Arterial hypotension or hypotension is a persistent or periodic decrease in blood pressure to levels that are considered less than the WHO limit - 100 per 60 mmHg.
Low pressure may have other values that differ from the “reference” indicator by 5-10 units. This is also a variant of the functional norm; there is no need to see a doctor with it if you feel well.
If the pressure is below 90 to 55 and drops further, this is a reason to seriously think about it and call an ambulance for initial treatment measures.
An individual norm should not be regarded as something inert; it can vary slightly throughout life. However, if a pressure of 100 over 60 and below is observed in an “avid” hypertensive patient, there is no question of any normality.
What do you need to know about hypotension in different categories of patients?
What pressure is considered low?
Low blood pressure is a fairly broad concept. Even doctors cannot come to a consensus on this matter.
Everyone adheres to the standards specified by the World Health Organization, that is, an indicator at 100 per 60 mmHg as the lower possible limit.
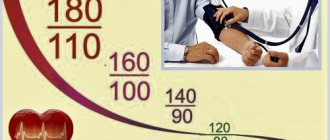
Depending on the level of blood pressure, several degrees of arterial hypotension can be distinguished:
- Level 100/60. This is not yet a pathology, but it is already an alarm bell, especially for patients with normal tonometer readings.
- 90 to 55 and slightly lower - arterial hypotension of degrees I-II. It occurs somewhat less frequently and indicates functional changes in the central nervous system, cardiovascular structures or excretory tract.
- 80 to 50 or less. Hypotension III-IV degree. Poses a danger to health and life. Requires urgent treatment in a hospital. Also continuous monitoring on an outpatient basis.
- Blood pressure is below 70/50, a critical indicator. Cardiogenic shock and death may occur.
The pressure is also considered low if the patient at the time of its level change feels worse than at the “working” indicator.
All of the above is true only for adults. Children have different standards and need to be assessed separately.
Drug therapy for hypotension
In the arsenal of modern pharmacology there are no special drugs that can quickly and safely increase blood pressure. Most existing hypertensive drugs have a number of side effects and are used primarily parenterally in hospital settings for acute hypotension. Available over-the-counter medications include caffeinated medications and adaptogens.
| Drug groups / Trade names | Indications | pharmachologic effect |
| Analgesics (with additional caffeine content) Citramon, Caffetin, Askofen, Pyramein, Coficil | Combined drugs. Indicated for hypotension complicated by pain, elevated body temperature, and inflammation | They have anti-inflammatory, analgesic, antipyretic, and moderate hypertensive effects. Caffeine activates the central nervous system, stimulates metabolism, accelerates heart rate, and restores the body's energy potential. |
| Adaptogens / Pantocrine, Saparal, tinctures of ginseng, lemongrass, rosea radiola | Natural preparations of plant or animal origin. Indicated for reduced performance, physical and nervous exhaustion, hypotension, metabolic disorders, anemia, intimate disorders | They have a stimulating (tonic) effect on the muscular and central nervous systems, and constrict peripheral blood vessels. Accelerate metabolism, increase the body’s resistance to adverse factors (infectious diseases, physical, mental overload) |
| Alpha adrenergic agonists / Clonidine, Gutron, Mezaton | Fast-acting drugs. Indicated for rapid elevation of blood pressure during orthostatic hypotension. Used by injection | They increase the tone of the vascular walls, increase peripheral resistance, and constrict blood vessels. Prevent congestion, improve blood supply to organs |
| Analeptics / Cordiamin, Corazol, Etimizol, Bemegride | "Revitalizing" drugs. Indicated in emergency conditions for acute forms of hypotension. Used for collapse, asphyxia, shock, acute circulatory disorders, respiratory failure, critical decrease in blood pressure | They stimulate the respiratory and vasomotor centers of the brain, stimulate blood circulation, and tone blood vessels. Activate the central nervous system, increase heart rate, increase blood pressure |
Physiological factors
- Prolonged stay in hot climates or high temperature conditions. For example, living in countries with a subtropical climate, working in a steel mill, etc. This is a natural defense mechanism of the body to prevent pathological changes in the heart and blood vessels.
- Professional sports. Low blood pressure is normal for athletes. The heart tries to avoid overload, thus the body prevents dangerous conditions.
- Borderline hormonal conditions. Like menopause (menopause in men and women), the menstrual cycle in any phase, pregnancy (functional physiological hypotension during gestation is common) or puberty, when a real storm is raging in the body of a young patient.
- Long-term smoking. Nicotine and harmful substances contained in cigarettes and all tobacco products affect the body in different ways. For some, blood pressure rises, while for others it drops to significant levels. In all cases, giving up a bad habit will be a reliable method of correcting the condition.
- Reduced consumption of table salt. The lack of minerals, namely sodium and potassium, in the body affects it. Although salt is considered a poison, it is necessary for the normal functioning of the human body.
- Abuse of antihypertensive drugs. If the treatment regimen for hypertension is incorrect or insufficiently adequate, a violation of the specific regulation of vascular tone and the production of special substances occurs. Both the patients themselves and illiterate doctors who do not take their work responsibly enough are to blame here.
When should you talk about reducing blood pressure?
The generally accepted norms for blood pressure are the numbers on the tonometer 120/80. Not only do people with such indicators feel comfortable, but also with a slight deviation from the scale. It depends on a person’s age, genetics, physiological characteristics, and pace of life.
A decrease in pressure to 110 to 70 or 65 for someone is a common condition in which there is no discomfort or loss of strength. In medical practice, it is not customary to talk about hypotension if the blood pressure of a healthy person fluctuates between 105 over 70 or 90 over 65.
On a note! But if additional symptoms appear, in addition to the digital values of low pressure, there is reason to think about consulting a therapist or cardiologist to find the root cause of the onset of hypotension.
There are people who feel great with a pressure of 100 over 70 or 140 over 90. They do not develop pathologies of the cardiovascular system and do not have any health problems after a full examination. If blood pressure begins to approach levels that are normal for most people, then complaints of some discomfort may appear. A sharp decrease in pressure as a symptom of the disease can only be discussed if there are systematic changes in the blood pressure monitor and the presence of additional symptoms.
Pathological factors
The list of pathological causes is much wider and everything here is not so harmless:
- Diseases of the excretory system. If the kidneys are not working properly, there may be a disruption in the secretion of prehormone renin, which is responsible for the normal regulation of vascular tone (strictly speaking, renin itself does not perform such a function, we are talking about its metabolites). Among the possible diseases, nephropathies, glomerulonephritis, pyelonephritis, and nephritis are on par.
- Pathologies of cerebral vessels. Hypotension may occur in case of cerebrovascular accident. The record holders for the number of causing phenomena are cervical osteochondrosis and vertebrobasilar insufficiency.
Attention:
Both diseases require mandatory treatment, since everything can end in a stroke.
- Stroke and condition after it. A low blood pressure level is considered quite normal after an emergency. The body adapts to new living conditions.
Such patients, however, need to be constantly monitored. Regular examinations help prevent relapse, which is often fatal.
- Heart pathologies. There are a lot of them. Among the most common processes are congestive heart failure, coronary heart disease, and heart attack. All pathologies require careful outpatient monitoring by a cardiologist.
- Anemia. Most often iron deficiency. Pathology associated with insufficient amount of hemoglobin in the blood.
Hence hypoxia and disruption of cellular nutrition, including the structures of the heart and brain in the system.
In addition to the main symptom, such as hypotension, there are many other manifestations. It is difficult, if not impossible, not to notice them. Therefore, diagnosis is not a problem.
- Avitaminosis, hypovitaminosis. Associated, as a rule, with poor nutrition. “Diet” girls know firsthand about the condition when their vision gets dark and there is no strength to do anything.
- Regular bleeding. They are especially common in pathologies of the gastrointestinal tract and gynecological profile.
Acute conditions associated with massive blood loss are accompanied by a critical drop in blood pressure, the reason being a violation of circulating blood volume and general hemodynamics.
- Endocrine diseases. Including those associated with insufficient synthesis of cortisol by the adrenal glands, TSH, T3, T4 by the thyroid gland and pituitary system. Changes in the patient's diabetes status are also possible.
- Infectious pathologies. The reason for the decrease in tonometer readings is intoxication of the body. Such dangerous diseases as tuberculosis are especially affected.
The list of reasons is incomplete, but they are talked about most often. Each specific case needs to be examined.
Attention:
Etiology plays a big role in prescribing adequate therapy: it is the fight against the root cause that is the main task of the doctor.
Why does blood pressure drop sharply?
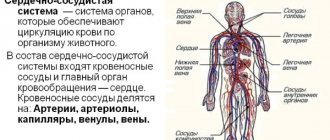
The physiological causes of a sharp drop in pressure are associated with a weakening of vascular tone. In hypotensive patients, the reactions of constriction and dilation of blood vessels slow down, resulting in oxygen starvation of organs and tissues. Due to insufficient blood supply, a deterioration in well-being is observed.
The function of controlling blood pressure levels is assigned to the hypothalamus and pituitary gland. The coordinated actions of these parts of the brain contribute to the transmission of nerve impulses to the vessels, which respond with contraction.
When the balance in the hypothalamic-pituitary system is disturbed, they remain dilated, and blood pressure does not rise. There are many reasons for the development of the disorder and a sharp drop in blood pressure - from the banal “being nervous” to serious diseases such as heart failure.
Types and causes of arterial hypotension
There are acute and chronic forms of hypotension. Acute develops against the background of myocardial infarction, thromboembolism, acute gastric ulcer, duodenal ulcer, peritonitis, as well as nasal, hemorrhoidal, and other internal bleeding.
Chronic hypotension is classified into: physiological, primary, secondary.
The cause of physiological hypotension is the congenital characteristics of the nervous system. Thus, a chronic decrease in blood pressure is typical for people with an asthenic body type. Asthenics have a hard time withstanding even a slight increase in blood pressure (up to 130/90). Physiological hypotension is also diagnosed in athletes and people whose activities involve physical labor. In such cases, the body simply adapts to consume oxygen sparingly.
Primary hypotension is most often the result of a strong emotional shock, physical overload, or the body’s individual reaction to some irritating factor. The disease develops as a result of:
- stress, increased nervousness, depression;
- use of certain medications (peripheral vasodilators, beta-blockers, antibiotics, sedatives);
- weather sensitivity;
- taking hot baths, body wraps, visiting baths, saunas;
- strict diets, hunger strikes, excessive physical activity.
Secondary hypotension is a symptom of an underlying disease. A chronic decrease in blood pressure is observed in neurocirculatory dystonia of the hypotonic type. It is characterized by increased production of the “weakness” hormone – acetylcholine. Sometimes mixed acetylcholine and adrenaline reactions are observed, which explains unreasonable jumps in blood pressure during the day.
In addition, secondary hypotension develops when:
- myocardial dysfunction (after endocarditis, myocarditis);
- liver cirrhosis;
- diseases of the spine, osteochondrosis;
- pathologies of the thyroid gland;
- iron deficiency anemia;
- diabetes mellitus;
- dehydration of the body;
- traumatic injury to the brain or spinal cord;
- acute intoxication.
Short-term hypotension (orthostatic) is possible with a sudden change in body position. The rapid outflow of blood from the brain provokes the development of an attack of dizziness.
Consequences of pathology
There is an opinion that low blood pressure exclusively affects the quality of life, without disrupting the functions of organs and systems. It is wrong.
At the physiological level, hypotension results in insufficient cerebral blood supply. The brain does not receive the necessary volumes of oxygen; against the background of oxygen starvation, the likelihood of:
- development of ischemic stroke;
- damage to areas responsible for vision and hearing;
- accelerated progression of angina pectoris, cardiosclerosis, and other myocardial diseases.
Low blood pressure should always be considered in combination with high blood pressure: chronic hypotension in youth against the background of vascular atherosclerosis, as well as chronic heart disease, is the cause of arterial hypertension in old age.
Characteristic symptoms
Possible symptoms include the following:
- Hypothermia. A decrease in body temperature below normal values of 36 degrees. Popularly called loss of strength. The reverse process is also possible - an increase in thermometer readings. What causes the violation of thermoregulation is not completely known.
- Yawn. It is considered a characteristic sign of lack of oxygen and tissue hypoxia. However, this has not been proven.
- Episodic or prolonged dizziness are typical signs of low blood pressure. It is determined by insufficient nutrition of the cerebellum, which controls the entire vestibular apparatus of the body.
- Dyspepsia, including nausea, vomiting, flatulence, intestinal motility disorders.
- Pallor of the dermal layer. The patient appears lifeless and waxy.
- Sweating or hyperhidrosis for no reason.
- Disturbances of cyclic processes in a woman’s body.
- Headache of a pressing, squeezing nature. Pulsates in time with the beat of the heart.
- Fainting and other syncope.
- Problems with erectile function in the stronger sex due to insufficient blood circulation in the cavernous bodies of the reproductive organ.
- Noise in ears.
- Darkening in the eyes.
- Chest pain. This symptom of low blood pressure may indicate an upcoming angina attack.
Patients are accompanied by the whole complex of sensations or only a part. It all depends on the nature and duration of the process and its root cause.
Hypotonic patients with experience partially adapt to the pathological condition. This makes diagnosis somewhat more difficult.
Manifestations of hypotension
Subjective symptoms with a sharp decrease in pressure are associated with insufficient blood supply to vital organs.
The main manifestations of chronic hypotension:
- throbbing headache localized in the forehead and temples, worsening after emotional or physical stress;
- general weakness, absent-mindedness, fatigue;
- decreased concentration, memory impairment, apathy;
- unreasonable irritability;
- frequent attacks of dizziness;
- noise in ears;
- pale skin;
- increased heart rate, shortness of breath;
- moderate pain in the heart area lasting up to 30 minutes;
- constipation, flatulence, colic;
- nausea, vomiting, belching.
Such diverse symptoms are characteristic not only of hypotension, but also of other more serious diseases, which confirms the need to visit a doctor for an accurate diagnosis.
In acute hypotension, the above symptoms are pronounced. The condition quickly worsens until loss of consciousness.
What are the dangers of developing low blood pressure?
Low blood pressure less than 90/55 mm Hg. Art. extremely dangerous, especially if the pathology lasts for a long time.
Attention:
Hypertensive patients are almost three times more likely to develop complications when their blood pressure decreases.
Possible consequences include:
- Fainting of a sudden nature. They may well catch the patient at the wrong moment: on the road, on the stairs, while driving a car. This is certain death or, at a minimum, severe injury.
- Heart failure and coronary heart disease. They develop as a result of malnutrition of organ structures. Often the next “stop” is myocardial infarction. Whether the patient will recover from this or not is a highly controversial issue.
- Problems with cognitive functions, mental disorders. A long-term hypotensive process poses an increased risk of developing Alzheimer's disease and early dementia.
- Stroke. In most cases ischemic. As a result of insufficient nutrition of cerebral structures. Atherosclerosis increases the risk by approximately 4 times.
- Morgagni-Adams-Stokes syndrome. A dangerous pathological process accompanied by fainting as a result of cerebral ischemia.
These are just some of the consequences. Contrary to what people may think, hypotension is no less dangerous than hypertension.
Is there a treatment for hypotension?
To understand how to treat a patient, the reason for the decrease in readings on the tonometer must be found. The disease hypotension is not the main pathology. This condition is usually preceded by some other illness, non-compliance with sleep and rest, neglect of the principles of proper nutrition, or a sharp refusal to eat in order to lose weight. If the root cause is not removed, attacks of sharp decline will be repeated.
In hypertension, a decrease in blood pressure is usually a good signal that you are feeling better and that your medication needs to be adjusted. Complete withdrawal of drugs is possible if the dynamics of pressure reduction to normal levels is stable and overall health is positive.
On a note! A sharp decrease in blood pressure in men is less common than in women and is observed with overwork or serious problems in the cardiovascular system.
What to do at home?
There is very little you can do at home. If the pressure has not been corrected with medications and permanent treatment has not yet been prescribed, and the numbers are steadily creeping down, you need to call an ambulance to resolve the issue of hospitalization or, at least, help on the spot.
First aid algorithm at the prehospital stage:
- Before the doctors arrive, you need to take a horizontal position and move as little as possible. This can be dangerous and can lead to a sharp drop in blood pressure levels.
- Next, you need to take a tonic drug - a caffeine tablet, maybe two. In the absence of this, Citramon will be used, but it is “heavier” due to the presence of paracetamol in the composition. Both drugs should be in your home medicine cabinet as a means to quickly raise blood pressure.
- Drink a tonic drink: you can have coffee or strong tea, one or two cups. Or eat a salty product, such as a cucumber.
- If after 20 minutes the pressure has not increased, drink tincture of eleutherococcus (one teaspoon) or ginseng (30 drops).
If after the above steps there is no normalization of the indicators, an ambulance call is required. This is definitely not a physiological phenomenon.
What to avoid:
- Physical activity.
- Wash with cold water, take baths, contrast showers.
- Drink alcohol.
In general, amateur activities should be kept to a minimum. You should rely on the experience and capabilities of doctors. This is the most correct and safe solution.
If hospitalization is impossible, it is recommended to quickly decide on a visit to the attending cardiologist to prescribe permanent therapy and its further correction.
Signs of emergency conditions
In addition to the symptoms already described, you need to keep in mind the signs of processes dangerous to health and life.
Among the symptoms:
- Acute headache of a stabbing nature.
- Loss of orientation in space.
- Mental disorders such as organic psychosis. This is also possible. Hallucinatory or delusional-hallucinatory symptoms predominate, as in schizophrenia or alcoholic delirium.
- Intense pain in the heart. They press, ache, and radiate to the epigastrium (the area above the abdomen) and the shoulder blade. They don't allow me to breathe normally.
- Shortness of breath, suffocation.
- Inability to control facial muscles.
- Disturbance in the speaking process.
In these cases, you need to urgently call an ambulance. Perhaps we are talking about a heart attack or stroke.
Symptoms that require you to see a doctor
In addition to the manifestations already mentioned, attention should be paid to the following points:
- Facial distortion. Impaired controllability of facial muscles. Often accompanies a stroke.
- Syncope more than once a day. In other words, fainting.
- Persistent arrhythmia such as tachycardia (pulse more than 80 beats per minute) or bradycardia (less than 60 beats per minute). Both scenarios are unfavorable in terms of prognosis if they are not corrected. A similar sign of low blood pressure in a woman ends in cardiogenic shock, thromboembolism, cardiac arrest, the development of tissue ischemia, chronic organ diseases, etc.
- Loss of vision, even short-term. Indicates stenosis of the retinal arteries. Possible ruptures of blood supply structures, hemophthalmos, secondary detachment and complete loss of function.
- Impaired motor activity of half the body. Manifestation of stroke.
- Inability to speak normally (slow, drawn out diction).
- Chest pain of a pressing nature. They radiate (give) to the stomach, back and arms. They don't allow you to breathe normally.
Any of the above symptoms requires calling an ambulance for initial measures and possible transportation to a cardiology hospital.
What needs to be examined?
A cardiology specialist is involved in the diagnosis and management of patients with arterial hypotension of cardiac origin.
With a mixed etiology of the process (for example, with kidney disease and osteochondrosis at the same time), additional help from an endocrinologist, neurologist or nephrologist is required. Perhaps all of them at once.
At the initial appointment, anamnesis is collected and complaints are objectified through a survey regarding complaints.
The list of studies may be as follows:
- Heart rhythm study. Tachycardia or bradycardia can say a lot about the process.
- Estimation of blood pressure level at the current time. The patient needs to calm down. Otherwise the result will be false.
- Estimation of daily blood pressure. It is carried out using a Holter monitor or, in other words, an automatic tonometer.
- Electrocardiography.
- Invasive tests to assess myocardial conductivity.
- Load tests.
- Study of the concentration of specific hormones in the bloodstream.
- Assessment of neurological and psychiatric status.
This is sufficient in the system, but additional tests may be performed to clarify the diagnosis. Everything is at the discretion of the treating specialist.
Necessary examinations
A comprehensive assessment of the patient’s condition is carried out by a cardiologist, nephrologist, neurologist, and endocrinologist.
Sometimes the first symptom is menstrual irregularity, and a woman turns to a gynecologist.
Such a “consilium” of specialists will help quickly understand the problem.
Approximate research scheme:
- Anamnesis collection. Including determination of family predisposition to hypotension.
- Interviewing the patient for complaints.
- Blood pressure measurements on both arms. The fact of deviation is established.
- Holter monitoring for 24 hours. The most informative procedure.
- Electrocardiography with stress tests to identify the etiology of the process.
- Tests of blood, urine, hormones of the thyroid gland, adrenal cortex, pituitary gland, sex substances (estrogen, progesterone, SHBG, LH, prolactin).
- Ultrasound of the kidneys and pelvis.
- If necessary, MRI, CT diagnostics. Especially if neoplasia (tumor) is suspected. Possibly with contrast enhancement with gadolinium preparations.
- Gynecological examination, palpation of the kidneys, assessment of neurological status.
- Electroencephalography.
Consistency is the main condition. Making a diagnosis does not take much time.
How is the treatment carried out and how to eliminate the pathological decrease in blood pressure?
Treatment is required only if a pathological origin of hypotension is proven.
In other situations, it is recommended to correct the underlying physiological cause in order to normalize blood pressure levels.
There are multiple medications for the treatment of hypotension; they are prescribed at the discretion of the doctor.
A sample list that can be used:
- Cerebrovascular. Improves cerebral circulation and heart trophism. Piracetam, Actovegin.
- Nootropics. Normalize metabolism in cerebral structures. Glycine.
- Midodrine and its analogs. Constrict blood vessels, increase blood pressure.
- Caffeine and preparations based on it. Including Citramon, but with caution.
However, symptomatic therapy alone is not enough. It is necessary to eliminate the root cause of the pathological process. This is the main task of a doctor.
Lifestyle correction plays an important role in therapy. It is necessary to give up smoking, alcoholic beverages (not a drop of alcohol), normalize your diet and drink enough liquid (but no more than 2 liters per day).
Plus, you need to live more actively, avoiding physical inactivity. Light physical activity under the supervision of a physical therapy doctor is recommended. No gyms or other places associated with exhausting workouts. Only prescribed sets of exercises.
Nutrition involves fragmentation, the predominance of fortified foods and the rejection of junk food. The same recommendations are used as prevention.
With a conscientious attitude to the doctors’ recommendations, the patient will quickly get back on his feet. It is possible to raise blood pressure in the long term only using systematic methods.
Several main causes of hypotension
To understand why there is low pressure during measurements, it is necessary to identify the pathological causes that provoke the phenomenon.
Among the reasons that lower blood pressure are the following:
- malfunctions of the peripheral nervous system, which is responsible for the normal functioning of blood vessels and internal organs. Concerns about manifestations of general weakness, increased sweating, difficulty breathing;
- pathological processes of the heart muscle and blood vessels. If the heart muscle does not function at full capacity, then the amount of blood flowing to the organs decreases and the pressure drops;
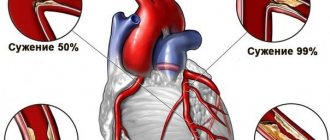
- atherosclerosis. The lumens of the vascular walls narrow, which is often observed in old age. Atherosclerosis develops due to changes in the structure of vascular tissue, which becomes less strong and elastic. A very strong plaque settles on the vascular walls, interfering with the normal supply of oxygen and nutrition to tissues;
- pathological processes occurring in the endocrine system, as a result of which the hormonal balance in the body is disrupted. If the functioning of the adrenal glands malfunctions, the level of sodium in the body is disrupted. Problems in the functioning of the thyroid gland lead to a decrease in the frequency of contraction of the heart muscle and affect vascular tone;
- blood clots that occur due to blockage of the vascular walls. This is one of the most dangerous reasons, which can cause very serious consequences;
- sunstroke, shock from pain;
- blood loss.
Taking more than one type of medication or diuretic can cause a decrease in blood pressure if taken uncontrolled and without medical prescription. In this case, drug-induced hypotension develops. By reducing high indicators, you can reduce indicators to a critical value.
Prognosis and prognostic factors
For long-term pathological hypotension, it is relatively favorable, subject to constant monitoring of the condition by a doctor and complete, comprehensive treatment.
Unfavorable in the absence of treatment, since there is a high risk of complications. Also unfavorable in the presence of severe consequences described above. If the disease lasts for a long time, they are irreversible.
We are talking about the prognosis for maintaining the ability to work, life and the ability to independently care. Complex therapy on an ongoing basis will help improve the outcome.