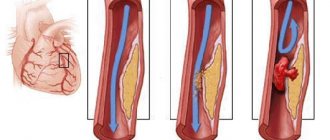
Myocardial infarction is an acute pathology that develops as a result of blockage of a cardiac artery. The formation of a cholesterol plaque can disrupt blood circulation within the entire heart muscle. In this case, a number of serious consequences may occur, leading to death. To accurately establish a diagnosis, modern cardiology uses an ECG study. Depending on the displayed image of this device, two types of this disease are distinguished: without a q wave (not a q heart attack) and with its presence. The first type does not relate to extensive heart damage, and mortality from it in hospital conditions is quite rare. The second option has a worse prognosis.
General provisions
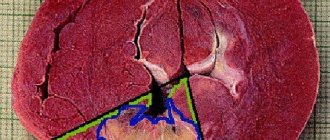
Q infarction is also called macrofocal or transmural. It is characterized by extensive necrosis of the heart muscle and is one of the most dangerous cardiac diseases. Such damage often affects the entire heart, causing sudden death of the organ.
Recently, cases of development of this species have become significantly more frequent. Today, among all heart attacks, its share is about 60%. Therefore, timely diagnosis and subsequent competent treatment are very important.
Reasons for development
Myocardial infarction q occurs as a complication of cardiac ischemia. This disease mainly affects older people. Most often it is detected in elderly patients who have any pathologies in the functioning of the cardiovascular system. The development of the disease is largely influenced by genetic predisposition. Therefore, people whose relatives have had a heart attack should undergo systematic monitoring by a cardiologist.
Today, experts identify the following risk factors for the disease:
- Having bad habits. This is alcohol, smoking, drugs.
- Dyslipidemia, characterized by an increase in the level of low-density lipoproteins.
- Diseases of the circulatory system.
- Insufficient physical activity.
- Venous thrombosis.
- Endocrine disorders (thyrotoxicosis, diabetes, obesity).
In youth, this disease most often affects men. The fact is that the presence of estrogens provides the female body with protection from cardiac diseases.
The situation changes during menopause, when pathology develops equally for both sexes.
Medical nutrition
Nutrition for patients in the intensive care unit should not be burdensome for the cardiovascular system. The daily energy value of the diet is 1000-1500 kcal.
In order to reduce the load on the cardiovascular system, split (5-6 meals a day) meals in small portions are recommended. Easily digestible, non-rough food is allowed, low in cholesterol and animal fats, which does not cause increased gas formation.
The diet must include foods that promote bowel movement (prunes, dried apricots, beets, vinaigrette, vegetable oil, etc.). Normalization of stool is extremely important, since constipation and straining worsen coronary circulation and contribute to the development of cardiac arrhythmias.
DETAILS: Myocardial rupture during myocardial infarction
Classification of the disease
There are several types of lesions of the heart muscle. They may differ in treatment and have different clinical signs. The severity of ischemia depends on the degree of tissue necrosis, the number of attacks observed during the year and associated complications.
Regarding the time of occurrence, cardiac muscle necrosis can be:
- Primary (acute form of heart attack), which manifests itself a couple of months after the development of ischemia.
- Repeated, appearing eight weeks after the initial attack.
- Recurrent if a new attack appears earlier than two months after the end of the old one.
Depending on how damaged the heart muscle is, the disease may be:
- Small-focal, which has a relatively mild course due to the fact that the lesion affects a smaller area of the heart muscle (on the ECG it appears as a heart attack without a Q wave).
- Large focal, in which almost the entire organ is affected (a Q wave is present).
Pathogenesis
During its development, the disease goes through two large phases:
- the occurrence of necrotic changes;
- scarring period.
At the first stage, signs of organ damage appear, after which they disappear. An ECG during the development of the disease can reveal the presence of abnormalities of the following nature:
- Acute stage. It is characterized by a relatively calm flow. At this stage, a necrotic area is actively forming, the patient’s body temperature rises slightly, and fatigue appears. During a Q-infarction, the patient's blood contains a high amount of the protein troponin. It is appropriate to study markers such as LDH, CPK, AST, since changes in the enzyme ratio are observed. Extensive necrosis of the heart muscle is indicated by the appearance of the Q wave. At first, the pathology may appear on the ECG as follows: positive progression of the T wave, and the R wave becomes part of the ST segment, without approaching the isoline.
- The most acute stage. At this stage, the ECG records the appearance of T-waves of enormous size and high amplitude - these are signs of subendocardial cardiac damage. Violations of coronary blood flow are primarily reflected in these areas. The patient complains of the presence of chest pain. The duration of this period can reach from half an hour to two hours.
- Subacute stage. Involves the transition of a necrotic area into connective tissue and usually lasts up to a month. At this stage, the mass of the heart muscle decreases, and arrhythmia or failure may appear. The patient's condition normalizes: a decrease in body temperature, favorable results of laboratory tests. But the pathological Q wave is still visible on the cardiogram, indicating the presence of a large necrotic focus. Other changes on the ECG present during this period: a deep T wave, which has a negative value. The ST segment approaches the isoline.
- Scarring period. Characterized by normalization of the number of leukocytes. In place of necrotic masses, scar tissue forms. Adhesions are formed, indicating the presence of large-focal cardiosclerosis. In the post-infarction state, the Q wave remains. The ST segment will be located exactly along the line, ending with a T wave, which has a positive or negative value.
The importance of ECG in the diagnosis of myocardial infarction
- What information is included in the ECG technique?
- What indicates the period and duration of the disease
- How is the location of a heart attack determined?
- Is it possible to find out how extensive the damage area is?
- Diagnosis of the depth of myocardial necrosis
- Difficulties of ECG diagnostics
Electrocardiography (ECG) plays an important role in making the diagnosis of myocardial infarction.
The technique is simple and informative. Modern portable devices allow you to take ECGs at home, in a factory health center. According to various authors, the signs identified during the examination can be deceptive in 9% of cases.
The nature of the ECG, which reflects the potential difference between healthy and diseased tissue, changes depending on the course of the pathological process in the tissue. Therefore, the results of repeated studies are important.
100 years ago, a method was developed to record electrical changes in the heart muscle. Electrocardiography is a method that allows you to record the action currents arising in the beating heart. In their absence, the galvanometer needle writes a straight line (isoline), and at different phases of excitation of myocardial cells, characteristic teeth appear with the direction up or down. The processes occurring in the heart tissue are called depolarization and repolarization.
This article will tell you more about the mechanisms of contraction, changes in depolarization and repolarization.
The ECG is recorded in three standard leads, three enhanced leads and six chest leads. If necessary, special leads are added to study the posterior parts of the heart. Each lead is fixed with its own line and is used in diagnosing heart damage. The complex ECG contains 12 graphic images, each of which must be studied.
In total, there are 5 waves on the ECG (P, Q, R, S, T), an additional U rarely appears. They are normally directed in their own direction, have width, height and depth. There are intervals between the teeth, which are also measured. In addition, the deviation of the interval from the isoline (up or down) is recorded.
Each of the teeth reflects the functionality of a specific part of the heart muscle. The relationship between individual teeth in height and depth and direction is taken into account. The information obtained allows us to establish the differences between normal myocardial function and altered ECG by various diseases.
Features of the ECG during myocardial infarction make it possible to identify and record signs of the disease that are important for diagnosis and subsequent therapy.
Acute infarction with a typical course goes through 3 periods of development. Each of them has its own manifestations on the ECG.
The early period - the first 7 days, is divided into the following stages:
- stage of ischemia (usually the first 2 hours) - a tall T wave appears above the focus;
- stage of damage (from a day to three) - the ST interval rises and the T wave moves down, it is important that these changes are reversible, with the help of treatment it is still possible to stop myocardial damage;
- formation of necrosis - an expanded and deep Q wave appears, R wave is significantly reduced. The focus of necrosis is surrounded by a zone of damage and ischemia. How large they are is indicated by the distribution of changes in different leads. Due to damage, the heart attack may increase. Therefore, treatment is aimed at helping the cells in these areas.
At the same time, various rhythm disturbances occur, so the ECG is expected to identify the first symptoms of arrhythmia.
Subacute - from 10 days to a month, the ECG gradually returns to normal, the ST interval drops to the isoline (the doctors at the functional diagnostics office say “sits down”), and signs of a scar form at the site of necrosis:
- Q decreases and may disappear completely;
- R rises to its previous level;
- only negative T remains.
The scarring period is from a month or more.
Thus, based on the nature of the ECG, the doctor can determine how long ago the disease appeared. Some authors distinguish separately the formation of cardiosclerosis at the site of a heart attack.
In most cases of ischemia, the infarction is located in the myocardium of the left ventricle; right-sided localization is much less common. Lesions on the anterior, lateral and posterior surfaces are distinguished. They are reflected in different ECG leads:
- with an anterior infarction, all characteristic signs appear in chest leads V1, V2, V3, 1 and 2 standard, in enhanced AVL;
- lateral wall infarction in isolation is rare, more often spreads from the anterior or posterior wall of the left ventricle, characterized by changes in leads V3, V4, V5, in combination with 1 and 2 standard and enhanced AVL;
- posterior infarction is divided into: lower (diaphragmatic) - pathological changes are detected in the enhanced lead AVF, the second and third standard; upper (basal) - manifested by an increase in the R wave in the leads to the left of the sternum, V1, V2, V3, the Q wave is rare.
Infarctions of the right ventricle and atria are very rare; they are usually “covered” by symptoms of damage to the left side of the heart.
The prevalence of a heart attack is judged by identifying changes in the leads:
- small focal infarction is manifested only by a negative “coronary” T and a shift in the ST interval, no R and Q pathology is observed;
- widespread infarction causes changes in all leads.
Depending on the depth of penetration of necrosis, the following are distinguished:
- subepicardial localization - the affected area is located under the outer layer of the heart;
- subendocardial - necrosis is localized near the inner layer;
- transmural infarction - affects the entire thickness of the myocardium.
When interpreting the ECG, the doctor must indicate the expected depth of the lesion.
The arrangement of teeth and intervals is influenced by various factors:
- the patient's obesity changes the electrical position of the heart;
- cicatricial changes after a previous heart attack do not allow identifying new ones;
- conduction disturbance in the form of a complete block along the left bundle branch makes it impossible to diagnose ischemia;
- A “frozen” ECG against the background of a developing cardiac aneurysm does not show new dynamics.
Modern technical capabilities of new ECG devices make it possible to simplify the doctor’s calculations (they are done automatically). Holter monitoring provides continuous recording throughout the day. Cardiac monitoring in the room with an audible alarm allows you to quickly respond to changes in heart rate.
The diagnosis is made by a doctor, taking into account clinical symptoms. ECG is an auxiliary method that can become the main one in decisive situations.
To make an accurate diagnosis of a patient with myocardial infarction, the following diagnostic methods are used:
- taking anamnesis;
- interviewing the patient to establish all symptoms;
- conducting an ECG;
- studying the composition of blood serum in order to find cardiac-specific macromolecules;
- differential analysis of the obtained data.
Inferobasal myocardial infarction is almost always diagnosed using an ECG.
Symptoms
The development of this pathology is indicated by the following symptoms:
- excessive sweating;
- the skin becomes sticky and cool;
- weak arms and legs;
- attacks of nausea, often ending in vomiting;
- feverish condition;
- the jugular veins increase in size and swell;
- pulmonary wheezing is observed when breathing;
- against the background of pericarditis, a characteristic noise caused by friction of the pericardium is possible;
- the appearance of systolic murmur;
- in some cases, the formation of dyskinetic apical beats occurs.
When the disease is in a period of exacerbation, the patient may suffer from pain similar to signs of angina pectoris. Only their intensity and duration will be more pronounced. Unpleasant sensations can spread throughout the chest.
A heart attack is accompanied by ischemic damage, leading to tissue death. During this process, the concentration of adenosine and lactate increases, which causes a longer effect on neurons. Therefore, pain can radiate to the shoulders, arms, and neck. The spread of pain occurs very quickly, accompanied by the patient's panic and fear of death.
Most often, the pain syndrome has a significant duration (up to several hours). Nitroglycerin is not able to stop an attack.
Treatment of autoimmune post-infarction Dressler syndrome
Autoimmune post-infarction Dressler's syndrome is a syndrome of autoimmune origin that develops in a patient with myocardial infarction in the 2-6th week of the disease and is manifested by pericarditis, pleurisy, joint lesions (synovitis, polyarthralgia), sternocostal joints (anterior chest wall syndrome), leukocytosis , eosinophilia, increased ESR, increased body temperature.
It should be noted that all of the listed symptoms are not always present in the clinic of Dressler syndrome; only symptoms of pericarditis, pleurisy, polyarthralgia, and laboratory signs of an inflammatory process may occur. Pericarditis and pleurisy can be fibrinous or exudative.
Typical autoimmune Dressler syndrome is observed in 3.5-5.8% of patients with myocardial infarction; the frequency of autoimmune syndrome, taking into account typical, atypical and asymptomatic forms, is 15-23%.
DETAILS: The principle of operation of an MRI tomograph - who invented the device and what is its structure?
Due to the autoimmune genesis of the syndrome, prednisolone is prescribed at an initial dose of 20-40 mg per day; if there is no effect, after 2-3 days this dose is increased by 1.5-2 times. After obtaining a therapeutic effect, the daily dose of prednisolone is reduced by 2.
5 mg every 5-7 days. For mild post-infarction syndrome, the duration of treatment with prednisolone is 2-4 weeks. In case of recurrent course of the syndrome, the minimum maintenance dose of prednisolone (usually 2.5-5 mg) is taken for months.
NSAIDs (indomethacin, voltaren, ibuprofen, etc.) are prescribed only for severe pain as analgesics for several days.
Occurrence of complications
Q-infarction is a much more dangerous form of the disease than the small-focal form, since the damage in this case affects almost the entire organ. Therefore, patients with detected ischemia need to periodically visit a doctor to prevent the development of an attack and unpleasant consequences. To minimize relapse, preventive therapy is carried out.
Q-forming myocardial infarction may have the following complications:
- significant damage to the heart muscle leads to the development of an aneurysm;
- cardiac rupture resulting from myomalacia;
- inflammation of the pericardium;
- heart failure in acute or chronic stages;
- problems with rhythm of a different nature;
- thrombus formation;
- cardiogenic shock.
Myocardial infarction with a q wave is especially dangerous when a complication appears in the form of Dressler's syndrome. Most often this leads to the development of pleurisy. Usually its occurrence occurs after ischemia.
Treatment of pericarditis
Approximately 10-20% of patients in the acute period of myocardial infarction show signs of pericarditis. Most often, pericarditis develops with transmural myocardial infarction. The course of pericarditis in most cases is favorable, usually dry (fibrinous) pericarditis.
Therapeutic measures for pericarditis are as follows.
NSAIDs are prescribed - indomethacin (75-100 mg per day), voltaren or ortofen (75-100 mg per day), ibuprofen (0.6-1.2 g per day). Treatment with NSAIDs is carried out for 6-7 days while taking antacids (to avoid damage to the gastric mucosa).
In case of severe pain and insufficient effectiveness of NSAIDs, treatment with glucocorticoid drugs can be carried out. Prednisolone is prescribed in an initial daily dose of 20-40 mg with a rapid reduction; the course of treatment usually does not exceed 7-10 days. Long-term therapy with glucocorticoids is contraindicated.
How does cardiogenic shock manifest?
This is one of the most severe consequences of a heart attack. The probability of patient death with this pathology significantly exceeds 50%. The reasons for its occurrence are the following factors:
- myocarditis in acute form;
- death of heart valve tissue in acute form;
- rupture of the interventricular septum;
- pulmonary embolism with significant coverage;
- acute heart valve insufficiency;
- damage to a significant area of the heart muscle.
Against the background of a heart attack, cardiogenic shock manifests itself as follows:
- The main function of the organ, which is to pump blood, is inhibited due to significant tissue necrosis. Due to the absence of normal myocardial contractions, the pressure in the blood vessels drops, and the brain stops receiving oxygen in the required quantities. This leads to loss of consciousness, after which cardiogenic shock develops. Urine production practically does not stop due to the fact that practically no blood flows to the kidneys. This leads to death, since with such pathologies the body will be forced to stop working.
- Severe heart rhythm disturbances. Since during a heart attack the contractile function of the organ decreases, problems arise in the coherence of its work. This leads to arrhythmia, blood pressure drops sharply, which leads to impaired blood circulation between the brain and heart.
- Ventricular tamponade. Unable to withstand the pressure, the interventricular septum ruptures, and blood from different parts of the heart begins to mix. This leads to choking of the organ and lack of adequate contractions. Excess fluid cannot be pumped out into the vessels, which causes another cardiogenic shock and can result in the death of the patient.
- The occurrence of this condition is often a consequence of pulmonary embolism, when the clearance of its trunk is blocked by a thrombus. The left sections experience a blockade and do not receive blood. The patient experiences a sharp drop in blood pressure as oxygen levels rise. This happens in all organs, causing the body to stop working smoothly. The prognosis is extremely unfavorable.
Cardiogenic shock is a very dangerous condition, often leading to fatal consequences. In particular, the likelihood of its occurrence increases with large lesions of the heart muscle. Therefore, Q-infarction creates all the conditions for the development of cardiogenic shock. Patients who have had a heart attack or suffer from ischemia need to regularly visit a specialist, undergo diagnostics and take a set of preventive measures.
How is Q-wave infarction treated?
Therapy for this disease usually involves an integrated approach:
- To return the patient to normal life, restoration of coronary blood flow is necessary. This is done surgically.
- Thrombolysis allows you to do without surgery. This procedure involves injecting special medications into a patient's vein to help break up blood clots blocking blood flow. Contraindications for thrombolytic therapy occur in approximately one third of patients who have had a myocardial infarction.
- In the most advanced cases, the patient may be prescribed balloon coronary angioplasty, which is performed in the first six hours after admission to the hospital.
- Another procedure used to treat acute heart attack is coronary artery bypass grafting. This technique is usually performed in acute infarction, when complications of the disease such as post-infarction angina, as well as heart failure or cardiogenic shock, appear.
Even if the thrombolysis procedure is performed successfully, subsequent diagnosis reveals a residual stage of arterial stenosis in most patients. Therefore, the doctor may decide to perform coronary angioplasty immediately after this procedure.