesis affects both the white and red sprouts of the bone marrow. In the bone marrow, young undifferentiated cells of the white row and blast anaplastic cells of the red line are found - erythro- and normoblasts in large numbers. Large red cells have an ugly appearance.
In the peripheral blood - persistent anemia, anisocytosis of erythrocytes (macrocytes, megalocytes), poikilocytosis, polychromasia and hyperchromia. Erythro- and normoblasts in peripheral blood - up to 200-350 per 100 leukocytes. Leukopenia is often observed, but there may be a moderate increase in leukocytes up to 20-30 g/l. As the disease progresses, blast forms-monoblasts appear. There is no lymphadenopathy; the liver and spleen may be enlarged or remain normal. The disease lasts longer than the myeloblastic form, in some cases there is a subacute course of erythromyelosis (up to two years without treatment).
Epidemiology, pathogenesis and etiology of acute leukemia
Michael Figel
Per. from English N.D. Firsova
Epidemiology and morbidity
Acute myeloid (AML) and acute lymphocytic leukemia (ALL) are rare diseases that account for approximately 1.3% and 0.4% of all new cancer cases in the United States. Although the overall incidence of leukemia has been stable since 1975 (13 new cases per 100,000 population in 1975 and 14 new cases per 100,000 in 2012), over the past decade, estimates of new cases of AML and ALL show an average increase of 2.2% and 0.6% respectively.
International and American statistics
The annual number of new cases per 100,000 population is 1.7 for ALL, and 4.0 for AML in the US, similar rates are observed in other industrialized countries such as Germany with 5.2 new cases of AML and 1.6 ALL in 2010 year and the UK with 4.5 cases of AML and 1.0 ALL. In other words, the incidence in these three countries is about 35,000 new cases per year. 5-year survival is estimated at 25.9% for AML and 67.5% for ALL, and these diseases are responsible for at least 12,000 deaths in 2020 in the US alone.
Age, gender and ethnic differences
Both forms of acute leukemia are associated with age, but in different ways. While ALL peaks in childhood, AML is more common in older adults. Accordingly, the median age at diagnosis for AML is 67 years and 14 years for ALL.
AML affects men more (4.8 new cases in men versus 3.3 in women), while there is no significant gender difference in ALL (1.9 new cases in men versus 1.5 in women). Caucasians have the highest incidence of AML, while people descended from Native North Americans have the lowest incidence. In the case of ALL, the incidence is highest in people of Hispanic origin, and the lowest in people of color.
Biology and pathogenesis of acute leukemia
Both myeloid and lymphocytic acute leukemia arise from genetic lesions in hematopoietic progenitor cells. The lineage of the progenitor in which the damage occurs determines the type of leukemia (lymphoid or myeloid), the least safe are the specific lineage-specific progenitor cells that are damaged. These transformed cells are called leukemia-initiating cells (LICs), but they do not necessarily contain hematopoietic stem cells.
VCIs represent a small minority of the overall population of leukemic cells; both types have the capacity for self-renewal and slight differentiation. They can be identified by functional characteristics (i.e., repopulation potential in mice) and phenotyping of cell surface markers (e.g., CD34, CD38, and human leukocyte antigen-DR [HLA-DR]).
The leukemic mass, while forming the majority of the tumor burden, does not have stem cell properties and therefore does not have the ability to transform or cause relapse in mice. However, this mass is responsible for the symptoms of the diseases: excessive growth of bone marrow with depletion of healthy progenitors and subsequent hematopoietic failure with (pan-)cytopenia and occasional hyperleukocytosis in the peripheral blood, leading to organ ischemia due to "white clots" including leukemic blasts, followed by organ failure.
Etiology of acute leukemia
Although the genetic abnormalities in hematopoietic stem cells that lead to malignant transformation are not fully understood, several risk factors for the development of acute leukemia have been identified. However, most patients with acute leukemia do not meet any of these conditions.
Exposure to ionizing radiation
Ionizing radiation can lead to mutations, deletions, or translocations of DNA by inducing double-strand breaks in hematopoietic stem cells in a dose-dependent manner. The leukosogenic effect of ionizing radiation has long been recognized, mainly due to the increased incidence of both AML and ALL in atomic bomb survivors and radiologists exposed to high doses of radiation. Similarly, radiation used in cancer treatment may be responsible for the development of acute leukemia.
Benzene exposure
Exposure to benzenes is known to increase the risk of developing AML and MDS (myelodysplastic syndrome) over several decades. There appears to be a dose-response relationship, with lower benzene levels increasing the risk of MDS but not AML; a threshold has been determined that can be considered safe. There is also an association with the development of ALL, and in many countries acute leukemia following exposure to benzene during work is recognized as an occupational disease.
Lifestyle
Not only exposure to chemicals, but also lifestyle can affect the development of AML and ALL. Although the pathophysiological mechanisms are unknown, excess weight and smoking have been shown to increase the risk of developing acute leukemia. There is no clear evidence for the role of alcohol consumption in the development of AML and ALL in adults, but parental alcohol consumption is known to increase the risk of childhood leukemia.
Genetic conditions
There are several genetic disorders with predominantly systemic manifestations associated with the development of acute leukemia, for example, Down syndrome and Li Fraumeni syndrome. In addition, inherited bone marrow dysfunction syndromes, such as Fanconi anemia and Shwachman-Diamond syndrome, predispose individuals to the development of myeloid neoplasia and acute leukemia.
In addition, there are rare forms of familial acute leukemia in which certain genes are affected and families exhibit minor or sometimes non-precursor hematopoietic abnormalities.
Pre-existing blood and bone marrow pathologies: secondary acute myeloid leukemia
Malignant as well as several non-malignant myeloid disorders increase the risk of developing AML, which is called secondary AML (sAML). The best known is AML secondary to MDS; The World Health Organization classification recognizes AML associated with myelodysplasia as a distinct entity.
MDS is a highly diverse group of diseases, and the risk of transformation to AML varies significantly between different subgroups. In general, the risk of MDS can be assessed by morphological subtype (where the forms with increasing number of blasts RAEB-1 (5-9%) and RAEB-2 (10-19%) have the lowest survival), but is more accurately reflected in the revised international prognosis system (IPSS-R), which takes into account cytopenia, blast count and cytogenetics. By analyzing these data, it is possible to estimate the probability of survival and identify groups with a very high risk of transformation to AML (for example, in a group of patients with a very high risk, 25% transform into AML within 0.7 years). Other myeloid neoplasias that pose a risk of transformation to AML include significant thrombocytopenia, polycythemia vera, and primary myelofibrosis.
Some non-cancerous diseases also increase the risk of developing acute leukemia, but the mechanism is unclear. The most common of these are paroxysmal nocturnal hemoglobinuria and severe aplastic anemia. Most patients with these diseases suffer from complications unrelated to acute leukemia, but this may change with the advent of more effective treatments (such as biotherapies), leading to increased survival by reducing non-malignant complications (such as thrombosis), but with unknown effect on the development of vAML.
Autoimmune conditions
Patients with autoimmune diseases (eg, rheumatoid arthritis) who are receiving immunosuppressive drugs are at increased risk of developing MDS or AML. However, because the doses of these immunosuppressants, including chemotherapy (methotrexate and cyclophosphamide), are low, the risk of therapy-related myeloid neoplasia is also low.
Viruses
There is no evidence of viral infection in the pathogenesis of AML. In some subsets of acute lymphocytic leukemia, viral infections have been reported to be associated with pathogenesis, such as adult T-cell leukemia (human T-lymphotropic virus type I lymphoma) and Burkitt's lymphoma (Epstein-Barr virus-associated leukemia), but also immunosuppression (eg, acquired immunodeficiency syndrome) and malaria coinfection.
Sources
*Horton SJ, Huntly BJ. Recent advances in acute myeloid leukemia stem cell biology. Haematologica. 2012; *Arber DA, Brunning RD, LeBeau MM, et al. Acute myeloid leukaemia with recurrent genetic abnormalities. In: World Health Organization Classification of Tumors of Haematopoietic and Lymphoid Tissues. Swerdlow SH, Campo E, Harris NL, et al (eds). Lyon: IARC Press; 2008; *Döhner H, Estey EH, Amadori S, et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood. 2010; *Marcucci G, Maharry K, Radmacher MD, et al. Prognostic significance of, and gene and microRNA expression signatures associated with, CEBPA mutations in cytogenetically normal acute myeloid leukemia with high-risk molecular features: a Cancer and Leukemia Group B Study. J Clin Oncol. 2008; *Devillier R, Gelsi-Boyer V, Brecqueville M, et al. Acute myeloid leukemia with myelodysplasiarelated changes are characterized by a specific molecular pattern with high frequency of ASXL1 mutations. Am J Hematol. 2012; *Miller CA, Wilson RK, Ley TJ. Genomic landscapes and clonality of de novo AML. N Engl J Med. 2013.
Acute lymphoblastic leukemia
This type of disease most often affects children and people at a young age.
The disease is characterized by a rapid increase in the number of blasts - immature cells, precursors of lymphocytes. They accumulate in the lymph nodes and spleen, creating an obstacle to the formation and functioning of normal blood components.
Patients often complain of fatigue and periodic joint pain. Some of them note an increase in cervical, inguinal and axillary lymph nodes. After some time, pronounced manifestations of the disease begin to be observed.
This type of acute leukemia may be suspected if the following symptoms are present:
- Severe form of sore throat.
- Anemia, in which the content of leukocytes in the blood sharply increases, while the content of platelets decreases.
- The spleen enlarges.
- Temperature increases. It may be slightly elevated or constantly high.
- Bleeding gums increase, nosebleeds often occur, and there is a tendency to bruise as a result of minor injuries.
- Damage to the ribs, collarbones and skull bones by infiltration.
This type - acute lymphoblastic leukemia - most often appears in children aged 3-6 years. The symptoms are as follows:
- The spleen and liver enlarge, causing the child’s abdomen to significantly increase in size.
- Lymph nodes enlarge. Enlargement of the thoracic lymph nodes is accompanied by shortness of breath and a painful dry cough.
- With this type of leukemia, children experience pain in the abdomen and legs.
- The child has pale skin and gets tired quickly.
- When infected with ARVI, pronounced manifestations are observed.
- The child often falls and loses balance.
What other types of acute leukemia exist?
Classification
Leukemia is divided into acute and chronic.
Acute leukemias have a common feature: the substrate of the tumor is blast cells. These are either progenitor cells of classes 2 and 3 with an undifferentiated form of blasts, or cells of class 4 - morphologically recognizable blasts that begin separate series of hematopoiesis.
Forms of acute leukemia: lymphoblastic, plasmablastic, myeloblastic, myelomonoblastic, erythromyelosis, promyelocytic, undifferentiated leukemia.
Clinical stages of acute leukemia:
- initial (most often set retrospectively); lethargy, loss of appetite, fatigue, pallor, low-grade fever are detected
- expanded - symptoms are associated with pronounced inhibition of normal hematopoietic germs and proliferative syndrome
- remission - complete - normalization of blood count, in the bone marrow the number of blasts is less than 5%, there are no blast cells in the cerebrospinal fluid - incomplete - blasts no more than 20%
- relapse - the appearance of clinical symptoms and/or hematological changes: aleukemic (bone marrow) - changes only in the bone marrow (blasts more than 5%), leukemic (blasts and in peripheral blood), local (extrabone marrow) - with a normal blood test and bone marrow lesion brain, testicles, liver, lungs.
- terminal - characterizes the incurable stage of tumor progression and the therapeutic possibilities of modern medicine. The immediate causes of death in most cases are sepsis, cerebral hemorrhage, and massive bleeding.
Clinical picture of ALL
consists of a number of syndromes.
Intoxication - lethargy, fatigue, loss of appetite, nausea and vomiting, sweating, fever (due to the release of pyrogens by tumor cells). Hyperthermia in leukemia is temporarily relieved by the use of non-steroidal anti-inflammatory drugs and normalizes with programmatic treatment of leukemia; There is no effect from the empirical use of antibiotics, because there is no focus of infection.
Osteoarticular - ossalgia due to expansion of the hematopoietic area (flat bones), due to osteoporosis, cortical destruction, periosteal layers (tubular bones, vertebrae).
Anemic – as a result of suppression of normal hematopoiesis and bleeding - pallor, weakness, fatigue, systolic murmur at the apex of the heart; blood test shows normochromic anemia.
Hemorrhagic - as a result of secondary thrombocytopenia - petechiae, ecchymosis on the skin and mucous membranes, bleeding from the mucous membranes (microcirculatory type of bleeding).
Syndrome of infectious complications - decreased immunity, frequent illnesses, infection, especially where there is a rich microbial flora - gingivitis, tonsillitis occur more often, a necrotic component is characteristic; severe course of infectious and inflammatory processes.
Hyperplastic - enlargement of the liver, spleen, lymph nodes - they are usually dense, painless (blast cells spread throughout the embryonic foci of hematopoiesis). Lymph nodes are more often enlarged in all groups, isolated appearance of conglomerates is possible, more often in the neck area. Leukemic infiltrates can also affect other organs (heart, kidneys, lungs). Leukemides on the skin in ALL in children are rare.
Neuroleukemia is especially distinguished - the presence of leukemic infiltration in the membranes of the brain and spinal cord, in the nerve trunks, ganglia of the autonomic nervous system. Neuroleukemia is a consequence of metastasis of blast cells in the initial stage of the disease. Metastasis can occur in two ways: contact (from the bones of the skull and spine to the dura mater and dural funnels of the cranial and spinal nerves) and more likely diapedetic (from the vessels of the soft shell into the cerebrospinal fluid and into the substance of the brain). The meningeal form is manifested by headaches, nausea, vomiting, hyperesthesia of the skin, and positive meningeal symptoms. Encephalitic—impaired consciousness, convulsions, focal symptoms of brain damage. When using encephalitic, the symptoms of the two previous forms are combined. Signs of diencephalic syndrome may include hyperthermia, drowsiness, bulimia, and polydipsia. Less commonly, in children, damage to the nervous system occurs in the form of myelitis, epiduritis, plexitis, and polyradiculoneuritis. Lumbar puncture findings for neuroleukemia include increased cerebrospinal fluid pressure, increased protein content, pleocytosis, decreased glucose levels, the presence of blast cells, a positive Pandi reaction. Changes in the cerebrospinal fluid can be detected in the absence of a clinical picture of central nervous system damage.
Syndromes
All clinical manifestations of leukemia are divided into 4 groups of syndromes:
- Hyperplastic syndromes. Characteristic signs of hyperplastic syndromes are enlarged and painful lymph nodes, enlarged spleen and liver, the appearance of pain and aching in the joints, the appearance of reddish-bluish plaques on the skin, damage to the oral mucosa, tonsils, the development of necrotic stomatitis, and gum hyperplasia. The syndromes are caused by leukemic infiltration of the spleen, liver, joint capsule and periosteum, as well as a tumor increase in bone marrow volume.
- Hemorrhagic syndromes. Manifested by the occurrence of bleeding and hemorrhages (gingival, nasal, internal). Unreasonable bruises often appear; even a minor injury can cause almost unstoppable bleeding; wounds take a long time to heal. The syndromes are caused by a blood clotting disorder due to platelet damage.
- Anemic syndromes. There is weight loss, increased heart rate, hair loss, general malaise, pale skin, memory loss and loss of concentration. The syndromes are caused by a decrease in hemoglobin levels, as there are not enough red blood cells in the blood.
- Immunodeficiency and intoxication syndromes. They manifest themselves in the form of weakness, fever, excessive sweating, headache, nausea and vomiting, lack of appetite, significant loss of body weight, and the development of various infectious and inflammatory processes that are very severe.
Each type of leukemia has its own specific symptoms. They also differ in the course of the pathology.
So, what are the main types of leukemia?