General information
Vascular occlusion is a blockage (more often of arteries than veins), which is characterized by a pronounced decrease in the speed and quality of blood flow. Occlusion can cause necrosis and, as a result, lead to death.
The pathology is quite common and can affect the organs of visual perception, the central nervous system, limbs and great vessels. sepsis and peritonitis develop . Abdominal ischemic syndrome develops against the background of a lack of adequate blood circulation in the digestive tract. The pathology is associated with occlusion of the unpaired visceral branches of the abdominal aorta - the celiac trunk and mesenteric arteries (superior, inferior). Abdominal toad can develop under the influence of both internal ( thrombosis ) and external factors (traumatic occlusion).
What is an occlusive dressing?
This method of sealing the lesion is used for wounds that require maintaining sterile conditions and protection from the external environment.
Applying an occlusive dressing to the knee joint requires certain skills and technique:
- cover the wound surface with sterile gauze;
- Place the top of the scarf on the thigh area and wrap it around the waist;
- bend the bandage at the base by 2 cm;
- cross the ends under the thigh, tie knots on the thigh;
- Throw the top over the knot formed and then pass it under the knot.
Treatment methods
Vascular obstruction is treated with medications. The first stage of the disease is treated conservatively with medications.
The second stage of the disease and subsequent ones are treated with surgery.
Conservative
Before treating blockages in the legs, the patient is examined and the diagnosis is confirmed. Then treatment is prescribed. At the onset of the disease, therapy is conservative and can be done at home. The patient is prescribed various groups of medications:
- Anticoagulants that reduce blood viscosity: Aspirin;
- Cardiomagnyl.
- Spasmol;
- Actylase;
- Ketanol;
- Digoxin;
Important information: How to treat obliterating endarteritis of the vessels of the lower extremities (legs)
They use drugs that improve heart contractions, such as Novocainamide. For local therapy, Heparin ointment is used. Patients are recommended vitamin complexes and physiotherapeutic treatment. Electrophoresis promotes rapid penetration of medicinal substances to the affected area. Patients are prescribed magnetic therapy, which relieves pain, normalizes blood circulation, and improves oxygen supply to the blood.
Operation
Patients at the second stage of the disease are prescribed surgery:
- stenting;
- bypass;
- thrombus excision;
- prosthetics.
The operation is intended to restore blood circulation. During bypass surgery, a shunt is placed to the affected area of the vessel and blood flow is restored. Thrombectomy is used to remove a blood clot from an artery. At stage 3 of the disease, patients are prescribed necrectomy, that is, amputation of necrotic tissue, as well as fasciotamia, when pressure on the muscle is reduced by cutting the fascia.
At stage 4 of the disease, more radical treatment is carried out. If the patient develops gangrene, the leg is amputated.
If amputation is not carried out, blood poisoning can lead to the death of the patient. At the initial symptoms of circulatory disorders in the legs, you should consult a doctor. An advanced disease carries many complications, including death.
ethnoscience
At the recovery stage, after consultation with a doctor, you can use traditional recipes. Patients drink decoctions of medicinal herbs and take baths.
For internal use, you can use the following recipe: take hawthorn and rose hips, 1 tbsp. l., add 1 tsp. crushed lingonberry and immortelle leaves. Pour the mixture into a thermos and pour boiling water over it. Leave for 3 hours. Drink throughout the day. Tea cleanses blood vessels from cholesterol plaques.
Patients are prescribed a decoction of valerian root internally and as compresses. You can prepare a collection from the fruits of hawthorn, strawberries, and rowan. 2 tablespoons of berries are poured into 400 g of boiling water. Brew for half an hour. Drink during the day in 4 doses.
Important information: How is blood erythremia and symptoms of Vaquez disease treated?
You can prepare an infusion of chestnut, fennel, adonis and lemon balm flowers. 1 tbsp. l. the mixture of herbs is brewed with a glass of boiling water. The medicine is drunk per day. The course of treatment is a week, after which they take a break and repeat the course again.
Walnuts, nettle leaves and garlic are used for treatment:
- A bath of nettle leaves will improve blood circulation. 4 tbsp. l. nettles pour 1 liter of boiling water. Add the infusion to the bath. The procedure takes 20 minutes.
- Take garlic infusion. You need to chop 50 g of garlic, pour a glass of vodka, leave for 2 weeks in a dark place. 10 drops of infusion are diluted in 100 g of boiled water, drunk 3 times a day.
- For the tincture, place 1 kg of peeled walnuts in a 3-liter bottle. Pour liquid honey and cover with cellophane. Fermentation occurs. The jar is closed with an iron lid and placed in the cold for 3 months. Then drain the liquid and add 30 g of bee pollen. For a month you should consume 1 tsp daily. this remedy. Then they take a break for 2 weeks and repeat the course.
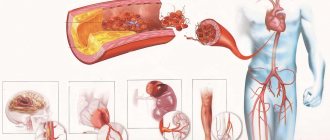
Pathogenesis
When the blood thickens, there is an accumulation of fibrin in its composition, which leads to thrombus formation . Venous formations are characterized by constancy - they are located in one area and clog the vessels of the extremities, leading to necrosis and gangrene . Arterial formations are characterized by migration; they often break away from the original source and disrupt the blood supply to large organs, provoking the development of stroke , heart attack and other dangerous conditions.
The concept of occlusion (blockage) of blood vessels in the legs
Impaired blood flow due to vascular occlusion
Blockage of the arteries of the lower extremities leads to a cessation of oxygen and nutrients to the organs and tissues they supply. The popliteal and femoral arteries are most often affected The disease develops abruptly and unexpectedly.
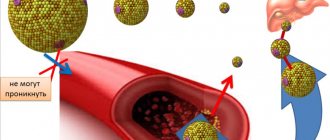
The lumen of the vessel can be blocked by thrombi or emboli of various origins. The diameter of the artery, which becomes impassable, depends on their size.
In this case, tissue necrosis quickly develops in the area below the blockage of the artery.
The severity of the signs of pathology depends on the location of the occlusion and the functioning of the lateral - collateral blood flow through healthy vessels running parallel to the affected ones. They deliver nutrients and oxygen to ischemic tissues.
Blockage of the arteries is often complicated by gangrene, stroke, or heart attack, which lead the patient to disability or death.
It is impossible to understand what leg vascular occlusion is, to understand the severity of this disease, without knowing its etiology, clinical manifestations, and treatment methods. We must also take into account the importance of preventing this pathology.
More than 90 % of cases of blocked arteries in the legs have two main causes:
- Thromboembolism - blood clots form in the main vessels, are delivered by the blood flow to the arteries of the lower extremities and block them.
- Thrombosis - a blood clot as a result of atherosclerosis appears in the artery, grows and closes its lumen.
Etiology
The etiology of the remaining cases is as follows:
- accumulation of cholesterol plaques on the walls of blood vessels during atherosclerosis until it becomes blocked;
- embolism with particles of fat or foreign body, air bubbles, injection fluid;
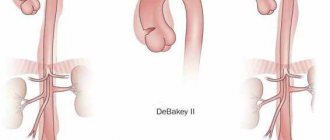
- arterial aneurysm - their stretching and protrusion, in which blood clots and emboli quickly accumulate;
- mechanical trauma to blood vessels, compression, blocking blood flow;
- inflammatory diseases of the arteries, which are accompanied by swelling and accumulation of exudate;
- cardiac ischemia, hypertension, heart disease, myocardial infarction, diabetes mellitus contribute to the development of occlusion;
- leukemia - the lumen of the artery is blocked by growing malignant cells.
Risk factors
Vascular occlusion is a disease for the development of which the presence of risk factors . Minimizing them reduces the possibility of obstruction. They are:
- alcoholism, drug addiction, smoking;
- heredity;
- surgery on the blood vessels of the legs;
- unbalanced diet;
- pregnancy, childbirth;
- excess weight;
- sedentary lifestyle;
- gender - men are more often affected, age - more than 50 years.
The effects of underlying causes and risk factors often take a long time to accumulate.
Important! Experts note the spread of leg vascular occlusion among young people, many of whom sit in front of computers and gadget monitors. Therefore, when the first signs of occlusion occur, regardless of age category, you must immediately consult a doctor.
Classification, types of occlusion
It is customary to distinguish between arterial and venous occlusion.
Types of occlusion by localization:
- Occlusion of mesenteric vessels . It is characterized by an acute circulatory disorder in the mesenteric vessels, which inevitably leads to intestinal ischemia. As a result of thrombosis, the trophism (nutrition) of the intestinal walls is disrupted, and an acute inflammatory process develops, including peritonitis .
- Occlusion of cerebral vessels. The gradual growth of cholesterol plaques in volume can lead to complete blockage of the vessels supplying blood to the brain. The vessels lose their elasticity and a blood clot forms at the site of attachment of the cholesterol plaque as a result of platelets adhering to the damaged vascular wall.
- Occlusion of the arteries of the lower extremities. In this case, a sharp closure of the lumen of the peripheral artery and the development of an acute form of ischemic syndrome are characteristic. Such changes lead to disruption of trophism and nutrition of the lower extremities, paralysis and even gangrene . With occlusion of the femoral artery, extensive circulatory disorders develop not only in the lower extremities, but also in the pelvic organs, which can pose a real threat to the life and health of the patient. Both the superficial (SFA) and deep femoral artery can be affected.
- Occlusion of cardiac vessels. Damage to the coronary arteries is very common. When the supply vessel is completely blocked, irreversible consequences develop in the form of necrosis - myocardial infarction . ischemia develops , which manifests itself as signs of angina pectoris . The blockage can occur due to a blood clot or atherosclerotic plaque. With long-term, chronic occlusion, bypass pathways are formed - collaterals, through which nutrients are supplied. In 98% of cases, the coronary arteries are affected by atherosclerosis .
- Occlusion of the subclavian artery. As a result of blockage, ischemia occurs not only in the upper extremities, but also in the brain. Dizziness , weakness in the arms, problems with speech and visual perception appear The consequences of occlusion of the subclavian arteries are severe.
- Occlusion of the carotid artery. There is both complete and partial blockage of the vessels that supply blood to the brain. Occlusion of the internal carotid artery, which nourishes and supplies the brain and is responsible for intracranial circulation, is rare. Damage to the common carotid artery can lead to problems with visual perception.
- Occlusion of the iliac artery. The first manifestation of the lesion is numbness in the legs, fatigue, ischemia of the legs, and the appearance of pain when walking. Gradually, damage manifests itself in the functioning of the pelvic organs, impotence , and the functioning of the abdominal organs is disrupted.
- Occlusion of the eye or occlusion of the retinal artery. It is extremely rare. It is characterized by a completely asymptomatic course and a sudden deterioration in vision up to complete blindness.
Occlusion in dentistry
In dentistry, occlusion is closure, i.e. the most complete and dense contact of the chewing surfaces with each other. In simple words, dental occlusion is the relationship of the jaws relative to each other.
The occlusal surface of the tooth is that part of the tooth surface that is located from the deepest part of the central fissure to the top of the cusps.
6 keys of occlusion according to Andrews
Andrews is credited with formulating his own theory based on crown morphology and evaluating 120 models with “ideal” occlusion in orthodontically untreated patients. He developed rules (keys) for the relationship of a single tooth to both the adjacent and the antagonist tooth, taking into account its position.
- Key 1 – ratio of painters;
- Key 2 – mesiodistal type (crown angulation);
- Key 3 – torque and inclination of tooth crowns;
- Key 4 – rotation;
- Key 5 – contact point;
- Key 6 – Spee curve.
Central occlusion
The definition includes other names:
- intertubercular contact;
- maximum closure of teeth;
- intertubercular contact position;
- intercuspation.
Central occlusion determines the position of the lower jaw, which is characterized by:
- uniform, symmetrical contraction of the muscles that raise the lower jaw;
- the central position of the heads of the temporomandibular joint in the articular fossae;
- maximum fissure-tubercle contacts of the dental rows.
Dental signs of central occlusion:
- Between the teeth of the lower and upper jaws there is the most dense tubercle-fissure contact.
- Each tooth intersects with two antagonists. The only exceptions are the lower central incisors and upper third incisors.
- The midlines between the central lower and upper incisors are located in the same sagittal plane.
- The lower teeth overlap the upper teeth by no more than a third of the length of the crown in the frontal region.
- The cutting edge of the lower incisors contacts the palatal cusps of the upper incisors.
- The upper first molar occludes the 2 lower molars, covering two-thirds of the first molar and one-third of the second.
- The buccal cusps of the lower teeth overlap the buccal cusps of the upper teeth in the transverse direction.
You can learn more about occlusion in dentistry in the book “Functional Occlusion” by Peter Dawson.
Types and signs of the disease
Occlusion of the lower extremities can occur in any area of the legs, and the lumen of large and small vessels is blocked.
There are such types of disease:
- Obstruction of large arteries, which interferes with blood flow in the femoral areas.
- Blockage of the small arteries that supply blood to the feet and legs.
- Mixed blockage of both small and large vessels.
Depending on what factors caused the development of the disease, the following types are distinguished:
- Arterial. A blood clot appears in large arteries or on the valves of the heart, and is then carried by the movement of blood to the lower systems of the body.
- Air. The lumen of the vessel closes the air, which can occur as a result of lung injury.
- Fat. After a bone fracture, a piece of fat blocks the vessel.
Arterial obstruction can be acute or chronic:
- Acute occlusion develops when a vessel is blocked by a thrombus and has a rapid course.
- Chronic occlusion develops slowly, its symptoms depend on the formation of cholesterol plaques on the walls of the arteries and the gradual decrease in the lumen of the vessel.
Important information: How to treat periarteritis nodosa in women and its symptoms
The initial symptom of the pathology is lameness. Walking quickly causes pain, so the patient, sparing his leg, begins to limp. After rest the pain goes away. But gradually the disease progresses, pain occurs more and more often.
The patient develops the following symptoms:
- Constant pain that gets worse with light exertion.
- The skin on the affected area turns pale and cold, then turns bluish.
- There is no pulsation of the arteries at the site of blockage.
- Sensitivity decreases and numbness occurs in the legs.
- Leg paralysis develops.
After blockage of a vessel, tissue necrosis occurs in a few hours at the site of occlusion, and gangrene may appear. This is an irreversible process that can lead to amputation of the limb. Therefore, if a person has symptoms of occlusion, he should urgently consult a doctor.
Causes
Most often, occlusion develops as a result of embolism, blockage of a blood vessel by a dense formation. This process can develop as a result of:
- Infectious disease . In this case, the blood flow is blocked by inflammatory-purulent blood clots or the accumulation of a large number of pathogenic microorganisms.
- Air embolism . It develops as a result of an air bubble entering the systemic bloodstream. It is determined after traumatic damage to a vessel or after an incorrectly performed injection.
- Fat embolism . As a result of metabolic , fat particles accumulate and a fat clot forms from them.
- Arterial embolism . Thrombi form on the valve apparatus of the heart and are characterized by instability and mobility, which can lead to separation of thrombotic masses and blockage.
Occlusion of the vessels of the neck and coronary arteries is formed in the area of their branching or narrowing.
Causes of thrombosis:
- malignant neoplasms;
- atherosclerosis;
- traumatic injuries;
- aneurysms;
- thromboembolism.
As a result of traumatic damage to muscle tissue and the skeletal system, compression occurs and blood flow is blocked.
Possible complications
Embolism, if treatment was started too late, causes complications. Most of them are serious diseases that lead to the death of the patient.
- Internal hemorrhage.
- Benign brain tumor.
- Disturbances in the functioning of the circulatory system.
- Disorders of the cardiac system.
But the most life-threatening complication of embolism is respiratory arrest; if you do not provide first aid to a person, he will die.
Prediction of the disease depends on what stage of development the disease was diagnosed at and when treatment began. There are no exact static data, but it is known that when an embolism affects a person outside the hospital, in most cases he dies. The reason is the fact that people do not immediately seek advice from a medical specialist.
If cerebral artery embolism was diagnosed in the early stages of development, the chances of a complete recovery of the patient are high. In rare cases, the patient suffers from concomitant pathologies for some time; over time, the body recovers and all residual effects disappear.
Symptoms
Against the background of damage to the brachiocephalic vessels, there is a decrease in performance, weakness and dizziness . The brachiocephalic trunk is responsible for the blood supply to the soft tissues of the head and the brain. If the left artery is additionally involved in the pathological process, then the clinical picture worsens significantly. Main manifestations:
- pale skin;
- nausea;
- headache;
- pain during physical activity;
- confusion;
- paraplegia;
- swelling and development of necrosis;
- burning sensation or numbness;
- deterioration of visual perception;
- hallucinations;
- difficulty breathing, swallowing;
- speech disorders;
- cardiopalmus;
- absence of pulse in the affected area.
If any of the above symptoms appear, it is necessary to conduct a thorough analysis and diagnosis to identify the true cause and subsequently prevent the development of severe complications.
Symptoms
Cerebral artery embolism results in one of two scenarios. The most unfavorable of these is ischemic stroke, which without treatment leads to the death of the patient. Another possible option is the chronic nature of the disease.
In this case, the person suffers from the clinical manifestations of the pathology for several tens of months. Over time, chronic patients get used to the symptoms of vascular embolism and stop paying attention to them.
Medical specialists divide a scenario with a chronic nature of the pathology into three stages.
- Initially, the walls of blood vessels lose their elasticity, which is accompanied by severe painful sensations, in this case, migraines. The patient becomes irritable, concentration deteriorates, and the person gets tired faster. The overall performance of the brain decreases.
- If treatment is not started at the first stage, the disease progresses. The clinical manifestations of the pathology intensify, in addition to headaches, constant tinnitus or insomnia occurs. General brain activity suffers even more, disturbances in the functioning of the motor system, and possible false urges to “go to the toilet” occur. Sometimes patients complain of decreased sensitivity in the limbs and problems with the visual system.
- When treatment was not started even at the second stage, the symptoms worsen even more. The patient may have difficulty moving, and it is difficult for him to control his body. Brain performance is severely affected. Involuntary urination is possible at any time. At stage 3, the patient must be under the supervision of medical specialists, this is explained by the fact that a person practically cannot control himself at this stage of the development of the disease. If there is no treatment at this stage, this will lead to immobilization of the person.
Tests and diagnostics
It is recommended to consult a doctor at the first manifestations of the disease. After examination, collecting anamnesis and assessing the manifestations of clinical symptoms, they begin diagnostics, which includes:
- CT arteriography;
- Doppler ultrasound;
- cerebral angiography;
- MR angiography;
- coagulogram;
- MRI of the brain.
Only after a comprehensive examination is appropriate treatment prescribed, which is selected individually for each patient.
What to do if you suspect
If there is serious concern that the patient has an embolism, the first thing to do is to lay him down, placing a pillow under his head and shoulders, and prohibit him from moving. If this is not done, the patient may experience an ischemic stroke.
After conducting the necessary diagnostic tests and making a diagnosis, the doctor prescribes treatment. At the same time, he necessarily takes into account the individual characteristics of the patient, concomitant diseases, and age.
However, as you know, any disease is easier to prevent than to treat. This also applies to blockage of blood vessels in the brain, which does not occur just like that, but is a consequence of pathologies already existing in the body.
The simplest preventive measures are giving up bad habits, promoting a healthy lifestyle, proper nutrition and reasonable physical activity. And, of course, we must not forget about systematic medical examinations, which will help to timely identify diseases such as cerebral embolism.
Diet for occlusion
To restore the elasticity of the vascular wall, strengthen it and reduce the severity of occlusion, it is recommended to adhere to certain dietary rules. In case of occlusion, it is recommended to adhere to a special cholesterol-lowering diet, which includes:
- Legumes . Beans and legumes are sources of protein, iron, folic acid and contain absolutely no fatty acids.
- Whole grains (wheat bread, buckwheat, oatmeal and brown rice).
- Cabbage (all types, especially broccoli). Prevents salt deposition, normalizes the lipid spectrum of cholesterol, enriches the body with vitamins K and C.
- Asparagus . Helps lower blood pressure and reduce cholesterol in the blood.
- Persimmon . Rich in fiber and has a pronounced antioxidant effect.
- Spinach . Allows you to reduce blood pressure in hypertensive patients.
- Turmeric . It has an anti-atherosclerotic effect, reduces the volume of cholesterol plaques, and reduces the severity of the inflammatory process.
Prevention
Following simple prevention rules significantly reduces the risk of developing the disease:
- Lead an active lifestyle, use moderate physical activity.
- Visit skating rinks, swimming pools, gyms.
- Quit smoking and alcohol or reduce the consumption of strong drinks to a minimum.
- Eat the right foods that contain enough vitamins and microelements. Avoid foods that increase blood cholesterol, blood viscosity, blood pressure, and those containing large amounts of fat.
- Avoid significant weight gain and maintain normal weight.
- Avoid stress, learn to get rid of it.
- Monitor the course and treatment of chronic diseases that can cause obstruction of the blood vessels of the legs.
List of sources
- Matyushenko A.A. “Pulmonary embolism as a general medical problem”, article in the journal RMZh No. 13 dated 07/03/1999
- Atayan A.A., Kosenkov A.N., Kuznetsov M.R., Chernookov A.I., Ivanova M.I., Khachatryan E.O. “Hybrid tactics in the treatment of acute disorders of mesenteric circulation”, RMZh No. 8(II) dated 10.25.2019
- Yavelov I.S. “The use of anticoagulants during thrombolytic therapy in patients with signs of acute occlusion of the coronary artery: how to individualize treatment?”, RMZh No. 26 of November 30, 2011
Diagnostics
During the examination of the patient, a preliminary diagnosis is made, and additional studies are urgently prescribed:
- general and biochemical blood test;
- duplex scanning;
- computer arteriography;
- abdominal radiography;
- selective mesentericography - it is used to determine the area in which occlusion of the mesenteric vessels is observed;
- magnetic resonance angiography.
Occlusion of the mesenteric artery on the diagram and angiogram
After a comprehensive study and confirmation of the diagnosis, treatment is prescribed. If the patient's condition is severe, immediate surgery is performed.
Separately about the concept of occlusion in dentistry
"Occlusion" is a broad term. In dentistry, for example, it refers to any contact between the teeth of the upper and lower jaw. Thus, central occlusion (the arrangement of teeth with the maximum number of interdental contacts, in which the line passing between the incisors of the upper and lower jaw coincides with the conditional middle of the face) is practically the same as the concept of occlusion. That is, a bite is considered to be one or another relationship of teeth, determined in central occlusion.
In dentistry, there are many types of occlusion. Thus, very common cases of malocclusion, for example, caused by underdevelopment of the lower jaw or, conversely, by its excessive development, are distal occlusion. You have probably observed such a bite: the upper front teeth cover the lower row of teeth.
But we will move on, finding out what occlusion is in general medicine.
Symptoms of carotid artery occlusion
The clinical picture of carotid artery obstruction depends on the location of the lesion, the rate of development of occlusion (suddenly or gradually) and the degree of development of vascular collaterals that provide alternative blood supply to the same areas of the brain. With the gradual development of occlusion, a restructuring of the blood supply occurs due to collateral vessels and some adaptation of brain cells to the current conditions (reduced supply of nutrients and oxygen); A clinic of chronic cerebral ischemia is being formed. The bilateral nature of the obstruction has a more severe course and a less favorable prognosis. Sudden occlusion of the carotid arteries usually leads to ischemic stroke.
In most cases, occlusion of the carotid arteries manifests itself as a transient ischemic attack (TIA), a transient disorder of cerebral circulation, the duration of which primarily depends on the degree of development of vascular collaterals in the affected area of the brain. The most typical symptoms of TIA in the carotid system are mono- or hemiparesis and sensory disturbances on the opposite side (heterolateral) in combination with monocular visual impairment on the affected side (homolateral). Typically, the onset of an attack is the occurrence of numbness or paresthesia of half the face and fingers, the development of muscle weakness in the entire arm or only in its distal parts. Visual disturbances range from the sensation of spots in front of the eyes to a significant decrease in visual acuity. In some cases, retinal infarction is possible, triggering the development of optic nerve atrophy. More rare manifestations of TIA with obstruction of the carotid arteries include: dysarthria, aphasia, facial paresis, headache. Some patients report dizziness, lightheadedness, swallowing problems, and visual hallucinations. In 3% of cases, local convulsions or major seizures are observed.
According to various data, the risk of ischemic stroke within 1 year after the onset of TIA ranges from 12 to 25%. In approximately 1/3 of patients with carotid artery occlusion, a stroke occurs after one or more TIAs, and in 1/3 it develops without previous TIAs. Another 1/3 are patients in whom ischemic stroke is not observed, but TIAs continue to occur. The clinical picture of ischemic stroke is similar to the symptoms of TIA, but it has a permanent course, i.e., the neurological deficit (paresis, hypoesthesia, visual disturbances) does not go away over time and can only decrease as a result of timely adequate treatment.
In some cases, manifestations of occlusion do not have an abrupt onset and are so unexpressed that it is very difficult to assume the vascular origin of the problems that have arisen. The patient’s condition is often interpreted as a clinical picture of a cerebral tumor or dementia. Some authors indicate that irritability, depression, confusion, hypersomnia, emotional lability and dementia can develop as a result of occlusion or microembolism of the ICA on the dominant side or on both sides.
Obstruction of the common carotid artery occurs in only 1% of cases. If it develops against the background of normal patency of the ECA and ICA, then the collateral blood flow going through the ECA to the ICA is sufficient to avoid ischemic brain damage. However, as a rule, atherosclerotic changes in the carotid arteries are multi-level, which leads to the symptoms of occlusion described above.
The bilateral type of occlusion of the carotid arteries with well-developed collaterals may have an asymptomatic course. But more often it leads to bilateral strokes of the cerebral hemispheres, manifested by spastic tetraplegia and coma.
Diagnostic methods
The initial diagnosis is made after collecting anamnesis and examining the patient. To clarify the diagnosis and the affected area, instrumental and laboratory diagnostic methods are used:
- Blood test for coagulation with assessment of prothrombin index and fibrinogen content.
- Ultrasound with duplex scanning allows you to identify the area of blood supply disturbances and assess the condition of the vessel walls.
- Angiography, MRI and CT are prescribed to obtain the most accurate picture of the pathology.
Advanced occlusion of the vessels of the lower extremities has serious consequences for the body, including amputation of the legs, so any suspicion of the disease requires a thorough examination in a hospital:
- The surgeon visually assesses the site of the suspected blockage, noting the presence of swelling, dryness and other skin lesions.
- Vascular scanning helps to identify injured segments.
- If the picture is unclear, an x-ray or angiography is ordered, in which contrast dye is injected into the artery.
- The ankle-brachial index helps assess the condition of the circulatory system.
Methods for diagnosing occlusions of various arteries include examinations by medical specialists. It is necessary to clarify the neurological pathology and identify the focality of symptoms. Cardiologists examine the heart in more detail. To diagnose central retinal artery occlusion, a detailed examination of the fundus is necessary.
In the study of the vessels of the head and extremities, the following are of great importance:
- rheoencephalography;
- ultrasonography;
- Doppler color study of blood flow;
- angiography with the introduction of contrast agents.
To establish the connection between brain symptoms and damage to the adductor arteries and subsequent treatment, it is important to know:
- which of the extracerebral vessels is damaged (carotid, subclavian or vertebral arteries);
- how severe is the stenosis;
- the size of the embolus or atherosclerotic plaque.
To do this, the duplex study technique uses the calculated occlusion coefficient. It is determined by the ratio of the diameter at the site of narrowing to the undamaged area.
Occlusion is assessed in five degrees depending on the speed of blood flow relative to normal (less than 125 cm/sec.). Subocclusion is considered a pronounced narrowing of the lumen (more than 90%), this stage precedes complete obstruction.
Treatment
Occlusion is most often treated with surgical intervention: the ducts are cleared, the affected areas are removed, and arterial bypass is performed.
The type of treatment will depend on the stage of the disease:
- Grade 1-A tension ischemia is the initial stage of the pathological process, conservative treatment is used, thrombolytics are administered, barotherapy, and magnetic therapy are performed;
- ischemia grade 1B–2B - a surgical intervention is performed that is aimed at restoring blood flow using bypass surgery, thrombectomy or embolectomy, and if tension occlusion is determined, then prosthetics of a section of the artery is performed;
- ischemia grades 3A–3B – bypass surgery is used, partial amputation of the limb is allowed;
- in case of 3D ischemia, surgical interventions on blood vessels are contraindicated, as they lead to post-ischemic syndrome, which can provoke the death of the patient, but amputation is mandatory.
After eliminating the cause of occlusion, medications may be prescribed:
- relieving inflammation;
- painkillers;
- antispasmodics;
- agents that improve blood flow and heart function;
- blood thinners.
At the same time, physiotherapy is prescribed:
- massages;
- physiotherapy;
- baths.
The patient is prescribed a diet to lose weight (if necessary) and prevent the formation of fat clots. In case of amputation of a limb, rehabilitation measures are prescribed, which include psychological training, and a prosthesis is selected.