Description of the pathology
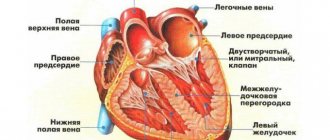
Most often, myocardial infarction of the left ventricle or simultaneous damage to both parts occurs. In right ventricular pathology, the posterior wall of the left side of the heart is usually affected. Less commonly, necrosis of the posterior wall of the right ventricle develops, subsequently spreading to its lateral or even anterior wall.
The right ventricle is a thick-walled chamber made of muscle. Its main function is to pump blood from the veins to the lungs and the left ventricle area. If there are malfunctions in the right side, the pulmonary system and left ventricle are primarily affected. This is accompanied by a decrease in pressure. A heart attack of this type is most often not an isolated disease and develops according to the following scenario:
- An ischemic focus appears in the posterior wall of the left ventricle.
- Over time, this process develops into tissue necrosis.
- As the disease progresses, the posterior wall of the right ventricle begins to die.
Such growth of the necrotic zone has a poor prognosis. But if we are talking about an isolated heart attack, then the main cause of its occurrence is the development of atherosclerosis of the right coronary artery. Due to the blockage of the vessel, an area of acute ischemia is formed, which then turns into necrosis.
Isolated right ventricular infarction usually affects three nodes:
- atrial;
- sinoatrial;
- atriovesicular.
Due to damage to the nodes described above, arrhythmias may develop against the background of right ventricular infarction. A number of other complications are also possible:
- sinus bradycardia;
- AV block;
- atrial fibrillation;
- atrial infarction (extremely rare).
Possible complications and consequences
The most severe complication is acute heart failure. There are 4 classes of deficiency manifestations with methods of their treatment:
- 1st class – there are no wheezing and “gallop rhythm” in the lungs (pathological III heart sound). Occurs in 40-50% of patients, and the mortality rate in the first class is 10%.
- Class 2 – wheezing appears in an area of less than 50% of the lung fields or a “gallop rhythm” appears. Class 2 affects 30-40% of people, and the mortality rate is 20%.
- Class 3 – wheezing on 50% of the area of the lung fields together with a “gallop rhythm”. 10-15% of people get sick, and the mortality rate is 40%.
- Class 4 – symptoms of cardiogenic shock appear (acute left ventricular failure of extreme severity). 5-20% of patients suffer from this, and mortality reaches up to 90%.
Reasons for development
If the necrotic process affects the right ventricle, this indicates a severe course of the disease. This phenomenon can occur for several reasons.
- Development of atherosclerotic changes.
- Ischemic damage.
- Myocardial necrosis from the right ventricle.
Prevention of heart attack
The most important thing is to lead a healthy lifestyle, quit bad habits, exercise moderately and keep your body weight under control. Of course, proper nutrition is important. The diet includes vegetables and herbs, root vegetables and fish and meat. Salty foods are excluded, blood pressure, sugar and cholesterol levels are controlled.
If an attack suddenly begins, you need to lie down and take an Aspirin tablet. You can also take Corvalol or Valocordin.
Read more about heart attack prevention here.
If the patient undergoes complete treatment in the hospital with strict adherence to all the doctor’s indications and instructions, this will guarantee him a complete recovery, normalize the functioning of the right ventricle and improve the very condition of the patient who has suffered a heart attack of this type.
Clinical picture
As the disease progresses, complete blockage of the vessel is possible. As a result, an ischemic area is formed, which, in the absence of timely treatment, leads to tissue necrosis.
With significant tissue death of the right ventricle, the first symptoms of its failure begin to appear. The patient experiences swelling, blood pressure decreases, and signs of hypotension may be detected due to the inferiority of the myocardium. In this case, the level of pressure in the right ventricle significantly exceeds the norm, and due to instrumental diagnostics, an enlargement of the liver is noted.
One of the most obvious signs of right ventricular infarction is a significant enlargement of the jugular veins during inspiration. This occurs due to an increase in blood flow, which the organ is no longer able to cope with. As a result, significant blood accumulations occur in the systemic circulation. Other manifestations of the disease:
- Shortness of breath, the patient complains of a constant lack of air. The reason for this is an insufficient amount of oxygen to supply the blood with oxygen.
- Substernal pain lasting from five minutes to a quarter of an hour.
- Pre-syncope, fainting and severe dizziness. This symptom is associated with low blood pressure and impaired cerebral blood supply.
- Due to lack of oxygen, confusion occurs. The patient constantly wants to sleep and has problems with thinking. Changes in mood are possible, from apathy to unmotivated aggression.
- Due to impaired blood supply to the kidneys (caused by hypotension), urine production may decrease.
- Blue discoloration of the skin of the extremities due to blood stagnation in the venous circle and oxygen starvation.
Causes
There are several factors contributing to the occurrence of right ventricular myocardial infarction. First of all, these include the following:
- atherosclerotic changes in the area of the right coronary artery;
- ischemia of the heart parts located on the right side;
- necrosis of the right ventricle.
Since the right ventricle is unable to increase stroke volume as blood flow increases, the most striking clinical sign of cardiovascular pathology is greatly enlarged jugular veins during inspiration (Kussmaul syndrome). Because of this, blood stagnates in the systemic circulation. In some cases, the blood pressure level is equal to the pressure in the atrium.
Right ventricular myocardial infarction is characterized by certain symptoms. Suspicion of pathology should be caused by:
- shortness of breath, which is caused by a lack of oxygen entering the blood;
- prolonged pain in the sternum (lasting up to 15 minutes);
- fainting, dizziness caused by low blood pressure and insufficient blood flowing to the brain;
- clouded consciousness, drowsiness, deterioration of the thinking process, lethargy or aggression;
- impaired blood supply to the kidneys and, accordingly, a decrease in the amount of urine excreted in combination with hypotension;
- cyanosis of certain areas of the skin, arms, legs due to oxygen deficiency.
If necrosis covers a significant area, not only the area of the right ventricle, a person’s blood pressure drops sharply and edema appears.
How does right ventricular infarction appear on an ECG?
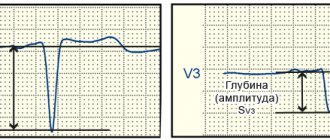
One of the most accurate methods for detecting this disease is a cardiogram. It allows you to accurately determine the presence of a pathological process. In case of acute manifestation of pathology, the following changes are noticeable on the ECG:
- ST segment elevation. With ischemic starvation of the posterior wall of the organ, a pathological Q wave may appear, which indicates the formation of a Q-infarction.
- T-wave depression is observed.
- A slight rise in the ST segment in the precordial leads while it falls in the anterior leads indicates right ventricular ischemia.
- There is a decrease in ST in lead V2.
The rise of the last segment observed in the right leads does not necessarily indicate the presence of right ventricular infarction. We may be talking about coronary artery disease. With timely assistance, such a pathology does not result in necrosis; complete restoration of blood flow is possible even without the formation of scar tissue.
It should be noted that the recovery potential of the right ventricle is higher than that of the left. This can be explained by the absence of contractions in full force, due to which not all of its energy reserves are consumed.
On the issue of ECG diagnosis of right ventricular myocardial infarction
The article draws attention to the importance of diagnosing right ventricular myocardial infarction. ECG diagnosis of right ventricular myocardial infarction is carried out by removing the so-called additional right chest leads V3R-V6R, which reveals pathological Q, ST segment elevation, negative T. The motivation for removing additional right chest leads are both the features of the clinical picture of the disease and mainly, the presence of ECG signs of inferior diaphragmatic or posterobasal myocardial infarction.
To question about ECG diagnosis of myocardial infarction of right ventricle.
The article pay attention to the importance of diagnostics of myocardial infarction of the right ventricle. ECG diagnosis of myocardial infarction of the right ventricle is carried out when removing the so-called additional right precordial leads V3R-V6R, in this case show pathological Q, rise segment ST, negative T. The motivation for the withdrawal of additional right precordial leads are both features of clinical disease and, mainly, the presence of ECG-signs inferior phrenic or posterobasal myocardial infarction.
Recognition of right ventricular myocardial infarction in widespread practice is casuistic. At the same time, its frequency is about 3%. A large number of patients have simultaneously myocardial infarction of the left and right ventricles, while right ventricular myocardial infarction is especially common in patients with damage to the lower wall of the left ventricle (up to 30% of patients). 13% of patients have a combination of myocardial infarction of the right ventricle and the anterior wall of the left ventricle. At autopsy, combined lesions of both ventricles are detected in 14-84% of the deceased (N.A. Mazur, 2009). Unfortunately (in terms of diagnosis), in patients with right ventricular myocardial infarction there are no clear specific differences in the clinical manifestations of the disease. ON THE. Mazur (2009) notes that some patients experience rapid development of right ventricular failure without stagnation of blood in the pulmonary circulation. At the same time, A.V. Shpector and E.Yu. Vasilyeva (2008) draw attention to the fact that in the acute stage of right ventricular infarction, right ventricular failure is usually manifested not by stagnation of blood in the systemic circulation, which develops later as fluid accumulates, but by hypotension. This is due to the fact that a feature of the mechanics of the right ventricle is its high dependence on preload. And therefore, if a patient with signs of right ventricular myocardial infarction has reduced blood pressure, he needs massive infusion therapy. At the same time, vasopressors are dangerous because, by increasing systemic pressure, they increase the pressure in the vessels of the pulmonary circulation, which sharply increases the load on the affected right ventricle. The volume of required infusion for hypotension associated with right ventricular myocardial infarction often reaches several liters. This is quite safe if there is an isolated lesion of the right ventricle, because with a healthy left ventricle, pulmonary edema does not develop. However, if there is combined damage to both ventricles, then the infusion must be carried out under the control of wedge pressure in the pulmonary artery to avoid overload of the pulmonary circulation. Due to the increased sensitivity of the right ventricle to preload, another feature of the treatment of right ventricular myocardial infarction is extreme caution in the use of nitrates and diuretics (as they reduce preload). Caution is also necessary in the use of morphine in such patients, because morphine has a moderate vasodilating effect.
Is it necessary to use thrombolytics for right ventricular myocardial infarction? No special studies have been conducted on this issue, but there is expert agreement on the advisability of their use, especially in the case of hypotension; Angioplasty is also indicated for patients with right ventricular myocardial infarction. It should be noted that the occurrence of atrial fibrillation in patients with right ventricular myocardial infarction leads to rapid deterioration of the condition; in such cases, urgent electrical cardioversion is necessary.
How is right ventricular myocardial infarction diagnosed in routine clinical practice using an ECG?
It is known that the right coronary artery is the common source of blood supply to both the posterior parts of the left ventricle and the right ventricle. Therefore, up to 1/3 of posterior left ventricular myocardial infarction is combined with right ventricular myocardial infarction. With the extreme right type of coronary circulation, the branches of the right coronary artery can extend to the lateral wall of the left ventricle and to the apex. A.V. Shpector and E.Yu. Vasilyeva (2009) note that 75% of patients with myocardial infarction have multiple lesions of the coronary arteries, which often leads to the development of collateral circulation. At this stage, the extent of myocardial infarction may not correspond to the classical anatomy of the coronary bed. Thus, if the patient had subtotal stenosis of the anterior interventricular artery and the blood supply to its zone was provided largely by collaterals from the right coronary artery, then thrombosis of the right coronary artery can lead to the development of a huge circular myocardial infarction.
Right ventricular myocardial infarction is diagnosed on the ECG using additional ECG leads - the so-called right chest leads: V3R-V4R-V5R-V6R. These leads must be removed in all cases of posterodiaphragmatic and posterobasal myocardial infarction, as well as when the localization of myocardial infarction according to standard ECG leads is unclear (Candell - Riera J. et al., 1981; Wenger N. et al., 1981; Goldberger A., 1984 ; Wagner G., 1994; Shevchenko N.M., 1994; Doshchitsin V.L., 1999; Mazur N.A., 2009). Registration of V3R-V6R or at least V4R in the first hours of the disease is very important for recognizing right ventricular myocardial infarction (N.A. Mazur, 2009).
In order to remove additional right chest leads, the active electrode is applied to the right half of the chest “mirror”, symmetrically with respect to the traditional chest leads (Fig. 1). In this case, electrodes V1-2 are left unchanged, and electrodes V3-6, transferred to the right half of the chest, form the right chest leads.
Figure 1. Additional right chest leads
a - diagram of the application of additional right chest leads
b — application of chest electrodes on the patient
c - ECG taken with left chest leads and additional right chest leads in a practically healthy person
In case of myocardial infarction of the right ventricle, the following changes are detected in the right precordial leads:
1) the presence of ST segment elevation of 0.5-1 mm in these leads is highly specific (however, ST segment elevation in half of the patients persists for no more than 10 hours from the onset of the disease);
2) pathological Q wave; the QRS complex has the form QR or QS (V.L. Doshchitsin, 1999). ON THE. Mazur (2009) notes that pathological Q in the right precordial leads has low specificity;
3) negative T wave;
4) in the case of necrosis of the lateral and anterior walls of the right ventricle, the same changes are recorded when electrodes V3R-V4R-V5R-V6R are applied two ribs above (Lyusov V.A. et al., 2008).
In addition, ST segment depression in leads V2 and aVF has a high predictive accuracy (about 80%); Right bundle branch block and atrioventricular block often occur.
We observed patient Sh., 70 years old, in the 11th city hospital of Kazan with extensive circular myocardial infarction, when an ECG during the first day of hospitalization initially revealed an elevation of the ST segment by 3 mm in leads V1-V4, depression of the ST segment in I, aVL, then a complete block of the right bundle branch developed, and then ST segment elevation occurred in III and aVF. ECG signs of inferior myocardial infarction (ST segment elevation in III and aVF) prompted us to take the right precordial ECG leads. When removing the right chest leads, pathological Q, ST segment elevation and negative T in V3R-V6R were detected, which indicates the development of myocardial infarction in the right ventricle as well.
We present an ECG of patient Sh., 70 years old (Fig. 2).
Figure 2. ECG of patient Sh., 70 years old.
Extensive circular myocardial infarction with a Q wave: myocardial infarction with a Q wave of the anteroseptal region of the left ventricle spreading to the apex and lateral wall of the left ventricle, myocardial infarction with a Q wave of the inferior wall of the left ventricle and right ventricle; complete right bundle branch block
Subsequent selective coronary angiography (at the Moscow Clinical Clinical Center) revealed a right coronary type of coronary circulation. The details of the angiographic study are as follows: left coronary artery - trunk without features, LAD - occlusion in the middle segment, distal LAD is not contrasted, subocclusion of the 1st arterial artery in the proximal section, OB - stenosis of the high-outgoing 1st arterial artery in the proximal segment up to 50%, stenosis of the left artery in the middle segment up to 75%. Right coronary artery - stenosis in the middle segment up to 50%, stenosis of the RV ostium up to 90%, WMA - stenosis in the middle segment up to 90% and 80%. ZMZhV - occlusion in the proximal part, the distal parts are contrasted by intrasystemic anastomoses.
So, with this message we want to draw attention to the issue of ECG diagnosis of right ventricular myocardial infarction. In routine clinical practice, with ECG signs of myocardial infarction of posterior localization, it is necessary to take an ECG in additional right chest leads V3R-V6R, which makes it possible to diagnose right ventricular myocardial infarction when a pathological Q wave, ST segment elevation and a negative T wave are detected in these leads. right ventricular myocardial infarction makes a significant correction in the management of patients with myocardial infarction.
V.N. Oslopov, O.V. Bogoyavlenskaya, Yu.V. Oslopova, M.A. Makarov, R.T. Khabibullina, M.G. Tregubova
Kazan State Medical University
City Clinical Hospital No. 11 UZ Kazan
Bogoyavlenskaya Olga Vladimirovna - Candidate of Medical Sciences, Associate Professor of the Department of Propaedeutics of Internal Diseases
Literature:
1. Mazur N.A. Practical cardiology. - M.: Medpraktika-M, 2009. - 616 p.
2. Shpector A.V., Vasilyeva E.Yu. Cardiology: clinical lectures. - M.: AST: Astrel, 2008. - 765 p.
3. Candell-Riera J., Figueras J., Valie V. et al. Right ventricular infarction. Relationships between ST segment elevation in V4R and hemodynamic, scintigraphic and echocardiographic findings in patients with acute inferior myocardial infarction. - Am. Heart J., 1981. - V. 101. - P. 281.
4. Wenger NK, Mock MB, Ringqvist I. Ambulatory electrocardiographic recording. — Chicago: Year Book Med. Publ., 1981. - 456 p.
5. Goldberger AL Myocardial infarction. Electrocardiographic differential diagnosis: 3rd ed. —St. Louis: Mosby, 1984. - 336 p.
6. Wagner GS Marriot's practical electrocardiography. 9th ed. - Baltimore: Williams & Wilkins, 1994. - 434 p.
7. Shevchenko N.M. Fundamentals of clinical electrocardiography. Qualification tests for ECG interpretation. - M.: Overley, 1994. - 156 p.
8. Doshchitsin V.L. Clinical electrocardiography. - M.: Medical Information Agency, 1999. - 373 p.
9. Lyusov V.A., Volkov N.A., Gordeev I.G. Myocardial infarction. In the book: Guide to Cardiology: Textbook in 3 volumes / ed. G.I. Storozhakova, A.A. Gorbachenkova. - M.: GEOTAR-Media, 2008. - T. 1 - P. 514-515.
Tags:Right ventricular myocardial infarction, Practical medicine 05 (10) Cardiology, ECG diagnostics
Diagnostic techniques
Determining right ventricular myocardial infarction on an ECG may not be enough to obtain a complete picture of the disease.
Therefore, in order to have all the information about the development of the pathological process, specialists use the following techniques:
- EchoCG. Performed in two-dimensional and Doppler modes. When carrying out this procedure, the doctor must pay attention to the expansion of the section being examined, the volume of ejected blood, the presence of changes in the interventricular septum, the rhythm of wall movement, etc.
- Coronary angiography. The procedure allows you to identify signs of coronary artery stenosis.
Diagnosis of an acute attack
The triad of signs that are inherent in a right ventricular infarction are: hypotension, increased volume of the jugular veins, and the fact that there is no wheezing when listening to the lungs.
These examinations help detect the following violations:
- ECG – ST above the baseline in V4R, Q wave in V1-3, rhythm disturbance in the form of atrial fibrillation or block. Changes may be limited to T shift in the right precordial leads.
- EchoCG - the pressure in the right atrium is increased, the ventricular cavity is expanded, the mobility of the wall, on which there is a zone of necrosis, is reduced. The septum between the ventricles shifts towards the left. The inferior vena cava is wider than normal and does not fall sufficiently during inspiration.
- PhonoCG – pathological 3rd tone, gallop rhythm, systolic murmur.
- Catheterization and coronary angiography - pressure in the right atrium exceeds 10 mm Hg. Art., systolic blood pressure in the system of pulmonary and other central arteries is normal or reduced.
ECG for right ventricular infarction
Features of treatment
The chosen therapy depends on the presence of complications of the disease and other pathologies accompanying its course, and the general condition of the patient. Age and gender factors play an important role.
Treatment of right ventricular infarction involves the following procedures:
- Thrombolytic therapy, which involves the introduction of special agents into the patient’s vessels that help destroy blood clots. This technique allows you to normalize the patient’s condition within a short time.
- Coronary balloon angioplasty, which allows you to expand the lumen of the artery in a minimally invasive way. During the operation, a special balloon catheter is inserted into the patient's vein. The doctor monitors his movement using X-ray equipment. Having reached the place of narrowing of the vessel, the balloon is inflated, which allows it to expand the lumen. With timely and professional intervention, it is possible to completely restore normal blood flow.
- Taking medications that increase heart rate. The most popular among them is Dobutamine.
- If arrhythmia occurs against the background of a heart attack, the patient may be prescribed Atropine. If it is impossible to take it due to contraindications, cardiac stimulation is performed.
Treatment of right ventricular infarction involves a comprehensive approach, including the following measures:
- reduction of physical activity;
- heart rate control;
- reperfusion, characterized by the resumption of normal blood flow in the ischemic zone;
- normalization of cardiac output through the use of nootropic drugs.
If arterial hypotension is detected, the patient is prescribed intravenous administration of a number of special solutions, such as “Reopoliglyukin”, “Sodium Chloride”, “Dextran”. They help improve blood circulation. If these remedies do not bring the desired results, then the doctor additionally prescribes drugs such as Dobutamine or Dopamine. If there are no expected treatment results, the patient is referred for angioplasty or thrombolytic therapy. As an additional technique, elimination of local hemodynamic consequences is used.
special instructions
When a right ventricular infarction is detected, specialists usually do not prescribe nitrate or diuretic drugs to patients. This is explained by the fact that the affected area is too sensitive to increased stress. This also applies to analgesics, which promote vasoconstriction. If taking drugs from this group is necessary to stabilize the patient’s condition, then they are replaced with analogues. As maintenance therapy, modern medicine widely uses special solutions injected into the patient’s veins. Their use can significantly alleviate the course of the disease, restore blood flow and increase blood pressure. Medications are also used to increase heart muscle contractions.
Principles of treatment
The list of common drugs includes sodium chloride, dextran or reopolyglucin. The names and names of other drugs should be checked with your doctor. These measures are aimed at increasing blood circulation. Sometimes they do not bring results, and then the doctor prescribes dopamine or dobutamine.
The last resort is balloon angioplasty or the administration of thrombolytic therapy, as well as pacemaker. Usually, to improve the patient’s condition, it is enough to normalize the blood volume and ensure a sufficient level of pressure during filling of the pancreas. Additionally, during treatment it will be necessary to eliminate local hemodynamic consequences.
- reperfusion procedures in the ischemic area;
- a sharp decrease in physical activity;
- constant heart rate monitoring;
- maintaining cardiac output by taking nootropic drugs.
Artery before and after angioplasty
Special instructions
During the treatment of myocardial infarction of the pancreas, doctors try not to prescribe diuretic and nitrate drugs, since the area of the affected area, including during ischemic damage, has excessive sensitivity to additional loads. These drugs, as well as vasoconstrictors, are usually excluded from therapy so as not to overload the pancreas area.
The introduction of special solutions for pancreatic infarction allows for a short period of time to normalize the patient’s condition and significantly alleviate a number of unpleasant symptoms. The purpose of administering the solution is to restore blood volume in the ventricle and eliminate the low pressure that accompanies this type of heart attack in the vast majority of cases.
When the use of the solution is ineffective, the patient is prescribed special medications to increase the frequency of muscle contractions. The most common medications of this type include dopamine and dobutamine. In the presence of arrhythmia, special correction with atropine is recommended; if it is impossible to take it due to various contraindications, temporary cardiac stimulation is used.
Installed pacemaker
Prevention
According to statistics, the majority of patients with identified right ventricular infarction could prevent the development of this disease. To do this, you need to at least take a responsible attitude towards your health status, namely:
- Timely identify and treat cardiac diseases (especially coronary artery disease and hypertension).
- Lead a healthy lifestyle with proper nutrition and sleep patterns.
- Give up bad habits such as smoking and alcohol.
- Move as much as possible and do cardiovascular exercises.
Consequently, right ventricular myocardial infarction is a rare and dangerous disease that, in the absence of adequate therapy, can be fatal. Only if the symptoms of the disease are detected in a timely manner and undergo a thorough examination, the patient will be able to avoid serious complications. Treatment of pathology involves an integrated approach and largely depends on the professionalism of the doctor.
Prognosis and nuances of rehabilitation
The patient’s health and life depend on the doctor’s ability to recognize symptoms and pathological changes on the electrocardiogram, make a diagnosis and prescribe the correct treatment.
It is important to know that in case of right ventricular infarction it is strictly forbidden to take nitrates (nitroglycerin) on your own. When prescribing them, careful monitoring of the patient in a hospital setting is required. Morphine is also not suitable for pain relief and is used only when absolutely necessary, since it dilates blood vessels and leads to a decrease in blood pressure and hemodynamic disturbances.
The main goal of therapy is to moderately reduce the load on the right ventricle, control the frequency and rhythm of heart contractions, regulate low blood pressure by intravenous drip administration of saline and other drugs that restore the missing blood volume (Reopoliglyukin, Reosorbilact, Stirofundin).
The treatment process is monitored using EchoCG and ECG. It is important for the patient to remain calm, since unnecessary movements, even such as moving from a horizontal to a vertical position when getting out of bed, strain the heart and can lead to aggravation of the condition.
Another nuance of recovery after a heart attack is the preference for drug treatment, since invasive interventions and studies can destabilize the functioning of the cardiovascular system. If thrombolytics are prescribed in a timely manner, surgery may not be necessary.
The consequence of transmural right ventricular infarction is often arrhythmia, which must be monitored during the recovery period, regularly conduct electrocardiography and use antiarrhythmic drugs.
Treatment of the patient
Treatment of right ventricular myocardial infarction should begin with increasing the amount of preload on the heart. This is achieved by administering saline, Polyglucin, Reopoliglucin, and colloids through a dropper. The criterion for the success of this stage is an increase in pressure in the right atrium to 15 mm Hg. Art.
It is dangerous to prescribe vasoconstrictor drugs, since they cannot increase the pressure in the arterial network in isolation without affecting the pulmonary circulation. High pressure in the blood vessels of the lungs creates excess stress on the heart.
If the effectiveness of drug therapy is weak, balloon plasty of the coronary arteries is prescribed. Thrombolytic therapy is carried out with Heparin or its low molecular weight analogues and enzymes.
The development of atrial fibrillation aggravates right ventricular failure, so it is necessary to restore the rhythm with drugs or electrical cardioversion.
When the heart rate slows down like bradycardia, Atropine is injected subcutaneously.
Myocardial infarction of the right ventricular localization is more often a consequence of extensive transmural lesions. Its development is provoked by overload of the pulmonary circulation. Typical signs are low blood pressure, absence of crackles over the lungs and engorgement of the neck veins.
We recommend reading the article about post-infarction cardiosclerosis. From it you will learn about the causes and symptoms of the pathology, types of post-infarction cardiosclerosis, diagnosis, treatment and rehabilitation.
And here is more information about myocardial hypertrophy.
To stabilize hemodynamics, plasma-substituting solutions and cardiotonics are administered; nitrates are not recommended. The course of the disease is severe with a combined infarction of both ventricles.
Recognizing myocardial infarction on an ECG can be difficult due to the fact that different stages have different signs and variations of waveforms. For example, the acute and acute stage may not be noticeable in the first hours. Localization also has its own characteristics: the infarction on the ECG is transmural, q, anterior, posterior, transferred, large-focal, lateral, different.
Post-infarction cardiosclerosis occurs quite often. He may have an aneurysm or ischemic heart disease. Recognizing symptoms and timely diagnosis will help save lives, and ECG signs will help establish the correct diagnosis. Treatment is lengthy, rehabilitation is required, and there may be complications, including disability.
The detected bundle branch block indicates many abnormalities in the functioning of the myocardium. It can be right and left, complete and incomplete, branches, anterior branches. Why is blockade dangerous in adults and children? What are the ECG signs and treatment?
Read also: Auscultation for myocardial infarction
Although not so often, myocardial rupture still occurs after a heart attack as a complication of the recovery period. The reasons may lie in non-compliance with the doctor’s recommendations. ECG readings will help identify and restore the walls of the heart and its functioning.
The causes of small-focal myocardial infarction are similar to all other types. It is quite difficult to diagnose; acute on ECG has an atypical picture. The consequences of timely treatment and rehabilitation are much easier than with a regular heart attack.
A cardiac aneurysm after a heart attack is considered a serious complication. The prognosis improves significantly after surgery. Sometimes treatment is carried out with medication. How long do people live with a post-infarction aneurysm?
Due to internal problems (defects, disorders), the load on the right atrium can be detected on the ECG. Signs of increased stress include dizziness and shortness of breath. A child's congenital heart disease is brought to her. Symptoms: increased fatigue, jaundice, and others.
As a result of increased load on the heart, right ventricular hypertrophy can develop in both adults and children. Signs are visible on the ECG. There may also be combined hypertrophy - of the right and left ventricles, right atrium and ventricle. In each case, it is decided individually how to treat the pathology.
A symptom such as pain during myocardial infarction is an important indicator. What kind of pain in the heart is there in terms of location, nature, duration? Can headaches occur or radiating headaches? Can you have a heart attack without pain?