© Author: Andrey Alekseevich Illarionov, therapist, bacteriologist, especially for SosudInfo.ru (about the authors)
Rheumatic heart disease (RHD) is an inflammatory infectious-allergic lesion of the connective tissue of the heart and blood vessels. This pathology is a complication of fever of rheumatic origin and is characterized by the proliferation of fibrous tissue on the valve flaps. Once formed, a heart defect is incurable and extremely dangerous to health. Over time, it becomes a cause of disability for patients. That is why it is necessary to consult a doctor in a timely manner.
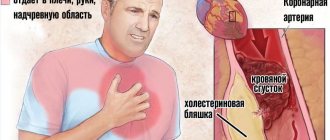
The causative agent of the infection is beta-hemolytic streptococcus, which initially causes an acute fever accompanied by tonsillitis and pharyngitis. Subsequently, the valves and frame of the heart are involved in the pathological process. Patients develop rheumatic carditis, which is complicated by acquired heart disease. Most often, the valves located in the left parts of the organ are affected. They stop opening and closing normally, disrupting the proper flow of blood.
Rheumatic heart disease develops as a result of repeated attacks of acute fever. Streptococcal infection is the cause of myocardial inflammation. The autoimmune reaction leads to scarring of the heart muscle. The acute form of the pathology occurs as pancarditis with damage to all its structures. Chronic inflammation affects the valves. When the connective tissue grows and affects their valves, stenosis or valve insufficiency occurs.
Patients with rheumatic heart disease complain of general weakness, fatigue, shortness of breath, swelling of the legs, palpitations, cardiac arrhythmias, and cardialgia. Symptoms, diagnostic measures and prognostic conclusions of RHD are in many ways similar to rheumatic fever. At the same time, in patients, signs of intoxication and other extracardiac manifestations are much less pronounced, the pathological process is more severe, and fatal complications more often develop. Clinical, laboratory and immunological parameters in RHD return to normal very slowly.
RHD is a dangerous disease that, if left untreated, leads to severe complications: heart failure, pulmonary embolism, thrombosis, arrhythmias, bacterial endocarditis, and death. Without specific therapy, the condition of the damaged valve gradually worsens. To stop further progression of the rheumatic process, it is necessary to undergo treatment. First, specialists prescribe conservative therapy to patients, including various groups of drugs. In severe cases, surgical intervention is resorted to. In case of severe hemodynamic disturbances, cardiac surgery is extremely necessary.
Currently, RHD is very rare. The pathology has an ICD-10 code from I05 to I09, depending on the type of affected valve. The prognosis of the disease with the right approach to patient management is relatively favorable. After timely and adequate therapy, patients feel satisfactory.
Pathogenesis (mechanism of development)
The appearance of rheumatic carditis is preceded by repeated streptococcal diseases, which lead to a change in the immune response to the introduction of infection. As a result, antibodies are produced that are aimed at destroying both bacteria and one’s own internal organs. The body's defenses recognize the connective tissue of the heart as foreign and attack its own cells - an autoimmune conflict develops. The synovium of large joints also undergoes this process.
The mechanism of heart damage is associated with the formation of CICs (circulating immune complexes), which consist of bacteria and antibodies. When the immune system malfunctions, CECs attach to the tissues of the heart, destroy cells here and cause aseptic inflammation, caused not by streptococci, but by their toxins and antibodies.
For the development of an autoimmune process, a genetic predisposition is necessary. In people sensitive to hemolytic streptococcus, the connective tissue contains proteins similar in structure to bacterial ones. As a result, the immune system synthesizes antibodies to destroy the infection, and, in fact, destroys the heart. This leads to the replacement of normal cells with rough connective tissue (fibrosis), shrinkage of the valves and the formation of defects.
Causes
Two main factors play a role in the development of rheumatism of the heart: streptococcal infections and impaired immune function due to genetic characteristics. The combination of these reasons leads to heart damage. If there is only one factor, the disease does not develop. Therefore, not all people suffer from rheumatic carditis, even with frequent streptococcal infections.
The state of the body's defenses affects the risk of disease. According to statistics, rheumatism more often occurs in children living in unfavorable living and social conditions, which leads to a decrease in immunity. The disease is also diagnosed in older people suffering from severe chronic diseases.
Unfavorable factors provoking the development of rheumatism of the heart:
- immunodeficiencies (critical decrease in the body's defenses);
- regular hypothermia and overheating;
- colds and acute respiratory viral infections (influenza, parainfluenza);
- prolonged course of infections;
- poor nutrition (deficiency of minerals and vitamins);
- living in damp and cold rooms;
- long-term stay in closed institutions (orphanages, boarding schools, dormitories);
- heredity.
The disease is more common in female patients, which is due to the peculiarities of the hormonal system. Genes that determine the structure of heart tissue are inherited, which increases the risk of developing rheumatic heart disease in members of the same family.
Causes of pathology
The heart becomes inflamed because its tissues are attacked by immune cells.
Scientists have found that the risk of rheumatism increases with:
- Genetic predisposition.
- Infection with certain microorganisms: group A hemolytic streptococcus (the causative agent of scarlet fever and tonsillitis), herpesvirus, hepatitis B, T-lymphotropic virus, cytomegalovirus, measles and mumps viruses.
- Chronic diseases of the nasopharynx: pharyngitis, tonsillitis.
The risk of rheumatism increases with chronic pharyngitis.
Click on the photo to enlarge The same reasons can lead to rheumatic damage to other organs (joints, blood vessels, lungs, skin, nervous system).
If you are at risk (for example, your direct relatives suffered from rheumatism), the disease may appear after a stressful situation for the body: severe hypothermia, sun or heatstroke, intense emotional experience, poisoning with toxic substances, sudden hormonal disruption.
The disease affects people of any age. Most often - children from 5 to 15 years old and adults over 50 years old. In children, rheumatic carditis usually occurs in an acute form as a complication of tonsillitis or scarlet fever, especially if treatment is untimely or incomplete. In adults, rheumatic heart disease can occur in a chronic form. The “trigger” for the onset of rheumatism development is usually age-related changes in the body, including hormonal disorders, as well as chronic infections.
Rheumatic carditis begins to appear 7–21 days after a streptococcal infection (angina or scarlet fever). Therefore, even after recovery, it is advisable to observe a doctor (pediatrician or therapist) for some time, and also undergo a preventive examination by a cardiologist.
Classification
In ICD-10, rheumatic carditis is assigned code 105-109, where 105 is rheumatic diseases of the mitral (bicuspid), 106 - aortic, 107 - tricuspid (tricuspid) valve, 108 - combined defect, 109 - other heart lesions. The classification allows us to systematize all rheumatic changes in the body, determine diagnostic and therapeutic tactics, and predict the outcome of the disease. The characteristics of the course and phase of activity of the inflammatory process are of clinical importance.
Table - Classification of rheumatism
| Name | Characteristic |
| Stages by phase of the rheumatic process | |
| Active (low, medium, high) | Clinical symptoms of the heart and other organs Signs of inflammation in laboratory tests Specific changes during instrumental diagnostics |
| Inactive | Absence of symptoms or blurred clinical signs Normal blood counts When conducting instrumental diagnostics, residual effects (signs of cardiac hemodynamic disturbances, valve defects) |
| Forms of rheumatic carditis according to the characteristics of the course | |
| Acute | Rapid onset, damage to joints and/or heart Vivid clinical manifestations High degree of inflammatory response Duration - 3 months Ends with recovery with adequate therapy |
| Subacute | Slow start Symptoms are mild Joint damage comes to the fore Duration - up to 6 months Difficulties in diagnosis Worsening prognosis if treatment is not started in a timely manner |
| Protracted | Blurred clinical picture Duration - more than 6 months Valve damage is accompanied by minor symptoms The prognosis is poor for severe heart damage |
| Latent (hidden) | There are no characteristic clinical symptoms Diagnosed during a heart examination for other diseases (the acquired defect is discovered retrospectively) |
| Chronic relapsing | Periods of exacerbation are accompanied by a bright clinical picture of the heart, joints, nervous system, and less often the skin Short periods of remission Rapid development of heart defects and severe complications that can lead to death The prognosis is unfavorable |
For children, acute and subacute forms of rheumatic carditis are most typical. Protracted and latent is more common in the elderly and mature people. The recurrent variant of the disease is associated with high activity of the autoimmune process and occurs in weakened patients.
What is rheumatism of the heart?
Rheumatism of the heart (or rheumatic carditis) is usually detected in the young population. The most dangerous age is 7-15 years old (schoolchildren). Moreover, females are at greater risk. Mental stress, rapid growth, hormonal changes, physical activity - all these are prerequisites for rheumatic lesions. To this list we can add a high incidence of acute respiratory infections among students. Many viruses spread easily in group gatherings of people through airborne droplets.
Elderly people are also at risk. Their predisposition to rheumatism can be explained by aging of the body, decreased immunity, the presence of many chronic diseases, as well as the presence in the medical history of cases of rheumatic inflammation in the early period of life.
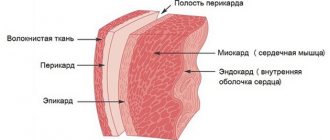
What is it - rheumatism of the heart? This is an inflammatory process that occurs in the connective tissues of the organ with the accompanying formation of specific nodules - potential scars. It can affect both individual layers of the heart wall (endocardium, myocardium, pericardium) and all three membranes simultaneously. The development of rheumatic fever is associated with autoimmune disorders. The disease provokes serious complications, and in its advanced form leads to death.
According to the ICD, the definition of chronic rheumatic heart disease includes pathologies with codes 105-109. Examples of prevalence by nationality:
- In Russia, the incidence of rheumatic carditis at an early age is one case in every five thousand children.
- In England, 2-3 thousand diseases are recorded annually in school-age children.
- The number of American residents decreases by 50 thousand every year due to complications of rheumatic heart disease.
Clinical picture
Rheumatic carditis occurs after a streptococcal infection. Heart damage is usually preceded by articular syndrome, which develops during the first rheumatic attack in 90% of cases. Thanks to this, it is possible to predict the pathology of the cardiovascular system at the stage of joint inflammation and begin comprehensive treatment. Less commonly, cardiac involvement is the only symptom, complicating the diagnosis. In such cases, an infection suffered the day before indicates in favor of rheumatism.
Streptococcal infections
The appearance of rheumatism is preceded by a streptococcal infection: tonsillitis, sinusitis, otitis, pharyngitis, scarlet fever, tonsillitis, caries, erysipelas. The connection between the two diseases has important diagnostic significance. Rheumatism occurs against the background of general well-being after recovery or residual effects of infection. During this period, a high titer of antistreptococcal antibodies (antistreptolysin-O, antistreptohyaluronidase, antistreptokinase) and CEC can be detected in the blood.
Sore throat and tonsillitis are more common. Inflammation of the pharyngeal tonsils occurs with colds, acute respiratory viral infections, and scarlet fever. Sore throat of varying degrees of intensity appears, discomfort when swallowing saliva and food, weakness, drowsiness, fever; pinpoint rash and “crimson tongue” with scarlet fever. Tonsillitis is accompanied by low-grade inflammation of the tonsils and is a chronic source of infection that weakens the body's defenses.
Joint damage due to fever
Rheumatism usually begins with inflammation of large joints: knees, elbows, shoulders, ankles. Clinical signs of joints occur 1-3 weeks after a streptococcal infection. The disease is manifested by a sharp increase in body temperature. Another name for the pathology is rheumatic fever. High temperature is accompanied by chills and sweating, mainly at night. Fever peaks deplete the body, causing loss of appetite and decreased physical activity.
Against the background of high temperature, intense joint pain appears, which has a “volatile” character. During the day, discomfort from one joint can move to another. The pain appears suddenly and ends just as quickly. The skin over the affected joint becomes red, swells, and the local temperature rises. Movements in the joint are difficult or impossible due to inflammatory changes and severe pain.
Symptoms disappear after 5-7 days. Rheumatism of the joints is not characterized by residual effects on the musculoskeletal system. After the acute process subsides, mobility in the joints is retained in full.
Heart symptoms
1-2 weeks after the onset of inflammation in the joints, the rheumatic process affects the heart. Rheumatic carditis is diagnosed in 50% of clinical cases at the first attack of the disease. Valve defects usually develop as a result of a long course of pathology, against the background of refusal of therapy and non-compliance with prophylaxis.
The disease begins with a new peak in temperature, which rises to 38-39 ℃. Weakness, drowsiness, and rapid fatigue appear during normal physical activity. Appetite worsens due to nausea, and sometimes vomiting occurs regardless of food intake. Fever and other symptoms are associated with poisoning of the body with toxic products of inflammation in the joints and internal organs.
Rheumatism affects all layers of the heart: muscular (myocarditis), internal (endocarditis), external serous (pericarditis). In severe cases of the disease, acute or chronic heart failure develops.
Myocarditis
With inflammation of the myocardium, hypertrophy (increase in volume) of the left, less often the right, parts of the heart appears. The contractile function of the muscle layer is impaired and the movement of blood through the heart chambers is impaired. Myocarditis is accompanied by chest pain, difficulty breathing, and an increase in body temperature up to 38 ℃. Significant thickening of the muscle layer leads to the appearance of a “bull’s heart” - on the x-ray, the shadow of the organ is expanded, congestion in the lungs and an enlarged liver are revealed. Characterized by increased heart rate and decreased blood pressure.
Endocarditis
Damage to the inner layer of the heart leads to the formation of blood clots on the mucous membrane and deformation of the valves. Blood clots can reach large sizes, break away from their primary location and clog large blood vessels. The most dangerous is thromboembolism of the branches of the pulmonary artery. Disruption of blood flow through the vessels causes intense burning pain in the chest, shortness of breath, dizziness, and loss of consciousness. If medical care is not provided in a timely manner, death occurs.
Deformation of the valves leads to heart defects. The left parts are most often affected - the mitral and aortic valves. The first is located between the atrium and the ventricle, the second controls the flow of blood into the largest vessel in the body (aorta). In the right parts, the tricuspid valve is deformed.
Rheumatic carditis is characterized by stenosis (narrowing) of the opening between the atrium and the ventricle. As a result of inflammation of the endocardium, the mucous membrane is replaced by rough connective tissue (scarring), which leads to a decrease in the diameter of the hole through which blood moves through the chambers of the heart. Stenosis of the aortic and mitral valves is most often detected.
Less commonly, valve insufficiency occurs, in which the valve flaps fuse together and lose their previous shape and elasticity. This leads to incomplete closure of the hole between the chambers of the heart, as a result of which the blood moves in the opposite direction, which is not typical for normal hemodynamics. Tricuspid valve insufficiency is usually diagnosed.
Heart defects cause decreased resistance to physical exertion, weakness, fatigue, shortness of breath, heaviness in the chest and right hypochondrium due to stagnation of blood in the lungs and liver. The pulse quickens or slows down, and drops in blood pressure occur. When listening to the heart, systolic and diastolic murmurs are determined.
The skin becomes pale or bluish, a dry or productive cough appears, and sometimes streaks of blood appear in the sputum. Characterized by dizziness, nosebleeds, decreased functioning of the immune system, which is manifested by frequent colds and acute respiratory viral infections.
Pericarditis
Inflammation of the serous membrane of the heart occurs less frequently than other layers of the organ. Dry or exudative (with fluid) pericarditis develops. Inflammatory effusion accumulates in the cavity of the serous membrane, which compresses the parts of the heart and disrupts contractile function. Pericarditis is accompanied by chest pain, the sound of pericardial friction in the dry form of the disease, shortness of breath, dry cough, and fever.
Heart failure
Myocarditis and pericarditis can cause acute heart failure; valve defects usually lead to chronic heart failure. Shortness of breath, swelling of the extremities at the end of the day, accumulation of fluid in the abdominal (ascites) and thoracic (hydrothorax) cavities, weakness, and decreased physical activity appear. Hemodynamic disturbances lead to hypoxia (lack of oxygen) in the internal organs. The functioning of the liver, lungs, and digestive tract deteriorates. Acute cardiac and end-stage chronic heart failure are associated with a high risk of death.
Treatment and consequences
If the results of a diagnostic examination confirm rheumatism, treatment should be started immediately to prevent complications. Treatment should be carried out under the strict supervision of a physician.
Treatment
The attending physician develops a treatment regimen that lasts for at least two weeks. In some cases, the course of treatment can last about two months.
If the disease is neglected and left untreated, the pathology becomes chronic. Unfortunately, rheumatic chronic heart defects cannot be cured, so from time to time the patient will have to deal with exacerbations of the pathology.
The most important requirement addressed to patients is strict adherence to bed rest. Any physical activity can provoke valvular heart defects and cause cardiosclerosis.
Initially, therapeutic treatment is carried out, which involves taking medications:
- antibiotics;
- anti-inflammatory steroid and non-steroidal drugs;
- drugs with immunosuppressive effects.
If drug treatment is not accompanied by the desired result, and rheumatism has already provoked valve disease, the doctor can make fundamental changes to the treatment regimen. In such cases, an operation is performed that involves valve repair or installation of a prosthesis.
If a prosthesis has been installed, the patient must be prescribed antiplatelet agents or anticoagulants for preventive purposes. This helps prevent the occurrence of blood clots. After surgery, the patient is recommended to undergo sanatorium treatment.
The attending physician does not reject the use of alternative medicine methods. It is only important that traditional methods are used with the permission of the doctor, and not at the patient’s own request. In some cases, even taking a decoction of medicinal herbs may be incompatible with certain medications.
Taking a decoction of medicinal herbs
If the doctor approves of treatment with folk remedies, then the patient is recommended to take decoctions of willow bark, buckthorn, birch leaves, and acacia branches. It is also useful to take a mixture of chopped dried apricots and raisins with the addition of honey.
So, the final decision on what specific methods to treat the cardiovascular problems is still made by the doctor, who also monitors the patient’s condition and changes the methods if the dynamics are negative.
Possible complications
In the absence of treatment or in cases where the patient shows signs of indiscipline, the first signs of complications of such a pathology may initially appear, such as arrhythmia or tachycardia.
If the treatment continues to be uncontrolled or incorrect, the patient begins to complain of pain in the heart area, and then circulatory failure is provoked, followed by:
- stenosis;
- aortic insufficiency;
- cerebral ischemia;
- renal infarction;
- thromboembolism of the great vessels.
Other forms of rheumatism
Most often, the joints and heart are involved in the inflammatory process, and less often other organs. Rheumatism of the skin and nervous system is distinguished. Damage to the integument of the body appears during the active phase of rheumatic carditis or articular syndrome, the nervous system - after the acute process has subsided against the background of general well-being.
Cutaneous form
The integument of the body is affected in 3% of cases of rheumatism. An annular (ring-shaped erythema) rash and nodules form on the skin. The inflammatory process can involve a large surface of the body and worsen the course of other forms of the disease.
The anular rash is ring-shaped, pale pink in color, passes without peeling and residual hyperpigmentation, and is localized on the trunk and extensor surface of the limbs.
Rheumatic nodules are located in the area of large joints. They are 3-20 mm in size, have a hard consistency, are localized under the skin, and are painless when pressed. The nodules usually resolve during remission; in the chronic course of rheumatism, they persist even when the acute process subsides.
Minor chorea (Sydenham)
In 10% of clinical cases, brain damage develops. As a result, the control of the higher centers of the nervous system over voluntary movements of the body is disrupted. Minor chorea begins with causeless crying or laughter. Patients cannot control their facial expressions, which causes grimaces and spasms of the lower jaw.
Damage to the extremities leads to muscle twitching and sweeping movements of the arms and legs. Gait and physical activity are impaired, and subsequently self-care at home becomes difficult. Speech becomes explosive and slurred. Minor chorea leads to general weakness and fatigue. A severe course of the disease ends in disability and dependence on the help of others.
Symptoms
As a rule, symptoms depend on the form of manifestation of the pathology. The acute phase is characterized by general and cardiac signs. Among them:
general weakness, lethargy;- loss of performance;
- increased body temperature;
- increased sweating;
- loss of appetite;
- nosebleeds;
- heart rhythm disturbance;
- feeling of discomfort and pain in the sternum;
- increased heart rate (tachycardia), sometimes slowed down (bradycardia);
- shortness of breath, cough, breathing problems;
- pale skin;
- blueness of the tip of the nose and fingers;
- swelling of the legs.
During examination, the patient is found to have an expansion of the boundaries of the heart, the appearance of noise in it, and changes in the structural components of the blood. The liver may also be enlarged.
Rheumatic carditis
The chronic form occurs with untreated rheumatic carditis. It often affects adults who suffered illnesses caused by streptococcal or viral infections in childhood, and also have chronic pathologies of the nasopharynx. Chronic rheumatism of the heart occurs latently, manifesting itself in attacks of exacerbation. Then the person exhibits signs inherent in the acute form of the pathology.
Diagnostics
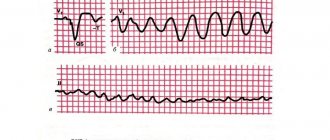
To identify rheumatism of the heart, clinical signs, the fact of a streptococcal infection suffered the day before, and the results of laboratory and instrumental examination methods are taken into account. At the onset of the disease, the Jones criteria are determined. During repeated attacks of rheumatic carditis, these indicators are not informative.
Jones criteria:
- Large (main) : polyarthritis (inflammation of more than 3 joints), rheumatic carditis, minor chorea, annular erythema, rheumatic nodules.
- Minor (additional) : “volatile” nature of joint pain, fever, high ESR (erythrocyte sedimentation rate) and concentration of C-reactive protein in the blood, prolongation of the PR (PQ) interval on the ECG (electrocardiogram).
The primary diagnosis of rheumatism is made if two major or one major and two additional criteria are present. Minor chorea is a sufficient sign and does not require consideration of other manifestations of the disease.
Additional examination methods reveal inflammatory changes in the blood, interruptions in heart function, and provide immunological (antibody) confirmation of streptococcal infection.
Table - Diagnosis of rheumatic carditis
| Method | results |
| General blood analysis | Neutrophilic leukocytosis (12-20 thousand/µl) ESR above 40 mm/h |
| Biochemical blood test | CRP (C-reactive protein) more than 2 mg/dl |
| Immunological blood test | Antistreptococcal antibodies (antistreptolysin-O, antihyaluronidase, antistreptokinase) in high titers Antibodies to DNase B (connective tissue protein) |
| Culture of a swab from the throat and nose | Growth of colonies of beta-hemolytic streptococcus type A on nutrient media |
| ECG | Prolongation of the PR interval (Q) |
| EchoCG (ultrasound examination of the heart) | Violation of hemodynamics (blood movement in the heart chambers) due to deformation of the valves Hypertrophy (thickening) of the myocardium |
| Phonocardiography | Determination of the purity of heart sounds Study of the localization and nature of noise (systolic, diastolic) |
If joints are affected, a puncture is performed to collect and examine the effusion (inflammatory fluid). In severe diagnostic cases, a biopsy with histology of the synovial membrane is prescribed.
Treatment tactics
Heart damage during the primary attack requires hospitalization in a rheumatology hospital under the supervision of a cardiologist. At the same time, inflammation of other organs, such as joints, can be diagnosed. If valve defects and heart failure develop, the patient is usually treated in the cardiology department.
Principles of therapy:
- Strict bed rest for the entire acute period.
- Diet food (table No. 10).
- Hormonal and non-hormonal anti-inflammatory drugs to prevent the death of heart tissue.
- Immunosuppressants to suppress the synthesis of antibodies against the body's own cells.
- Antibiotics to kill streptococcal infections.
- Medicines to support heart function.
During the period of remission, chronic foci of infection are rehabilitated: treatment of caries, removal of decayed teeth, tonsillectomy (removal of pharyngeal tonsils). Strengthen the immune system to prevent colds and infectious diseases. Rational nutrition, proper daily routine, and hardening help increase the body's defenses.
Table - Drugs for rheumatic heart disease
| Name of medications | Mechanism of action | Recommended dosage and duration of use |
| NSAIDs (non-steroidal anti-inflammatory drugs): Acetylsalicylic acid (Aspirin), Naproxen, Diclofenac, Phenylbutazone, Indomethacin | Relieves swelling of tissues Pain relief Suppresses the inflammatory response | Recommend maximum doses for a course of 14-21 days |
| Corticosteroids : Prednisolone, Methylprednisolone, Triamcinolone | Eliminate intense pain Prevents the formation of inflammatory fluid in the joint Reduce the activity of the immune system against heart tissue | Dose 0.25-1 mg/kg per day, maximum 60 mg Duration of therapy - 7-10 days High-dose pulse therapy: 1 g/day intravenously for 3 days in severe cases and a high risk of defect formation |
| Penicillin antibiotics : Ampicillin, Oxacillin, Augmentin | Lead to the death of streptococci | The dose depends on the severity and activity of the infection. Duration of therapy is 10-14 days. |
| Immunosuppressants : Azathioprine, Chlorobutin, 6-Mercaptopurine | Suppresses the formation of antibodies against one's own tissues | Minimum effective dosages are prescribed for carditis Doses are increased if there is a risk of rapid formation of defects Duration of therapy - 2-6 months |
| Means to support heart function: diuretics (Furosemide, Hypothiazide), ACE inhibitors (Enalapril, Lisinopril) calcium channel blockers (Amlodipine, Verapamil) beta blockers (Atenolol, Bisoprolol), cardiac glycosides (Digoxin, Celanide) | Normalizes blood pressure and heart rate Improves metabolic processes in the myocardium Increases the strength of heart contractions Prevents the development of arrhythmias | The dosage is selected depending on the location of carditis and the severity of the disease. |
The basic treatment regimen for rheumatic carditis includes NSAIDs, and in severe cases, glucocorticoids. High activity of the autoimmune process is associated with the risk of developing defects during the first attack of the disease. In such cases, immunosuppressants are prescribed. Antibiotic therapy is recommended in the active phase of streptococcal diseases or in the presence of chronic foci of infection in the body (tonsillitis, sinusitis, caries).
In the event of the formation of heart defects, the issue of performing an operation to reconstruct the valves or replacing them with artificial implants is decided.
Treatment
Therapeutic measures for rheumatism of the heart have a number of features. All therapeutic measures have several goals:
- Elimination of the pathogen;
- Relief of autoimmune aggression;
- Compensation of cardiac activity.
Treatments are carried out in a hospital setting. When diagnosing chronic rheumatic heart disease, mandatory hospitalization is indicated.
For this purpose, the following groups of drugs are used:
- antibiotics: penicillin group,
- lincosamide group,
- groups of macrolides.
Loop diuretics (furosemide, torsemide) are used to treat edema.
To correct and compensate for cardiac activity, the following is used:
- Ca channel blockers;
- b-blockers;
- Cardiac glycosides;
- ACE inhibitors, etc.
Attention! Complexes of drugs and dosages are selected by the attending physician individually in each individual case. Self-medication for rheumatism of the heart is strictly contraindicated!
This is interesting! New developments in treatment
Advances in genetic engineering have led to the emergence of a new generation of drugs—drugs of biological origin. They are synthesized based on monoclonal antibodies present in every living organism to suppress inflammation. The development was based on the study of TNF, a tumor necrosis factor. In rheumatism, it contributes to frequent exacerbations of the disease and increases the risk of deformation of the heart valve apparatus.
In the last decade, TNF inhibitors have been created: Infliximab, Etanercept, Adalimumab. These drugs are successfully used in the treatment of rheumatoid arthritis, which, like rheumatism, is a systemic autoimmune disease. Inhibitors can effectively suppress the destructive effect of antibodies on the body’s own tissues without causing side effects.
Currently, doctors are considering the possibility of including biological drugs in the treatment of rheumatic carditis. For this purpose, clinical studies and observations are carried out. So far, TNF inhibitors are only experimental agents in the treatment of rheumatism.
Diet food
For rheumatic carditis, treatment table No. 10 according to Pevzner is prescribed. Salt in the diet is limited to 6 g/day and fluid intake to 1-1.2 l/day. Dishes are prepared boiled and baked. Frequency of meals: 5-6 times a day.
Table - Diet for rheumatic heart disease
| Recommended Products | Prohibited Products |
| Lean meats (veal, beef, turkey, chicken) | Fatty meats and fish (pork, lamb, mackerel, herring) |
| Soft-boiled eggs, white omelettes | Hard-boiled and fried eggs |
| Lean fish (hake, pollock, carp) | Meat, mushroom, fish broths |
| Cereals (oatmeal, wheat, buckwheat), pasta | Legumes |
| Unsalted butter and vegetable oil | Smoked meats, sausages, canned food |
| Low-fat cheese, cottage cheese, milk | Marinades |
| Bread 2 types, dietary salt-free | Onions, garlic, turnips, radishes, sorrel |
| Vegetables (carrots, zucchini, potatoes, beets) | Mushrooms |
| Ripe fruits, dried fruits | Baking, fresh bread |
| Biscuit, savory cookie | Chocolate |
| Weak tea, fresh vegetable and fruit juices, jelly, rosehip decoction | Coffee, cocoa, alcoholic drinks |
It is recommended to drink mineral water with an alkaline composition: “Essentuki” No. 4 and 17, “Dilijan”, “Borjomi”, “Polyana Kvasova”.
Treatment of rheumatism of the heart
The following groups of drugs are used to treat patients with rheumatism of the heart:
- Antibacterial agents based on penicillin (Amoxiclav).
- Immunosuppressants that can relieve inflammation (“Hydroxylochlorine”).
- Hormonal-based anti-inflammatory steroid drugs (Prednisolone).
- Medicines related to non-steroids ("Ketoprofen").
- To prevent blood clots, antiplatelet agents and anticoagulants (Aspirin) are used.
Surgery is indicated for mature heart valve defects. The affected valves are replaced with artificial prostheses or the normal functioning of the valves is restored using balloon angioplasty.
It is advisable to seek the help of physiotherapy. This method of treatment includes mud baths, ultraviolet irradiation, electrophoresis with an antibacterial solution. All these procedures are an integral part of the sanatorium-resort medical complex.
Traditional medicine is an effective aid in the fight against rheumatism.
Recipe examples:
- Mix two parts beet juice with one part honey. Drink a tablespoon several times a day.
- Mint tea is very easy to prepare: a teaspoon of dried crushed leaves is brewed in 300 ml of water. You should drink on an empty stomach. One glass three times a day.
- Boil a few onions for 10-15 minutes. Let the broth cool and drink 200 g in the morning and evening.
- Dilute lemon juice with water in a 1:1 ratio. Consume on an empty stomach before each meal.
Prevention
Children with rheumatic carditis are subject to clinical observation. Prevention of relapse of the disease is carried out every month for 5 years by prescribing penicillin antibiotics.
Rheumatic carditis prevention regimens:
- Benzylpenicillin - intramuscular injection of 1.2 million units or 600 thousand units (for body weight less than 30 kg).
- Sulfadiazine tablets 1 gram/day (body weight more than 30 kg), 500 mg/day (in case of smaller weight).
- Erythromycin tablets 250 mg 2 times a day for intolerance to penicillin antibiotics.
The prevention regimen is chosen by the attending physician depending on the degree of heart damage, the activity of the rheumatic process and the age of the patient.
Treatment process
Depending on the severity of the pathological process and the general condition of the patient, specialists choose treatment tactics. Drug therapy can only achieve temporary improvement. In most cases, patients undergo surgical correction of existing valve defects, which consists of their replacement or reconstruction.
Medicines intended to eliminate pathology, strengthen the myocardium and stabilize heart function:
- Antibiotics are necessary to eliminate pathogenic bacteria - hemolytic streptococcus. People with rheumatism undergo antibiotic therapy for a long time, in some cases for a lifetime. This is necessary to prevent recurrence of the infection, further damage to the heart and the development of bacterial endocarditis.
- Medicines that improve the rheological properties of blood, prevent thrombosis and stabilize hemodynamic processes are prescribed before and after surgery to all patients. They can prevent the development of a deadly complication - a heart attack. Vascular medications normalize blood flow through artificial valves.
- NSAIDs and corticosteroids reduce signs of inflammation and reduce the risk of heart damage.
- Symptomatic therapy is carried out to eliminate the unpleasant manifestations of the disease. For the treatment of heart failure, patients are prescribed: antiarrhythmic drugs, diuretics, antihypertensive drugs, cardiac glycosides.
- Vitamins and microelements are prescribed to strengthen the myocardium and improve its functioning.
If valve damage leads to hemodynamic disturbances, there is no effect from conservative therapy, or the patient is aggravated by the pathogenesis of the disease, surgical intervention is performed. The defective valve is replaced with a prosthesis, the damaged valves are reconstructed or dissected, and large vessels are stented if necessary. After cardiac surgery, patients undergo rehabilitation treatment and fully recover.
heart valve replacement
Forecast
With timely diagnosis and adequate therapy, rheumatic carditis has a favorable course. Heart defects usually develop due to refusal of treatment and prevention. An unfavorable prognosis occurs in patients with a low level of body defenses. Frequent streptococcal infections contribute to exacerbation of carditis and deformation of the heart valve apparatus. A high risk of mortality from heart failure is observed in children under 7 years of age and elderly patients with concomitant chronic diseases.
Possible complications
Acquired heart disease is a common complication of rheumatic carditis. Most often, the patient is diagnosed with valve insufficiency or stenosis. Against the background of exacerbation of pathology, the following may occur:
- heart and respiratory failure;
- pulmonary artery thrombosis;
- diffuse cardiosclerosis;
- pulmonary hypertension.
Rheumatic attacks provoke arrhythmia, which can lead to sudden stoppage of the main organ. Due to thromboembolism, the development of a heart attack or stroke is possible.
Answers on questions
Question: Which doctor should I contact for rheumatism of the heart?
Answer: When the first symptoms of the disease appear, you should visit a general practitioner or family doctor. The specialist will conduct a complaint survey, examination, listen to heart sounds and prescribe the necessary examinations. Once the diagnosis is confirmed, the doctor will refer you for a consultation with a cardiologist. If there are signs of joint damage, it is necessary to undergo an examination by a rheumatologist.
Question: How is rheumatic carditis prevented in adults?
Answer: Rheumatism is more common in children, so preventive measures have been developed for them. Adults are registered with a cardiologist. Prophylaxis after the first rheumatic attack is not indicated. Before dental and surgical procedures, including invasive examination methods (colonoscopy, biopsy, angiography, etc.), it is recommended to take a short course of penicillin antibiotics to prevent streptococcal infections.
Question: What kind of physical rehabilitation is needed?
Answer: After the acute process subsides, it is necessary to expand physical activity. Semi-bed rest is prescribed for the entire period of exacerbation. At the same time, prolonged physical inactivity promotes the formation of clots in the bloodstream and increases the risk of arterial thromboembolism. Patients are prescribed a course of exercise therapy during the recovery phase. Hiking, swimming, cycling are recommended. When heart defects develop, physical activity is limited according to the severity of the damage to the valve apparatus.
Question: Does a child with a defect require special care?
Answer: Deformation of the valves during rheumatism can have varying degrees of severity. Complex heart defects with critical hemodynamic impairment rarely develop. In this case, the child is prescribed surgery to replace the affected valves. In most cases, acquired defects are compensated by therapy, a special diet and restriction of physical activity. Caring for a child consists of following the doctor’s recommendations and not exceeding the permissible load on the heart.
Question: How to live with heart disease?
Answer: Rheumatic valve disease is not a death sentence. Stenosis or insufficiency limits daily activities only in severe cases. When a heart defect appears, the main task is to prevent the progression of rheumatism. Repeated attacks lead to more severe valve damage and subsequently result in heart failure.
It is necessary to follow a daily routine. Sleeping at least 8 hours helps restore normal functioning of the cardiovascular system. Physical and emotional overload is contraindicated. Daily walks in the fresh air improve blood circulation. You should stick to your diet. Preventative examinations once every 6-12 months allow us to identify negative changes in the functioning of the heart and prescribe treatment. Strengthening the immune system is aimed at preventing colds and viral diseases. They recommend a contrast shower, hardening, and taking immunomodulatory drugs in consultation with your doctor.
What you need to remember
Rheumatic carditis is an autoimmune systemic disease affecting the heart. Pathology develops when the immune system malfunctions, which perceives its own tissues as foreign and destroys them.
What is important to know:
- Rheumatism is more common in children and elderly debilitated patients.
- Repeated infections caused by beta-hemolytic streptococcus type A play a leading role in the development of the disease.
- For the development of an autoimmune conflict, a genetic predisposition is required, which lies in the special structure of the connective tissue of the heart and other internal organs.
- Most often the myocardium and valve apparatus are affected. Acquired defects without treatment lead to heart failure and early mortality.
- Rheumatism of the heart and joints is often encountered in the clinic. Symptoms from the musculoskeletal system precede valve damage.
- Anti-inflammatory, immunosuppressive and antibacterial agents are used in treatment. To influence cardiac symptoms, glycosides, diuretics, antihypertensives, and antiarrhythmic drugs are prescribed.
- Children are given prophylaxis with penicillin to prevent exacerbation and progression of the disease.
- The prognosis is favorable in the absence of severe heart defects.
Clinical observation by a rheumatologist and cardiologist can reduce the risk of complications. Annual medical examinations are aimed at early diagnosis of heart defects.
Rheumatic heart disease can be avoided if the primary manifestation of the infection, rheumatism of the joints, is promptly identified and properly treated. The insidiousness of the disease lies in the fact that it can be asymptomatic. Read about how not to miss rheumatism of the joints, about modern methods of diagnosing and treating pathology in the article here.
Symptoms
A typical manifestation of rheumatism in a child or an elderly person is chronic fatigue. Any load is difficult. Efficiency, physical and mental activity decreases.
Other characteristic symptoms of the disease in children and adults:
- attacks of tachycardia;
- chest pain in the heart area;
- increased sweating;
- shortness of breath on exertion;
- muscle weakness, lethargy, drowsiness;
- headache;
- white tint of the skin;
- frequent nosebleeds;
- feverish state with high wave-like thermometer readings;
- discomfort, swelling and pain in the joints.
- sometimes a rash appears and rheumatic tubercles form.