Impaired blood supply to the heart due to atherosclerotic changes in the coronary vessels is called coronary disease. This concept combines angina pectoris, myocardial infarction, cardiosclerosis, arrhythmia, cardiac failure, and sudden coronary death. All these pathologies can be prevented, but only by influencing modifiable risk factors for the development of myocardial ischemia.
Knowing the main reasons for the development of the disease, groups of people are identified who should undergo cardiac examinations more often and make lifestyle changes.
Main risk factors for coronary heart disease
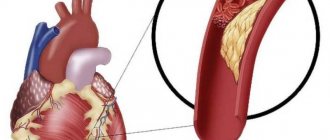
The basis of coronary heart disease is the formation of cholesterol deposits inside the vessel. This leads to filling of their lumen and obstruction of blood flow. Due to a lack of nutrients, tissues experience acute or chronic hypoxia, and degenerative processes develop with the replacement of functioning cells by connective tissue.
Vessels of large and medium diameter are most often affected. The most severe consequences are with damage to the cerebral and coronary arteries.
The division of risk factors into subgroups underlies preventive measures that can reduce the risk of pathologies such as stroke and myocardial infarction. In ischemic disease, the causes of its development coincide with the ethology of atherosclerosis and are divided into:
- removable (modifiable);
- irreducible (biological determinants);
- partially removable.
All of these factors are important to prevent coronary artery disease; if several of them are present, the risk increases exponentially.
We recommend reading about the treatment of angina pectoris. You will learn about the diagnosis of heart failure, drug treatment, changes in the patient’s life after hospitalization, and prognosis. And here is more information about how to take Nitroglycerin for angina pectoris.
Causes
Atherosclerosis
It is believed that IHD begins with damage to the inner layer of the coronary arteries, sometimes from childhood. Damage can be caused by various factors such as:
- smoking;
- arterial hypertension (high blood pressure);
- high cholesterol;
- diabetes;
- radiation therapy to the chest (used for some types of tumors);
Once the artery wall is damaged, fatty deposits, consisting of cholesterol and cellular breakdown products, begin to accumulate in the vessel. This process is called atherosclerosis. When these plaques begin to disintegrate and crack, platelets from the bloodstream try to close the defect, forming a blood clot. The resulting blood clot can block a coronary artery, which in turn can lead to a heart attack.
Modifiable risk factors for coronary artery disease
Half of all diseases are caused by an unhealthy lifestyle, and for the cardiology group this figure is even higher. Therefore, removable risk factors for coronary artery disease are the most promising category; their elimination significantly reduces the incidence of damage to the heart and blood vessels.
There are reasons that do not directly depend on the person (genetics, ecology, age, level of medicine), but after eliminating bad habits, you can transfer the disease to a milder form and avoid complications.
Eating habits
The basis for the violation of fat metabolism in the body is the consumption of foods that contain large amounts of cholesterol and other saturated fats. These are primarily animal products:
- fatty varieties of lamb, pork, beef;
- offal (brains, liver, kidneys, lung, heart);
- sausage, frankfurters and sausages;
- eggs;
- butter, heavy cream;
- canned fish in oil, mackerel, carp;
- semi-finished meat products, ready-made minced meat.
Their consumption leads to the accumulation of cholesterol in liver cells. This reduces the formation of special receptors that capture fats from the blood. Therefore, atherogenic lipids remain in the vascular bed and are fixed on the walls of the arteries. Reducing the proportion of fatty meat in the diet helps slow down the blockage of the lumen of the vessel, and, consequently, increase the length and quality of life.
In addition, you need to include in your daily menu foods that help remove excess saturated fatty acids from the body and prevent fatty liver degeneration. These include dietary fiber contained in vegetables and fruits, bran and cereals, as well as unsaturated fats from vegetable oils, fish, and seafood. The healthiest combination is boiled fish with herbs and a salad of fresh vegetables with vegetable oil.
Smoking
The condition of blood vessels and the blood coagulation system is negatively affected not only by nicotine, but also by a huge number of chemical compounds from tobacco smoke. Their action is manifested in this way:
- stimulation of adrenaline receptors;
- increased need of myocardial cells for oxygen;
- increased excitability of the heart muscle;
- rhythm disturbance and risk of muscle fiber fibrillation;
- decreased transport and absorption of oxygen due to the combination of hemoglobin with low concentration of high-density lipoproteins in the blood;
- high risk of blood clots.
Quitting smoking or reducing the number of cigarettes smoked helps normalize blood flow and nutrition of the tissues of the heart, brain, limbs, and restores lung and kidney tissue.
Stress
The release of adrenal hormones into the blood when exposed to a psycho-emotional stimulus is most dangerous for people whose reaction belongs to behavioral type A. It is also called coronary, since the risk of atherosclerosis and heart attack in such individuals increases even at a young age. Main features:
- desire to compete and dominate;
- intolerance to other people's opinions;
- cruelty, aggressiveness, outbursts of anger;
- constant rush, lack of time.
Neutralizing such character traits often requires the help of a psychologist, mastering relaxation techniques, and allocating sufficient time in the daily routine for rest.
Alcohol
Although there is evidence of the benefits of moderate consumption of alcoholic beverages for the condition of blood vessels, they cannot be recommended for the prevention of atherosclerosis due to
for such an effect on the body:
- increased blood pressure;
- risk of cardiac arrhythmia and sudden cardiac arrest;
- addiction with the need to increase the dose.
The maximum dose of ethanol is 30 g per day no more than 2 times a week. This amount is contained in a glass of wine or 70 g of spirits. It should be borne in mind that alcohol has a stronger effect on women, so you need to control the amount of alcohol taken even more carefully.
Lack of movement
The incidence of myocardial ischemia with low levels of physical activity is two times higher than in those who lead an active lifestyle. The optimal activities for the prevention of coronary artery disease should be:
- frequency per week – 4 or 5 times;
- regular, without long breaks;
- duration 30 minutes (5-10 minutes are allocated for warm-up and final recovery);
- heart rate 50 - 70% of maximum (220 minus age);
- in case of heart disease, the activity level is determined after exercise tests during an ECG.
The degree of exposure to all types of risk factors
If we talk about the listed risk factors for coronary heart disease, then coronary heart disease, which develops as a result of a significant deterioration in the condition of blood vessels and disruption of the circulatory process, is most often diagnosed in the presence of such indicators as being male, age over 55 years, the presence of bad habits and unhealthy Lifestyle. It is these parameters that significantly influence the likelihood of developing a given lesion of the cardiac system.
Being male
According to medical statistics, men most often suffer from various lesions of the cardiovascular system, and coronary disease occupies one of the leading places.
It is in men, especially upon reaching a certain age, that various functional disorders are observed that can affect the functioning of the myocardium and impair blood circulation. The adherence of the male half of the population to such bad habits as smoking in significant quantities and excessive consumption of alcoholic beverages (for comparison, women drink strong alcohol three times less often than men) also weakens the heart muscle to a greater extent, making it more susceptible to negative changes.
Women under the age of 35-40 years are less susceptible to the effects of disturbances in myocardial function; however, upon reaching 65-70 years of age, the likelihood of developing IHD becomes approximately equal in men and women.
Age category
Today, coronary disease is being reported at younger and younger ages. But patients over 55 years of age and women over 65 years of age are more susceptible to pathological changes.
Heredity factor
If among your immediate family there are those who have been identified as having a tendency or presence of heart disease, the risk of developing ischemia increases significantly.
If you add bad habits, an unhealthy and sedentary lifestyle to the existing genetic factors, you can “get” coronary heart disease in a short time.
Disturbances in the process of fat metabolism
Changes in the speed and quality of fat metabolism, which is expressed in an increase in the volume of formation of low-density lipoproteins, which transport cholesterol molecules to the walls of blood vessels. This process can cause a rapid increase in cholesterol plaque, which interferes with the normal movement of blood through the vessels.
In a normal state, there is a balance in the body between low-density and high-density lipoproteins, which are antagonists of the former and prevent cholesterol from settling on the walls of blood vessels. At the onset of atherosclerotic processes, the amount of high-density lipoproteins decreases in comparison with low-density lipoproteins.
Presence of arterial hypertension
With excessively elevated blood pressure, there is a significant increase in the risk of diagnosing and developing coronary heart disease. A high systolic pressure (as well as diastolic) increases the risk of ischemia by 2-7 times.
Hypertension is characterized by the gradual development of left ventricular hypertrophy, which can also provoke the occurrence and further aggravation of coronary artery disease.
Disorders in carbohydrate metabolism
Any disturbances in metabolism immediately affect the functioning of the heart muscle. Diabetes mellitus, which is a pronounced disorder or malfunction of carbohydrate metabolism, most often becomes the cause of neuropathic lesions, accompanied by the manifestation of the first signs of ischemia.
The presence of risk factors such as diabetes mellitus and atherosclerosis, especially advanced degrees, become the cause of death from myocardial infarction in 25-30% of cases. The painless course of a heart attack causes death in 75% of cases of this condition.
Bad habits
Among the bad habits that significantly affect the condition of the myocardium and the functioning of the entire cardiovascular system, smoking should be considered first. Its negative influence can quickly and permanently damage the heart. 14% - this is how much the risk of formation and development of coronary heart disease increases when smoking.
Manifestations that can worsen the functioning of the heart and cause disturbances in its circulation include the following:
- increase in blood clotting rate;
- a decrease in the amount of high-density lipoproteins released, which leads to a faster process of cholesterol deposition on the walls of blood vessels;
- the negative effect of carbon monoxide on the condition of the myocardium is manifested in a change in the number of heart contractions, a change in the supply of blood to the myocardial tissue, as a result of which oxygen starvation occurs in this area.
There is also significant stimulation of the adrenal glands, which increase the dose of adrenaline and norepinephrine entering the blood. This manifestation, in turn, increases the risk of developing hypertension.
With frequent smoking, severe spasm of blood vessels occurs, which provokes the rapid formation of cholesterol plaques on their walls. Cholesterol plaques cause a deterioration in the process of blood movement, significant oxygen starvation of heart tissue, which can also be considered the initial stage of coronary heart disease.
The listed risk factors for the development of coronary artery disease, with their single manifestation, negatively affect the condition of both the heart muscle and blood vessels. With any combination of them, the degree of exposure increases significantly, which also becomes a risk factor. Knowledge of these factors will allow everyone to control their own health, identify even minor negative changes in well-being and prevent the risk of worsening the process.
Non-modifiable provocateurs of ischemic heart disease
It is impossible to influence factors that are related to the biological characteristics of the body by changing behavior or drug intervention. These include gender, age and heredity.
Persons who are included in the most dangerous risk groups for developing coronary diseases should take into account that it is necessary to exclude all modifiable causes of IHD from their lives and undergo regular examination and preventive treatment.
Floor
The ratio of men and women who develop coronary disease before the age of 40 is 10:1. Then this difference gradually decreases, and by age 70 the risk becomes equal. This disproportion is associated with the protective properties of female sex hormones. In the absence of smoking, hormonal imbalance and obesity, menstruating women rarely suffer from angina.
After the onset of menopause, the level of high-density lipoproteins in the blood increases, and atherosclerotic changes progress.
Therefore, women over 50 years of age are recommended to undergo examination at least once a year, even in the absence of complaints about heart function, and to take estrogen replacement therapy.
In men, atherosclerosis is much more pronounced; for them, an important protective mechanism can be changing their diet, increasing activity and giving up harmful addictions.
Even in the absence of other risk factors, changes in the properties of the vascular wall and the ratio of lipids in the blood occur with age. This is caused by a decrease in the level of metabolic processes, damage to the inner layer of arteries by free radicals accumulated throughout life, and insufficient formation of hormones.
At the same time, a connection was found between the risk of complications of atherosclerosis and getting rid of bad habits. The likelihood of myocardial infarction in people over 55 with a healthy lifestyle is almost 10 times lower.
Heredity
At high risk are those people whose parents developed coronary artery disease before the age of 57. A predisposition to disorders of fat and carbohydrate metabolism, increased blood pressure, as well as behavioral characteristics is inherited. In addition, there are family traditions - large feasts, overeating, fatty and sweet foods, drinking alcohol, smoking, and low physical activity.
Therefore, obesity and hypercholesterolemia are often not genetic problems, but acquired due to improper eating behavior.
Lifestyle modification
- To give up smoking . Complete cessation of smoking, including passive smoking. The overall risk of mortality for those who quit smoking is halved within two years. After 5–15 years, it levels out with the risk of those who have never smoked. If you cannot cope with this task on your own, contact a specialist for advice and help.
- Physical activity . All patients with coronary artery disease are recommended to engage in daily physical activity at a moderate pace, such as walking for at least 30 minutes a day, home activities such as cleaning, gardening, and walking from home to work. If possible, endurance training is recommended 2 times a week. Patients at high risk (for example, after a heart attack or with heart failure) need to develop an individual physical rehabilitation program. It must be adhered to throughout your life, periodically changing on the recommendation of a specialist.
Partially modifiable risk factors for coronary heart disease
Pathological conditions that contribute to the development and progression of atherosclerosis include:
- Dyslipidemia – high levels of cholesterol, saturated fats, decreased levels of high-density lipoproteins.
- Hypertension – high blood pressure leads to myocardial hypertrophy, which impairs coronary blood flow.
- Diabetes mellitus – insulin deficiency causes an increase in glucose and cholesterol levels in the blood.
- Blood coagulation disorders - increased fibrinogen and platelet aggregation rate accelerate thrombus formation.
- Obesity is the most dangerous abdominal obesity, as it is combined with impaired insulin sensitivity, increased blood pressure and cholesterol levels in the blood.
- Infections – the development of atherosclerosis was noted after suffering from herpes, chlamydia, cytomegalovirus disease, as well as in the presence of persistent foci of infection (tonsillitis, periodontitis).
We recommend reading about post-infarction cardiosclerosis. You will learn about the causes and symptoms of the disease, classification, complications, diagnosis and treatment. Read more about the complications of myocardial infarction here.
Symptoms
Narrowed coronary arteries are unable to deliver enough oxygen-rich blood to the heart—especially during times of increased heart rate, such as during exercise. At first, reduced blood flow to the heart may not cause symptoms of coronary artery disease. However, as plaque continues to grow in your coronary arteries, you may experience symptoms such as:
Chest pain (angina pectoris).
You may feel a tightness in your chest, as if someone is standing on your chest. Pain is considered angina if it is caused by physical or emotional stress. It usually disappears within a few minutes after the causative factor disappears. For some people, especially women, the pain may be fleeting or sharp and localized to the abdomen, back, or arm.
Dyspnea.
If the heart is unable to pump enough blood to meet the body's needs, shortness of breath and extreme fatigue from exertion may develop.
Heart attack (myocardial infarction).
A heart attack can occur when a coronary artery is completely blocked. Classic symptoms of myocardial infarction include chest compression, pain radiating to the arm, shortness of breath, and profuse sweating. Women tend to experience less typical symptoms such as nausea, back pain and jaw pain. In some cases, myocardial infarction is not accompanied by any symptoms.
If you suspect a heart attack, call an ambulance immediately or have someone take you to the nearest hospital.
If you are at risk for coronary artery disease due to high blood pressure, high cholesterol, diabetes or excess weight, contact your doctor. You may be referred for testing, especially if you have symptoms of narrowing of the coronary arteries. Even if you don't have coronary heart disease, your doctor may recommend treatment for risk factors. Early diagnosis and treatment can stop the progression of CAD and prevent myocardial infarction.
Prevention of coronary heart disease
To prevent impaired blood supply to the myocardium, it is necessary to review the diet, ensure a sufficient level of physical activity, taking into account age, fitness and the presence of diseases, give up nicotine and minimize alcohol consumption.
If there is a hereditary predisposition, and especially for older men, these recommendations will help avoid serious complications such as stroke and heart attack. If there are concomitant disorders of fat or carbohydrate metabolism, then drug therapy is used to restore normal levels of glucose and cholesterol in the blood.
Daily monitoring of blood pressure, losing excess weight, and taking blood thinners helps to significantly reduce the risk of vascular accidents and maintain activity.
Coronary heart disease is associated with a decrease in myocardial nutrition with difficulty in blood flow through the coronary vessels. The main reason is atherosclerosis. Its development can be influenced by eliminating modifiable risk factors. This task is especially relevant in the presence of biological determinants (male sex, old age, family history) or diabetes, obesity, hypertension, coagulopathy.
Diet for IHD
Diet . The goal is to optimize nutrition. It is necessary to reduce the amount of solid animal fats, cholesterol, and simple sugars. Reduce sodium (table salt) intake. Reduce the total caloric intake of the diet, especially if you are overweight. To achieve these goals, you must adhere to the following rules:
- Eliminate or limit as much as possible the consumption of any animal fat: lard, butter, fatty meat.
- Limit (or better yet completely eliminate) fried foods.
- Limit eggs to 2 per week or less.
- Reduce table salt consumption to 5 grams per day (salt in a plate), and in patients with hypertension to 3 or less grams per day.
- Limit confectionery products, pastries, cakes, etc. as much as possible.
- Increase your consumption of grains, as minimally processed as possible.
- Increase the amount of fresh vegetables and fruits.
- Eat sea fish at least three times a week instead of meat.
- Include omega-3 fatty acids (ocean fish, fish oil) in your diet.
This diet has a high protective effect for blood vessels and prevents further development of atherosclerosis.
Weight loss . The goals of the weight loss program for coronary artery disease are to achieve a body mass index in the range of 18.5 - 24.9 kg/m2 and an abdominal circumference of less than 100 cm in men and less than 90 cm in women. To achieve these indicators, it is recommended to increase physical activity, reduce calorie intake, and, if necessary, develop an individual weight loss program and stick to it. At the first stage, it is necessary to reduce the weight by at least 10% of the original and maintain it.
In case of severe obesity, it is necessary to consult a specialist nutritionist and endocrinologist.
Reduce alcohol consumption. According to the latest WHO recommendations, the amount of alcohol consumed should not exceed one bottle of dry wine per week.
Complications
Coronary heart disease can lead to:
Substernal pain.
When the coronary arteries narrow, the heart experiences a lack of blood flow, and during times of increased demand - such as during physical activity - this can cause chest pain or shortness of breath.
Myocardial infarction.
An atherosclerotic plaque, when destroyed, stimulates thrombus formation in the coronary artery, which can lead to its complete blockage, which can cause myocardial infarction. Lack of blood flow to the heart can damage the heart muscle. The volume of damage will directly depend on the speed of medical care.
Heart failure.
If parts of the heart are chronically deficient in oxygen and nutrients due to reduced blood flow, or if the heart muscle has suffered a myocardial infarction, the heart may become unable to pump enough blood to meet the body's needs. This condition is known as heart failure.
Pathological heart rhythm (arrhythmia).
Inadequate blood supply or damage to heart tissue can affect the heart's electrical impulses, causing abnormal rhythms.
Monitoring key indicators
Arterial pressure. If it is within normal limits, you need to check it twice a year. If your blood pressure is elevated, you should take measures as recommended by your doctor. Very often, long-term use of blood pressure-lowering medications is required. The target blood pressure level is less than 140/90 mmHg in people without underlying medical conditions, and less than 130/90 in people with diabetes or kidney disease.
Cholesterol levels. An annual screening should include a blood test for cholesterol. If it is elevated, it is necessary to begin treatment on the recommendation of a doctor.
Blood sugar. It is necessary to monitor blood sugar levels especially carefully if you have diabetes or are prone to it; in such cases, constant supervision by an endocrinologist is necessary.
Diagnostic methods
If coronary heart disease is suspected, the patient should consult a cardiologist. The specialist will conduct a survey to find out about the presence of other pathologies, disturbing symptoms, heredity and other factors. Then he will examine the patient. Having identified signs characteristic of IHD (edema, arrhythmia, heart murmurs, cyanosis), the doctor will prescribe the following examination methods:
- Donating blood to assess the concentration of enzymes, whose increase is observed during angina pectoris and heart attack (myoglabin, troponin, aminotrosferase, creatine phosphokinase). Their high level is detected during the death of cardiomyocytes (heart cells). No less important for accurate differentiation of the disease is a blood test for cholesterol, glucose, AST, lipoproteins and ALT.
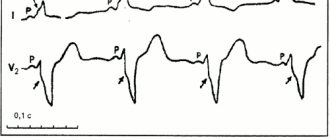
- Electrocardiography (ECG) is considered the primary and most important method for studying coronary artery disease. It allows you to record changes in electrical activity and identify malfunctions in the myocardium.
- A stress ECG is prescribed to determine the presence of the disease in the early stages, when it manifests itself only due to physical activity. The patient will be asked to exercise on special exercise equipment (treadmill, exercise bike) and the results will be recorded. The diagnostic method is contraindicated if it is not possible to perform the actions required by the doctor. Excessive physical activity can aggravate the condition, leading to complications.
- The transesophageal form of ECG is used for a detailed study of the conduction system and electrical activity of the myocardium due to the location of the device so close to the heart. During the procedure, a sensor is inserted into the esophagus and the necessary indicators are recorded. Unlike other examination methods, this form of ECG avoids distortions caused by the skin, chest and other tissues.
- Daily ECG monitoring allows you to study the work of the heart in various situations. Data recording occurs for 24 hours thanks to a portable device. It's called a Holter monitor. The pictures on its screen will allow the doctor to differentiate ischemia among other pathological processes. Decryption occurs using a computer. A clear advantage of the method is the accuracy of the data and the ability to find out the conditions of occurrence and causative factors of attacks, which is extremely important for drawing up a correct treatment regimen.
- Ultrasound examination (ultrasound) of the heart muscle is performed to study the cavities and valves, assess the size and degree of contractility, and listen to acoustic noise.
- Coronography is prescribed to the patient to study the patency and assess the integrity of the heart vessels. The procedure is carried out by injecting a contrast agent and further identifying changes using x-rays. This examination method is usually used to decide on surgical intervention on the coronary vessels. People who are prone to allergic reactions should be careful, as they can also occur to the contrast agent.
The data obtained will be sufficient to assess the performance of the heart and differentiate coronary artery disease from other pathologies. Focusing on the cause and form of the disease, a treatment regimen is drawn up, which is based on lifestyle correction and the use of medications.
Clinical picture
The first signs of cardiac ischemia depend on its form. Attacks of the disease have a wave-like course, that is, the patient’s well-being is constantly changing under the influence of various factors. Approximately 30% of patients do not feel any discomfort at all. They are characterized by an imperceptible progression of a painless type of pathology. Minor manifestations may occur only after decades. This nuance depends on the course of the disease. Among the common symptoms of IHD, the most common are:
- pain in the heart area that occurs due to stress and overload;
- dyspnea;
- feeling of heartbeat;
- tachycardia (increased contraction frequency);
- general weakness;
- cyanosis (blue skin);
- decreased mental abilities;
- loss of consciousness;
- nausea;
- excessive sweating;
- dizziness.
Pain in the chest area can radiate to the jaw, arm and back. If cardiac ischemia has led to the development of heart failure, then the patient experiences swelling of the legs and constant shortness of breath, forcing him to sit down for a short time.
Ischemia of the heart muscle manifests itself differently in each case. This nuance depends on the form of the pathology. The following symptoms are considered harbingers of the most dangerous type of coronary heart disease (coronary death):
- sharp and frequent attacks of chest pain;
- uncontrollable fear of death;
- spontaneous mood changes;
- loss of consciousness;
- absence of pulse in large arteries;
- respiratory arrest;
- change in skin tone;
- absence of heart muscle sounds;
- pupil dilation.
Important! More than half of people with CAD die due to cardiac arrest.
Death often occurs in the prehospital stage.